©The Author(s) 2026.
World J Stem Cells. Jan 26, 2026; 18(1): 113614
Published online Jan 26, 2026. doi: 10.4252/wjsc.v18.i1.113614
Published online Jan 26, 2026. doi: 10.4252/wjsc.v18.i1.113614
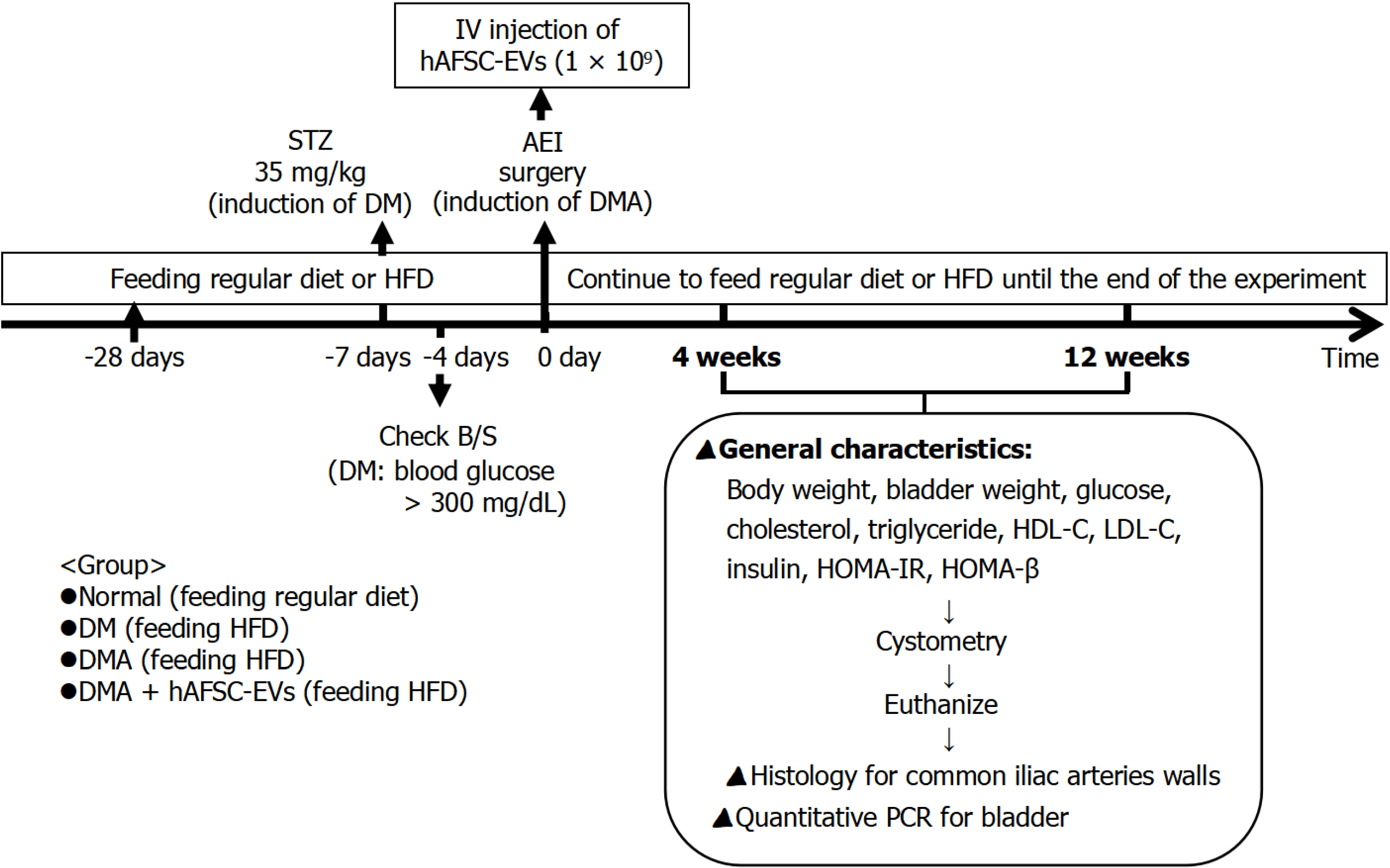
Figure 1 Flowchart of the experimental procedures.
IV: Intravenous injection; hAFSC-EVs: Human amniotic fluid stem cell-derived extracellular vesicles; STZ: Streptozotocin; AEI: Arterial balloon endothelial injury; DM: Diabetes mellitus; DMA: Diabetic atherosclerosis; HFD: High-fat diet; B/S: Blood sugar; HDL-C: High-density lipoprotein cholesterol; LDL-C: Low-density lipoprotein cholesterol; HOMA-IR: Homeostasis model assessment insulin resistance; HOMA-β: Homeostasis model assessment-β; PCR: Polymerase chain reaction.
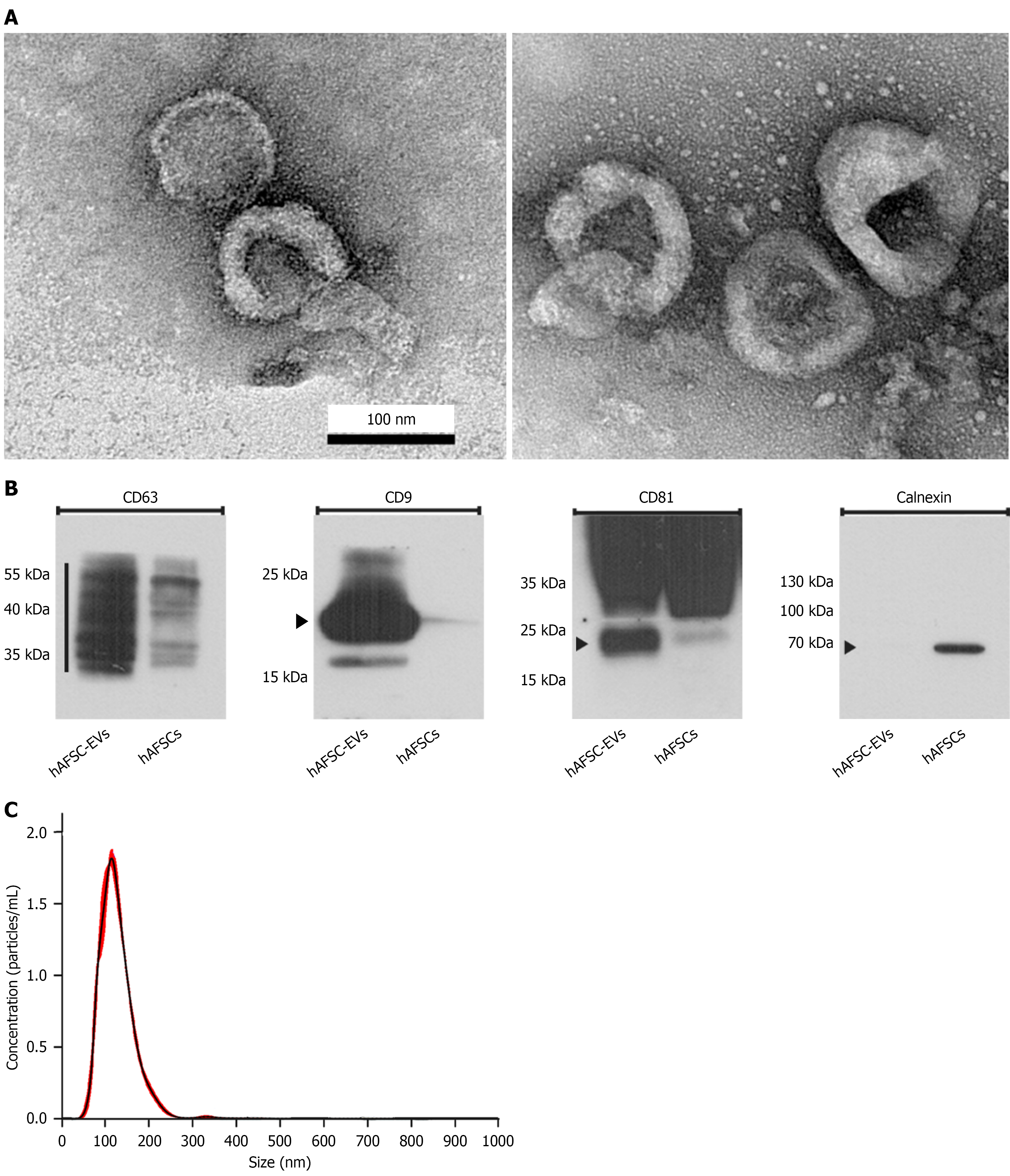
Figure 2 Characterization of human amniotic fluid stem cell-derived extracellular vesicles.
Transmission electron microscopy shows that human amniotic fluid stem cell-derived extracellular vesicles exhibit a bilayered spherical morphology with diameters ranging from 50 nm to 150 nm. Bars indicate 100 nm. Western blot analysis confirms the expression of exosomal surface markers CD63, CD81, and CD9. Nanoparticle tracking analysis reveals that the majority of human amniotic fluid stem cell-derived extracellular vesicles fall within the 50-150 nm size range. A: Transmission electron microscopy; B: Western blot analysis; C: Nanoparticle tracking analysis. hAFSC-EVs: Human amniotic fluid stem cell-derived extracellular vesicles; hAFSCs: Human amniotic fluid stem cells.
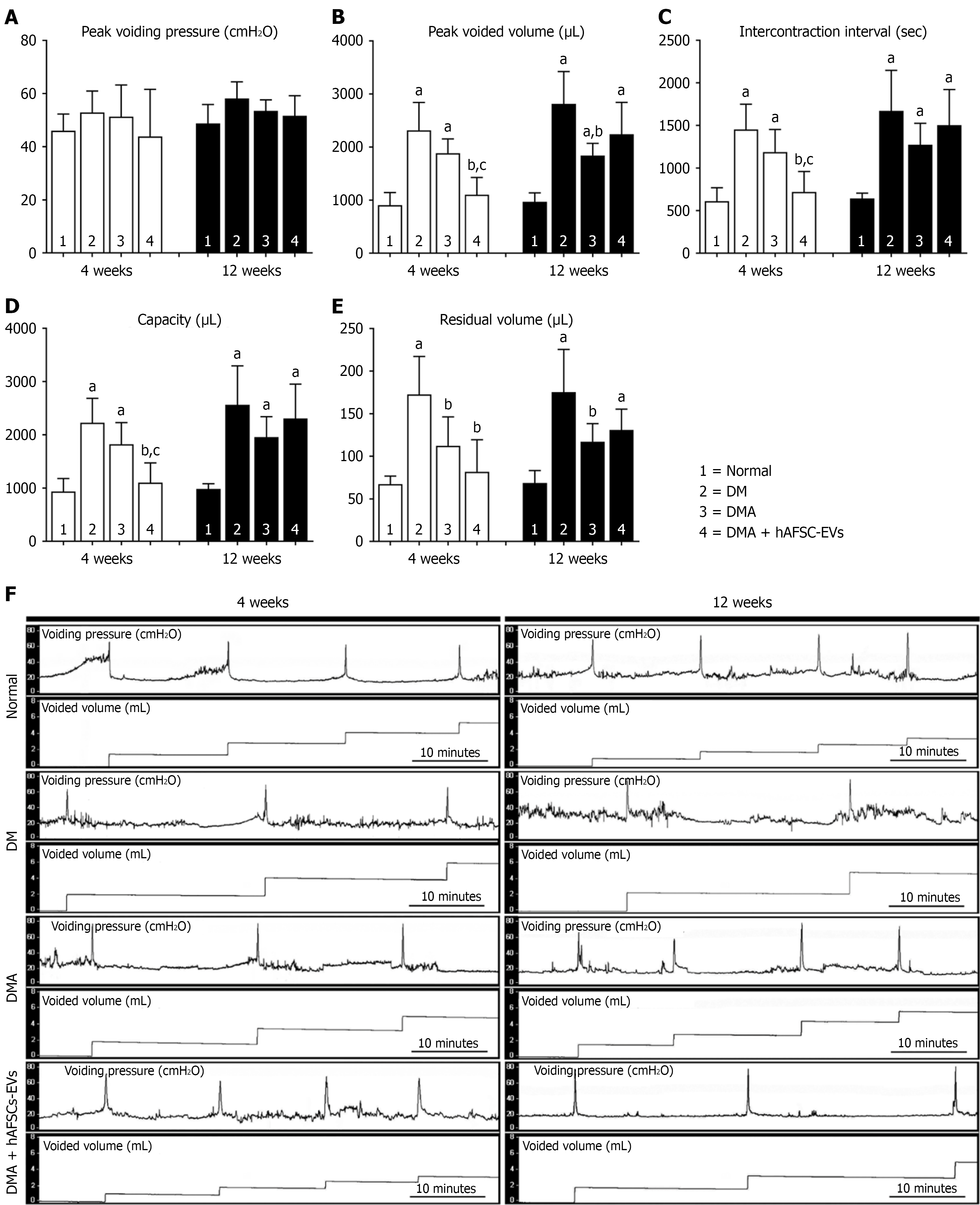
Figure 3 Cystometric evaluation of bladder function.
A-F: At 4 weeks and 12 weeks after induction, peak voided volume, intercontraction interval and bladder capacity were significantly increased in both diabetes mellitus (DM) and diabetic atherosclerosis (DMA) groups compared with the control group, whereas residual volume was elevated only in the DM group. Furthermore, compared with the DM group, DMA rats had significantly reduced residual volume at 4 weeks and 12 weeks after induction, and peak voided volume was decreased at 12 weeks. In DMA rats treated with human amniotic fluid stem cell-derived extracellular vesicles, peak voided volume, intercontraction interval and bladder capacity were significantly reduced at 4 weeks after induction. P values are shown in each comparison. Cystometric variables include: Peak voiding pressure (A); peak voided volume (B); intercontraction interval (C); bladder capacity (D); residual volume (E); representative cystometry tracings for normal, DM, DMA, and DMA + human amniotic fluid stem cell-derived extracellular vesicles groups at 4 weeks and 12 weeks after induction (F). aP < 0.05 vs normal control, bP < 0.05 vs diabetes mellitus, cP < 0.05 vs diabetic atherosclerosis. DM: Diabetes mellitus; DMA: Diabetic atherosclerosis; hAFSC-EVs: Human amniotic fluid stem cell-derived extracellular vesicles.
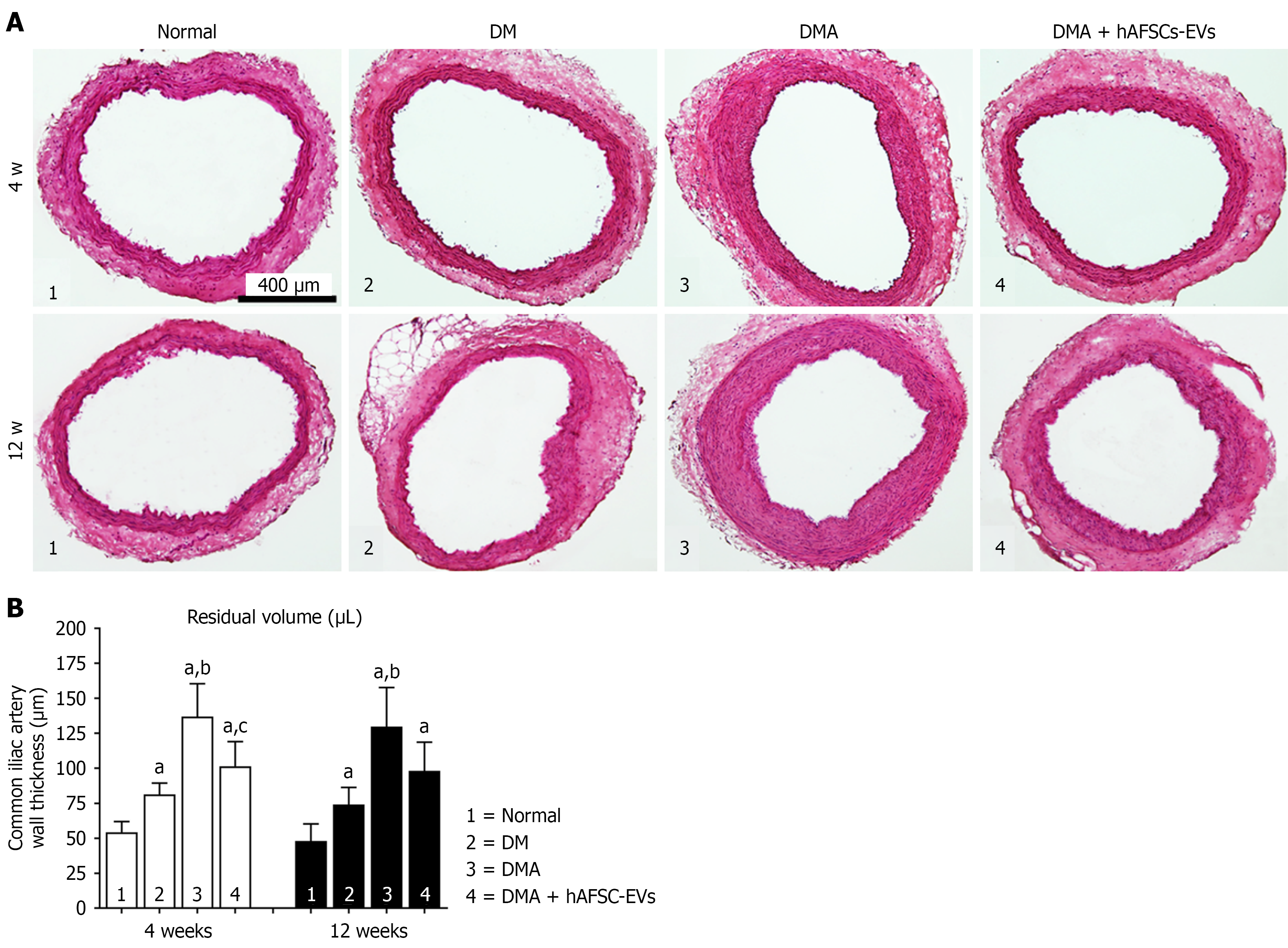
Figure 4 Histological findings of the common iliac arteries.
The intima thickness of the common iliac arteries in the diabetic atherosclerosis group significantly increased compared with the control and diabetes mellitus groups. However, the intima thickness of diabetic atherosclerosis rats treated with human amniotic fluid stem cell-derived extracellular vesicles was significantly reduced at 4 weeks after induction. Bars indicate 400 μm. A: Hematoxylin and eosin staining of the common iliac arteries; B: Common iliac artery wall thickness. aP < 0.05 vs normal control, bP < 0.05 vs diabetes mellitus, cP < 0.05 vs diabetic atherosclerosis. DM: Diabetes mellitus; DMA: Diabetic atherosclerosis; hAFSC-EVs: Human amniotic fluid stem cell-derived extracellular vesicles.
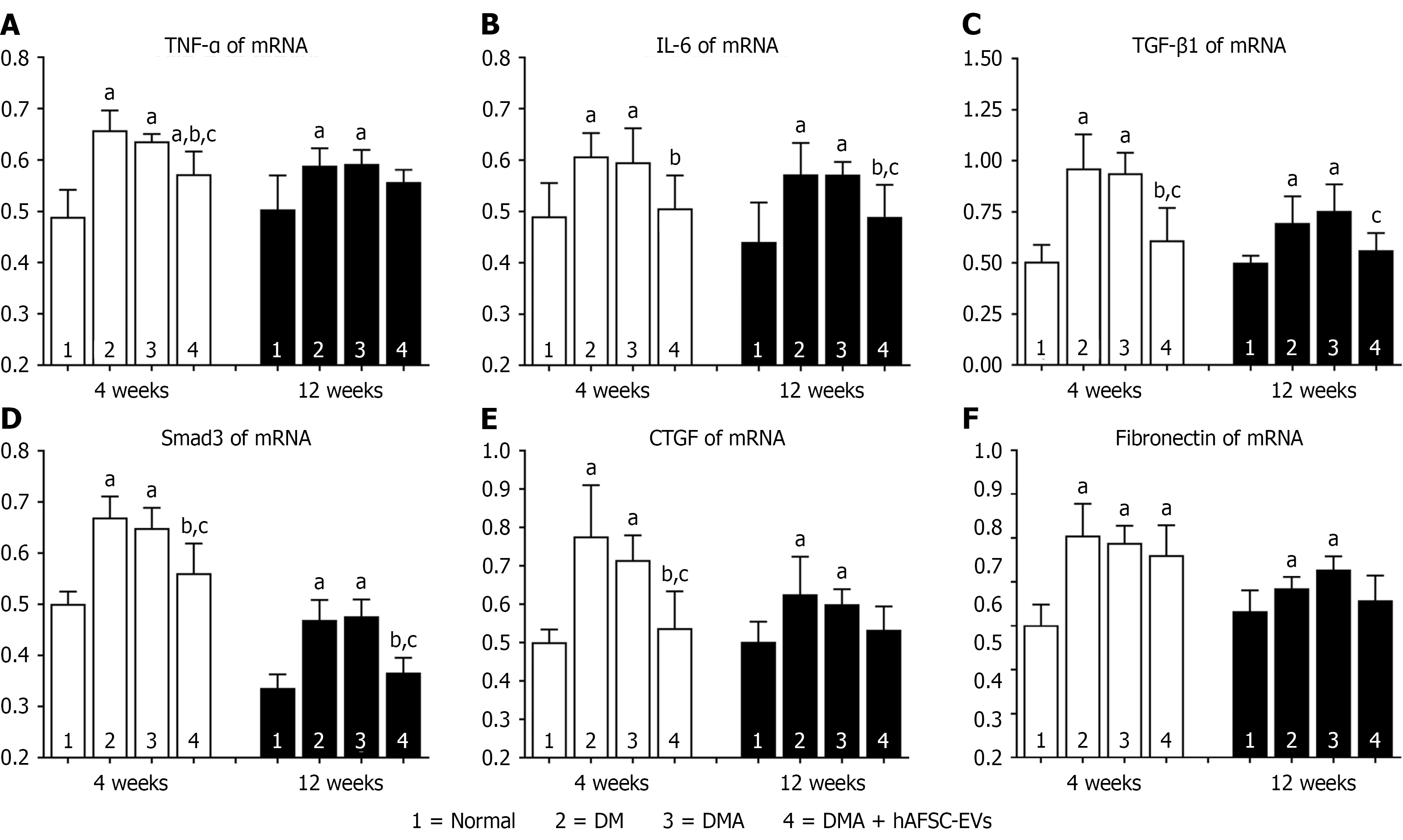
Figure 5 Relative mRNA expressions of tumor necrosis factor-α, interleukin-6, transforming growth factor-β1, Smad3, connective tissue growth factor, and fibronectin in the bladder of control and diabetic groups.
A-F: Compared with the control group, diabetes mellitus and diabetic atherosclerosis (DMA) bladders showed significant increases in the mRNA expression of tumor necrosis factor α (TNF-α), interleukin-6 (IL-6), transforming growth factor β1 (TGF-β1), Smad3, connective tissue growth factor (CTGF), and fibronectin at 4 weeks and 12 weeks after induction. Compared with the diabetes mellitus and DMA groups, the mRNA expression of TNF-α, TGF-β1, and CTGF in DMA rats treated with human amniotic fluid stem cell-derived extracellular vesicles were significantly decreased at 4 weeks after induction, while the mRNA expression of IL-6 and Smad3 were significantly decreased 12 weeks. aP < 0.05 vs normal control (4 weeks and 12 weeks), bP < 0.05 vs diabetes mellitus (4 weeks and 12 weeks), cP < 0.05 vs diabetic atherosclerosis (4 weeks and 12 weeks). TNF: Tumor necrosis factor; IL: Interleukin; TGF: Transforming growth factor; CTGF: Connective tissue growth factor; DM: Diabetes mellitus; DMA: Diabetic atherosclerosis; hAFSC-EVs: Human amniotic fluid stem cell-derived extracellular vesicles.
- Citation: Liang CC, Lin YH, Liang CY, Ro A, Huang YH, Shaw SW. Extracellular vesicles derived from human amniotic fluid stem cells improve bladder dysfunction in rat model of diabetic atherosclerosis. World J Stem Cells 2026; 18(1): 113614
- URL: https://www.wjgnet.com/1948-0210/full/v18/i1/113614.htm
- DOI: https://dx.doi.org/10.4252/wjsc.v18.i1.113614