Published online Nov 21, 2025. doi: 10.3748/wjg.v31.i43.111906
Revised: September 3, 2025
Accepted: October 20, 2025
Published online: November 21, 2025
Processing time: 131 Days and 6.4 Hours
Colonic diverticular bleeding is a significant cause of acute overt lower gastr
We present the case of a 70-year-old male with acute painless hematochezia. Colonoscopy showed active bleeding originating from a diverticulum, and the EyeMax direct visualization system was used in the treatment of the colonic diverticular bleeding. No further evidence of bleeding was observed at the end of the procedure. The patient was discharged from hospital on the seventh day.
The EyeMax system proved advantageous in localizing the bleeding diverticulum, thereby facilitating successful hemostatic measures.
Core Tip: Colonic diverticular bleeding is a significant cause of acute overt lower gastr
- Citation: Han TJ, Li JS. Utilizing the EyeMax direct visualization system for the treatment of colonic diverticular bleeding: A case report. World J Gastroenterol 2025; 31(43): 111906
- URL: https://www.wjgnet.com/1007-9327/full/v31/i43/111906.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i43.111906
Colonic diverticular bleeding (CDH) is a notable clinical condition characterized by the rupture of blood vessels in the diverticulum, leading to gastrointestinal bleeding[1]. The etiology of CDH is associated with various risk factors, including hypertension, diabetes, heart disease, and obesity[2]. Moreover, lifestyle factors such as smoking and alcohol consumption have been implicated in increasing the risk of diverticular bleeding, Additionally, using two nonsteroidal anti-inflammatory drugs or two anti-platelet drugs raises the risk of CDH in patients over 65 years old[3]. CDH can lead to life-threatening bleeding episodes[4]. The condition is particularly prevalent among older adults, with studies indicating that the incidence of diverticular disease increases with age[3]. The clinical presentation often includes painless hematochezia, which can be alarming for patients and necessitates prompt medical intervention. Colonoscopy plays a crucial role in both the diagnosis and management of diverticular bleeding, allowing for direct visualization of the colon and potential therapeutic interventions[5].
Given its propensity to spontaneously resolve in some cases, coupled with a high risk of rebleeding, it is imperative to promptly identify and address the bleeding diverticulum, thereby facilitating effective hemostasis[6]. In this case report, we present a 70-year-old male who experienced acute painless hematochezia due to diverticular bleeding. This case is noteworthy as it highlights the successful application of the EyeMax direct visualization system in the treatment of CDH, a relatively rare intervention that may serve as a valuable option in similar clinical scenarios. EyeMax is a digital single-operator cholangioscope (EyeMax, 3 mm; Micro-Tech, Nanjing, China). The use of EyeMax allowed for precise lo
A 70-year-old man presented with acute painless hematochezia that began nine hours prior to his arrival at the hospital.
Symptoms started nine hours before presentation with acute painless hematochezia.
The patient had a 20-year history of hypertension and coronary artery disease, and had a stent placed 7 years ago when having a heart attack. The patient was treated with oral anti-platelet medication and nifedipine daily. He did not have a history of other diseases and no food or drug allergies.
The patient had no history of substance abuse, consanguineous marriage with parental relatives, or familial genetic disorders.
On physical examination, the vital signs were as follows: Body temperature, 36 °C; blood pressure, 129/88 mmHg; heart rate, 80 bpm; respiratory rate, 22 breaths/minute.
On the day of admission, laboratory tests revealed several abnormalities: Stool tests showed the presence of fat droplets, red blood cells (++) (normal: -); routine blood tests showed a hemoglobin level of 92 g/L (normal: 130-175 g/L), blood biochemistry indicated decreased levels of total protein (57.9 g/L; normal: 60-80 g/L) and albumin (33.9 g/L; normal: 40-55 g/L). Other parameters, including liver and kidney function, pancreatic enzymes, blood glucose, electrolytes, and thyroid function, were within normal ranges.
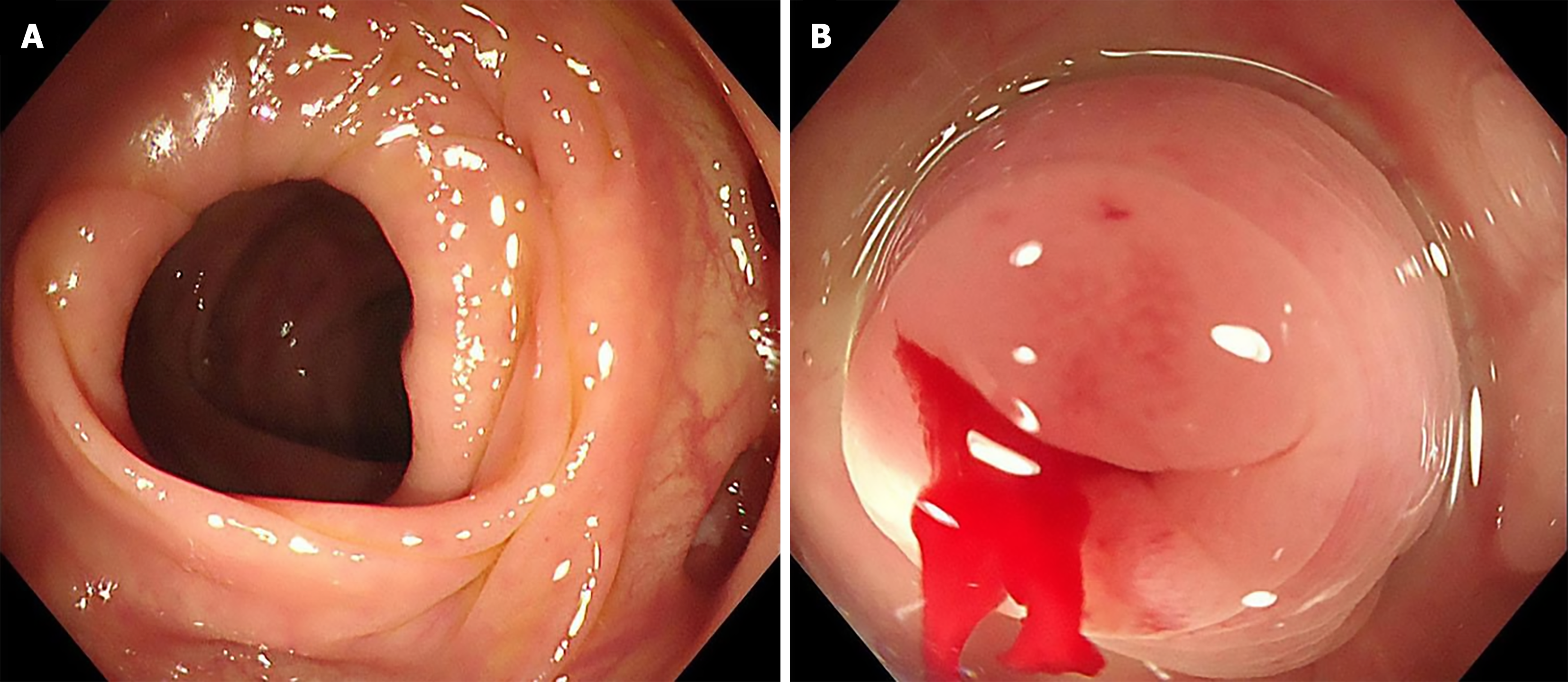
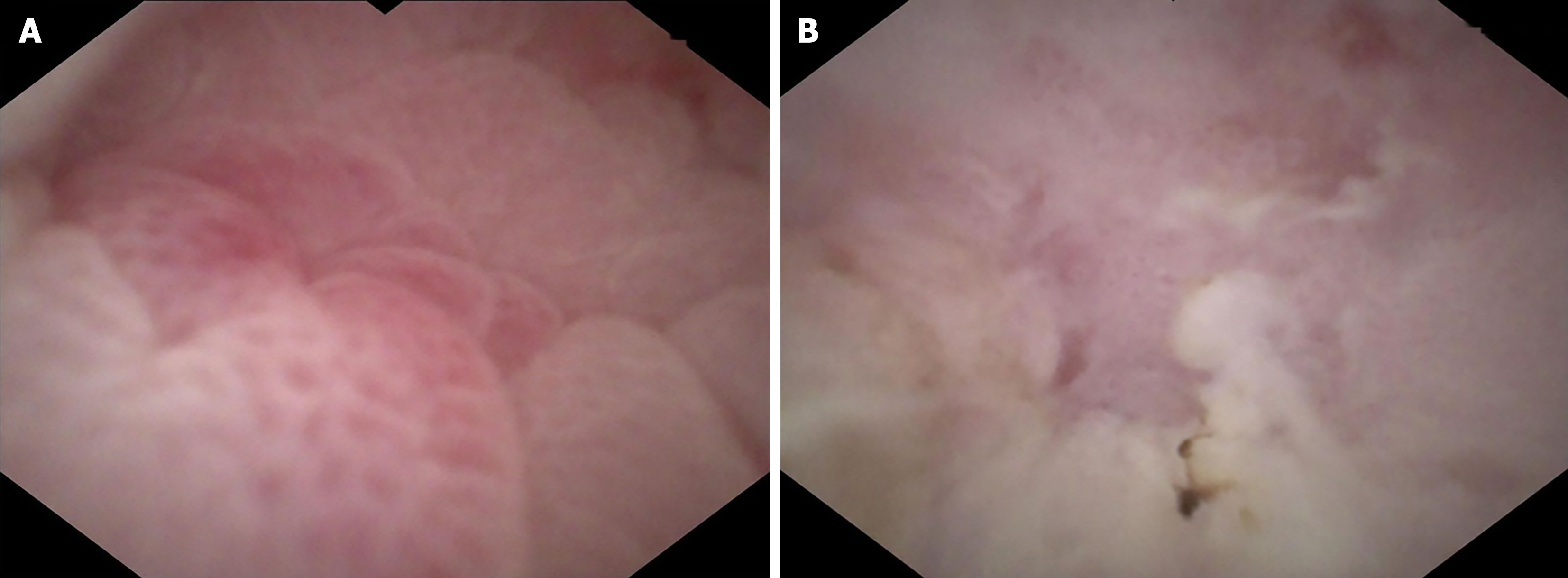
Initial colonoscopy conducted within 24 hours revealed severe diverticulosis in the colon, but the cause of bleeding and active hemorrhage remained undetermined (Figure 1A). On the third day, the patient experienced recurrent bleeding, prompting a repeat colonoscopy. This procedure confirmed active bleeding originating from a diverticulum located 50cm from the anal margin (Figure 1B). CDH can stop spontaneously, an attempt to use an endoscopic cap to invert the diverticulum was unsuccessful, and we were unable to determine the specific location of the bleeding diverticulum. Therefore, the EyeMax direct visualization system (9F) was employed, which revealed bleeding from a vessel in the colonic diverticulum neck (Figure 2A).
CDH.
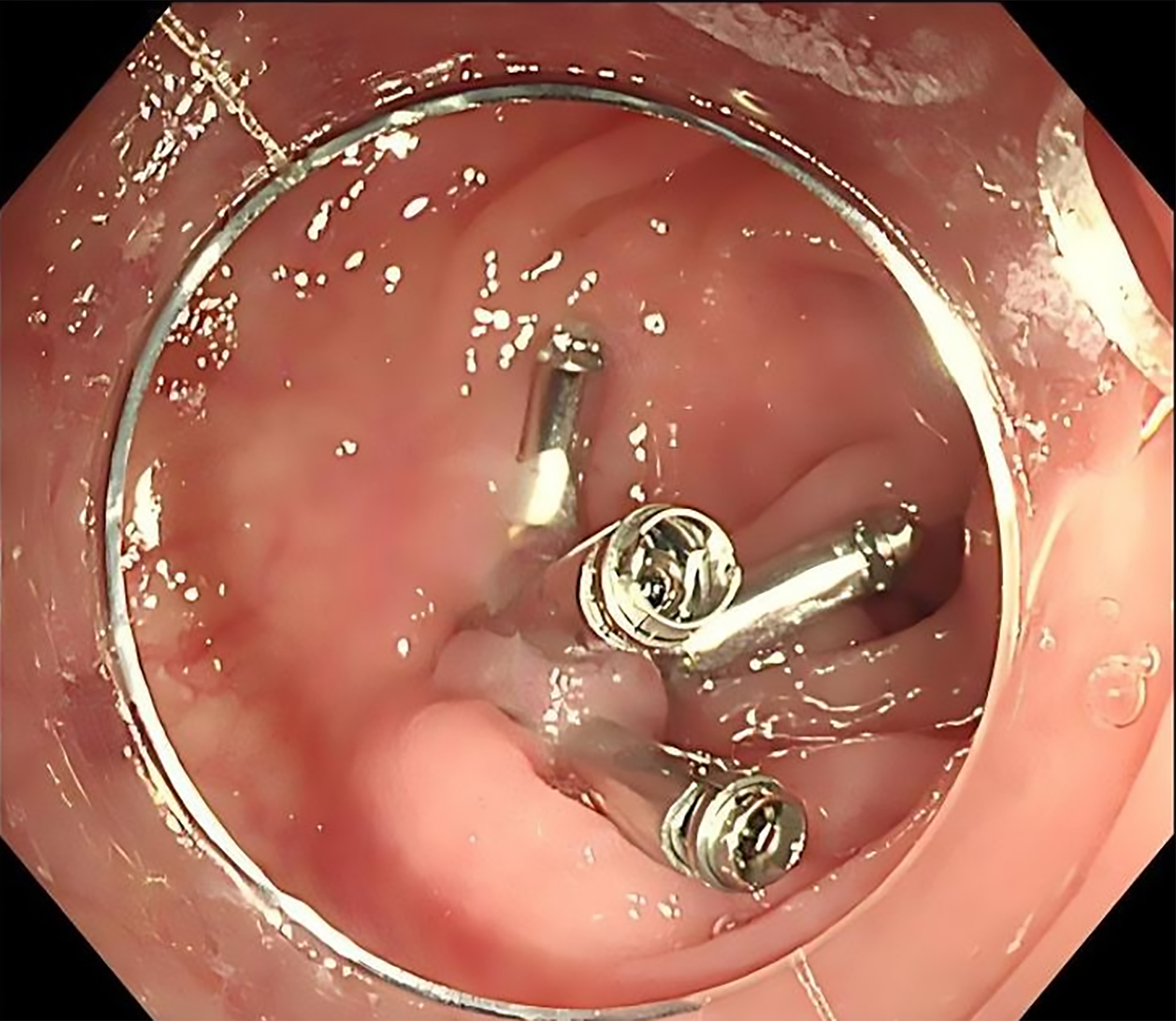
Multipolar electrocoagulation was subsequently utilized to halt diverticular bleeding. The EyeMax system was used again, and contractions and coagulation of the bleeding vessel were observed (Figure 2B). Subsequent endoscopic clipping was performed to occlude the bleeding diverticulum (Figure 3).
No further evidence of bleeding was observed at the end of the procedure. Follow-up telephone consultation 3 months after hospital discharge revealed no evidence of further bleeding.
CDH is a significant cause of acute overt lower gastrointestinal hemorrhage, representing a clinical challenge due to its propensity for spontaneous resolution and the high risk of rebleeding. Findings indicate that individuals with multiple diverticulitis and those under long-term nonsteroidal anti-inflammatory drug or anti-platelet therapy are at a heightened risk of recurrence[7]. Notably, cessation of these medications significantly reduces long-term recurrence rates. Recent studies highlight that the vascular architecture within the diverticulum plays a crucial role in diverticular bleeding, as the local arteries are vulnerable to injury and rupture, often leading to bleeding that is independent of inflammation[8]. The treatment of CDH has evolved significantly, particularly with the advent of endoscopic techniques that offer less invasive options for hemostasis during surgical interventions. Various endoscopic hemostatic methods have been employed, including submarginal injection of adrenaline, thermal coagulation, spraying of hemostatic powder, closure with metal clips, endoscopic band ligation (EBL), and endoscopic detachable snare ligation[9,10]. Each of these techniques has its advantages and indications, contributing to improved outcomes in patients undergoing repair of CDH. A suitable endoscopic intervention must be chosen with careful consideration of the size and anatomical position of the diver
Moreover, previous studies have also indicated that if the bleeding is caused by blood vessels at the neck of the diverticulum, it is recommended to perform electrocautery hemostasis at the bleeding site[13]. Thus, we used multipolar electrocoagulation in conjunction with the EyeMax system which allowed effective hemostasis by directly targeting visible vessels in the diverticulum neck. The diverticulum was closed via clip placement to prevent perforation and promote healing.
The successful outcome in this patient, with no further evidence of bleeding at the conclusion of the procedure and a prompt discharge after seven days, reinforces the efficacy of utilizing advanced visualization techniques in managing diverticular bleeding. It also emphasizes the importance of a tailored approach to patient management, where timely identification and treatment of the bleeding diverticulum can significantly reduce the risk of rebleeding and associated complications.
The EyeMax direct visualization system demonstrates significant advantages in the treatment of CDH. It allows for better localization of the bleeding site and facilitates effective hemostasis, which is paramount in the management of this condition. Future clinical practice should consider incorporating such advanced technologies into routine protocols for managing diverticular bleeding to enhance patient safety and treatment outcomes. The ongoing evaluation of these techniques in larger cohorts will be essential in establishing standardized approaches to managing colonic diverticular disease effectively. In this particular case, it proved advantageous in localizing the bleeding diverticulum, enabling successful hemostasis.
| 1. | Sebastian SA, Co EL, Panthangi V, Bansal R, Narayanan V, Paudel S, Raja R, Padda I, Mohan BP. Colonic diverticular bleeding: An update on pathogenesis and management. Dis Mon. 2023;69:101543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 2. | Imaeda H, Hibi T. The Burden of Diverticular Disease and Its Complications: West versus East. Inflamm Intest Dis. 2018;3:61-68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 74] [Article Influence: 9.3] [Reference Citation Analysis (1)] |
| 3. | Tsuruoka N, Takedomi H, Sakata Y, Shimoda R. Recent Trends in Treatment for Colonic Diverticular Bleeding in Japan. Digestion. 2020;101:12-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Kirita K, Kodaka Y, Shibata Y, Ueki N, Agawa S, Yamawaki H, Niikura R, Yamamichi N, Izumi K, Hojo M, Maruyama K, Yamamoto T, Gudis K, Watanabe M, Kaise M, Iwakiri K, Futagami S. Impact of clinical characteristics of colonic diverticular bleeding in extremely elderly patients treated with direct oral anti-coagulant drugs: a retrospective multi-center study. J Clin Biochem Nutr. 2021;69:222-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 5. | Tomizawa Y, Strate LL. Colonoscopy for colonic diverticular bleeding: more evidence for finding and treating stigmata of recent hemorrhage. Gastrointest Endosc. 2022;95:1223-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 6. | Nagata N, Ishii N, Manabe N, Tomizawa K, Urita Y, Funabiki T, Fujimori S, Kaise M. Guidelines for Colonic Diverticular Bleeding and Colonic Diverticulitis: Japan Gastroenterological Association. Digestion. 2019;99 Suppl 1:1-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 139] [Article Influence: 19.9] [Reference Citation Analysis (0)] |
| 7. | Nagata N, Niikura R, Aoki T, Shimbo T, Sekine K, Okubo H, Watanabe K, Sakurai T, Yokoi C, Akiyama J, Yanase M, Mizokami M, Uemura N. Impact of discontinuing non-steroidal antiinflammatory drugs on long-term recurrence in colonic diverticular bleeding. World J Gastroenterol. 2015;21:1292-1298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 23] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Wedel T, Barrenschee M, Lange C, Cossais F, Böttner M. Morphologic Basis for Developing Diverticular Disease, Diverticulitis, and Diverticular Bleeding. Viszeralmedizin. 2015;31:76-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Hayasaka J, Kikuchi D, Odagiri H, Nomura K, Ochiai Y, Okamura T, Suzuki Y, Mitsunaga Y, Dan N, Tanaka M, Yamashita S, Matsui A, Hoteya S. Effectiveness of Clipping for Definitive Colonic Diverticular Bleeding in Preventing Early Recurrent Bleeding. Intern Med. 2022;61:451-460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Kawano K, Takenaka M, Kawano R, Kagoshige D, Kawase Y, Moriguchi T, Tanabe H, Katoh T, Nishi K, Kudo M. Efficacy of Over-The-Scope Clip Method as a Novel Hemostatic Therapy for Colonic Diverticular Bleeding. J Clin Med. 2021;10:2891. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 11. | Narimatsu K, Ishii N, Yamada A, Aoki T, Kobayashi K, Yamauchi A, Omori J, Ikeya T, Aoyama T, Tominaga N, Sato Y, Kishino T, Sawada T, Murata M, Takao A, Mizukami K, Kinjo K, Fujimori S, Uotani T, Fujita M, Sato H, Suzuki S, Narasaka T, Hayasaka J, Funabiki T, Kinjo Y, Mizuki A, Kiyotoki S, Mikami T, Gushima R, Fujii H, Fuyuno Y, Hikichi T, Toya Y, Manabe N, Nagaike K, Kinjo T, Sumida Y, Funakoshi S, Kobayashi K, Matsuhashi T, Komaki Y, Hokari R, Kaise M, Nagata N. Impact of long-term trends on outcomes in the management of colonic diverticular bleeding: mediation analyses in a large multicenter study. J Gastroenterol. 2025;60:174-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 12. | Zhang W, Hou SL, Tian J, Zhang LC. The combination of eyeMax direct visualization system, EUS and ERCP for the precise treatment of intraductal papillary mucinous neoplasm. Rev Esp Enferm Dig. 2023;115:740-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Jensen DM. Endoscopic Diagnosis and Treatment of Colonic Diverticular Bleeding. Gastrointest Endosc Clin N Am. 2024;34:345-361. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/