Published online Jun 21, 2021. doi: 10.3748/wjg.v27.i23.3303
Peer-review started: January 28, 2021
First decision: February 24, 2021
Revised: March 10, 2021
Accepted: May 24, 2021
Article in press: May 24, 2021
Published online: June 21, 2021
Processing time: 140 Days and 5.9 Hours
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causative agent of coronavirus disease 2019 (COVID-19), is responsible for the first pandemic of the 21st century. As found in adults, signs and symptoms related to the disease mainly involve the respiratory tract in the paediatric population. However, a considerable number of children present with gastrointestinal symptoms such as vomiting, abdominal pain, and diarrhea. The purpose of this review is an accurate description, from pathogenesis to clinical presentation, diagnosis and treatment, of COVID-19 effects on the gastrointestinal system at a paediatric age. SARS-CoV-2 can be identified in stool specimens of affected children by real-time polymerase chain reaction techniques. Positivity can last for several weeks after the end of the symptomatic phase. Gastrointestinal signs and symptoms are generally self-limited, can correlate with blood tests and imaging alterations, and may require supportive treatment such as hydration. However, they can precede severe disease manifestations such as the COVID-19-related multisystem inflammatory syndrome. Children belonging to risk categories such as those affected by celiac disease, inflammatory bowel disease, and hepatic disease seem to not have a more severe course than the others, even if they are undergoing immunosuppressant treatment. Medical follow-ups of patients with chronic diseases need to be revised during the pandemic period in order to postpone unnecessary tests, mainly endoscopic ones.
Core Tip: Gastrointestinal signs and symptoms seem to be more common in paediatric coronavirus disease 2019 (COVID-19) compared to adults. Manifestations are generally self-limited, and may only require supportive treatment. In a minority of children, gastrointestinal involvement may precede severe forms such as the multisystem inflammatory syndrome. Conversely to what is expected, the COVID-19 impact on paediatric patients with chronic gastrointestinal diseases is limited, with no need for therapeutic regimen changes. However, the severe acute respiratory syndrome coronavirus 2 pandemic determined multiple variations in routine practice. The use of telemedicine and telehealth can be a solution in order to continue to provide regular follow-up to chronic patients, avoiding the risk of viral transmission.
- Citation: Calitri C, Fumi I, Ignaccolo MG, Banino E, Benetti S, Lupica MM, Fantone F, Pace M, Garofalo F. Gastrointestinal involvement in paediatric COVID-19 — from pathogenesis to clinical management: A comprehensive review. World J Gastroenterol 2021; 27(23): 3303-3316
- URL: https://www.wjgnet.com/1007-9327/full/v27/i23/3303.htm
- DOI: https://dx.doi.org/10.3748/wjg.v27.i23.3303
The coronavirus disease 2019 (COVID-19) is caused by single-stranded RNA severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). The disease was first described in Wuhan, China, in December 2019. Then the virus spread rapidly worldwide, making the World Health Organization declare the first pandemic of the 21st century in March 2020[1]. On March 4, 2021, there were more than 114 million confirmed cases of COVID-19 worldwide, with nearly 3 million registered deaths[2].
The clinical spectrum of COVID-19 in children and adolescents ranges from asymptomatic/pauci symptomatic infection to severe disease. Digestive symptoms related to COVID-19 such as vomiting, diarrhea, and abdominal pain have emerged as extrapulmonary manifestations, with SARS-CoV-2 RNA detected in the faeces of people affected, suggesting faecal-oral transmission. Children with gastrointestinal (GI) chronic diseases, including those undergoing immunosuppressive or biological treatment, need to be strictly evaluated for the risk of developing severe forms of COVID-19. GI involvement may play a role in the presentation of symptoms in children affected by the multisystem inflammatory syndrome (MIS-C) associated with COVID-19[3].
The purpose of this review is to summarise what is known about COVID-19 GI manifestations in children, from diagnosis to symptoms and treatment, including the peculiar aspects of patients with GI chronic diseases.
There are many mechanisms through which SARS-CoV-2 can interact and damage the GI system.
The first is a virus-induced cytopathic effect. SARS-CoV-2 interacts with membrane receptors of the host cells through the spike protein, which mediates the fusion of the virus and the cell membrane[4]. Angiotensin-converting enzyme receptor 2 (ACE-2) and transmembrane protease serine 2 (TMPRSS2) are both essential for the cellular entry process of the virus. They are co-expressed at a high level both in the type II alveolar cells of the lung, in the glandular cells of the gastric, duodenal, and rectal epithelium, and in the enterocytes of ileum and colon[4]. After viral entry, new virions are synthesised in the cytoplasm of the GI cells and then are released in the GI tract, causing direct disruption of enterocytes and the viral shedding in the stool[5,6]. As absorptive enterocytes are destroyed by SARS-CoV-2, this changes the intestinal permeability, leading to malabsorption and unbalanced intestinal secretion, resulting in the genesis of diarrhea[6-8].
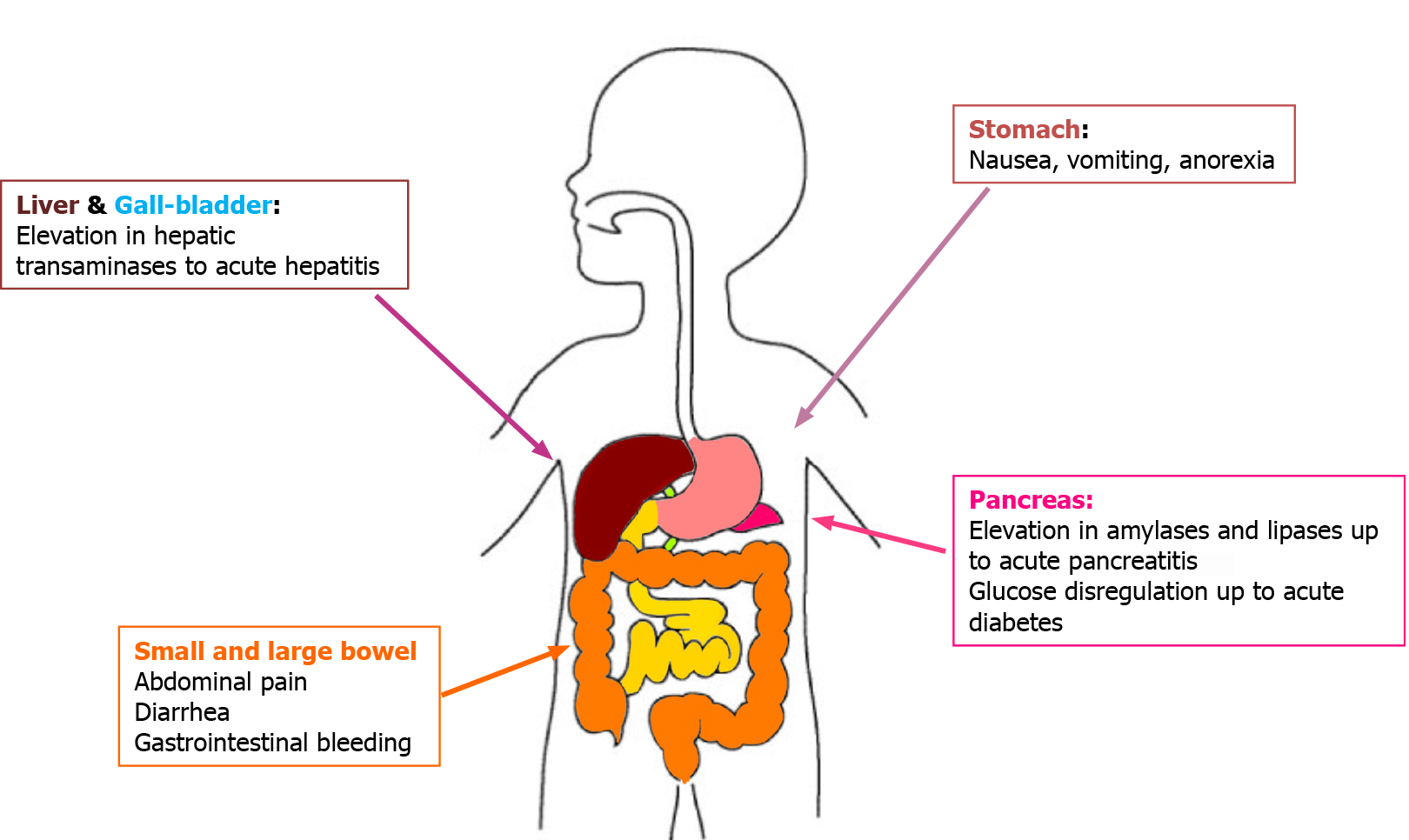
As ACE-2 is equally expressed in liver and pancreas, the virus cytopathic effect can also be detected in these organs. Hepatic distribution of ACE-2 is peculiar; it is highly expressed in the endothelial layer of small blood vessels but not in the sinusoidal endothelium[9]. Its concentration on cholangiocytes’ surface is higher than of the hepatocyte surface and is similar to the type II alveolar cells of the lungs. SARS-CoV-2 may have the ability to infect cholangiocytes via the ACE-2 receptor and directly dysregulate liver function[7,9]. However, there is no evidence of active virus replication in hepatocyte cells[6]. A histological examination of a liver biopsy obtained from a deceased COVID-19 patient showed no viral inclusions, but rather a microve
SARS-CoV-2 can affect both the exocrine and endocrine pancreas; an abnormal elevation of amylase and lipase, together with glucose dysregulation and acute diabetes are described in patients with severe COVID-19 pneumonia, with develo
The second mechanism depends on immune-system activation[11]. SARS-CoV-2-infected cells release a large number of inflammatory mediators and chemokines such as interleukin (IL)-2, IL-7, granulocyte colony-stimulating factor, interferon-γ inducible protein 10, monocyte chemoattractant protein 1, macrophage inflammatory protein 1-α and tumour necrosis factor-alpha (TNF-α). This “cytokine storm” causes neutrophil aggregation and activates type 1 helper cells. This promotes the accumulation of immune cells in the GI system[7]; a large number of infiltrating plasma cells and lymphocytes together with interstitial oedema have been found in the inherent layers of the stomach, duodenum, and rectum in adult COVID-19 patients[8]. The cytokine overproduction correlates with disease severity and multiple organ insufficiency development outside the lung, liver, and pancreas.
SARS-CoV-2 may alter the intestinal microbiome even when only the respiratory mucosa is involved (the “gut-lung axis”)[5,6]. Increased inflammatory mediators lead to lung hyperpermeability so that the virus and inflammatory mediators migrate to the intestine via circulation. SARS-CoV-2 and the inflammatory mediators disrupt the intestinal permeability leading to the leakage of gut microbes and associated metabolites into circulation. The leaked microbes and products migrate to organs including lungs and produce abnormalities.
Other hypothesised mechanisms of liver and pancreatic damage include hypoxic injury due to respiratory distress and drug-induced injury[5-7,10]. Kidneys can also be involved, as they are fundamental in eliminating amylases and lipases from the circulatory stream: Their malfunction can lead to a transient increase in pancreatic enzymes[10].
Children and adolescents with GI symptoms such as nausea, vomiting, or diarrhea should be seriously evaluated for COVID-19, as the faecal-oral route transmission of SARS-CoV-2 is extensively described (Figure 1). Oba et al[12] reported that GI signs and symptoms may affect 3% to 79% of children, adolescents and adults with COVID-19. Various paediatric systematic reviews evidenced similar results[4,6,13], curiously with different frequencies in the United States and Europe compared to China (21.1% vs 12.9%)[4]. Manifestations include diarrhea (2%-50%), anorexia (40%-50%), vomiting (4%-67%), nausea (1%-30%), abdominal pain (2%-6%) and GI bleeding (4%-14%). Diarrhea and vomiting are the most common GI symptoms described, sometimes as the first symptoms of disease, even before or in absence of respiratory manifestations. Diarrhea, often watery, occurs from 1 d to 8 d after the onset of COVID-19, with a median time of 3.3 d, and lasts for a mean of 4 d[12]. Vomiting is more often reported in the paediatric population than in the adult one.
GI symptoms may correlate with severe COVID-19 in children admitted to hospital. A Spanish multicentre study involving 101 paediatric inpatients noticed that patients presenting with GI symptoms tended to have higher C-reactive protein (CRP), procalcitonin (PCT), ferritin and aspartate aminotransferase values, and to receive antibiotics, lopinavir-ritonavir, corticosteroids and immunoglobulins more frequently than the others. Moreover, they had a higher risk of paediatric intensive care unit (ICU) admission, regardless of age, gender, immunosuppressive therapy and previous underlying conditions[14]. Similar findings were evidenced in studies among adults, where those with diarrhea had a higher risk of ICU admission regardless of the age, sex and comorbidities[15,16].
GI symptoms such as vomiting, abdominal pain and/or diarrhea are typically present and considered diagnostic criteria in children with the COVID-19-related MIS-C (71%-84% of the cases), along with fever lasting more than 3 d, evidence of mucocutaneous inflammation (rash, conjunctivitis, oromucosal changes), lymphopenia and high levels of circulating inflammation[3,17-19]. Abdominal pain may be so relevant that few children with a final diagnosis of MIS-C initially present with acute surgical abdomen; they may undergo exploratory laparotomy with intra-operative findings of mesenteric lymphadenitis and peritonitis[20]. Evolution to severe disease including cardiac involvement, hypotension and shock is often described in children with MIS-C[19].
Prompt diagnosis of SARS-CoV-2 infection can determine treatment strategies and influence the outcome of the disease in children. Suggestive symptoms together with the history of a close contact with a COVID-19 patient are the most useful criteria for a suspicion of infection[21]. Diagnosis is confirmed by SARS-CoV-2 isolation in patient samples, while auxiliary examinations are useful to determine the severity of the disease and organ involvement in infected children.
Leukopenia with neutropenia and lymphocytosis or lymphopenia are the most common findings at blood count. Erythrocyte sedimentation rate is elevated in a great number of children, as well as IL-10 and IL-6. CRP and PCT levels can be normal. However, a PCT value > 0.5 ng/mL may be suggestive of bacterial coinfection or of a severe autoinflammatory state such as the MIS-C[22,23].
A mild increase in liver enzymes is well described in COVID-19, with various percentages among studies, ranging from 13% to 50% in paediatric patients; however, serious liver dysfunction is uncommon[6,24]. Elevated aspartate aminotransferase levels (> 50 UI/L; 20.4%-50% of cases) are observed more frequently than alanine aminotransferase levels (> 45 UI/L; 9%-35% of cases). Increased transaminases are often accompanied by high creatinine kinase and lactate dehydrogenase, suggesting the possibility of a viral myositis[25,26].
Considerable alteration in liver enzymes is common in those with severe spectrum of disease (40%-60%) compared to those who are asymptomatic or have mild manifestations (18%-25%). Nevertheless, every child with COVID-19 and raised transaminases should be investigated for other causes of liver pathology[5].
Patients with MIS-C present with a remarkable elevation in transaminases levels (52.3%) together with a mild decrease in albumin rates. Elevation of lipase levels > 3 times the normal limit was observed in one paediatric patient with MIS-C[3,25]. In fact, pancreatic involvement in adults with COVID-19 is well described, with a lipase increase in 7.9% of cases. Bilirubin levels are also more than doubled in those with severe infection, when compared to those with mild disease[10].
Nucleic acid testing is the method of choice for virus identification. SARS-CoV-2 RNA can be detected in sputum, lower respiratory tract secretions, urine, stool, tears, and blood samples by real-time polymerase chain reaction (RT-PCR) technology or by viral gene sequencing. RT-PCR on nose-pharyngeal swab (NPS) is the diagnostic method of choice in children. However, paediatric patients tested for SARS-CoV-2 by RT-PCR on a rectal swab or stool returned a positive result in 89% of cases, despite not presenting with any GI symptoms. Moreover, COVID-19 children may have a stool SARS-CoV-2 RT-PCR positive result more frequently than adults in spite of a negative respiratory swab; RT-PCR on stool samples seems to be as accurate as those performed on the NPS in order to identify SARS-CoV-2[27,28].
As the faecal-oral route is confirmed as a way for SARS-CoV-2 transmission, all children with digestive tract symptoms should be tested for SARS-CoV-2 on faeces[12,29]. RT-PCR on stool becomes positive from 2 d to 2 wk after the respiratory specimen ones, and 23%-82% of patients continue to have positive faecal test for approximately 1-16 d after their NPS turn negative[4,28]. The interval to stool negativisation may be prolonged, exceeding 70 d in healthy children, longer in patients treated with corticosteroids[4].
Therefore, despite major evidence being necessary to consider a negative RT-PCR on faeces as one of the discharge criteria, it may be important to recommend isolation at home for at least 2 wk after hospital discharge[4].
Little is known about typical imaging findings in COVID-19 paediatric patients with GI symptoms. Abdominal ultrasonography to computed tomography or magnetic resonance imaging may be taken into consideration in patients with a severe course of disease or relevant blood test alterations (e.g., increased transaminases and/or lipases). Miller et al[3] described a paediatric population of 44 cases with MIS-C and GI symptoms, with abdominal images collected in 15 patients. Common findings were mesenteric adenitis (2 patients), biliary sludge or acalculous cholecystis (6) and ascites (6). Normal abdominal imaging was found in 20% of cases. In 3 patients, ultrasonography or magnetic resonance imaging evidenced bowel wall thickening analogous to that of inflammatory bowel disease (IBD). One child had severe clinical manifestations (fever, abdominal pain, rash) with evidence of concentric mural thickening, oedema and hyperenhancement of a short segment of terminal ileum, with similar findings in the rectosigmoid colon. Two patients had nonspecific ultrasonography imaging, with thickened bowel loops on the right iliac site associated with highly elevated inflammatory index and mildly decreased albumin levels[3].
Generally, COVID-19 paediatric patients require symptomatic care, both because the great majority of them has mild symptoms and also because all virus-targeted therapies are employed exclusively in clinical trial settings[30]. Supportive care included fever treatment, oxygen therapy in patients with respiratory complications with or without airway management, and nasogastric or intravenous hydration in children unable to tolerate oral fluids such as those with severe GI symptoms[30].
COVID-19 children are at higher risk of developing malnourishment during critical illness, which has been associated with increased morbidity and mortality; therefore, nutritional therapy plays a significant role in these children[12]. The European Society of Paediatric and Neonatal Intensive Care cornerstones for nutrition recommend commencing early enteral feeding within 24 h of hospital admission in critically ill children unless contraindicated. Energy requirements need not exceed resting energy expenditure during the acute phase and an increase in enteral nutrition in a stepwise fashion is recommended until the goal for delivery is achieved. Overfeeding harms critically ill children, especially during the acute phase[31].
In children with severe GI COVID-19 and MIS-C, enteral nutrition support may be continued for a long time into the recovery phase until sufficient oral intake is consistently achieved to support physical and nutritional rehabilitation[32]. Enteral nutrition is also recommended in critically ill children on hemodynamic support with a stable clinical condition; parenteral nutrition has to be withheld during the first 7 d of admission[12,31]. However, in children who continue to require fluid resuscitation or escalating doses of vasoactive agents with evidence of severe GI dysfunction and MIS-C, enteral nutrition may be withheld for up to 7 d[32].
It may be useful to consider providing enteral feeds via a post-pyloric tube in critically ill children with COVID-19 with severe GI symptoms or cardiac manifestations or inotrope resistance shock in which early gastric enteral feeding is not possible[12,32].
There is no evidence to support supra-physiological doses of micronutrients supplementation, including zinc during the acute phase[32].
Recent literature suggests the role of probiotics in manipulating the gut microbiota, as they may play a fruitful role as a therapeutic strategy for GI COVID-19 and its comorbidities. Focused clinical trials are needed to support this hypothesis[33].
Based on currently available limited data, children with comorbidities or pre-existing chronic diseases, such as IBD or liver disease, do not seem to carry a higher risk of COVID-19 infection compared to the general population (see below)[34,35].
Celiac disease (CeD), also known as celiac sprue or gluten-sensitive enteropathy, is a common immune-mediated inflammatory disease of the small intestine resulting from sensitivity to dietary gluten and related proteins in genetically predisposed individuals[36]. It is estimated that CeD affects approximately 0.5% to 1% of the general population[37]. CeD therapy consists in a strict gluten-free diet (GFD) to achieve complete resolution of symptoms and mucosal healing for most individuals. It also reduces the risk of long-term adverse health outcomes including intestinal lymphoma[38].
During the COVID-19 pandemic, it has been postulated that some patients with chronic GI disease may be at an increased risk of a more severe illness due to COVID-19. Potential risk factors in these patients include their chronic inflammatory disease, comorbidities (e.g., diabetes mellitus), and the use of glucocorticoids[39].
Considering that CeD subjects have an increased risk of both bacterial and viral infections, such as pneumococcal pneumonia[40], sepsis[41], and complications from influenza virus, probably due to malnutrition and increased mucosal permeability[42]. Various studies have investigated the possibility of a higher risk of SARS-CoV-2 infection in CeD patients compared to the general population.
Data on patients with chronic GI disease who have been infected by SARS-CoV-2 are accumulating, and disease-specific patient registries include Surveillance Epidemiology of Coronavirus Under Research Exclusion (SECURE-Celiac). This is an international, paediatric and adult database to monitor and report the outcomes of COVID-19 in patients with CeD. On January 17, 2021 a total number of 111 cases was reported; 4 cases < 18 years of age, nobody was hospitalised, and no death was registered (SECURE-Celiac Database, available at: https://covidceliac.org/data). Several studies evidenced that the risk of severe COVID-19 is not increased in patients with CeD both in adulthood and childhood[43-48]. A large-scale study, performed on 18000 participants from different Countries, including Argentina, Australia, Canada, Italy, Mexico, New Zealand, Spain, Uruguay, and the United States, examined the risk of COVID-19 in CeD compared with the nonceliac population. They found that patients with CeD had similar odds to contract SARS-CoV-2 infection compared to the control subjects. The presence of comorbidities, which were identified as an important predictor of morbidity and mortality associated with COVID-19, were more frequent in CeD than the control subjects. However, they did not determine higher odds for SARS-CoV-2 infection in CeD. The authors observed that the sole factor increasing the odds of a positive test was exposure to a COVID-19 contact. In this study, patients with CeD were less exposed to COVID-19 than the control subjects, probably due to a careful prevention related to their chronic condition[46]. Moreover, a cross-sectional study conducted by a paediatric celiac centre in Central Italy did not show any significant increase in SARS-CoV-2 infection prevalence among the group of children with CeD compared to the general population[48].
A relevant aspect of the COVID-19 pandemic is the impact of restrictive measures on primary health care. In this new scenario, all elective diagnostic procedures such as paediatric digestive endoscopy have been suspended and were allowed only in emergency cases[49,50].
As esophagogastroduodenoscopy is still necessary for CeD diagnosis in children with low antibodies titres and this elective procedure has been substantially shut down during the COVID-19 pandemic, many children remained undiagnosed and therefore untreated for a long time. The European Society of Paediatric Gastroenterology Hepatology and Nutrition (ESPGHAN) analysed the feasibility and accuracy of a biopsy-free approach in suspected CeD children with tissue transglutaminase-immunoglobulin A (TGA-IgA) values < 10 time upper the normal limit (ULN) during the COVID-19 outbreak. A temporary reduction of the TGA-IgA threshold seems feasible in antiendomysial antibodies (EMA) positive children with TGA-IgA between 5 and 10 ULN for a biopsy-sparing approach[51].
The global impact of the lockdown on the compliance to GFD in CeD patients was investigated in a cross-sectional survey conducted in Italy on a total of 1983 patients with CeD, 1614 (81.4%) adults and 369 (18.6%) children. The compliance to GFD was unchanged for 70% of the subjects, and even improved for 29%, in particular for those with a previous worse disease control, due to reduced opportunities for contamination and transgression and an increased use of naturally gluten-free ingredients[52].
An observational study on 71 paediatric patients with CeD examined the prevalence of functional GI disorders (FGIDs) in children during the COVID-19 lockdown. The Authors observed a reduced prevalence of FGIDs in these patients, probably due to a good quality of life and a low state of anxiety related to the positive effects of reducing stressful events, such as school, as well as to an increased parental closeness, which may have influenced the occurrence of GI symptoms and the related FGIDs. Psychosocial aspects may play a particularly important role in the genesis of the FGIDs, despite the presence of a residual low-grade chronic inflammatory process[53].
IBD, including Crohn’s disease (CD) and ulcerative colitis, are chronic pathologies of the GI system characterised by a dysregulated immune response with an over production of pro-inflammatory cytokines. To control the disease, patients require frequent treatment with corticosteroids, immunosuppressants, and/or biological drugs with the consequence of an increased risk of infections. IBDs tend to be more extensive and severe in children than in adults, with a consistently greater need for immunomodulators and biological agents to maintain remission in this population[54].
The IBD-related immunosuppressive treatment has raised concerns regarding the management and the risk of SARS-CoV-2 infection severity. On the other hand, it can be assumed that immunosuppressive medications may be associated with a decreased risk of poor COVID-19 outcomes by limiting the cytokine storm typical of severe COVID-19.
The first document on the global impact of SARS-CoV-2 infection on paediatric IBD was published in March 2020 by the Paediatric IBD Porto Group of ESPGHAN. It was a survey among 102 Paediatric IBD centres affiliated with the Porto and Interest-group of ESPGHAN, with external paediatric experts from China and South Korea invited to participate. All cases of COVID-19 in IBD paediatric patients enrolled were mild despite they were under immunosuppressive treatment. The study expert group suggested that IBD children, with or without immunosuppressive and biological therapy, do not seem to have a greater risk of severe SARS-CoV-2 infection compared to the general population. Due to this, they recommend not stopping standard IBD treatments[35].
A total of 522 IBD patients were enrolled in one of the Italian regions with greater COVID-19 incidence and were followed for a 1-mo period between February and March 2020. Fifty-nine (11%) paediatric patients (7-18-years-old) were included. In this IBD cohort, the Authors did not report any case of COVID-19 despite the fact that the enrolled patients continued to receive immunosuppressive treatments such as thiopurines or methotrexate and steroids[55].
Surveillance Epidemiology of Coronavirus Under Research Exclusion (SECURE-IBD) is an international, paediatric and adult database to monitor and report on outcomes of COVID-19 occurring in IBD patients. On January 5, a total number of 4280 cases was reported; 441 cases < 19 years of age, only 22% hospitalised, and no death evidenced[56].
Brenner et al[57] described the course of the disease of COVID-19 in a sample of 209 paediatric IBD patients (age 18 years and younger) from the 2 international databases (The SECURE-IBD and the COVID-19 database of the Paediatric IBD Porto group of ESPGHAN). They reported a hospitalisation rate of 7%; only 2 patients (1%) required mechanical ventilation, one for a MIS-C and one for a secondary infection. There were no deaths. Risk factors for hospitalisation included other comorbidities, moderate/ severe IBD disease activity, and GI symptoms.
In March 2020 Paediatric IBD Porto group of ESPGHAN generated guidance points for paediatric gastroenterologists in the era of the COVID-19 pandemic. These points are mainly focus on therapy indications. There is no evidence that any of the drugs used in IBDs, including immune-modulators and biological drugs, increases the severity of COVID-19. IBD patients should stay on IBD medications prescribed before the SARS-CoV-2 pandemic[35]. Newly diagnosed patients should be treated according to the standard protocols as before the spread of the virus[5,12].
SARS-CoV-2 enters cells via the ACE-2 receptor, widely expressed in the GI tract. Its expression is upregulated during inflammation and this overexpression may therefore increase host susceptibility. There are two forms of ACE-2: full-length ACE-2 with a structural transmembrane domain, which anchors its extracellular domain to the cellular membrane, and a soluble form of ACE-2 that lacks the membrane anchor and circulates in the blood. Some authors have speculated that the soluble form may act as a competitive interceptor for SARS-CoV-2, preventing the binding of the viral particle to the surface full-length ACE-2[58]. It can explain why children with IBD have a COVID-19 course similar to healthy individuals.
By contrast, immune dysfunction in untreated IBD children may increase the risk of a severe inflammatory response to SARS-CoV-2 infection. Pro-inflammatory cytokines, TNF-α, IL-1β, and IL-6 are overproduced in IBD patients[59], and serum concentration of TNF-α and IL-6 are associated with severe COVID-19 illness[60]. Dolinger et al[61] described a case of MIS-C associated with COVID-19 in a recently diagnosed paediatric CD patient. He was treated with infliximab for both clinical entities with a successful result. The authors speculated that anti-TNF agents could play a role in the therapy of patients with active IBD and MIS-C temporally related to COVID-19.
A COVID-19 Risk Calculator is on the SECURE-IBD website and it is intended for use by physicians caring for patients with IBD to calculate the risk of hospitalisation, ICU admission, mechanical ventilation, or death in IBD patients with COVID-19. It is available at: https://covidibd.org/covid-19-risk-calculator/.
Regarding CeD, the COVID-19 pandemic determined essential healthcare changes, mainly during the lockdown period, which could alter IBD follow-up in children. These include postponed elective appointments, reduced access to diagnostic endoscopy, and difficulties in continuing infusion therapy, with potential clinical and psychological negative impact on the course of the disease.
A recent survey, conducted in the United Kingdom, outlined that more than 50% of children and young people presenting with a suspected diagnosis of IBD were diagnosed without a histological examination due to restrictions placed on endoscopy at over 90% of centres across the United Kingdom. The authors observed that “diagnosing children and young people with IBD, without a histological confirmation, is controversial and only acceptable given the special circumstances we are currently finding ourselves in”[62].
A multicentre investigation of the Italian Society of Paediatric Gastroenterology, Hepatology and Nutrition (SIGENP) analysed the impact of COVID-19 related lockdown on the levels of care offered to paediatric IBD patients all over the Italian territory[63]. In total, 2291 children affected by IBD were regularly followed by the 21 participating referral centres; a total of 6 cases of SARS-CoV-2 infections of 2291 (0.2%) patients were identified. In 5 of 6 (83.3%) cases, the clinical course of the SARS-CoV-2 infection resulted as mild, without the need for hospitalisation. The authors observed a reduction of hospitalisations for new diagnosis and endoscopic re-evaluation, while the number of hospitalisations for relapse and surgical procedure remained substantially unchanged. The number of outpatients’ visits were significantly decreased. Biologics’ infusions did not significantly vary and Italian paediatric IBD centres did not modify their therapeutic approach in the majority of cases, as recommended by the ESPGHAN guidelines.
Differently from the United Kingdom data, the multicentre Italian survey found a drop in the new diagnoses during the lockdown.
The fear of SARS-CoV-2 infection could determine the risk of inappropriate management of IBD with consequent significant impact on the health of IBD patients[35]. As the decrease of face-to-face consultations, telemedicine represents a promising opportunity. In the Italian survey, telemedicine services for children with IBD were activated in 52.3% of the participating centres.
Recently, members of the SIGENP IBD group study drafted a position paper with the aim of providing guidance for the management of paediatric IBD on the basis of the existing evidence[64].
In addition to specific recommendations regarding diagnostic procedures and therapies, the position paper provides general indications for a safer and gradual restarting of routine clinical activities after the COVID-19 peak, with particular attention also on psychological issues.
At present, there is no concrete evidence that the SARS-CoV-2 infection causes significant worsening in underlying chronic liver disease. Children undergoing treatment for pathologies like Wilson disease, autoimmune hepatitis, hepatitis B and C should continue their treatment protocols[5]. Elevated transaminases in COVID-19 are not a contraindication for antiviral therapy in viral chronic hepatitis, even if regular monitoring of liver function is needed[65].
Reports of critical disease in adults and children with cancer have raised concerns about the risk of a severe COVID-19 course in patients with immune system impairment, including recipients of solid organ transplants on long-term immune suppression[66].
Data on the COVID-19 course and outcome in children needing liver solid organ transplantation (SOT), or already transplanted, are limited. Reports by the team of the Transplantation Unit of Papa Giovanni XXIII Hospital in Bergamo (Italy) are reassuring; liver-transplanted young patients did not experience any severe respiratory infection, despite residing in one of the earliest and hardest-hit areas world
Six cases of children awaiting transplantation and eight cases of paediatric transplant recipients infected by SARS-CoV-2 were reported by Doná et al[68] None of the candidates in the SOT waiting list, nor any of the SOT recipients, presented severe COVID-19.
It seems that the immunosuppressive treatment in immunocompromised children may not significantly increase the risk of severe COVID-19, as its complications are mainly driven by a well-documented pro-inflammatory state[69].
Post-liver transplant patients need particular emphasis on preventive measures, such as frequent hand washing, frequent cleaning of touched surfaces and social distancing. Generally, as the cell injury in COVID-19 disease is thought to be immune-mediated, immunosuppression and mycophenolate should not be reduced or stopped in asymptomatic post-transplant patients. In an established COVID-19, the continu
The emergence of COVID-19 has had a profound impact on transplantation worldwide, both for issues regarding donors and recipients viral transmission and for healthcare resources, as the magnitude of COVID-19 cases in certain regions exceeds the available capacity of the health system[70].
Members of the European Reference Network of Paediatric Transplantation investigated the impact of the COVID-19 outbreak on paediatric transplant activity and healthcare practices in both SOT and hematopoietic stem cell transplantation: transplantation activity as well as outpatient visits were negatively affected by the COVID-19 pandemic across Europe[68]. The risk of SARS-CoV-2 transmission and the shortage of hospital bed capacity and staff might be the main determinants of this reduction. Significant extension of these limitations in healthcare resources may have severe consequences both for children on the transplant waiting list and for transplanted patients as the access to close monitoring and diagnostic testing would be significantly reduced. In this emerging public health context, there are no reasons to delay or interrupt oncological treatments or withdraw immune suppression, to postpone life-saving treatments in liver-transplanted patients, or to suspend transplant programs as an a priori preventative measure[71].
The COVID-19 pandemic determined diagnosis delay and higher complication rates among common paediatric medical conditions[72].
An example may be represented by the increased incidence of complicated appendicitis among children: no changes in patient demographics nor in the rate of appendicitis itself could explain this phenomenon. A considerable extension in the average time between the onset of symptoms and surgery was identified as the causative agent: normally, surgical intervention time is influenced by other factors such as elective activity and availability of theatre and staff. The fear of contracting SARS-CoV-2 infection leads the parents to avoid hospital access of their child at the early stages of the disease, doubling the time before the patient’s access to the Emergency Department (ED). Delayed access to ED may explain the higher prevalence of complicated appendicitis[73]. At the same time and for the same reasons, a statistically significant increased rate of appendiceal perforation during the COVID-19 pandemic was reported. In a cross-sectional study, appendiceal perforation also resulted in pelvic abscess, bowel obstruction, and sepsis[74]. Delayed presentation of children with acute appendicitis at the ED may increase the morbidity related to a common childhood condition, leading to increased complications and poor outcomes[75,76].
Although complicated courses have arisen, an Italian study noticed a reduction in the total number of acute appendicitis cases. A decrease in social contacts during the lockdown period, a reduction of respiratory and GI infections, healthy food intake due to the permanence at home and increased domestic hygiene could have played a crucial role, bringing mild appendicitis to a spontaneous resolution cases with or without domestic treatments[77,78].
This review describes the spectrum of GI manifestations in paediatric COVID-19, from signs and symptoms of disease to laboratory and imaging tests alterations. All the organs can be involved, ranging from mild to severe alterations. Pathogenesis is outlined, however further clarifications of virus-induced damages are needed. Although generally self-limited, GI signs and symptoms are closely related to complicated courses of disease: As a matter of fact, GI involvement is a diagnostic-criteria for the MIS-C. Close monitoring of infected children will permit to delineate potential predictors of severe COVID-19 evolution.
Conversely to what is expected, the COVID-19 impact on children with chronic GI diseases appears to be limited, with no need for therapeutic regimen changes. Ongoing studies may confirm these initial observations. Certainly, the SARS-CoV-2 pandemic determined multiple variations in routine practice of these patients. The use of telemedicine and telehealth can be a solution in order to continue to provide regular follow-up to chronic patients, avoiding the risk of viral transmission.
Thanks to Professor Basta F. for the language revision.
| 1. | World Health Organization. WHO Coronavirus Disease (COVID-19) pandemic. [cited 4 March 2021]. In: World Health Organization [Internet]. Available from: https:// covid-19.who.int/. |
| 2. | World Health Organization. WHO Coronavirus Disease (COVID-19) dashboard. [cited 4 March 2021]. In: World Health Organization [Internet]. Available from: https://covid-19.who.int/. |
| 3. | Miller J, Cantor A, Zachariah P, Ahn D, Martinez M, Margolis KG. Gastrointestinal Symptoms as a Major Presentation Component of a Novel Multisystem Inflammatory Syndrome in Children That Is Related to Coronavirus Disease 2019: A Single Center Experience of 44 Cases. Gastroenterology 2020; 159: 1571-1574. e2. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 160] [Cited by in RCA: 183] [Article Influence: 30.5] [Reference Citation Analysis (0)] |
| 4. | Wang JG, Cui HR, Tang HB, Deng XL. Gastrointestinal symptoms and fecal nucleic acid testing of children with 2019 coronavirus disease: a systematic review and meta-analysis. Sci Rep. 2020;10:17846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 29] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 5. | Matthai J, Shanmugam N, Sobhan P; Indian Society of Pediatric Gastroenterology; Hepatology and Nutrition; Pediatric Gastroenterology Chapter of Indian Academy of Pediatrics. Coronavirus Disease (COVID-19) and the Gastrointestinal System in Children. Indian Pediatr. 2020;57:533-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 6. | Chiappini E, Licari A, Motisi MA, Manti S, Marseglia GL, Galli L, Lionetti P. Gastrointestinal involvement in children with SARS-COV-2 infection: An overview for the pediatrician. Pediatr Allergy Immunol. 2020;31 Suppl 26:92-95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Patel KP, Patel PA, Vunnam RR, Hewlett AT, Jain R, Jing R, Vunnam SR. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J Clin Virol. 2020;128:104386. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 144] [Cited by in RCA: 121] [Article Influence: 20.2] [Reference Citation Analysis (1)] |
| 8. | Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-1833. e3. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1985] [Cited by in RCA: 2016] [Article Influence: 336.0] [Reference Citation Analysis (3)] |
| 9. | Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and the liver. J Hepatol. 2020;73:1231-1240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 364] [Cited by in RCA: 364] [Article Influence: 60.7] [Reference Citation Analysis (4)] |
| 10. | Zippi M, Hong W, Traversa G, Maccioni F, De Biase D, Gallo C, Fiorino S. Involvement of the exocrine pancreas during COVID-19 infection and possible pathogenetic hypothesis: a concise review. Infez Med. 2020;28:507-515. [PubMed] |
| 11. | Lei HY, Ding YH, Nie K, Dong YM, Xu JH, Yang ML, Liu MQ, Wei L, Nasser MI, Xu LY, Zhu P, Zhao MY. Potential effects of SARS-CoV-2 on the gastrointestinal tract and liver. Biomed Pharmacother. 2021;133:111064. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 66] [Cited by in RCA: 62] [Article Influence: 12.4] [Reference Citation Analysis (3)] |
| 12. | Oba J, Carvalho WB, Silva CA, Delgado AF. Gastrointestinal manifestations and nutritional therapy during COVID-19 pandemic: a practical guide for pediatricians. Einstein (Sao Paulo). 2020;18:eRW5774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 13. | Xu Y, Li X, Zhu B, Liang H, Fang C, Gong Y, Guo Q, Sun X, Zhao D, Shen J, Zhang H, Liu H, Xia H, Tang J, Zhang K, Gong S. Characteristics of pediatric SARS-CoV-2 infection and potential evidence for persistent fecal viral shedding. Nat Med. 2020;26:502-505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1183] [Cited by in RCA: 1058] [Article Influence: 176.3] [Reference Citation Analysis (0)] |
| 14. | Gonzalez Jimenez D, Velasco Rodríguez-Belvís M, Ferrer Gonzalez P, Domínguez Ortega G, Segarra O, Medina Benitez E, Garcia Tirado D, Garcia Romero R, Vecino López R, Crehuá-Gaudiza E, Queralt M, Palomino Pérez LM, Diaz Martin JJ. COVID-19 Gastrointestinal Manifestations Are Independent Predictors of PICU Admission in Hospitalized Pediatric Patients. Pediatr Infect Dis J. 2020;39:e459-e462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 28] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Jin X, Lian JS, Hu JH, Gao J, Zheng L, Zhang YM, Hao SR, Jia HY, Cai H, Zhang XL, Yu GD, Xu KJ, Wang XY, Gu JQ, Zhang SY, Ye CY, Jin CL, Lu YF, Yu X, Yu XP, Huang JR, Xu KL, Ni Q, Yu CB, Zhu B, Li YT, Liu J, Zhao H, Zhang X, Yu L, Guo YZ, Su JW, Tao JJ, Lang GJ, Wu XX, Wu WR, Qv TT, Xiang DR, Yi P, Shi D, Chen Y, Ren Y, Qiu YQ, Li LJ, Sheng J, Yang Y. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut. 2020;69:1002-1009. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 944] [Cited by in RCA: 874] [Article Influence: 145.7] [Reference Citation Analysis (0)] |
| 16. | Wan Y, Li J, Shen L, Zou Y, Hou L, Zhu L, Faden HS, Tang Z, Shi M, Jiao N, Li Y, Cheng S, Huang Y, Wu D, Xu Z, Pan L, Zhu J, Yan G, Zhu R, Lan P. Enteric involvement in hospitalised patients with COVID-19 outside Wuhan. Lancet Gastroenterol Hepatol. 2020;5:534-535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 124] [Cited by in RCA: 119] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 17. | Nakra NA, Blumberg DA, Herrera-Guerra A, Lakshminrusimha S. Multi-System Inflammatory Syndrome in Children (MIS-C) Following SARS-CoV-2 Infection: Review of Clinical Presentation, Hypothetical Pathogenesis, and Proposed Management. Children (Basel). 2020;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 247] [Cited by in RCA: 277] [Article Influence: 46.2] [Reference Citation Analysis (0)] |
| 18. | Radia T, Williams N, Agrawal P, Harman K, Weale J, Cook J, Gupta A. Multi-system inflammatory syndrome in children & adolescents (MIS-C): A systematic review of clinical features and presentation. Paediatr Respir Rev. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 142] [Cited by in RCA: 188] [Article Influence: 37.6] [Reference Citation Analysis (0)] |
| 19. | Vogel TP, Top KA, Karatzios C, Hilmers DC, Tapia LI, Moceri P, Giovannini-Chami L, Wood N, Chandler RE, Klein NP, Schlaudecker EP, Poli MC, Muscal E, Munoz FM. Multisystem inflammatory syndrome in children and adults (MIS-C/A): Case definition & guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 176] [Cited by in RCA: 175] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 20. | Guanà R, Pagliara C, Delmonaco AG, Scottoni F, Bordese R, Pruccoli G, Gennari F. Multisystem inflammatory syndrome in SARS-CoV-2 infection mimicking acute appendicitis in children. Pediatr Neonatol. 2021;62:122-124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 21. | Miao H, Li H, Yao Y, Wu M, Lu C, Wang J, Tian M, Li Y, Luo P, Gu J, Yuan B, Wang S, Zhao X, Gan W, Zhao D. Update on recommendations for the diagnosis and treatment of SARS-CoV-2 infection in children. Eur J Clin Microbiol Infect Dis. 2020;39:2211-2223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Li B, Zhang S, Zhang R, Chen X, Wang Y, Zhu C. Epidemiological and Clinical Characteristics of COVID-19 in Children: A Systematic Review and Meta-Analysis. Front Pediatr. 2020;8:591132. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 75] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 23. | Henry BM, Lippi G, Plebani M. Laboratory abnormalities in children with novel coronavirus disease 2019. Clin Chem Lab Med. 2020;58:1135-1138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 147] [Article Influence: 24.5] [Reference Citation Analysis (0)] |
| 24. | Esmaeili Dooki M, Mehrabani S, Sorkhi H, Nikpour M, Tabatabaie M, Mohammadi M, Kiani M. COVID-19 and Digestive System in Children: A Retrospective Study. Arch Iran Med. 2020;23:782-786. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 25. | Parri N, Lenge M, Buonsenso D; Coronavirus Infection in Pediatric Emergency Departments (CONFIDENCE) Research Group. Children with Covid-19 in Pediatric Emergency Departments in Italy. N Engl J Med. 2020;383:187-190. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 450] [Cited by in RCA: 478] [Article Influence: 79.7] [Reference Citation Analysis (0)] |
| 26. | Zhang C, Shi L, Wang FS. Liver injury in COVID-19: management and challenges. Lancet Gastroenterol Hepatol. 2020;5:428-430. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1348] [Cited by in RCA: 1308] [Article Influence: 218.0] [Reference Citation Analysis (8)] |
| 27. | Xu CLH, Raval M, Schnall JA, Kwong JC, Holmes NE. Duration of Respiratory and Gastrointestinal Viral Shedding in Children With SARS-CoV-2: A Systematic Review and Synthesis of Data. Pediatr Infect Dis J. 2020;39:e249-e256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 55] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 28. | Zhang L, Peres TG, Silva MVF, Camargos P. What we know so far about Coronavirus Disease 2019 in children: A meta-analysis of 551 Laboratory-confirmed cases. Pediatr Pulmonol. 2020;55:2115-2127. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 48] [Article Influence: 8.0] [Reference Citation Analysis (0)] |
| 29. | Tian Y, Rong L, Nian W, He Y. Review article: gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;51:843-851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 594] [Cited by in RCA: 587] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 30. | Chan K, Beck C, Chauvin-Kimoff L, Gripp K, Krmpotic K, Thakore S, Trottier ED; Acute Care Committee. The acute management of COVID-19 in paediatrics. Posted on April 20, 2020. [cited 4 March 2021]. In: Canadian Paediatric Society [Internet]. Available from: https://www.cps.ca/en/documents/position/the-acute-management-of-paediatric-coronavirus-disease-2019covid-19. |
| 31. | Tume LN, Valla FV, Joosten K, Jotterand Chaparro C, Latten L, Marino LV, Macleod I, Moullet C, Pathan N, Rooze S, van Rosmalen J, Verbruggen SCAT. Nutritional support for children during critical illness: European Society of Pediatric and Neonatal Intensive Care (ESPNIC) metabolism, endocrine and nutrition section position statement and clinical recommendations. Intensive Care Med. 2020;46:411-425. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 215] [Cited by in RCA: 177] [Article Influence: 29.5] [Reference Citation Analysis (0)] |
| 32. | Marino LV, Valla FV, Tume LN, Jotterand-Chaparro C, Moullet C, Latten L, Joosten K, Verbruggen SCAT. Considerations for nutrition support in critically ill children with COVID-19 and paediatric inflammatory multisystem syndrome temporally associated with COVID-19. Clin Nutr. 2021;40:895-900. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 33. | Din AU, Mazhar M, Waseem M, Ahmad W, Bibi A, Hassan A, Ali N, Gang W, Qian G, Ullah R, Shah T, Ullah M, Khan I, Nisar MF, Wu J. SARS-CoV-2 microbiome dysbiosis linked disorders and possible probiotics role. Biomed Pharmacother. 2021;133:110947. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 67] [Cited by in RCA: 70] [Article Influence: 14.0] [Reference Citation Analysis (0)] |
| 34. | Murray KF, Gold BD, Shamir R, Agostoni C, Pierre-Alvarez R, Kolacek S, Hsu EK, Chen J. Coronavirus Disease 2019 and the Pediatric Gastroenterologist. J Pediatr Gastroenterol Nutr. 2020;70:720-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 35. | Turner D, Huang Y, Martín-de-Carpi J, Aloi M, Focht G, Kang B, Zhou Y, Sanchez C, Kappelman MD, Uhlig HH, Pujol-Muncunill G, Ledder O, Lionetti P, Dias JA, Ruemmele FM, Russell RK; Paediatric IBD Porto group of ESPGHAN. Corona Virus Disease 2019 and Paediatric Inflammatory Bowel Diseases: Global Experience and Provisional Guidance (March 2020) from the Paediatric IBD Porto Group of European Society of Paediatric Gastroenterology, Hepatology, and Nutrition. J Pediatr Gastroenterol Nutr. 2020;70:727-733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 94] [Cited by in RCA: 99] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 36. | Schuppan D. Current concepts of celiac disease pathogenesis. Gastroenterology. 2000;119:234-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 349] [Cited by in RCA: 326] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 37. | Gujral N, Freeman HJ, Thomson AB. Celiac disease: prevalence, diagnosis, pathogenesis and treatment. World J Gastroenterol. 2012;18:6036-6059. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 412] [Cited by in RCA: 426] [Article Influence: 30.4] [Reference Citation Analysis (6)] |
| 38. | Consensus Development Conference on Celiac Disease. NIH Consens State Sci Statements. 2004;21:1-23. [PubMed] |
| 39. | Centers for Disease Control and Prevention. People with certain medical conditions. [cited 29 December 2020]. In: Centers for Disease Control and Prevention [Internet]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/groups-at-higher-risk.html. |
| 40. | Thomas HJ, Wotton CJ, Yeates D, Ahmad T, Jewell DP, Goldacre MJ. Pneumococcal infection in patients with coeliac disease. Eur J Gastroenterol Hepatol. 2008;20:624-628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 41. | Ludvigsson JF, Olén O, Bell M, Ekbom A, Montgomery SM. Coeliac disease and risk of sepsis. Gut. 2008;57:1074-1080. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 94] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 42. | Mårild K, Fredlund H, Ludvigsson JF. Increased risk of hospital admission for influenza in patients with celiac disease: a nationwide cohort study in Sweden. Am J Gastroenterol. 2010;105:2465-2473. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 62] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 43. | Gokden Y, Hot S, Adas M, Ogutmen Koc D, Atak S, Hot AB. Celiac disease and COVID-19 pandemic: should we worry? Acta Gastroenterol Belg. 2020;83:517-525. [PubMed] |
| 44. | Zingone F, D'Odorico A, Lorenzon G, Marsilio I, Farinati F, Savarino EV. Risk of COVID-19 in celiac disease patients. Autoimmun Rev. 2020;19:102639. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 45. | Emmi G, Bettiol A, Mattioli I, Silvestri E, Di Scala G, Urban ML, Vaglio A, Prisco D. SARS-CoV-2 infection among patients with systemic autoimmune diseases. Autoimmun Rev. 2020;19:102575. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 114] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 46. | Zhen J, Stefanolo JP, Temprano MP, Tedesco S, Seiler C, Caminero AF, de-Madaria E, Huguet MM, Vivas S, Niveloni SI, Bercik P, Smecuol E, Uscanga L, Trucco E, Lopez V, Olano C, Mansueto P, Carroccio A, Green PHR, Day A, Tye-Din J, Bai JC, Ciacci C, Verdu EF, Lebwohl B, Pinto-Sanchez MI. The Risk of Contracting COVID-19 Is Not Increased in Patients With Celiac Disease. Clin Gastroenterol Hepatol. 2021;19:391-393. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 47. | Schiepatti A, Alimenti E, Maimaris S, Nicolardi ML, Manzella La Barbera F, Baiardi P, Biagi F. Prevalence, incidence and clinical features of SARS-CoV-2 infection in adult coeliac patients. Eur J Gastroenterol Hepatol. 2021;Publish Ahead of Print. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Lionetti E, Fabbrizi A, Catassi C. Prevalence of COVID-19 in Italian Children With Celiac Disease: A Cross-Sectional Study. Clin Gastroenterol Hepatol. 2021;19:1075. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 49. | Gralnek IM, Hassan C, Beilenhoff U, Antonelli G, Ebigbo A, Pellisè M, Arvanitakis M, Bhandari P, Bisschops R, Van Hooft JE, Kaminski MF, Triantafyllou K, Webster G, Pohl H, Dunkley I, Fehrke B, Gazic M, Gjergek T, Maasen S, Waagenes W, de Pater M, Ponchon T, Siersema PD, Messmann H, Dinis-Ribeiro M. ESGE and ESGENA Position Statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020;52:483-490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 263] [Cited by in RCA: 298] [Article Influence: 49.7] [Reference Citation Analysis (0)] |
| 50. | Ruan W, Fishman DS, Lerner DG, Engevik MA, Elmunzer BJ, Walsh CM; International Pediatric Endoscopy COVID-19 Alliance. Changes in Pediatric Endoscopic Practice During the Coronavirus Disease 2019 Pandemic: Results From an International Survey. Gastroenterology. 2020;159:1547-1550. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 51. | Trovato CM, Montuori M, Cucchiara S, Oliva S. ESPGHAN 'biopsy-sparing' guidelines for celiac disease in children with low antitransglutaminase during COVID-19. Eur J Gastroenterol Hepatol. 2020;32:1523-1526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 52. | Monzani A, Lionetti E, Felici E, Fransos L, Azzolina D, Rabbone I, Catassi C. Adherence to the Gluten-Free Diet during the Lockdown for COVID-19 Pandemic: A Web-Based Survey of Italian Subjects with Celiac Disease. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 30] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 53. | Nastro FF, Tolone C, Serra MR, Pacella D, Campanozzi A, Strisciuglio C. Prevalence of functional gastrointestinal disorders in children with celiac disease during the COVID-19 Lockdown. Dig Liver Dis. 2020;52:1082-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 54. | Moon JS. Clinical Aspects and Treatments for Pediatric Inflammatory Bowel Diseases. Pediatr Gastroenterol Hepatol Nutr. 2019;22:50-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 55. | Norsa L, Indriolo A, Sansotta N, Cosimo P, Greco S, D'Antiga L. Uneventful Course in Patients With Inflammatory Bowel Disease During the Severe Acute Respiratory Syndrome Coronavirus 2 Outbreak in Northern Italy. Gastroenterology. 2020;159:371-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 114] [Cited by in RCA: 120] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 56. | Brenner EJ, Ungaro RC, Colombel JF, Kappelman MD. SECURE-IBD Database Public Data Update. [cited 7 Jan 2021]. In: SECURE-IBD Database [Internet]. Available from: https://covidibd.org/. |
| 57. | Brenner EJ, Pigneur B, Focht G, Zhang X, Ungaro RC, Colombel JF, Turner D, Kappelman MD, Ruemmele FM. Benign Evolution of SARS-Cov2 Infections in Children With Inflammatory Bowel Disease: Results From Two International Databases. Clin Gastroenterol Hepatol 2021; 19: 394-396. e5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 58. | Batlle D, Wysocki J, Satchell K. Soluble angiotensin-converting enzyme 2: a potential approach for coronavirus infection therapy? Clin Sci (Lond). 2020;134:543-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 327] [Article Influence: 54.5] [Reference Citation Analysis (0)] |
| 59. | Singh UP, Singh NP, Murphy EA, Price RL, Fayad R, Nagarkatti M, Nagarkatti PS. Chemokine and cytokine levels in inflammatory bowel disease patients. Cytokine. 2016;77:44-49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 256] [Article Influence: 23.3] [Reference Citation Analysis (0)] |
| 60. | Chen G, Wu D, Guo W, Cao Y, Huang D, Wang H, Wang T, Zhang X, Chen H, Yu H, Zhang M, Wu S, Song J, Chen T, Han M, Li S, Luo X, Zhao J, Ning Q. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130:2620-2629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2835] [Cited by in RCA: 3470] [Article Influence: 578.3] [Reference Citation Analysis (0)] |
| 61. | Dolinger MT, Person H, Smith R, Jarchin L, Pittman N, Dubinsky MC, Lai J. Pediatric Crohn Disease and Multisystem Inflammatory Syndrome in Children (MIS-C) and COVID-19 Treated With Infliximab. J Pediatr Gastroenterol Nutr. 2020;71:153-155. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 101] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 62. | Ashton JJ, Kammermeier J, Spray C, Russell RK, Hansen R, Howarth LJ, Torrente F, Deb P, Renji E, Muhammed R, Paul T, Kiparissi F, Epstein J, Lawson M, Hope B, Zamvar V, Narula P, Kadir A, Devadason D, Bhavsar H, Beattie RM. Impact of COVID-19 on diagnosis and management of paediatric inflammatory bowel disease during lockdown: a UK nationwide study. Arch Dis Child. 2020;105:1186-1191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 63. | Arrigo S, Alvisi P, Banzato C, Bramuzzo M, Celano R, Civitelli F, D'Arcangelo G, Dilillo A, Dipasquale V, Felici E, Fuoti M, Gatti S, Knafelz D, Lionetti P, Mario F, Marseglia A, Martelossi S, Moretti C, Norsa L, Panceri R, Renzo S, Romano C, Romeo E, Strisciuglio C, Martinelli M. Impact of COVID-19 pandemic on the management of paediatric inflammatory bowel disease: An Italian multicentre study on behalf of the SIGENP IBD Group. Dig Liver Dis. 2021;53:283-288. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 64. | Arrigo S, Alvisi P, Banzato C, Bramuzzo M, Civitelli F, Corsello A, D'Arcangelo G, Dilillo A, Dipasquale V, Felici E, Fuoti M, Gatti S, Giusti Z, Knafelz D, Lionetti P, Mario F, Marseglia A, Martelossi S, Moretti C, Norsa L, Nuti F, Panceri R, Rampado S, Renzo S, Romano C, Romeo E, Strisciuglio C, Martinelli M. Management of paediatric IBD after the peak of COVID-19 pandemic in Italy: A position paper on behalf of the SIGENP IBD working group. Dig Liver Dis. 2021;53:183-189. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 65. | Bangash MN, Patel J, Parekh D. COVID-19 and the liver: little cause for concern. Lancet Gastroenterol Hepatol. 2020;5:529-530. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 324] [Cited by in RCA: 359] [Article Influence: 59.8] [Reference Citation Analysis (0)] |
| 66. | Zhang L, Zhu F, Xie L, Wang C, Wang J, Chen R, Jia P, Guan HQ, Peng L, Chen Y, Peng P, Zhang P, Chu Q, Shen Q, Wang Y, Xu SY, Zhao JP, Zhou M. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020;31:894-901. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 819] [Cited by in RCA: 1025] [Article Influence: 170.8] [Reference Citation Analysis (16)] |
| 67. | D'Antiga L. Coronaviruses and Immunosuppressed Patients: The Facts During the Third Epidemic. Liver Transpl. 2020;26:832-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 479] [Cited by in RCA: 495] [Article Influence: 82.5] [Reference Citation Analysis (0)] |
| 68. | Doná D, Torres Canizales J, Benetti E, Cananzi M, De Corti F, Calore E, Hierro L, Ramos Boluda E, Melgosa Hijosa M, Garcia Guereta L, Pérez Martínez A, Barrios M, Costa Reis P, Teixeira A, Lopes MF, Kaliciński P, Branchereau S, Boyer O, Debray D, Sciveres M, Wennberg L, Fischler B, Barany P, Baker A, Baumann U, Schwerk N, Nicastro E, Candusso M, Toporski J, Sokal E, Stephenne X, Lindemans C, Miglinas M, Rascon J, Jara P; ERN TransplantChild. Pediatric transplantation in Europe during the COVID-19 pandemic: Early impact on activity and healthcare. Clin Transplant. 2020;34:e14063. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 69. | Li X, Geng M, Peng Y, Meng L, Lu S. Molecular immune pathogenesis and diagnosis of COVID-19. J Pharm Anal. 2020;10:102-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1000] [Cited by in RCA: 946] [Article Influence: 157.7] [Reference Citation Analysis (0)] |
| 70. | Aslam S, Mehra MR. COVID-19: Yet another coronavirus challenge in transplantation. J Heart Lung Transplant. 2020;39:408-409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 64] [Cited by in RCA: 98] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 71. | Nicastro E, Di Giorgio A, Zambelli M, Ginammi M, Bravi M, Stroppa P, Casotti V, Palladino R, Colledan M, D'Antiga L. Impact of the Severe Acute Respiratory Syndrome Coronavirus 2 Outbreak on Pediatric Liver Transplant Recipients in Lombardy, Northern Italy. Liver Transpl. 2020;26:1359-1362. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 72. | Snapiri O, Rosenberg Danziger C, Krause I, Kravarusic D, Yulevich A, Balla U, Bilavsky E. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672-1676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 129] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 73. | Raffaele A, Cervone A, Ruffoli M, Cereda E, Avolio L, Parigi GB, Riccipetitoni G. Critical factors conditioning the management of appendicitis in children during COVID-19 Pandemic: experience from the outbreak area of Lombardy, Italy. Br J Surg. 2020;107:e529-e530. [PubMed] |
| 74. | Place R, Lee J, Howell J. Rate of Pediatric Appendiceal Perforation at a Children's Hospital During the COVID-19 Pandemic Compared With the Previous Year. JAMA Netw Open. 2020;3:e2027948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 47] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 75. | Lee-Archer P, Blackall S, Campbell H, Boyd D, Patel B, McBride C. Increased incidence of complicated appendicitis during the COVID-19 pandemic. J Paediatr Child Health. 2020;56:1313-1314. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 76. | Velayos M, Muñoz-Serrano AJ, Estefanía-Fernández K, Sarmiento Caldas MC, Moratilla Lapeña L, López-Santamaría M, López-Gutiérrez JC. [Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis]. An Pediatr (Barc). 2020;93:118-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 77. | Zampieri N. Effect of SARS-CoV-2 on the Incidence of Appendicitis: The Role of Quarantine. Pediatr Emerg Care. 2020;36:e482-e483. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 78. | Tankel J, Keinan A, Blich O, Koussa M, Helou B, Shay S, Zugayar D, Pikarsky A, Mazeh H, Spira R, Reissman P. The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-centre Study. World J Surg. 2020;44:2458-2463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: Italy
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ashktorab H S-Editor: Gao CC L-Editor: Filipodia P-Editor: Ma YJ