修回日期: 2025-04-16
接受日期: 2025-05-08
在线出版日期: 2025-05-28
对于无法经口进食的患者, 胃造瘘的最佳应用技术一直存在争议, 目前外科胃造瘘术在临床上已较少应用, 而经皮内镜胃造瘘术(percutaneous endoscopic gastrostomy, PEG)和X线或CT引导下经皮穿刺胃造瘘术(percutaneous radiologic gastrostomy, PRG)应用较为广泛.
系统评价经皮内镜胃造瘘术和X线或CT引导下经皮穿刺胃造瘘术的临床疗效.
截止至2024-12, 在PubMed、Embase、Cochrane Library、中国生物医学数据库、中国知网、万方、维普等数据库收集关于PEG和PRG对比的临床研究, 对纳入的文献进行资料提取和质量评价后, 采用RevMan5.3软件进行Meta分析.
(1)共纳入16篇研究, 总计2770例患者; (2)结果显示: PEG和PRG在置管成功率(95%CI: 0.01-0.12, P<0.05)、瘘管堵塞或狭窄(95%CI: 0.23-0.50, P<0.05)、30天死亡率(95%CI: 0.42-0.95, P<0.05)差异有显著性意义; (3)但2种方法在瘘口感染(95%CI: 0.53-1.10, P>0.05)、疼痛(95%CI: 0.40-1.32, P>0.05)、腹膜炎(95%CI: 0.36-3.94, P>0.05)方面差异无显著性意义.
提示PRG组在置管成功率方面优于PEG组, PEG组术后瘘管堵塞或狭窄发生率、术后30 d死亡率较PRG组更低, 但二者在瘘口感染、疼痛、腹膜炎方面没有统计学差异.
核心提要: 胃造瘘的最佳应用技术临床存在争议, 目前中文期刊未搜索到相关系统评价, 本文通过荟萃分析, 为临床提供胃造瘘术的建议.
引文著录: 胡云凯, 贺博武, 苏玉钢, 陈永堂, 茹清静. 经皮内镜胃造瘘术与X线或CT引导下经皮穿刺胃造瘘术置入效果的Meta分析. 世界华人消化杂志 2025; 33(5): 412-422
Revised: April 16, 2025
Accepted: May 8, 2025
Published online: May 28, 2025
The optimal technique for gastrostomy in patients with impaired oral intake remains controversial. While surgical gastrostomy has become less common in clinical practice, percutaneous endoscopic gastrostomy (PEG) and percutaneous radiologic gastrostomy (PRG) have emerged as the predominant techniques.
To systematically evaluate the clinical efficacy of PEG vs PRG.
A comprehensive literature search was conducted in PubMed, Embase, Cochrane Library, CBM, CNKI, Wanfang, and VIP databases up to December 2024. Comparative clinical studies on PEG and PRG were included. Data extraction and quality assessment were performed, followed by Meta-analysis using RevMan 5.3 software.
Sixteen studies involving 2770 patients were included. Significant differences were observed in tube placement success rate (95% confidence interval [CI]: 0.01-0.12, P < 0.05), tube obstruction/stricture (95%CI: 0.23-0.50, P < 0.05), and 30-day mortality (95%CI: 0.42-0.95, P < 0.05), favoring PRG for procedural success and PEG for reduced tube-related complications and mortality. No statistical differences were found in stoma infection (95%CI: 0.53-1.10, P > 0.05), pain (95%CI: 0.40-1.32, P > 0.05), or peritonitis (95%CI: 0.36-3.94, P > 0.05).
The PRG group demonstrated superior catheterization success rates compared to the PEG group. However, the PEG group exhibited lower incidences of postoperative fistula obstruction/stenosis and lower 30-day postoperative mortality rates. No statistically significant differences were observed between the two groups in terms of stoma infection, pain, or peritonitis.
- Citation: Hu YK, He BW, Su YG, Chen YT, Ru QJ. Meta-analysis of clinical efficacy of percutaneous endoscopic gastrostomy vs percutaneous radiologic gastrostomy. Shijie Huaren Xiaohua Zazhi 2025; 33(5): 412-422
- URL: https://www.wjgnet.com/1009-3079/full/v33/i5/412.htm
- DOI: https://dx.doi.org/10.11569/wcjd.v33.i5.412
据报道, 全球约有29%-33%的住院患者存在营养不良的状况, 同时有高达43%的患者存在营养不良的风险[1,2]. 适当的营养支持能防止肠道内细菌和内毒素的移位, 促进人体代谢, 保持消化道粘膜屏障和网状内皮细胞的正常功能[3,4]. 因此, 对于吞咽困难或无法经口进食的患者, 进行必需的营养支持治疗对患者的健康恢复有着积极意义. 胃造瘘术的常见技术包括外科胃造瘘术、经皮内镜胃造瘘术(percutaneous endoscopic gastrostomy, PEG)、X线或CT引导下经皮穿刺胃造瘘术(percutaneous radiologic gastrostomy, PRG)[5]. 目前, 外科胃造瘘术在临床上已较少应用, 而PEG和PRG应用较为成熟、广泛和安全[6,7]. 过去经皮内镜胃造瘘术是肠内营养支持的首选治疗手段. 然而, 对于严重食管裂孔疝或上消化道狭窄的患者, PEG容易失败, 而PRG可有效避开梗阻段, 越来越受到临床医师的重视. 但目前对经皮内镜胃造瘘术和X线或CT引导下经皮穿刺胃造瘘术缺乏大样本研究, 二者在技术成功率、术后并发症、死亡率等方面也存在较大争议.
文章通过对符合纳入标准的文献进行Meta分析, 通过对比二者在置管成功率、轻微并发症、严重并发症, 死亡率等方面的差异, 比较PEG和PRG进行肠内营养支持的优劣, 为临床决策提供依据.
1.1.1 文献检索方法: 计算机检索PubMed、EMBASE、Cochrane Library、中国生物医学数据库、中国知网、万方、维普等数据库, 检索时间自数据库建立至2024-12, 英文检索词: Gastrostomy, percutaneous endoscopic gastrostomy, percutaneous radiologic gastrostomy, radiologically inserted gastrostomy; 中文检索词: 胃造瘘术, 经皮内镜胃造瘘术, 经皮放射胃造瘘术, X线引导下经皮穿刺胃造瘘术, CT引导下经皮穿刺胃造瘘术.
1.2.1 纳入标准: (1)短期内(4 wk)不太可能经口进食的患者, 且伴有高度的营养不良的风险; (2)国内外发表的经皮内镜胃造瘘术和X线或CT引导下经皮穿刺胃造瘘术进行营养支持的病例对照研究或队列研究; (3)各组样本量均需≥10; (4)研究成果以论文形式发表, 并能获取原文.
1.2.2 排除标准: (1)研究对象为儿童患者; (2)文献类型为综述、会议论文、个案报道等; (3)the Newcastle-Ottawa Scale评分≤5分的文献; (4)存在数据雷同或抄袭、反复发表、或无法获取原文数据的文献.
此项Meta分析的评价指标包括置管成功率、轻微并发症(瘘口感染、造瘘管堵塞或狭窄、疼痛)、严重并发症(腹膜炎), 30 d死亡率. 由两位研究员分析、审核所有文献及数据, 如遇分歧, 采取讨论解决或第三方协助裁定. 所纳入的文献质量由质量评估员评估, 随机对照试验采用Cochrane系统评价标准, 回顾性研究采用NOS评分.
统计学处理 采用RevMan 5.3软件进行分析. OR表示计数资料, WMD表示计量资料, 两者均给出95%CI. 当各研究间有统计学异质性(P<0.05, I2>50%时), 采用随机效应模型进行分析, 或考虑采用亚组分析、敏感性分析; 反之则采用固定效应模型.
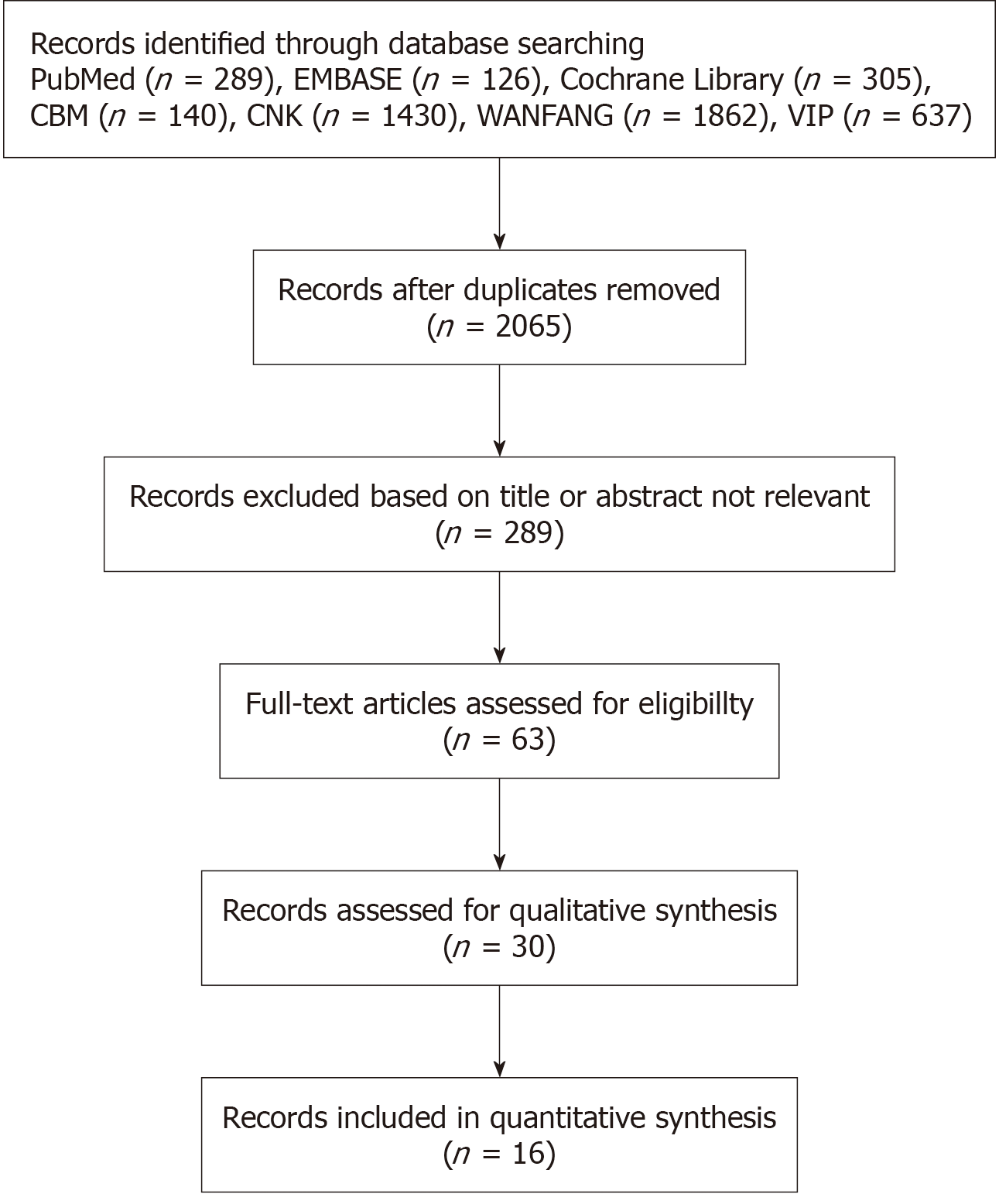
初步检索出相关文献4196篇, 根据纳入及排除标准进行剔除, 最终纳入16篇文献[8-23]. 其中13篇回顾性研究[8-11,13-15,17-21,23], 3篇随机对照研究[12,16,22], 随机对照研究根据Cochrane风险评估为低风险, 回顾性研究根据NOS评分标准, 其中13篇文献中, 1篇为稍高质量文献, 12篇均为中等质量文献, 纳入的13篇文献中共计2770例患者, 文献流程图、纳入研究基本特征、NOS评分表详见图1, 表1和表2.
| 研究 | 国家 | 稿件类型 | 治疗方法 | 样本量 | 年龄(year) | 性别(M/F) | 结果指标 |
| Wollman and D'Agostino[8], 1997 | United States | Retrospective | PEG; PRG | 114 | 55 | 71/43 | ①②③④⑤⑥ |
| 68 | 54 | 38/30 | |||||
| Bazarah et al[9], 2001 | Saudi Arabia | Retrospective | PEG; PRG | 19 | 65 | 14/5 | ①⑤⑥ |
| 33 | 51 | 16/17 | |||||
| Neeff et al[10], 2003 | New Zealand | Retrospective | PEG; PRG | 56 | 65 | 43/13 | ①⑤ |
| 18 | 66 | 13/5 | |||||
| Silas et al[11], 2005 | United States | Retrospective | PEG; PRG | 177 | 68±15 | 100/77 | ②③④ |
| 193 | 63±14 | 114/79 | |||||
| Desport et al[12], 2005 | France | Prospective | PEG; PRG | 30 | 65.7±10.3 | Not described | ①④⑥ |
| 20 | 66.1±9.7 | ||||||
| Eze et al[13], 2006 | United Kingdom | Retrospective | PEG; PRG | 44 | Not described | Not described | ⑤⑥ |
| 15 | |||||||
| MacLean et al[14], 2007 | United States | Retrospective | PEG; PRG | 268 | 51±21 | 115/155 | ①③ |
| 110 | 57±19 | 74/36 | |||||
| Galaski et al[15], 2009 | Canada | Retrospective | PEG; PRG | 30 | 55±21 | 19/11 | ②③ |
| 40 | 65±19 | 31/9 | |||||
| Leeds et al[16], 2009 | United Kingdom | Prospective | PEG; PRG | 233 | 61.6 | 146/87 | ⑥ |
| 170 | 62.8 | 119/51 | |||||
| La Nauze et al[17], 2012 | Australia | Retrospective | PEG; PRG | 80 | 61 | 53/27 | ②④⑤ |
| 97 | 61 | 69/28 | |||||
| Allen et al[18], 2012 | United States | Retrospective | PEG; PRG | 57 | 61.7 | Not described | ①⑥ |
| 51 | 61.2 | ||||||
| McAllister et al[19], 2013 | United Kingdom | Retrospective | PEG; PRG | 21 | Not described | Not described | ③⑥ |
| 89 | |||||||
| Vidhya et al[20], 2018 | Australia | Retrospective | PEG; PRG | 85 | 65 | Not described | ②③⑤⑥ |
| 52 | 64 | ||||||
| Park et al[21], 2018 | Korea | Retrospective | PEG; PRG | 324 | 66.7±14.8 | 234/90 | ②③④ |
| 94 | 66.2±13.3 | 58/36 | |||||
| Sundbom et al[22], 2023 | Sweden | Prospective | PEG; PRG | 51 | 51 | 28/23 | ②④⑥ |
| 55 | 56 | 30/25 | |||||
| Du et al[23], 2023 | China | Retrospective | PEG; PRG | 38 | 67.1±7.7 | 19/19 | ①②③④ |
| 38 | 65.6±8.2 | 21/17 |
| 研究 | 选择 | 可比性 | 暴露 |
| Wollman and D'Agostino[8], 1997 | ★★ | ★★ | ★★ |
| Bazarah et al[9], 2001 | ★★ | ★★ | ★★ |
| Neeff et al[10], 2003 | ★★ | ★★ | ★★ |
| Silas et al[11], 2005 | ★★ | ★★ | ★★ |
| Eze et al[13], 2006 | ★★ | ★★ | ★★ |
| MacLean et al[14], 2007 | ★★★ | ★★ | ★★ |
| Galaski et al[15], 2009 | ★★ | ★★ | ★★ |
| La Nauze et al[17], 2012 | ★★ | ★★ | ★★ |
| Allen et al[18], 2012 | ★★ | ★★ | ★★ |
| McAllister et al[19], 2013 | ★★ | ★★ | ★★ |
| Vidhya et al[20], 2018 | ★★ | ★★ | ★★ |
| Park et al[21], 2018 | ★★ | ★★ | ★★ |
| Du et al[23], 2023 | ★★ | ★★ | ★★ |
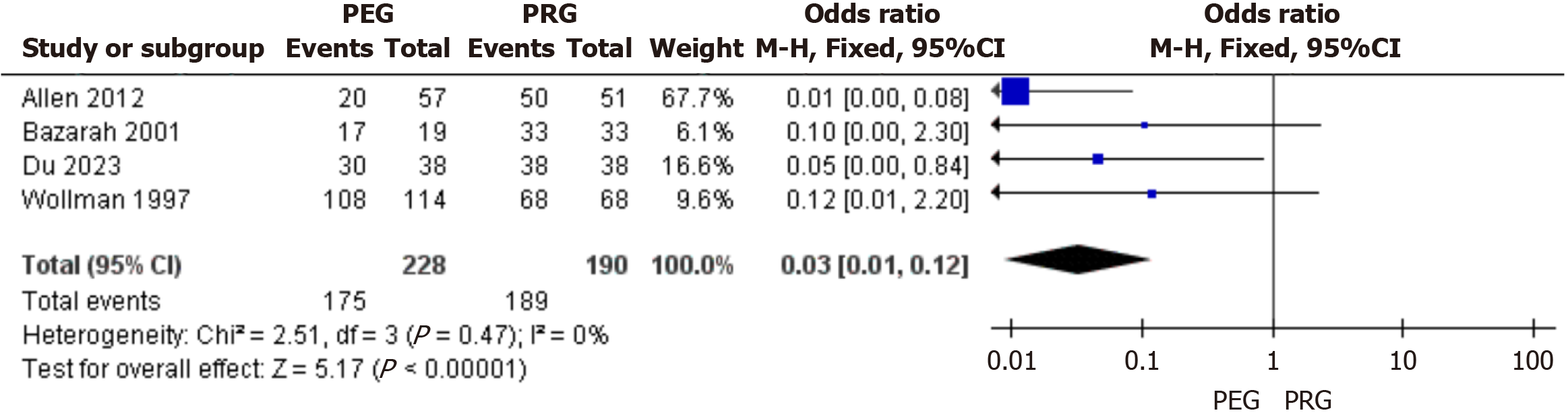
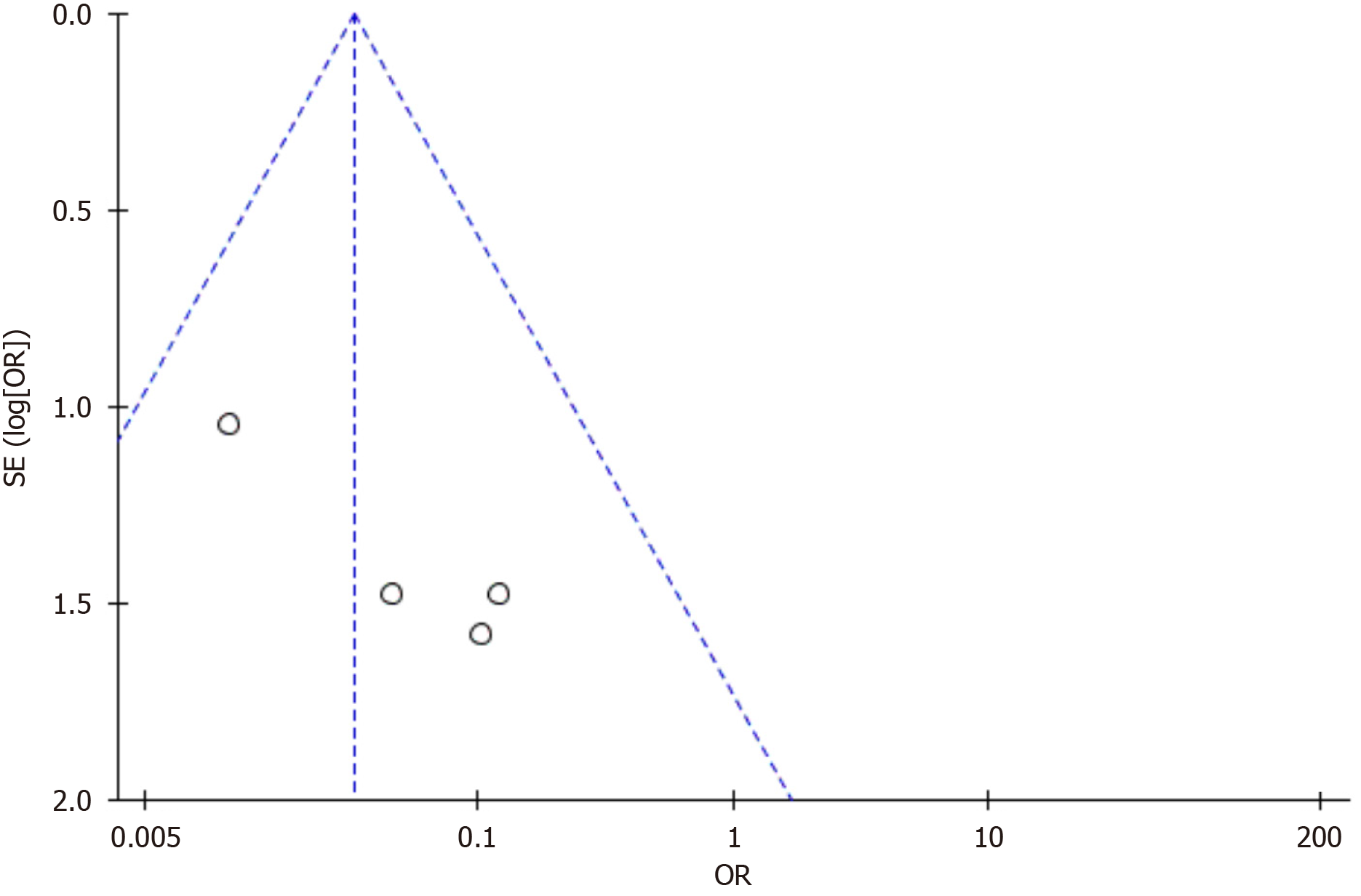
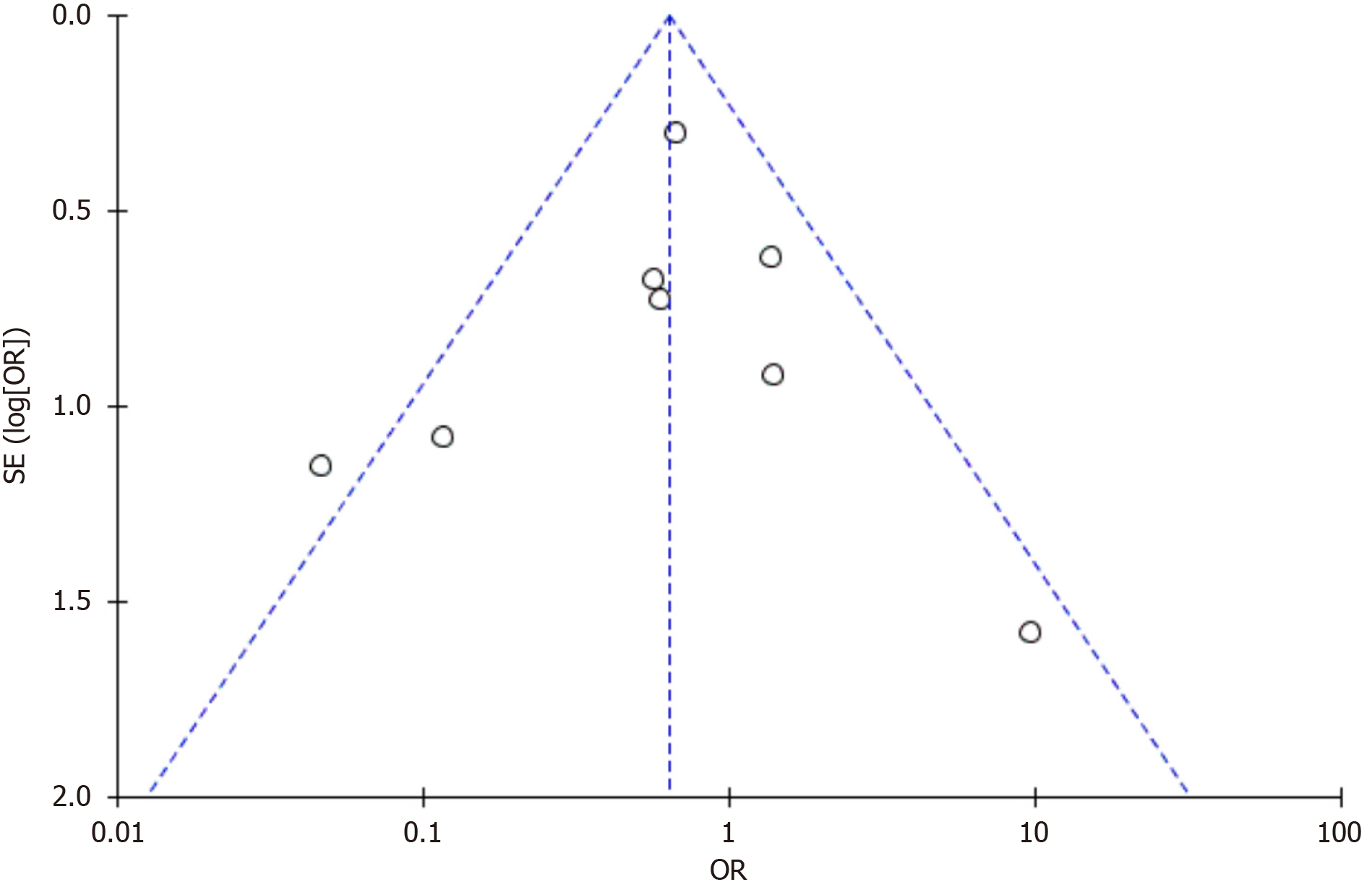
2.2.1 置管成功率: 纳入4篇文献对PEG和PRG置管成功率做了比较[8,9,18,23], 各研究结果间异质性较低(I2 = 0%), 采用固定效应模型进行合并分析. 结果显示: 相对于经皮内镜胃造瘘术, X线或CT引导下经皮穿刺胃造瘘术置管成功率更高, 2组间差异有显著性意义(95%CI: 0.01-0.12, P<0.05), 漏斗图显示可能存在发表偏移, 见图2和图3.
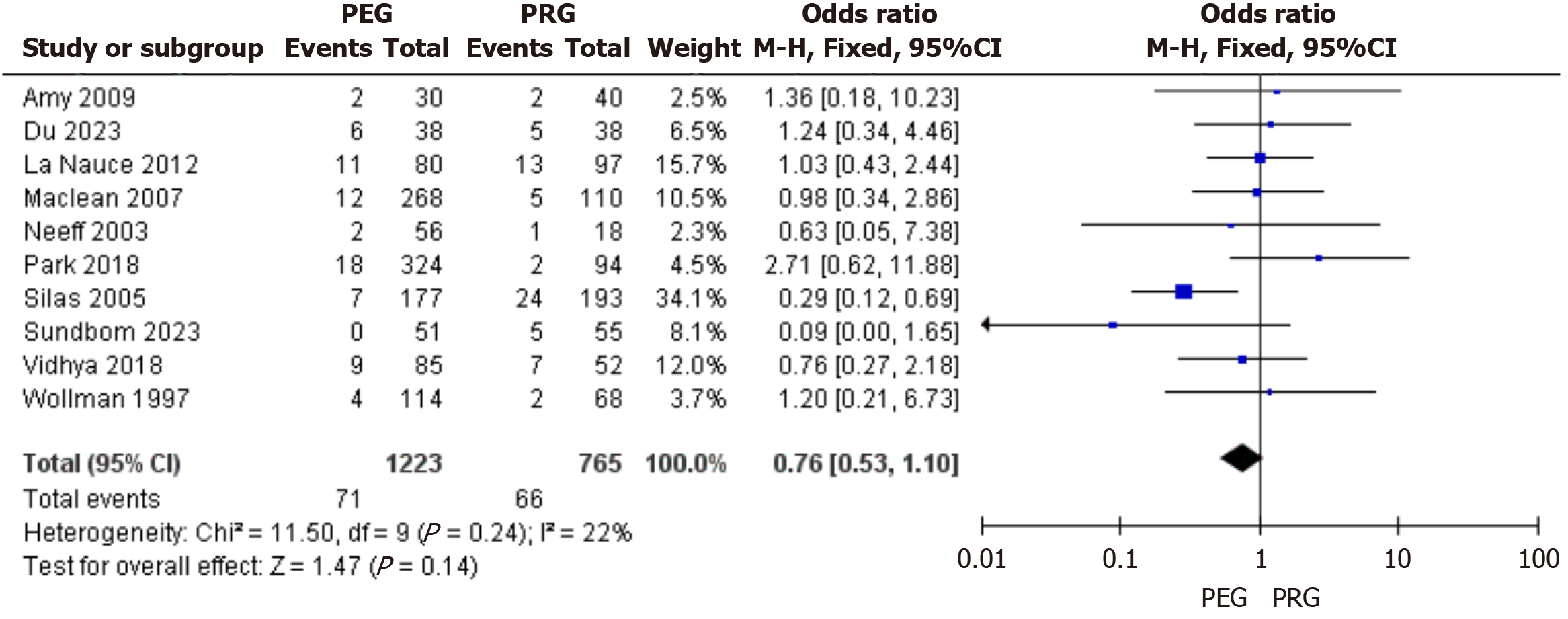
2.2.2 瘘口感染: 纳入10篇文献对PEG和PRG术后瘘口感染率做了比较[8,10,11,14,15,17,20-23], 各研究结果间异质性较低(I2 = 22%), 采用固定效应模型进行合并分析. 结果显示: 经皮内镜胃造瘘术相对于X线或CT引导下经皮穿刺胃造瘘术在术后瘘口感染率方面差异无显著性意义(95%CI: 0.53-1.10, P>0.05), 漏斗图显示可能存在发表偏倚, 见图4和图5.
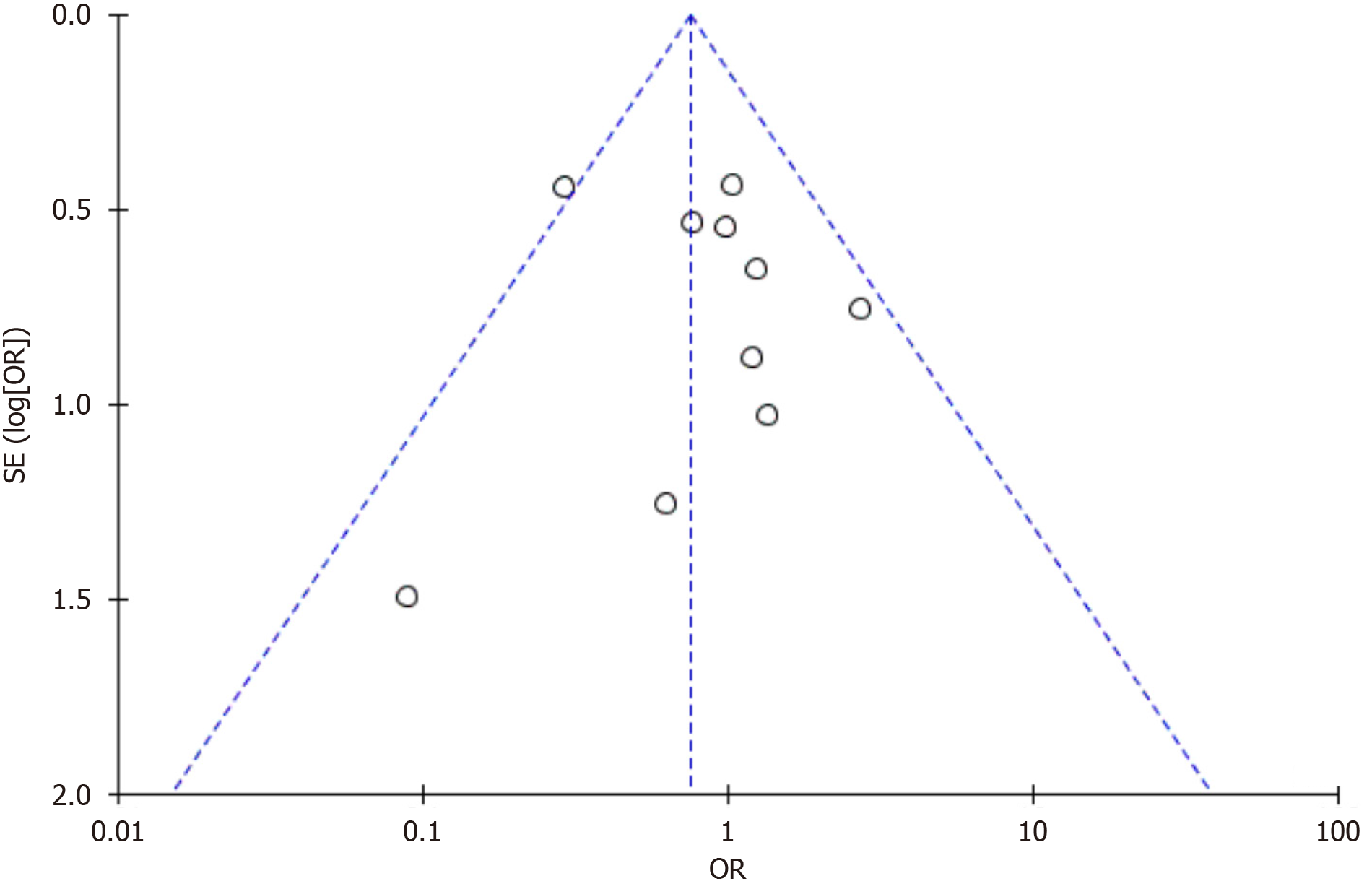
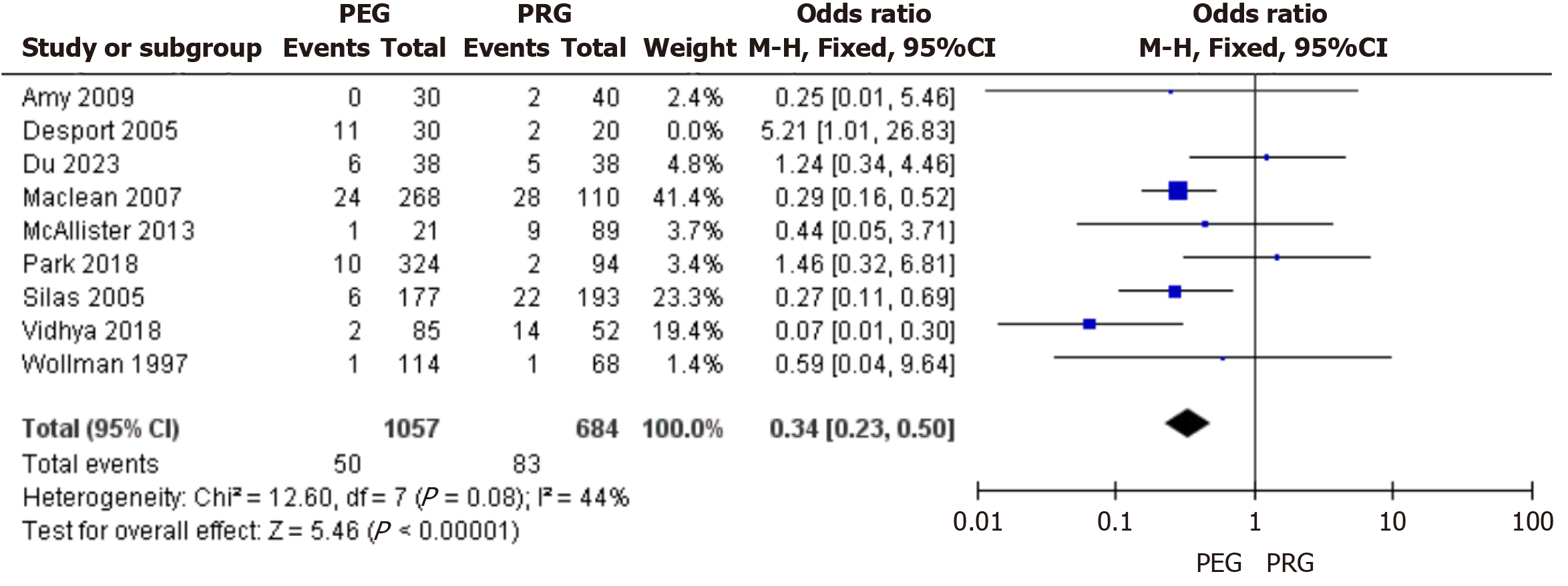
2.2.3 瘘管堵塞或狭窄: 纳入9篇文献对PEG和PRG术后瘘管堵塞或狭窄发生率做了比较[8,11,12,14,15,19,20,21,23], 各研究结果间异质性较低(I2 = 44%), 采用固定效应模型进行合并分析. 结果显示: 相对于X线或CT引导下经皮穿刺胃造瘘术, 经皮内镜胃造瘘术术后瘘管堵塞或狭窄发生率更低, 2组间差异有显著性意义(95%CI: 0.23-0.50, P<0.05), 漏斗图显示不存在发表偏倚, 见图6和图7.
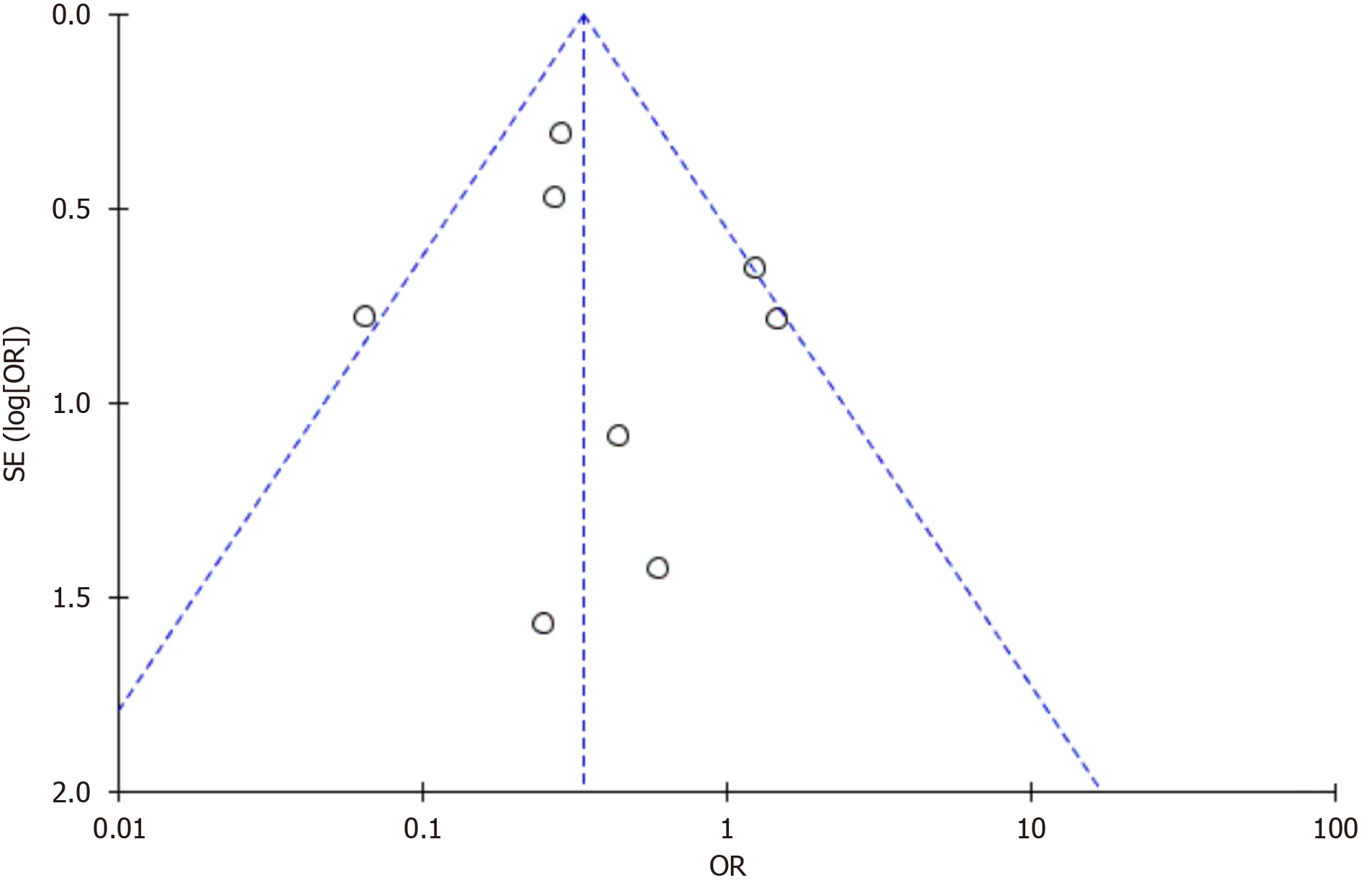
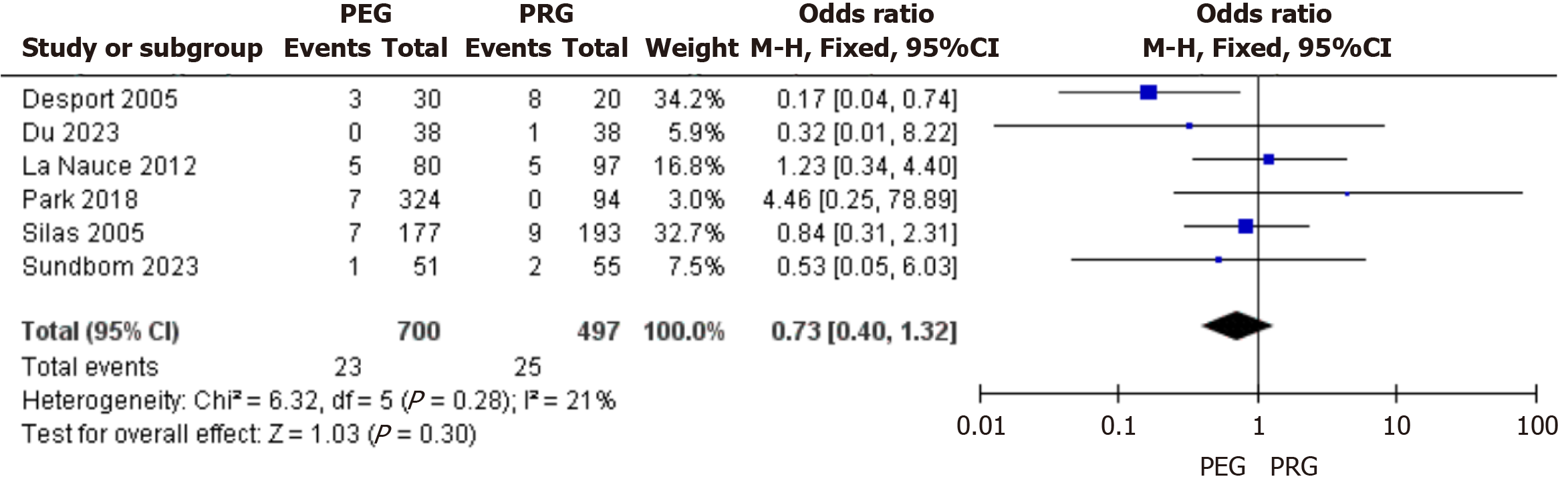
2.2.4 疼痛: 纳入6篇文献对PEG和PRG术后疼痛发生率做了比较[11,12,17,21-23], 各研究结果间异质性较低(I2 = 21%), 采用固定效应模型进行合并分析. 结果显示: 经皮内镜胃造瘘术相对于X线或CT引导下经皮穿刺胃造瘘术在术后疼痛发生率方面差异无显著性意义(95%CI: 0.40-1.32, P>0.05), 漏斗图显示不存在发表偏倚, 见图8和图9.
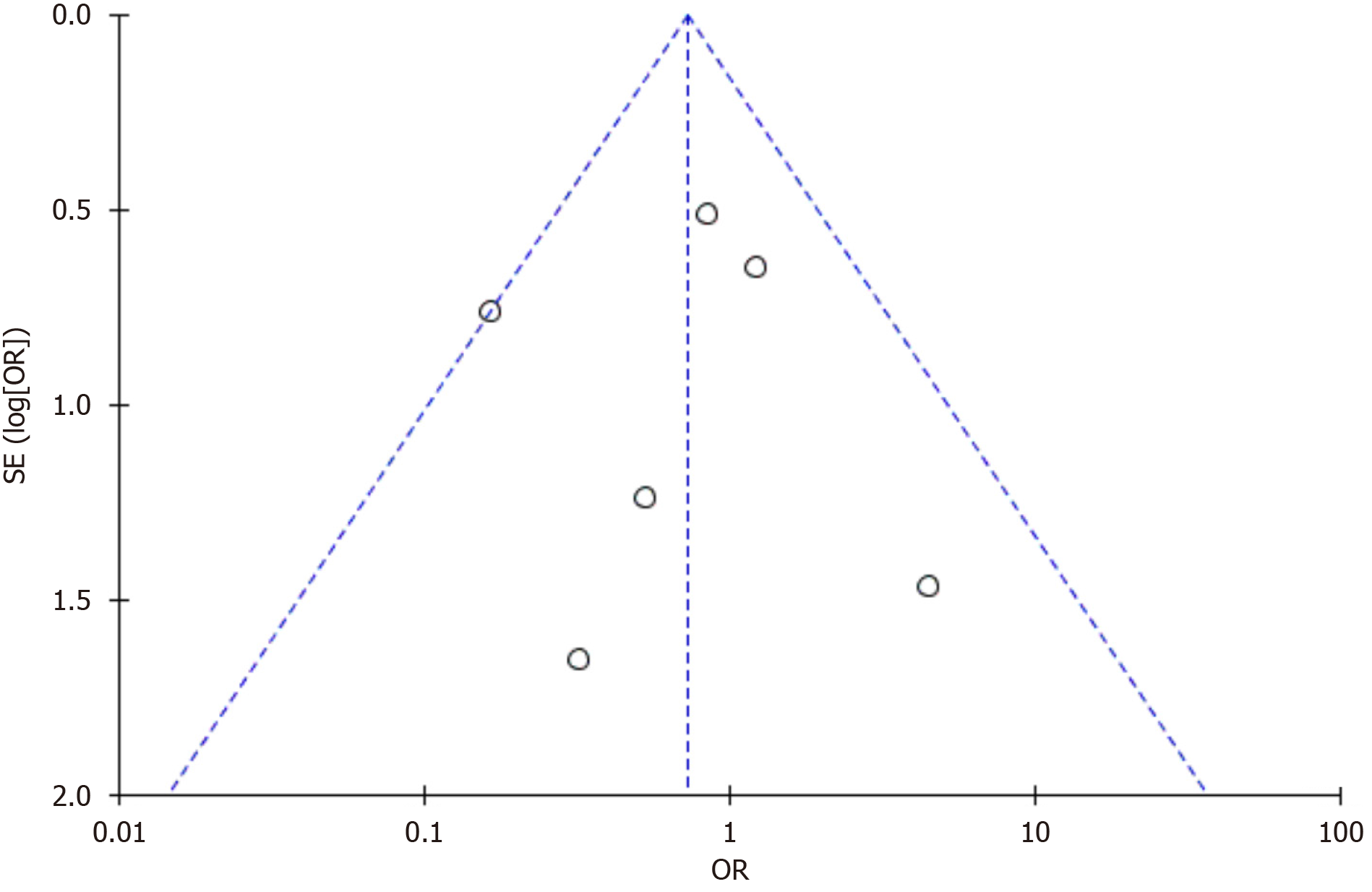
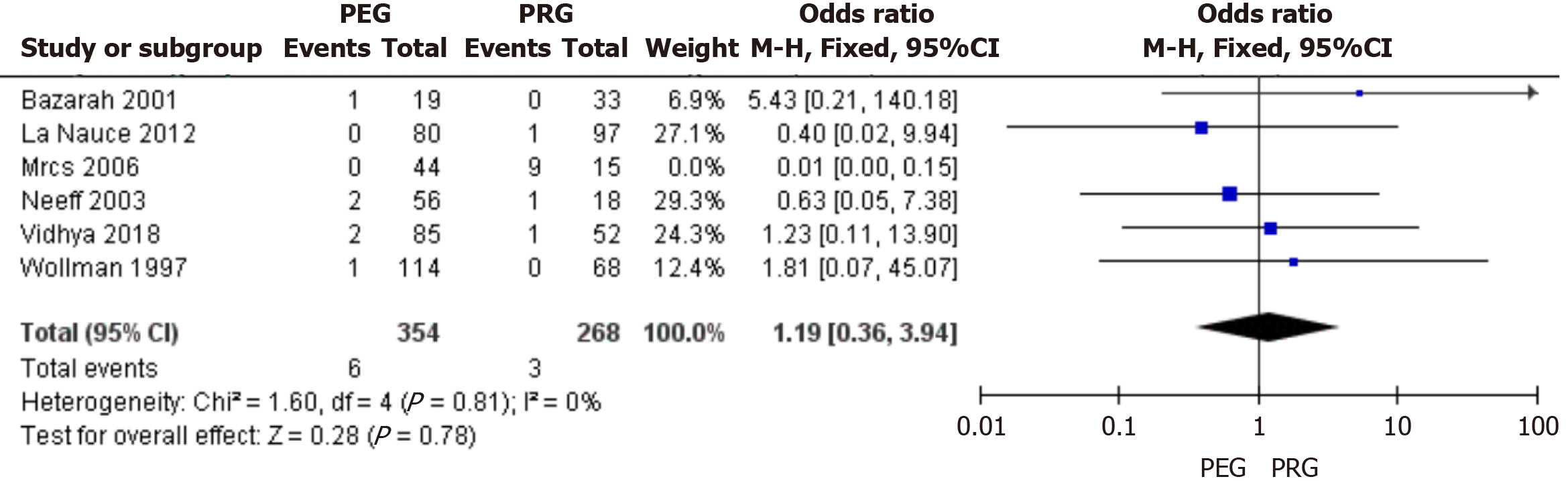
2.2.5 腹膜炎: 纳入6篇文献对PEG和PRG术后腹膜炎发生率做了比较[8-10,13,17,20], 各研究结果间异质性较低(I2 = 0%), 采用固定效应模型进行合并分析. 结果显示: 经皮内镜胃造瘘术相对于X线或CT引导下经皮穿刺胃造瘘术在术后腹膜炎发生率方面差异无显著性意义(95%CI: 0.36-3.94, P>0.05), 漏斗图显示不存在发表偏倚, 见图10和图11.
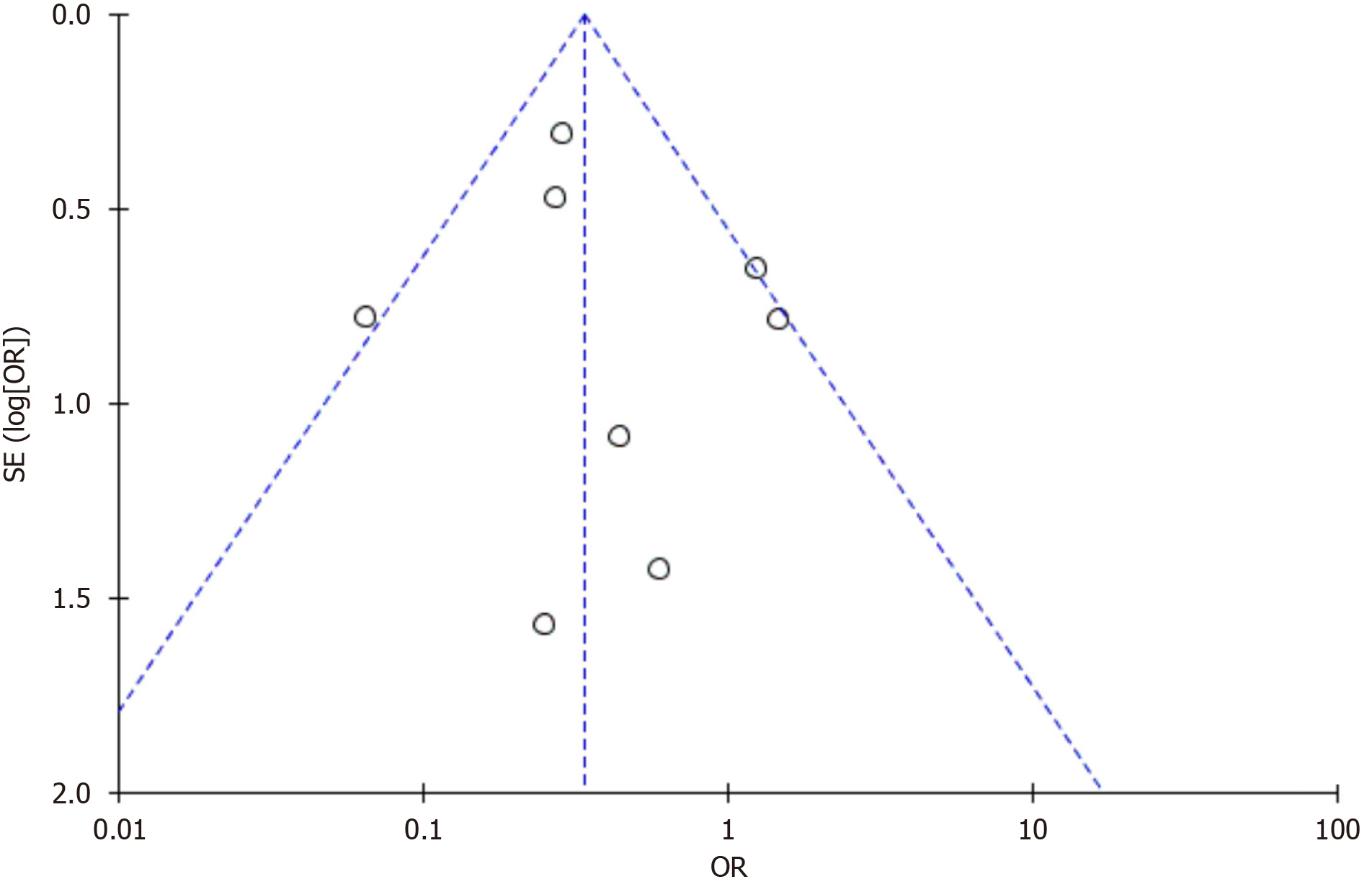
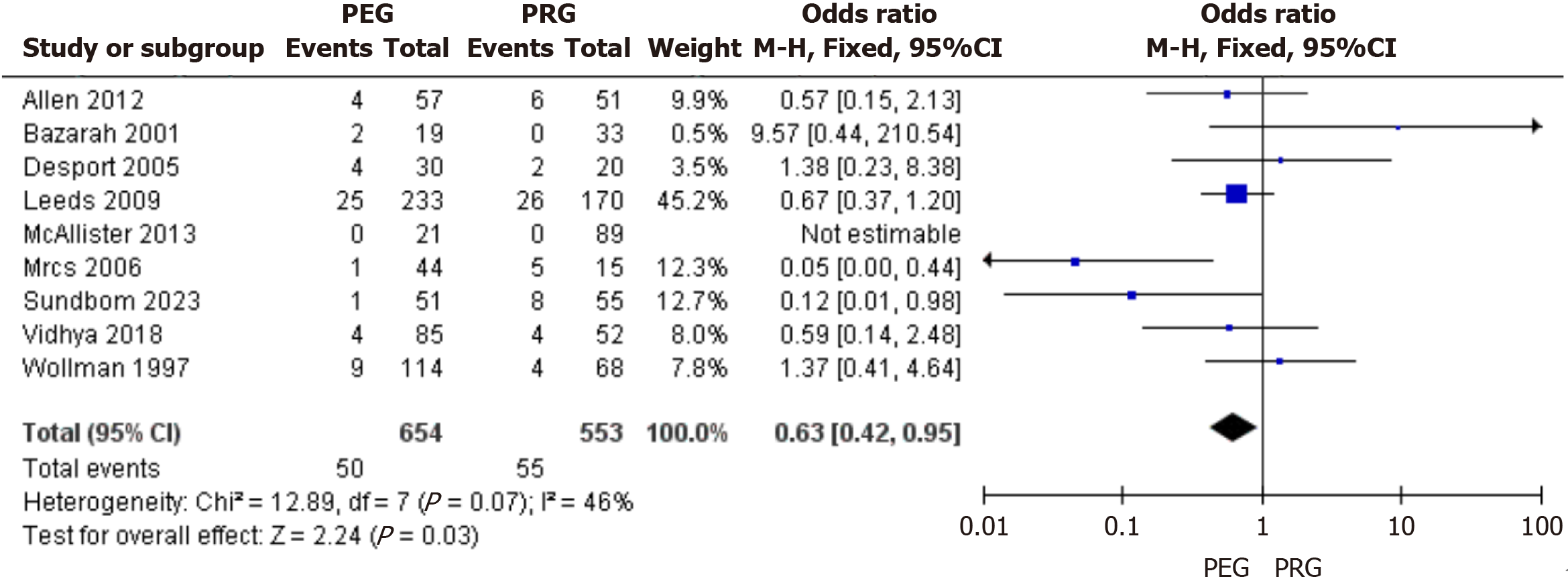
2.2.6 30 d死亡率: 纳入9篇文献对PEG和PRG术后30 d死亡率做了比较[8,9,12,13,16,18-20,22], 各研究结果间异质性较低(I2 = 46%), 采用固定效应模型进行合并分析. 结果显示: 相对于X线或CT引导下经皮穿刺胃造瘘术, 经皮内镜胃造瘘术术后30 d死亡率更低, 2组间差异有显著性意义(95%CI: 0.42-0.95, P<0.05), 漏斗图显示不存在发表偏倚, 见图12和图13.
对于各种原因(如上消化道肿瘤、心脑血管意外、颅脑神经损伤等)引起吞咽功能障碍、或长期不能经口进食的患者, 营养支持是治疗的重要手段. 临床常见的营养支持途径包括鼻胃管置入和胃造瘘术. 相较于胃造瘘术, 鼻胃管置入术操作简单、手术风险低, 但长期留置鼻胃管容易引起胃潴留、吸入性肺炎, 甚至继发全身严重感染等风险[24,25], 难以广泛应用于长期营养支持治疗. 目前, 对于超过30 d的营养支持治疗, 首选方式是经皮内镜胃造瘘术[26]. PEG是通过胃镜介导下, 经腹部皮肤穿刺置入胃造瘘管而建立肠内营养. PEG有多种方法, 如拉出法(Pull-PEG)、推入法(Push-PEG)、插入法(Introducer-PEG). 我国目前普遍采用的是由Gauderer于1980年报道的Pull法[27]. 这一术式须经上消化道置入胃镜和造瘘管, 因此不适用于开口受限、上消化道狭窄或梗阻者, 同时也有可能造成口咽部肿瘤或细菌的播散种植. Introducer法因无需经上消化道置入造瘘管, 故可代替Pull法, 用来解决部分上消化道狭窄或梗阻者. 有学者对比了几种PEG方法的临床效果, 但研究结果存在差异[28-30]. 随着微创影像技术的迅速发展, X线或CT引导下经皮穿刺胃造瘘术由于具备成功率高、手术时间短、并发症少等优点, 越来越得到临床医师的重视[31,32]. PRG技术方法选择包括X线透视引导、DSA透视联合C-arm CT引导、全程CT引导[33]. X线透视引导是较为传统的技术方法, 主要优点是设备要求低, 辐射剂量少, 容易推广普及, 但存在容易误伤左肝或结肠等严重并发症. DSA透视联合C-arm CT引导避免了上述方法的不足, 使其临床应用更加安全. 全程CT扫描对于精确定位和评估胃与周围脏器的解剖关系作用更好, 对于残胃造瘘患者应首先考虑, 缺点是增加了患者手术期间的辐射剂[34]. 胃造瘘术通常被认为是一种安全的手术, 但在不同的受试群体中, 其并发症的发生率存在很大差异. PEG和PRG的并发症按照介入放射学的分类可以分为轻微并发症和严重并发症[35]. 轻微并发症主要包括导管堵塞或脱落、造瘘口周围感染、渗漏、气腹等; 严重并发症包括腹膜炎、结肠穿孔、出血、死亡等.
近年来, 有不少临床作者发表了关于PEG和PRG对比的临床研究及荟萃分析, 讨论比较二者的疗效差异. 但许多研究存在着诸如样本量较小, 研究质量参差不齐的缺陷, 故此次笔者以Meta分析的方法, 增加样本研究量, 剔除低质量文献, 以期得出客观可靠的结论, 为肠内营养支持治疗提供一定的参考.
本次研究共纳入16项关于PEG和PRG对比的临床研究. Meta分析结果显示: PRG置管成功率更高, 差异具有统计学意义, 这与Kohli等[36]的Meta分析结果相一致. 相较于PEG, PRG整个操作过程具有实时可视性, 可清晰显示胃与周围肠管、腹壁的解剖关系, 视野更广, 可操作性更强, 同时不需经口操作, 对咽喉部及食管明显狭窄的患者更具优势. 在瘘管堵塞或狭窄发生率、术后30 d死亡率方面, PEG组低于PRG组, 差异具有统计学意义. 最新一项Meta分析[37]结果显示: PEG组的导管相关并发症是2.7%, 30 d全因死亡率较PRG组降低40%, 与本研究结果相近. 造瘘管堵塞或狭窄最常见的原因是半流有渣食物、片剂药物碾碎不够充分、药物食物配伍不当形成凝块堵塞管道等[38], 有学者认为采用20F的胃造瘘管可有效避免发生阻塞[39]. PRG组30 d全因死亡率较高的原因可能与X线/CT引导穿刺充气时存在一定的滞后性, 操作医师经验不丰富, 诱发胃肠道出血、胃肠穿孔等不良事件[40]. PEG组在瘘口感染率、疼痛发生率方面低于PRG组, 但差异无统计学意义.
本次研究尚存在以下不足: (1)纳入研究多为单中心病例对照研究, 样本量较少, 具有潜在的发表性偏移; (2)受试者基础疾病存在差异, 可能影响部分数据结果; (3)各研究术者操作水平不一, 可能导致相关研究指标异质性偏高; (4)本研究尚未对其他结局指标(例如出血、结肠穿孔等)进行Meta分析, 可能影响最终结果的研判.
综上所述, PEG优势是可以同时进行内镜下检查和治疗, 置入管径相对较粗, 能够注入匀浆流质, 不易堵塞造瘘管, 为患者提供全面均衡的营养摄入, 从而降低30 d全因死亡率, 改善患者的预后, 是一种适合长期提供肠内营养的有效方法; 而PRG不需静脉麻醉、不需经口操作, 理论上能够提高造瘘的成功率与安全性, 同时也降低了口咽部肿瘤或细菌播散种植的可能性, 因此特别适合头颈部或食管上段肿瘤致严重管腔狭窄的患者. 但在临床实际操作中, 临床医师应根据患者具体病情, 结合医院实际情况, 合理选择胃造瘘术方法; 同时也建议开展多中心、大样本的前瞻性临床队列研究, 以得出证据等级更高的研究结论.
对各种原因引起的吞咽功能障碍或长期不能经口进食的患者, 肠内营养支持治疗能够维持患者的营养水平, 改善生活质量. 但目前就肠内营养的应用时机、方式选择、适宜人群尚未形成统一的临床实践指南, 因此, 亟需研究深入探讨, 以建立基于循证医学证据的胃造瘘术式选择.
旨在评估经皮内镜胃造瘘术(percutaneous endoscopic gastrostomy, PEG)与X线或CT引导下经皮穿刺胃造瘘术(percutaneous radiologic gastrostomy, PRG)的临床效果.
通过Meta分析对PEG与PRG的病例对照研究进行系统评价, 为指导个体化肠内营养干预策略提供循证医学依据.
对国内外主流数据库进行文献检索, 根据文献纳入及排除标准纳入文献, 对符合纳入的研究进行Meta分析.
共纳入16篇研究, 总计2770例患者, PEG术后瘘管堵塞或狭窄发生率、术后30 d死亡率低于PRG, PRG置管成功率高于PEG.
PRG的成功率与安全性更高, 特别适合头颈部或食管上段肿瘤致严重管腔狭窄的患者, 而PEG可以同时进行内镜下检查和治疗, 不易堵塞造瘘管, 能降低30 d全因死亡率, 改善患者的预后.
希望未来能开展更大样本的真实世界临床研究, 优化评判标准, 为制定精准的胃造瘘术式选择提供依据.
学科分类: 胃肠病学和肝病学
手稿来源地: 浙江省
同行评议报告学术质量分类
A级 (优秀): 0
B级 (非常好): B
C级 (良好): C, C
D级 (一般): 0
E级 (差): 0
科学编辑: 刘继红 制作编辑:郑晓梅
| 1. | Liu H, Jiao J, Zhu M, Wen X, Jin J, Wang H, Lv D, Zhao S, Sun X, Wu X, Xu T. Nutritional Status According to the Short-Form Mini Nutritional Assessment (MNA-SF) and Clinical Characteristics as Predictors of Length of Stay, Mortality, and Readmissions Among Older Inpatients in China: A National Study. Front Nutr. 2022;9:815578. [PubMed] [DOI] |
| 2. | McClave SA, Taylor BE, Martindale RG, Warren MM, Johnson DR, Braunschweig C, McCarthy MS, Davanos E, Rice TW, Cresci GA, Gervasio JM, Sacks GS, Roberts PR, Compher C; Society of Critical Care Medicine; American Society for Parenteral and Enteral Nutrition. Guidelines for the Provision and Assessment of Nutrition Support Therapy in the Adult Critically Ill Patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40:159-211. [PubMed] [DOI] |
| 3. | Bankhead R, Boullata J, Brantley S, Corkins M, Guenter P, Krenitsky J, Lyman B, Metheny NA, Mueller C, Robbins S, Wessel J; A. S.P.E.N. Board of Directors. Enteral nutrition practice recommendations. JPEN J Parenter Enteral Nutr. 2009;33:122-167. [PubMed] [DOI] |
| 4. | Luo QF, Zhang XF, Jin HB, Lv W, Yang JF, Shen HZ, Zheng LY. Comparative study of two small intestinal nutrient tubes by percutaneous endoscopic gastrostomy. Zhongguo Nei Jing Zazhi. 2022;28:20-23. |
| 5. | Kohli DR, Kennedy KF, Desai M, Sharma P. Comparative Safety of Endoscopic vs Radiological Gastrostomy Tube Placement: Outcomes From a Large, Nationwide Veterans Affairs Database. Am J Gastroenterol. 2021;116:2367-2373. [PubMed] [DOI] |
| 6. | Itkin M, DeLegge MH, Fang JC, McClave SA, Kundu S, Janne d'Othee B, Martinez-Salazar GM, Sacks D, Swan TL, Towbin RB, Walker TG, Wojak JC, Zuckerman DA, Cardella JF; Interventional Radiology and American Gastroenterological Association; American Gastroenterological Association Institute; Canadian Interventional Radiological Association; Cardiovascular and Interventional Radiological Society of Europe. Multidisciplinary practical guidelines for gastrointestinal access for enteral nutrition and decompression from the Society of Interventional Radiology and American Gastroenterological Association (AGA) Institute, with endorsement by Canadian Interventional Radiological Association (CIRA) and Cardiovascular and Interventional Radiological Society of Europe (CIRSE). J Vasc Interv Radiol. 2011;22:1089-1106. [PubMed] [DOI] |
| 7. | Blondet A, Lebigot J, Nicolas G, Boursier J, Person B, Laccoureye L, Aubé C. Radiologic versus endoscopic placement of percutaneous gastrostomy in amyotrophic lateral sclerosis: multivariate analysis of tolerance, efficacy, and survival. J. Vasc Interv Radiol. 2010;21:527-533. [PubMed] [DOI] |
| 8. | Wollman B, D'Agostino HB. Percutaneous radiologic and endoscopic gastrostomy: a 3-year institutional analysis of procedure performance. AJR Am J Roentgenol. 1997;169:1551-1553. [PubMed] [DOI] |
| 9. | Bazarah SM, Al-Rawas M, Akbar H, Qari Y. Percutaneous gastrostomy and gastrojejunostomy: radiological and endoscopic approach. Ann Saudi Med. 2002;22:38-42. [PubMed] [DOI] |
| 10. | Neeff M, Crowder VL, McIvor NP, Chaplin JM, Morton RP. Comparison of the use of endoscopic and radiologic gastrostomy in a single head and neck cancer unit. ANZ J Surg. 2003;73:590-593. [PubMed] [DOI] |
| 11. | Silas AM, Pearce LF, Lestina LS, Grove MR, Tosteson A, Manganiello WD, Bettmann MA, Gordon SR. Percutaneous radiologic gastrostomy versus percutaneous endoscopic gastrostomy: a comparison of indications, complications and outcomes in 370 patients. Eur J Radiol. 2005;56:84-90. [PubMed] [DOI] |
| 12. | Desport JC, Mabrouk T, Bouillet P, Perna A, Preux PM, Couratier P. Complications and survival following radiologically and endoscopically-guided gastrostomy in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Other Motor Neuron Disord. 2005;6:88-93. [PubMed] [DOI] |
| 13. | Eze N, Jefford JM, Wolf D, Williamson P, Neild P. PEG and RIG tube feeding in Head and Neck patients: a retrospective review of complications and outcome. J Eval Clin Pract. 2007;13:817-819. [PubMed] [DOI] |
| 14. | MacLean AA, Alvarez NR, Davies JD, Lopez PP, Pizano LR. Complications of percutaneous endoscopic and fluoroscopic gastrostomy tube insertion procedures in 378 patients. Gastroenterol Nurs. 2007;30:337-341. [PubMed] [DOI] |
| 15. | Galaski A, Peng WW, Ellis M, Darling P, Common A, Tucker E. Gastrostomy tube placement by radiological versus endoscopic methods in an acute care setting: a retrospective review of frequency, indications, complications and outcomes. Can J Gastroenterol. 2009;23:109-114. [PubMed] [DOI] |
| 16. | Leeds JS, McAlindon ME, Grant J, Robson HE, Lee FK, Sanders DS. Survival analysis after gastrostomy: a single-centre, observational study comparing radiological and endoscopic insertion. Eur J Gastroenterol. Hepatol. 2010;22:591-596. [PubMed] [DOI] |
| 17. | La Nauze RJ, Collins K, Lyon S, Bailey M, Kemp W, Nyulasi I, Roberts SK. Outcomes of percutaneous endoscopic gastrostomy versus radiologically inserted gastrostomy tube insertion at a tertiary hospital. ESPEN J. 2012;7:144-148. [DOI] |
| 18. | Allen JA, Chen R, Ajroud-Driss S, Sufit RL, Heller S, Siddique T, Wolfe L. Gastrostomy tube placement by endoscopy versus radiologic methods in patients with ALS: a retrospective study of complications and outcome. Amyotroph Lateral Scler Frontotemporal Degener. 2013;14:308-314. [PubMed] [DOI] |
| 19. | McAllister P, MacIver C, Wales C, McMahon J, Devine JC, McHattie G, Makubate B. Gastrostomy insertion in head and neck cancer patients: a 3 year review of insertion method and complication rates. Br J Oral Maxillofac Surg. 2013;51:714-718. [PubMed] [DOI] |
| 20. | Vidhya C, Phoebe D, Dhina C, Jayne S, Robert F. Percutaneous endoscopic gastrostomy (PEG) versus radiologically inserted gastrostomy (RIG): A comparison of outcomes at an Australian teaching hospital. Clin Nutr ESPEN. 2018;23:136-140. [PubMed] [DOI] |
| 21. | Park SK, Kim JY, Koh SJ, Lee YJ, Jang HJ, Park SJ; Small Intestine and Nutrition Research Group of the Korean Association for the Study of Intestinal Diseases (KASID). Complications of percutaneous endoscopic and radiologic gastrostomy tube insertion: a KASID (Korean Association for the Study of Intestinal Diseases) study. Surg Endosc. 2019;33:750-756. [PubMed] [DOI] |
| 22. | Sundbom M, Cabrera E, Nyman R, Barbier CE, Johnson U, Ljungdahl M. A randomized trial comparing percutaneous endoscopic gastrostomy (PEG) and radiologically inserted percutaneous gastrostomy (RIG). Scand J Surg. 2023;112:69-76. [PubMed] [DOI] |
| 23. | Du KP, He YC, Lou XF, Wang M, Li YD, Gao MY, Gao F, Zhou ZG. A comparative study on the success rate and safety between computed tomography-guided gastrostomy and endoscopic gastrostomy. Zhonghua Xiaohua Zazhi. 2023;43:102-106. |
| 24. | Lu J, Yu Q, Shen Y, Zhuang ZW. Application of percutaneous endoscopic gastrostomy in elderly patients with high risk of aspiration. Jiangsu Yiyao. 2017;43:1087-1089. |
| 25. | Dietrich CG, Schoppmeyer K. Percutaneous endoscopic gastrostomy - Too often? Too late? Who are the right patients for gastrostomy? World J Gastroenterol. 2020;26:2464-2471. [PubMed] [DOI] |
| 26. | Chang WK, Lin KT, Tsai CL, Chung CH, Chien WC, Lin CS. Trends regarding percutaneous endoscopic gastrostomy: A nationwide population-based study from 1997 to 2010. Medicine (Baltimore). 2016;95:e3910. [PubMed] [DOI] |
| 27. | 曾 丽婷, 吴 嘉骏, 范 晶娴, 王 伟, 杨 天页, 王 繁麟, 徐 兵, 葛 奎. 拉出法与插入法经皮内镜下胃造瘘术在口腔颌面部恶性肿瘤患者中的应用效果比较. 中国口腔颌面外科杂志. 2022;20:401-404. [DOI] |
| 28. | Lee SW, Lee JH, Cho H, Ha Y, Lim H, Ahn JY, Choi KS, Kim DH, Choi KD, Song HJ, Lee GH, Jung HY, Kim JH. Comparison of clinical outcomes associated with pull-type and introducer-type percutaneous endoscopic gastrostomies. Clin Endosc. 2014;47:530-537. [PubMed] [DOI] |
| 29. | Van Dyck E, Macken EJ, Roth B, Pelckmans PA, Moreels TG. Safety of pull-type and introducer percutaneous endoscopic gastrostomy tubes in oncology patients: a retrospective analysis. BMC Gastroenterol. 2011;11:23. [PubMed] [DOI] |
| 30. | Chang A, Watcharamon C, Rattanasupa A, Thongsonkleeb K, Chowdok B, Khaimook A, Ovartlarnporn B, Prachayakul V. Comparison of Clinical Outcomes Between Surgical Gastrostomy and Percutaneous Endoscopic Gastrostomy with Introducer Technique in Patients with Upper Aerodigestive Malignancies: A Single-Center Analysis. World J Surg. 2020;44:3070-3076. [PubMed] [DOI] |
| 35. | Covarrubias DA, O'Connor OJ, McDermott S, Arellano RS. Radiologic percutaneous gastrostomy: review of potential complications and approach to managing the unexpected outcome. AJR Am J Roentgenol. 2013;200:921-931. [PubMed] [DOI] |
| 36. | Kohli DR, Radadiya DK, Patel H, Sharma P, Desai M. Comparative outcomes of endoscopic and radiological gastrostomy tube placement: a systematic review and meta-analysis with GRADE analysis. Ann Gastroenterol. 2022;35:592-602. [PubMed] [DOI] |
| 37. | Radadiya D, Desai M, Patel HK, Khurana S, Melquist SJ, Chandrasekar VT, Devani K, Sharma P, Kohli DR. Comparison of outcomes between percutaneous endoscopic and percutaneous radiological gastrostomy placement:a systematic review and meta-analysis. Gastrointest Endosc. 2022;95:471-472. [DOI] |
| 38. | Hoang PT, Menias CO, Niemeyer MM. Percutaneous Gastrostomy Tube Placement: Recognizing When Things Go Wrong. Semin Intervent Radiol. 2019;36:264-274. [PubMed] [DOI] |
| 39. | Trerotola SO, Shah H, Johnson MS, Namyslowski J, Moresco K, Patel NH. Single-step dilation for large-bore percutaneous gastrostomy and gastrojejunostomy. J Vasc Interv Radiol. 1998;9:579-582. [PubMed] [DOI] |
| 40. | 吴 嘉骏, 王 繁麟, 葛 卫文, 范 晶娴, 曾 丽婷, 王 齐, 谢 挺, 张 霖, 徐 兵, 葛 奎. Introduce法经皮胃造瘘术在上消化道狭窄肿瘤患者中的应用. 中国口腔颌面外科杂志. 2020;18:60-63. |