Published online Nov 7, 2025. doi: 10.3748/wjg.v31.i41.110398
Revised: August 5, 2025
Accepted: September 28, 2025
Published online: November 7, 2025
Processing time: 154 Days and 2.1 Hours
Pancreatic tuberculosis (TB) is a rare clinical condition that is frequently misdiagnosed. A definitive diagnosis is often established through surgical biopsy.
We report a previously healthy 21-year-old male who presented with epigastric pain and fever. Initially diagnosed with a pancreatic abscess and duodenal bulb perforation, the patient declined surgical intervention and was subsequently re
Pancreatic TB should be included in differential diagnosis; prompt endoscopic ul
Core Tip: Pancreatic tuberculosis (TB) is a rare entity that is frequently misdiagnosed, often leading to unnecessary surgery. We report the case of a healthy 21-year-old patient initially suspected of having a pancreatic abscess, who was ultimately diagnosed with pancreatic TB via endoscopic ultrasound-guided fine-needle aspiration. The patient achieved full recovery after anti-TB treatment. This case highlights the importance of considering pancreatic TB in differential diagnosis to avoid invasive procedures, especially in young patients from TB-endemic areas.
- Citation: Nima CL, Wang HG, Zhou Q. Pancreatic tuberculosis: A case report and review of literature. World J Gastroenterol 2025; 31(41): 110398
- URL: https://www.wjgnet.com/1007-9327/full/v31/i41/110398.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i41.110398
Pancreatic tuberculosis (TB) is a rare form of extrapulmonary TB, accounting for approximately 0.2%-2% of all TB cases worldwide[1,2]. The relative resistance of the pancreas to mycobacterial infection contributes to the rarity of this condition, which often poses diagnostic challenges[3]. Patients typically present with nonspecific symptoms, including epigastric pain, weight loss, and fever, which overlap with many gastrointestinal disorders. As a result, pancreatic TB is often misdiagnosed as pancreatitis, a pancreatic tumor, or a pancreatic abscess. Imaging studies, such as conventional computed tomography (CT) or magnetic resonance imaging, are generally unreliable in distinguishing pancreatic TB from other pancreatic masses, further complicating diagnosis. This report describes a case initially suspected to be a pancreatic abscess with duodenal bulb perforation, but ultimately diagnosed as primary pancreatic TB through endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA). This report highlights the diagnostic complexity of pancreatic TB and offers practical insights into its clinical management, supported by a representative case and a systematic review of the literature.
A 21-year-old male presented with a 1-month history of recurrent epigastric pain, abdominal distension, and low-grade fever, with a maximum recorded temperature of 37.4 °C.
Initial evaluation at a local hospital suggested a pancreatic abscess. The patient was treated with antibiotics and gastroprotective therapy, but his symptoms persisted. Although a Whipple procedure (pancreaticoduodenectomy) was considered, the patient and his family chose to seek further evaluation at our institution.
The patient had no history of TB, hepatitis, smoking, or alcohol use.
The patient had no chronic or familial inherited diseases.
Upon examination, his vital signs were stable. Mild tenderness was noted in the left upper quadrant, with no palpable hepatosplenomegaly.
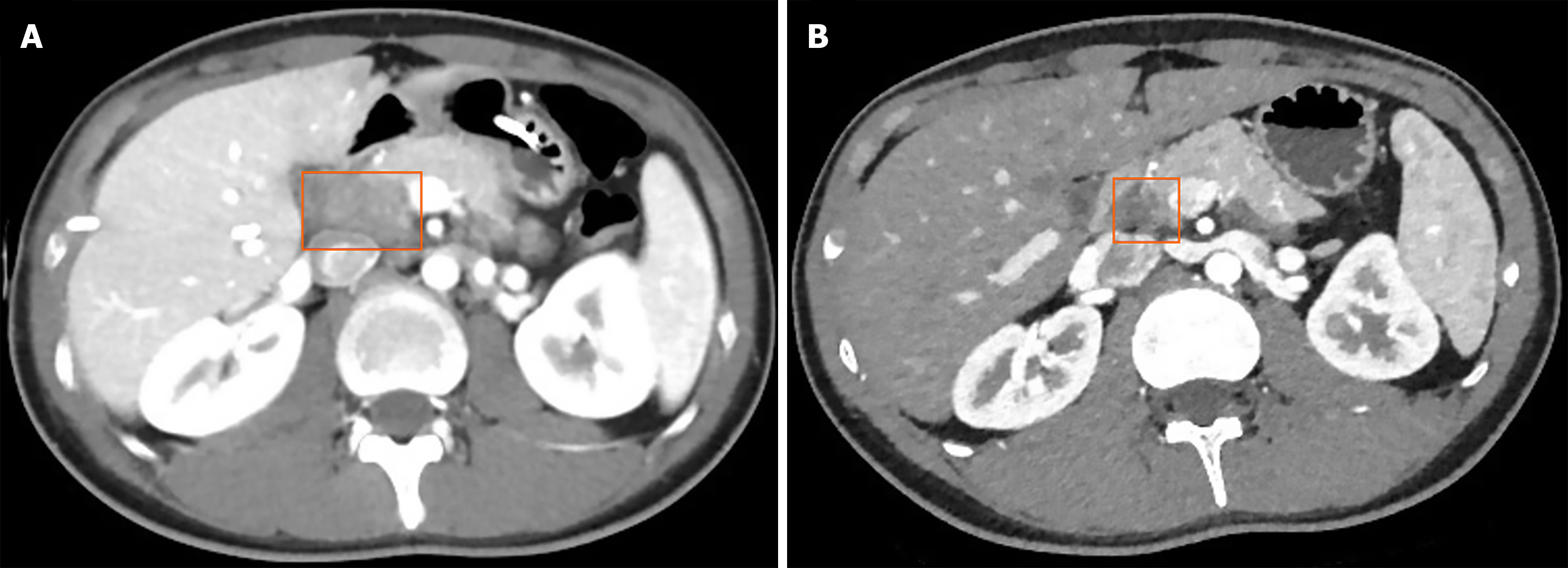
Laboratory tests revealed elevated liver enzymes, C-reactive protein, and pancreatic injury markers. Infectious disease screening for human immunodeficiency virus (HIV), hepatitis B virus, and hepatitis C virus was negative (Table 1). Contrast-enhanced CT showed multiple encapsulated air and fluid collections in the pancreatic head, measuring approximately 29.8 mm × 22.0 mm, likely connected to the duodenal bulb, with suspected ulcer perforation (Figure 1).
| Parameter | Result (reference values) |
| Biochemical test | |
| ALT, U/L | 53 (9-50) |
| AST, U/L | 20 (15-40) |
| ALP, U/L | 132 (45-125) |
| GGT U/L | 113 (10-71) |
| LPS, IU/L | 66.6 (13.00-60.00) |
| p-AMY U/L | 71 (15-53) |
| Inflammatory markers | |
| CRP, mg/L | 47.3 (< 1) |
| Infectious disease screening | |
| HIV | Negative |
| HBV | Negative |
| HCV | Negative |
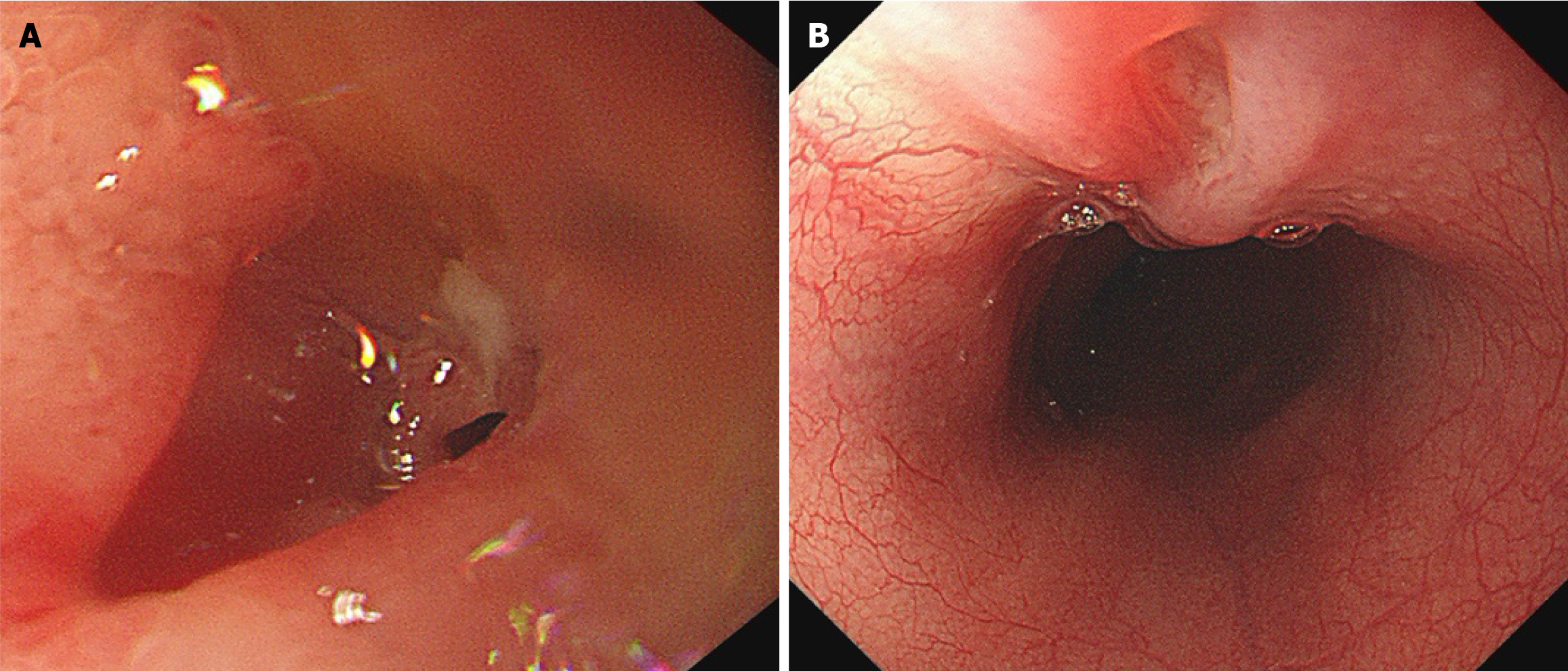
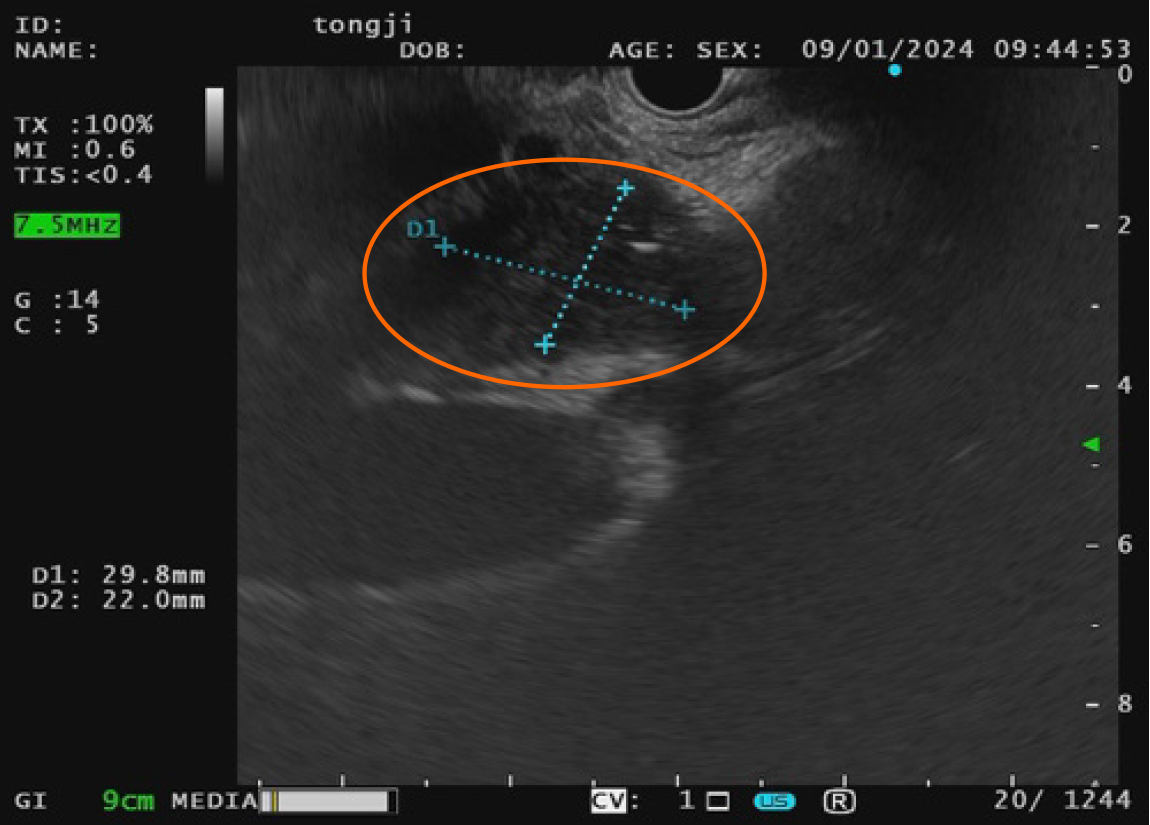
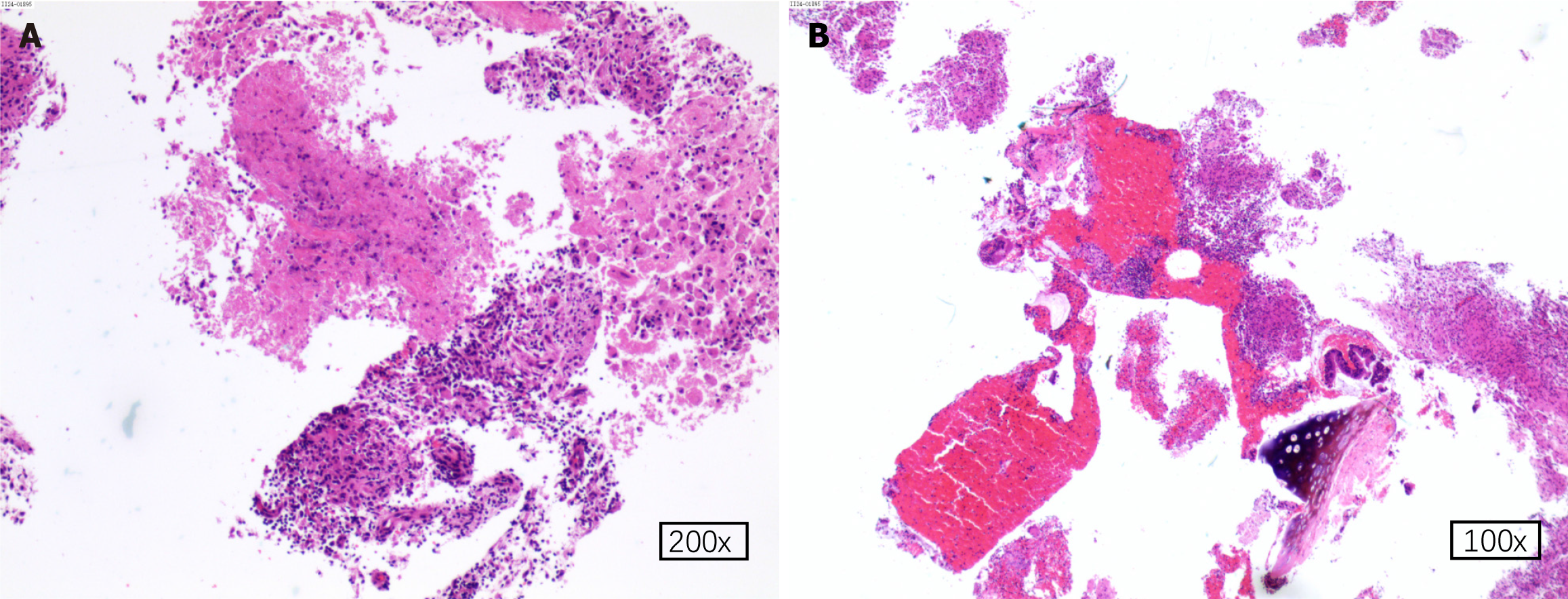
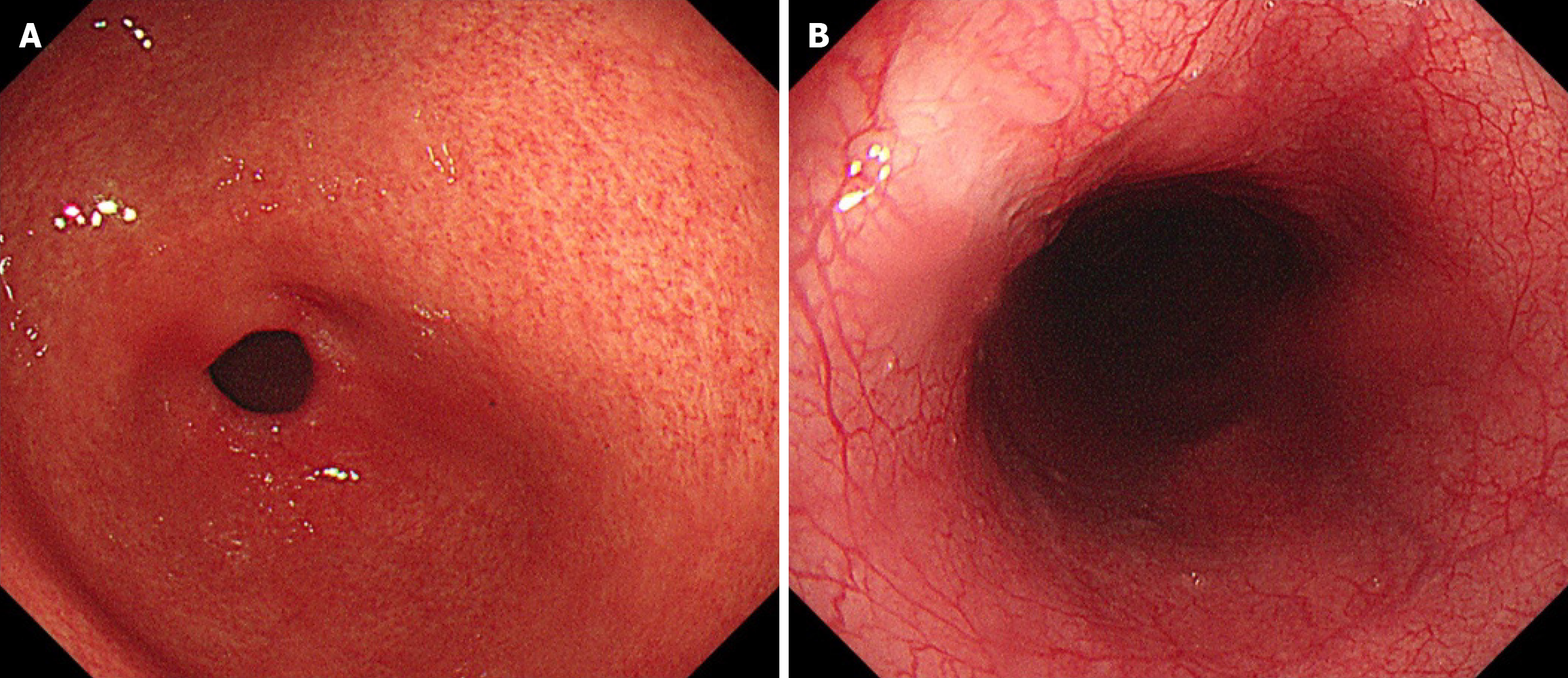
Gastroscopy revealed a duodenal bulb ulcer with perforation, an esophageal ulcer, and chronic superficial gastritis (Figure 2A and B). Chest CT indicated mild inflammation in the right upper lung. Despite initial treatment, the patient remained febrile, prompting a TB skin test, which returned strongly positive (> 20 mm), raising suspicion for pancreatic TB. EUS with FNA identified hypoechoic masses in both the esophageal wall and pancreatic head (Figure 3). Cytology revealed granulomatous inflammation (Figure 4A) with areas of central necrosis. Scattered mucinous epithelial cells with preserved differentiation were identified, along with fragmented lymphocytes, histiocytes, and cartilage components (Figure 4B). These findings, in combination with molecular diagnostic results, are consistent with TB-related pathological changes.
Molecular diagnostics tests, including TB reverse transcription polymerase chain reaction and Mycobacterium TB gene detection, confirmed the pancreatic TB diagnosis(Table 2).
| Diagnostic method | Details | Outcome |
| Clinical presentation | Abdominal pain, weight loss, fever, jaundice, and anorexia | Nonspecific symptoms leading to initial misdiagnosis |
| Imaging (computed tomography/endoscopic ultrasound) | Imaging showed a pancreatic mass, suggestive of malignancy | Mass located in the head of the pancreas |
| Endoscopic ultrasound-guided fine needle aspiration | Biopsy performed to obtain esophageal tissue | Identified granulomas; supported tuberculosis diagnosis |
| Histopathological examination | Granulomas observed on biopsy; caseating necrosis suspected | Confirmed tuberculosis via granuloma presence |
| Molecular testing (PCR) | PCR testing for Mycobacterium tuberculosis performed | Positive result confirmed pancreatic tuberculosis diagnosis |
The patient was initially started on a triple anti-TB regimen consisting of isoniazid, rifampin, and ethambutol; however, his liver function deteriorated. This was attributed to bile duct compression by the pancreatic mass, leading to obstructive jaundice, which was confirmed by magnetic resonance cholangiopancreatography. The patient underwent percutaneous transhepatic biliary drainage combined with hepatoprotective therapy, resulting in improved liver function (Table 3). Following stabilization, anti-TB therapy was gradually reintroduced, starting with 750 mg ethambutol once daily. The regimen was then escalated to triple therapy comprising 300 mg isoniazid, 450 mg rifampin, and 500 mg ethambutol once daily. The patient was advised to continue this regimen after discharge with close follow-up.
| Parameter | After anti-tuberculosis treatment initiation | Post-hepatoprotective treatment | After 1 month of treatment |
| ALT, U/L (9-50) | 332 | 89 | 7 |
| AST, U/L (15-40) | 349 | 45 | 17 |
| CB, μmol/L (≤ 6.89) | 11.7 | 6.1 | 5.5 |
| UCB, μmol/L (≤ 16.8) | 7.3 | 3.0 | 11.2 |
| ALP, U/L (45-125) | 296 | 197 | 80 |
| GGT, U/L (10-71) | 484 | 142 | 35 |
Post-treatment, the patient was closely monitored for clinical symptoms, liver function parameters, and pancreatic mass size. One month after discharge, liver function had returned to normal (Table 2). Throughout therapy, hepatic and renal function remained stable under regular surveillance. At the 1-year follow-up, contrast-enhanced CT revealed a mildly hypodense 7 mm mass in the duodenal-pancreatic head region, showing a significant size reduction compared to the prior scan (December 25, 2023; Figure 1). Follow-up endoscopy demonstrated scar-like changes in the mid-esophagus and ulcer-related scarring on the anterior wall of the duodenal bulb (Figure 5A and B).
TB remains one of the most significant infectious diseases globally. Although individuals of all age groups are susceptible, most cases occur in immunocompetent adults[4]. Approximately 98% of TB cases are reported in low- and middle-income countries, with increased vulnerability in individuals with immunodeficiency, diabetes, malnutrition, or a history of smoking[4]. The lungs are the most affected organ, accounting for approximately 80% of all TB cases. Extrapulmonary TB occurs in approximately 20% of all TB cases, often involving the lymph nodes, genitourinary tract, gas
We performed a literature review by searching PubMed and Google Scholar for case reports on pancreatic TB[4,6-82]. The search strategy included the following keywords: “primary pancreatic tuberculosis”, “pancreatic tuberculosis”, “pancreatic neoplasia”, combined with “case reports”, “case”, or “review”. Boolean operators (AND, OR) were applied as appropriate to refine and expand the search results. The inclusion criteria were as follows: (1) Articles providing complete patient information, including clinical presentation, diagnostic approach, treatment, and prognosis; (2) Case reports, case series, or reviews relevant to pancreatic TB or pancreatic neoplasia; and (3) Full-text availability. Exclusion criteria included articles lacking essential clinical data or those without sufficient diagnostic or therapeutic details. The primary search covered publications from January 2010 to July 2025. However, earlier studies were also included if they offered comprehensive and clinically relevant information deemed valuable for this review.
The mean age of onset for pancreatic TB was 41.12 ± 15.74 years, with a range of 11 to 86 years. The condition was more common in males (52, 56.5%) than in females (40, 43.5%). Most reported cases originated from Asia (47.8%), followed by Europe (19.6%) and Africa (18.5%). Fewer cases were reported from North America and New Zealand (7.6%) and South America (3.3%). Among the hospitalized patients, six tested positive for HIV and two had a prior history of TB (Table 3).
The most common clinical symptom of pancreatic TB was epigastric pain, reported in 73.9% of cases, followed by weight loss (51.1%), anorexia, nausea, or vomiting (35.9%), fever (32.6%), jaundice (17.4%), night sweats (9.8%), and fatigue (6.5%). These nonspecific symptoms contribute to diagnostic delays and often result in misdiagnoses. Imaging studies showed that pancreatic TB most involved the head of the pancreas (69.6%), followed by the body (18.5%), the tail (18.5%), and the neck (1.1%) (Table 4). Diagnosing pancreatic TB typically requires a combination of imaging, histopathological examination, and molecular biological tests. Although imaging studies can detect structural abnormalities, they are limited in distinguishing pancreatic TB from malignancies, as both conditions share overlapping radiological features[6].
| Variables | Value |
| Age, years | 41.12 ± 15.74 |
| Age range, years | 11-86 |
| Sex | |
| Male | 52 (56.5) |
| Female | 40 (43.5) |
| Origin | |
| Asia | 44 (47.8) |
| Africa | 17 (18.5) |
| Europe | 18 (19.6) |
| North America and New Zealand | 7 (7.6) |
| South America | 3 (3.3) |
| HIV-positive | 6 (6.5) |
| Previous tuberculosis | 2 (2.2) |
| Symptoms | |
| Fever | 30 (32.6) |
| Epigastric pain | 68 (73.9) |
| Night sweats | 9 (9.8) |
| Weight loss | 47 (51.1) |
| Jaundice | 16 (17.4) |
| Fatigue | 6 (6.5) |
| Anorexia/nausea/vomiting | 33 (35.9) |
| Distribution | |
| Pancreatic head | 64 (69.6) |
| Pancreatic body | 17 (18.5) |
| Pancreatic tail | 12 (13.0) |
| Pancreatic neck | 1 (1.1) |
Among the cases reviewed, the diagnostic methods included EUS-guided FNA in 42.4% of patients, CT-guided FNA in 12.0%, and exploratory laparotomy in 39.1% (Table 5). Once a definitive diagnosis of pancreatic TB was confirmed, most patients (84.8%) were treated with anti-tuberculous pharmacological therapy as first-line treatment. In 12.0% of cases, pancreatic surgery was performed first, with TB subsequently confirmed through pathological examination, prompting the initiation of anti-tuberculous therapy. Notably, two patients underwent surgical treatment alone without receiving pharmacological intervention (Table 6). Most patients exhibited symptomatic improvement following anti-tuberculous therapy. However, one patient developed secondary pulmonary TB after refusing medical treatment, and another, co-infected with HIV, succumbed to sepsis 5 months after beginning anti-tuberculous therapy (Table 7).
| Diagnostic modalities | Value |
| Endoscopic ultrasound-guided fine-needle aspiration | 39 (42.4) |
| Computed tomography-guided fine-needle aspiration | 11 (12.0) |
| Exploratory laparotomy | 36 (39.1) |
| Treatment | Value |
| Pharmacological | 78 (84.8) |
| Surgical + pharmacological | 11 (12.0) |
| Surgical | 2 (2.2) |
| Outcome | Value |
| Cured | 83 (90.2) |
| Secondary pulmonary tuberculosis | 1 (1.1) |
| Died | 1 (1.1) |
Pancreatic TB is a rare form of extrapulmonary TB that presents significant diagnostic challenges due to its nonspecific clinical features and radiological similarities to pancreatic malignancies. Our literature review demonstrates that pancreatic TB predominantly affects young and middle-aged male patients, particularly in TB-endemic regions, especially in Asia and Africa. In these areas, the clinical presentation can be more heterogeneous and subtle, likely due to the high background prevalence of latent infections[82]. The most frequently reported clinical symptoms include epigastric pain, fever, and weight loss. Less common manifestations such as jaundice, anorexia, night sweats, and fatigue may also occur, though these nonspecific symptoms contribute to diagnostic delays and increase the risk of misdiagnosis.
A definitive pancreatic TB diagnosis generally requires histopathological and molecular confirmation. In our review, 42.2% of cases were diagnosed using EUS-FNA, 12.0% with CT-guided FNA, and 39.1% through exploratory laparotomy. Notably, more than half of the cases were confirmed using minimally invasive, non-surgical techniques, emphasizing the value of EUS-FNA as a preferred first-line diagnostic tool when available. Pancreatic TB can also present with elevated carbohydrate antigen 19-9 Levels[33,67], which may resemble those seen in pancreatic malignancies. Radiological features such as lesion calcification[52,77] and vascular involvement[52] can closely mimic the imaging characteristics of pancreatic cancer. Even with EUS, distinguishing between pancreatic TB and neoplastic lesions can be challenging[7]. This diagnostic uncertainty frequently leads to unnecessary surgical resections, increasing the risk of complications, delaying recovery, and imposing substantial financial and psychological burdens on patients.
Our findings highlight the importance of maintaining a high index of suspicion for pancreatic TB in patients presenting with pancreatic masses, especially in TB-endemic settings or among high-risk populations. A thorough diagnostic workup, including tissue sampling and molecular testing, is essential to avoid misdiagnosis and inappropriate surgical interventions. Once a pancreatic TB diagnosis is established, early initiation of anti-tuberculous therapy is crucial. According to the literature, most patients respond favorably to pharmacological treatment, showing significant clinical and radiologic improvement during follow-up.
The major challenge in managing pancreatic TB lies in achieving accurate and timely diagnosis. Clinicians must maintain a high index of suspicion, particularly in patients from TB-endemic regions who present with pancreatic masses. Early recognition and confirmation through histopathology and molecular testing are crucial for accurate diagnosis. Prompt initiation of anti-tuberculous therapy can significantly improve patient outcomes and prevent unnecessary surgical interventions.
We sincerely appreciate the patient and his family for their cooperation during information acquisition, treatment, and follow-up.
| 1. | Gapizov A, Singla B, Mehta D, Chaudhry M, Subhan M. The Great Mimicker: Pancreatic Tuberculosis Masquerading as a Pancreatic Neoplasm. Cureus. 2025;17:e82298. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Sharma V, Rana SS, Kumar A, Bhasin DK. Pancreatic tuberculosis. J Gastroenterol Hepatol. 2016;31:310-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 46] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 3. | Franco-Paredes C, Leonard M, Jurado R, Blumberg HM, Smith RM. Tuberculosis of the pancreas: report of two cases and review of the literature. Am J Med Sci. 2002;323:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 55] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 4. | Diaconu CC, Gheorghe G, Hortopan A, Enache V, Ceobanu G, Jinga V, Adrian C, Ionescu VA. Pancreatic Tuberculosis-A Condition That Mimics Pancreatic Cancer. Medicina (Kaunas). 2022;58:1165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 5. | Bhansali SK. Abdominal tuberculosis. Experiences with 300 cases. Am J Gastroenterol. 1977;67:324-337. [PubMed] |
| 6. | Panic N, Maetzel H, Bulajic M, Radovanovic M, Löhr JM. Pancreatic tuberculosis: A systematic review of symptoms, diagnosis and treatment. United European Gastroenterol J. 2020;8:396-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 45] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 7. | Abbaszadeh M, Rezai J, Hasibi M, Larry M, Ostovaneh MR, Javidanbardan S, Mirbagheri SA. Pancreatic Tuberculosis in an Immunocompetent Patient: A Case Report and Review of the Literature. Middle East J Dig Dis. 2017;9:239-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Aggarwal S, Nandi S, Verma A, Kumar N. Peripancreatic tuberculosis. BMJ Case Rep. 2023;16:e256433. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Ali M, Shaukat A, Al-Suwaidi Z, Al-Maslamani M. Tuberculosis of pancreas, the first case reported from Qatar. Int J Mycobacteriol. 2019;8:101-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 10. | Alsaif FA, Hassanain MM, Aljebreen AM, Alsharaabi AB, Alalem FA, Alharbi RA, Ali FS, Idriss HK, Alkhalaf OA. Pancreatic tuberculosis in immunocompetent patients. At the University Hospital in Kingdom of Saudi Arabia. Saudi Med J. 2019;40:1052-1057. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Amri F, Chahi K, Mojahid A, Zazour A, Koulali H, Mqaddem OE, Skiker I, Ismaili Z, Kharrasse G. Pancreatic tuberculosis mimicking pancreatic cancer in immunocompetent patients: Case series and diagnostic pathways. Radiol Case Rep. 2025;20:3051-3058. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Arcangeli A, Vilela A, Ross F, Berzaín M, Noboa D, Canaveri A. [Pancreatic tuberculosis]. Medicina (B Aires). 2024;84:992-996. [PubMed] |
| 13. | Arora A, Mukund A, Garg H. Isolated pancreatic tuberculosis: a rare occurrence. Am J Trop Med Hyg. 2012;87:1-2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Barquilla-Cordero P, Chiquero-Palomo M, Martín-Noguerol E, Pacheco-Gómez N, Vinagre-Rodríguez G, Moyano-Calvente SL, Molina-Infante J. [Primary pancreatic tuberculosis in an immunocompetent patient: first case report in Spain]. Gastroenterol Hepatol. 2010;33:582-585. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (1)] |
| 15. | Ben Hammouda S, Chaka A, Njima M, Korbi I, Zenati H, Zakhama A, Hadhri R, Zouari K. Primary pancreatic tuberculosis mimicking pancreatic body cancer. A case report and review of the literature. Ann Med Surg (Lond). 2020;58:80-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 16. | Bhurwal A, Haq MM, Sapru S, Tortora M, Ramasamy D. Isolated Pancreatic Tuberculosis Mimicking Pancreatic Cancer: A Diagnostic Challenge. Case Rep Gastrointest Med. 2018;2018:7871503. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Boutin L, Nayeri M, Frandon J, Borie F. Pancreatic tuberculosis in an 18-year-old patient. Acta Chir Belg. 2024;124:406-408. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Brusko G, Melvin WS, Fromkes JJ, Ellison EC. Pancreatic tuberculosis. Am Surg. 1995;61:513-515. [PubMed] |
| 19. | Catalya S, Tulpule S, Arshed S, Nai Q, Sen S. A Rare Case of Pancreatic Tuberculosis. Pancreas. 2017;46:964-965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Chandrasekhara KL, Iyer SK, Stanek AE, Herbstman H. Pancreatic tuberculosis mimicking carcinoma. Gastrointest Endosc. 1985;31:386-388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Chen CH, Yang CC, Yeh YH, Yang JC, Chou DA. Pancreatic tuberculosis with obstructive jaundice--a case report. Am J Gastroenterol. 1999;94:2534-2536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 22. | Cheng J, Tadi K, Halpern M, Feurdean M, McNelis J, Brensilver J. Pancreatic tuberculosis in a human immunodeficiency virus positive patient: a case report. World J Gastroenterol. 2008;14:939-940. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 5] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Chuabio V, Bandoy J, Ong A, Te M 3rd, Maralit R. Pancreatic masses clinically diagnosed as tuberculosis: Case reports. SAGE Open Med Case Rep. 2024;12:2050313X241262192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 24. | D'Cruz S, Sachdev A, Kaur L, Handa U, Bhalla A, Lehl SS. Fine needle aspiration diagnosis of isolated pancreatic tuberculosis. A case report and review of literature. JOP. 2003;4:158-162. [PubMed] |
| 25. | Debnath P, Jain S, Junare P, Deshmukh R, Patel S, Chandnani S, Kamat R, Contractor QQ, Rathi P. Primary pancreatic tuberculosis with a duodenal fistula in an immunocompetent young man. Clin J Gastroenterol. 2021;14:1567-1570. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 26. | Nanda S, Duarte-Chavez R, Stone L, Fegley M, Amin A, Matin A, Longo S. Pancreatic mass in a 95-year-old male: A rare presentation of tuberculosis. Int J Acad Med. 2017;3:285. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 27. | Evans JD, Hamanaka Y, Olliff SP, Neoptolemos JP. Tuberculosis of the pancreas presenting as metastatic pancreatic carcinoma. A case report and review of the literature. Dig Surg. 2000;17:183-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 28. | Gartini S, Ramdani A, Rhazari M, Thouil A, Kouismi H, Aharmim M, Bourkadi JE. Exceptional association of hepatic and pancreatic tuberculosis mimicking metastatic pancreatic neoplasia: A case report and review of the literature. Ann Med Surg (Lond). 2022;77:103717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Gu Y, Xiao M, Wan Z, Li Q. Isolated pancreatic tuberculosis masquerading as malignancy in an immunocompetent host: a case report and review of the literature. J Int Med Res. 2023;51:3000605231189134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 30. | Gupta D, Patel J, Rathi C, Ingle M, Sawant P. Primary Pancreatic Head Tuberculosis: Great Masquerader of Pancreatic Adenocarcinoma. Gastroenterology Res. 2015;8:193-196. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 31. | Haseeb S, Bilal MI, Bokhari SA, Mirza RT, Riyaz S. Pancreatic Tuberculosis: A Diagnostic Dilemma. Cureus. 2021;13:e16734. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 32. | Hong SG, Kim JS, Joo MK, Lee KG, Kim KH, Oh CR, Park JJ, Bak YT. Pancreatic tuberculosis masquerading as pancreatic serous cystadenoma. World J Gastroenterol. 2009;15:1010-1013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 33. | Kaur M, Dalal V, Bhatnagar A, Siraj F. Pancreatic Tuberculosis with Markedly Elevated CA 19-9 Levels: A Diagnostic Pitfall. Oman Med J. 2016;31:446-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 34. | Khalil B, Adeyeri A, Ramcharan A. Pancreatic tuberculosis mimicking malignancy. J Am Coll Surg. 2009;208:476-477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 35. | Kiziltaş Ş, Çolak Y, Ulaşoğlu C, Öztürk O, Yorulmaz E, Adali G, Enç F, Tuncer İ. A case of isolated pancreatic tuberculosis mimicking pancreatic carcinoma. Turk J Gastroenterol. 2011;22:566-567. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 36. | Kumar PA, Singh G, Joseph JB, Swaminathan S, Venkatakrishnan L. Pancreatic Tuberculosis: A Puzzle for Physicians. A Rare Case and Review of Literature. J Clin Diagn Res. 2016;10:PD29-PD31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 37. | Laamrani FZ, Dafiri R. A rare pediatric case of pancreatic tuberculosis with veinous thrombosis. Diagn Interv Imaging. 2014;95:455-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 38. | Ladas SD, Vaidakis E, Lariou C, Anastasiou K, Chalevelakis G, Kintzonidis D, Raptis SA. Pancreatic tuberculosis in non-immunocompromised patients: reports of two cases, and a literature review. Eur J Gastroenterol Hepatol. 1998;10:973-976. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 25] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 39. | Lakmal K, Jayarajah U, Chandraguptha MR, Nandasena M, Pathirana A. Misdiagnosis of pancreatic tuberculosis as a pancreatic cystic neoplasm - A case report. SAGE Open Med Case Rep. 2023;11:2050313X231200289. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 40. | Machicado JD, Papachristou GI. Pancreatogenic diabetes, acute pancreatitis management, and pancreatic tuberculosis: Appraising the present and setting goals for the future. United European Gastroenterol J. 2020;8:365-368. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 41. | Majid Z, Rehman AU, Ismail H, Luck NH, Mubarak M. Pancreatic Tuberculosis mimicking as a Pancreatic Mass Lesion. J Coll Physicians Surg Pak. 2022;32:1486-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 42. | Matondang SBRE, Wibowo TA, Hilmy IA, Siregar TP, Yonathan IWM. Isolated pancreatic tuberculosis with splenic tuberculosis mimicking lymphoma malignum: A case report. Radiol Case Rep. 2023;18:1775-1778. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 43. | Meesiri S. Pancreatic tuberculosis with acquired immunodeficiency syndrome: a case report and systematic review. World J Gastroenterol. 2012;18:720-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 44. | Miyamoto T, Tone K, Inaki S, Saito R, Maeda M, Nagano Y, Akutsu T, Furube A, Gochi M, Motohashi K, Koido S, Takagi M, Kuwano K. Pancreatic tuberculosis in an immunocompetent young female mimicking a malignant tumor: A case report and diagnostic radiological investigation. Clin Imaging. 2022;81:114-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 45. | Müller MA, Selzner M, Willmann JK. [Pancreatic tuberculosis--a diagnostic chameleon]. Rofo. 2006;178:446-448. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 46. | Pandita KK; Sarla, Dogra S. Isolated pancreatic tuberculosis. Indian J Med Microbiol. 2009;27:259-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 47. | Panzuto F, D'Amato A, Laghi A, Cadau G, D'Ambra G, Aguzzi D, Iannaccone R, Montesani C, Caprilli R, Delle Fave G. Abdominal tuberculosis with pancreatic involvement: a case report. Dig Liver Dis. 2003;35:283-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 48. | Patel ST, Contractor QQ, Nayak CS, Rathi PM. Synchronous pancreatic and scrotal tuberculosis: Double jeopardy. J Postgrad Med. 2023;69:231-233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 49. | T Siddeek RA, Gupta A, Singla T, Rajput D, Ahmed SS, Jeladharan R. Pancreatic tuberculosis mimicking as pancreatic malignancy: Surgeon's dilemma. Indian J Pathol Microbiol. 2023;66:614-617. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 50. | Raghavan P, Rajan D. Isolated pancreatic tuberculosis mimicking malignancy in an immunocompetent host. Case Rep Med. 2012;2012:501246. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Rana SS, Sharma V, Sampath S, Sharma R, Mittal BR, Bhasin DK. Vascular invasion does not discriminate between pancreatic tuberculosis and pancreatic malignancy: a case series. Ann Gastroenterol. 2014;27:395-398. [PubMed] |
| 52. | Rana SS, Sharma V, Sharma R, Bhasin DK. Involvement of mediastinal/intra.abdominal lymph nodes, spleen, liver, and left adrenal in presumed isolated pancreatic tuberculosis: An endoscopic ultrasound study. J Dig Endosc. 2015;06:015-018. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 53. | Rehman A, Maliyakkal AM, Farfar KL, Shaath NM, Naushad VA. An Unusual Cause of a Pancreatic Mass: Pancreatic Tuberculosis. Cureus. 2019;11:e4732. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 54. | Rezeig MA, Fashir BM, Al-Suhaibani H, Al-Fadda M, Amin T, Eisa H. Pancreatic tuberculosis mimicking pancreatic carcinoma: four case reports and review of the literature. Dig Dis Sci. 1998;43:329-331. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 55. | Saavedra JEM, Martínez CAP, Fierro GMT, Bolívar Aguilera IC, Jímenez MCM, Valbuena GLM, Gaona MCM. Pancreatic tuberculosis mimicking a neoplastic mass in an immunosuppressed patient who also presented adenopathy syndrome: Case report. IDCases. 2022;30:e01642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 56. | Sanabe N, Ikematsu Y, Nishiwaki Y, Kida H, Murohisa G, Ozawa T, Hasegawa S, Okawada T, Toritsuka T, Waki S. Pancreatic tuberculosis. J Hepatobiliary Pancreat Surg. 2002;9:515-518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 57. | Sano A, Nishiyama O, Sano H, Yoshida K, Tohda Y. [A Case of Pulmonary Tuberculosis With Pancreatic Lesion]. Kekkaku. 2016;91:617-622. [PubMed] |
| 58. | Selviani Tanic A, Dewi Tetanel LA, Xaverius Rinaldi F, Levina Polanit V, Ivano Kalaij AG, Julian Nelwan B. Pancreatic Tuberculosis Mimicking Pancreatic Tumor: A Case Report from Rural Area in Indonesia. Middle East J Dig Dis. 2024;16:119-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 59. | Shaikh OH, Sunil J, Prakash S, Vijaykumar C, Kumbhar US. Isolated pancreatic tuberculosis masquerading pancreatic malignancy. BMJ Case Rep. 2023;16:e254250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 60. | Shastri A, Davra B, Ashraf MU, Lal R, Gupta N, De A. Tuberculosis masquerading as a pancreatic cyst in a patient with cirrhosis. Trop Doct. 2025;55:54-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 61. | Singh DK, Haider A, Tatke M, Kumar P, Mishra PK. Primary pancreatic tuberculosis masquerading as a pancreatic tumor leading to Whipple's pancreaticoduodenectomy. A case report and review of the literature. JOP. 2009;10:451-456. [PubMed] |
| 62. | Słupski M, Wiciński M, Khuat D, Pawlak-Osińska K. A rare case of isolated pancreatic tuberculosis in a 70-year-old patient - a case report. Pol Przegl Chir. 2019;91:48-50. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 63. | Sohni D. Pancreatic Mass: Include Tuberculosis in the Differential Diagnosis. Cureus. 2021;13:e15430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 64. | Soni A, Tyagi R, Selhi PK, Sood A, Sood N. Pancreatic tuberculosis: A close mimicker of malignancy. Turk J Gastroenterol. 2019;30:1001-1003. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 65. | Sonthalia N, Ray S, Pal P, Saha A, Talukdar A. Fine needle aspiration diagnosis of isolated pancreatic tuberculosis: A case report. World J Clin Cases. 2013;1:181-186. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (4)] |
| 66. | Stambler JB, Klibaner MI, Bliss CM, LaMont JT. Tuberculous abscess of the pancreas. Gastroenterology. 1982;83:922-925. [PubMed] [DOI] [Full Text] |
| 67. | Sun PJ, Lin Y, Cui XJ. Isolated pancreatic tuberculosis with elevated CA 19-9 levels masquerading as a malignancy: A rare case report and literature review. Medicine (Baltimore). 2018;97:e13858. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 68. | Sun SL, Gao F, Cui DX, Wang BS. Isolated pancreatic tuberculosis in non-immunocompromised patient treated by Whipple's procedure: a case report. Chin Med Sci J. 2014;29:58-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 69. | Tri Wicaksana AAF, Bramantono B, Rusli M, Arfijanto MV, Hadi U. Puzzling Clinical Appearance of a Pancreatic Tuberculosis Case. Acta Med Indones. 2023;55:315-319. [PubMed] |
| 70. | Vafa H, Arvanitakis M, Matos C, Demetter P, Eisendrath P, Toussaint E, Hittelet AB, Deviere J, Delhaye M. Pancreatic tuberculosis diagnosed by EUS: one disease, many faces. JOP. 2013;14:256-260. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 71. | van der Naald N, Engelsman AF, Engelbrecht MRW, Verheij J, Besselink MG, Busch OR, van Gulik T. Tuberculosis presenting as a pancreatic cystic neoplasm. BMJ Case Rep. 2018;11:e225983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 72. | Veerabadran P, Sasnur P, Subramanian S, Marappagounder S. Pancreatic tuberculosis-abdominal tuberculosis presenting as pancreatic abscesses and colonic perforation. World J Gastroenterol. 2007;13:478-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 73. | Victor DR, Peixoto PHTM, Medeiros PRA, Barbosa Neto HC, Silva AOR, Victor MER, Ferraz TLL. Pancreatic tuberculosis in a liver transplant recipient: a case report. Rev Inst Med Trop Sao Paulo. 2023;65:e44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 74. | Weiss ES, Klein WM, Yeo CJ. Peripancreatic tuberculosis mimicking pancreatic neoplasia. J Gastrointest Surg. 2005;9:254-262. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 75. | Woodfield JC, Windsor JA, Godfrey CC, Orr DA, Officer NM. Diagnosis and management of isolated pancreatic tuberculosis: recent experience and literature review. ANZ J Surg. 2004;74:368-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 76. | Wu CS, Wang SH, Kuo TT. Pancreatic tuberculosis mimicking pancreatic head carcinoma: a case report and review of the literature. Infection. 1994;22:287-289. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 77. | Xia F, Poon RT, Wang SG, Bie P, Huang XQ, Dong JH. Tuberculosis of pancreas and peripancreatic lymph nodes in immunocompetent patients: experience from China. World J Gastroenterol. 2003;9:1361-1364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 66] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 78. | Yan Y, Hou M, Jin P, Ma B. A case of pancreatic tuberculosis mimicking solid pseudopapillary neoplasm of the pancreas. Asian J Surg. 2024;47:4657-4658. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 79. | Yang YJ, Li YX, Liu XQ, Yang M, Liu K. Pancreatic tuberculosis mimicking pancreatic carcinoma during anti-tuberculosis therapy: A case report. World J Clin Cases. 2014;2:167-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 80. | Yokoyama T, Miyagawa S, Noike T, Shimada R, Kawasaki S. Isolated pancreatic tuberculosis. Hepatogastroenterology. 1999;46:2011-2014. [PubMed] |
| 81. | Zhu M, Zhang N, Tao W, Wang Z, He S. Pancreatic Tuberculosis with Vascular Involvement and Peritoneal Dissemination in a Young Man. Case Rep Med. 2017;2017:4396759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 82. | Gowthaman U, Mushtaq K, Tan AC, Rai PK, Jackson DC, Agrewala JN. Challenges and solutions for a rational vaccine design for TB-endemic regions. Crit Rev Microbiol. 2015;41:389-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
Open Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/