Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.820
Peer-review started: August 2, 2014
First decision: August 27, 2014
Revised: September 12, 2014
Accepted: November 18, 2014
Article in press: November 19, 2014
Published online: January 21, 2015
Processing time: 171 Days and 10.5 Hours
Endoscopic ultrasound (EUS) is clinically useful not only as a diagnostic tool during EUS-guided fine needle aspiration, but also during interventional EUS. EUS-guided biliary drainage has been developed and performed by experienced endoscopists. EUS-guided choledocoduodenostomy (EUS-CDS) is relatively well established as an alternative biliary drainage method for biliary decompression in patients with biliary obstruction. The reported technical success rate of EUS-CDS ranges from 50% to 100%, and the clinical success rate ranges from 92% to 100%. Further, the over-all technical success rate was 93%, and clinical success rate was 98%. Based on the currently available literature, the overall adverse event rate for EUS-CDS is 16%. The data on the cumulative technical and clinical success rate for EUS-CDS is promising. However, EUS-CDS can still lead to several problems, so techniques or devices that are more feasible and safe need to be established. EUS-CDS has the potential to become a first-line biliary drainage procedure, although standardizing the technique in multicenter clinical trials and comparisons with endoscopic biliary drainage by randomized clinical trials are still needed.
Core tip: Endoscopic ultrasound-guided choledocoduodenostomy (EUS-CDS) is relatively well established as an alternative biliary drainage method. The reported technical success rate of EUS-CDS ranges from 50% to 100%, and the clinical success rate ranges from 92% to 100%. Further, the over-all technical success rate was 93%, and clinical success rate was 98%. Based on the currently available literature, the overall adverse event rate for EUS-CDS is 16%. EUS-CDS may become the first choice of the biliary tract drainage procedure in the local cases such as poor prognosis, the contraindication of percutaneous transhepatic biliary drainage.
- Citation: Ogura T, Higuchi K. Technical tips of endoscopic ultrasound-guided choledochoduodenostomy. World J Gastroenterol 2015; 21(3): 820-828
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/820.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.820
Obstructive jaundice is a major adverse effect of pancreatic or biliary carcinoma. This adverse event requires treatment, especially in patients who cannot be treated surgically due to concurrent chemotherapy. Endoscopic biliary stenting (EBS) is a gold standard method of treatment for obstructive jaundice[1,2]. However, this method is associated with several problems, such as post-endoscopic retrograde cholangiopancreatography (ERCP) pancreatitis. In addition, EBS cannot be performed in patients with selective cannulation failure of the major papilla or an inaccessible papilla due to duodenal invasion. The alternative method under these conditions is percutaneous transhepatic biliary drainage (PTBD)[3,4]. However, PTBD can lead to several adverse events, such as cholangitis, bile leakage and pneumothorax. Moreover, the frequency of major complications, such as prolonged hospital stay and permanent adverse sequelae, is 4.6%-25%, and that of procedure-related deaths is 0%-5.6%[5,6]. Cosmetic issues due to external drainage also compromise the patient’s quality of life.
Endoscopic ultrasound (EUS) is clinically useful not only as a diagnostic tool during EUS-guided fine needle aspiration (FNA), but also during interventional EUS. Among the different types of interventional EUS, endoscopic ultrasound-guided biliary drainage (EUS-BD) has been developed and performed by experienced endoscopists. The technique of EUS-BD depends on the approach route. For transgastric EUS-BD, EUS-guided hepaticogastrostomy (EUS-HGS) is performed, in which the intrahepatic bile duct (usually segment 3; B3) is punctured via the stomach, and stent placement is performed from the intrahepatic bile duct to the stomach[7]. For transduodenal EUS-BD, EUS-guided choledochoduodenostomy (EUS-CDS) is performed, in which the common bile duct (CBD) is punctured, and stent placement is performed from the CBD to the duodenum. For transgastric or transduodenal EUS-BD, EUS-guided gallbladder drainage (EUS-GBD) is performed, in which the gallbladder is punctured and a stent is placed from the gallbladder to the stomach or duodenum[8]. In addition, the EUS-guided rendezvous technique (EUS-RV) is also included as EUS-BD[9].
While EUS-HGS and EUS-GBD have clinical benefits in certain patients, their use is associated with several adverse events, including stent migration. If stent migration does occur, it is sometimes fatal. Therefore, novel methods or new devices are required to prevent the complications associated with these procedures. EUS-RV is only indicated for patients in whom the ampulla of Vater is accessible by duodenoscopy. This procedure is sometimes difficult and requires a long procedure time[9].
On the other hand, EUS-CDS is relatively well established as an alternative biliary drainage method with a relatively low rate of adverse events, for biliary decompression in patients with biliary obstruction. However, EUS-CDS can still lead to several problems, so techniques or devices that are more feasible and safe need to be established.
Table 1 shows an overview of previous reports of EUS-CDS[10-45]. Herein, we present technical tips on the performance of EUS-CDS and review of the literature on EUS-CDS, especially its techniques and adverse events.
| Ref. | n | Disease (n) | Indications | Technical success | Clinical success | Puncture devise (n) | Dilation devise | Stents | Adverse events (n) |
| Giovannini et al[10] | 1 | Pancreatic carcinoma | Faild EBD | 1 (100) | 1 (100) | 5 Fr needle knife | 6.5 Fr dilataor | 10 Fr PS | None |
| Burmester et al[11] | 2 | Pancreatic carcinoma (2) | Faild EBD | 1 (50) | 1 (100) | 19 G fistulome | None | 8.5 Fr PS | Bile peritonitis (1) |
| Püspök et al[12] | 5 | N/D | Faild EBD | 4 (80) | 4 (100) | Needle knife, 19 G FNA needle | 8 mm balloon | 7-10 Fr PS | None |
| Kahaleh et al[13] | 1 | Pancreatic carcinoma | Faild EBD | 1 (100) | 1 (100) | 19 G FNA needle | N/D | 10 mm MS | Pneumoperitoneum (1) |
| Yamao et al[14] | 5 | Pancreatic carcinoma (3), ampulla carcinoma (2) | Faild EBD | 2 (100) | 2 (100) | Needle knife | 7 Fr, 9 Fr dilator | 7-8.5 Fr PS | Pneumoperitoneum (1) |
| Ang et al[16] | 2 | Pancreatic carcinoma (2) | Faild EBD | 2 (100) | 2 (100) | 19 G FNA needle | 7 Fr dilator | 7 Fr PS | Pneumoperitoneum (1) |
| Fujita et al[17] | 1 | Ampulla carcinoma | Faild EBD | 1 (100) | 1 (100) | 19 G FNA needle | Dilator | 7 Fr PS | None |
| Tarantino et al[18] | 4 | Pancreatic carcinoma (2), cholangiocarcinoma (1), malignant lymphoma (1) | Faild EBD | 4 (100) | 4 (100) | 19 G, 22 G FNA needle, needle knife | 4 mm balloon | PS | None |
| Itoi et al[19] | 4 | Pancreatic carcinoma (2), ampulla carcinoma (2) | Faild EBD | 4 (100) | 4 (100) | Needle knife, 19 G FNA needle | 7 Fr, 9 Fr dilator, balloon | 7 Fr PS (3), NBD (1) | Bleeding (1), peritonitis (1) |
| Brauer et al[20] | 3 | Pancreatic carcinoma (1), gastric carcinoma (1), choledocholithiasis (1) | Faild EBD | 3 (100) | 3 (100) | 19 G FNA needle, needle knife | N/D | 5 Fr, 10 Fr PS | Cardicac and respiratory failure (1), pneumoperitoneum (1) |
| Horaguchi et al[21] | 8 | Pancreatic carcinoma (5), ampulla carcinoma (1), choledocholithiasis (1), Lymph note metastasis (1) | Faild EBD | 8 (100) | 8 (100) | 19 G FNA needle | 5 Fr dilator, 4 mm balloon | 7 Fr PS (7), NBD (1) | Peritonitis (1) |
| Hanada et al[22] | 4 | Pancreatic carcinoma (4) | Faild EBD | 4 (100) | 4 (100) | 19 G FNA needle | 6 Fr, 7 Fr dilator | 6 Fr, 7 Fr PS | None |
| Iwamuro et al[23] | 5 | Pancreatic carcinoma (4), ampulla carcinoma (1) | Duodenal obstruction | 5 (100) | 5 (100) | Needle knife | 7 Fr dilator | 7 Fr PS | Abdominal pain, fever (1) |
| Artifon et al[24] | 3 | Pancreatic carcinoma (3), ampulla carcinoma (2) | Faild EBD (2), | 3 (100) | 3 (100) | 19 G FNA needle | Needle knife | 10 mm MS | None |
| duodenal invasion (1) | |||||||||
| Belletrutii et al[25] | 1 | Pancreatic carcinoma | Faild EBD | 1 (100) | 1 (100) | 19 G FNA needle | 6 mm balloon | 10 mm MS | None |
| Hara et al[26] | 18 | Pancreatic carcinoma (15), uterus carcinoma (1), gastric carcinoma (1), | Lower biliary obstruction | 17 (94) | 17 (100) | 22G FNA needle, needle knife | 6, 7, 9 Fr dilator | 7, 8.5 Fr PS | Bile peritonitis (2), hemobilia (1) |
| gallbladder carcinoma (1) | |||||||||
| Siddiqu et al[27] | 8 | Pancreatic carcinoma (6), cholangiocarcinoma (2) | Faild EBD | 8 (100) | 8 (100) | 19 G FNA needle | Needle knife | 10 mm MS | Stent migration/duodenal perforation (1), abdominal pain (1) |
| Fabbri et al[28] | 12 | Pancreatic carcinoma (7), cholangiocarcinoma (4), ampulla carcinoma (1), | Faild EBD | 9 (75) | 9 (100) | 19 G FNA needle, needle knife | 4 mm balloon | MS | Pneumoperitoneum (1) |
| gallbladder carcinoma (1) | |||||||||
| Komaki et al[29] | 15 | Unresectable malignant biliary obstruction | Faild EBD | 14 (93) | 14 (100) | 19 G FNA needle | Dilator | 7 Fr PS | None |
| Prachayakul et al[30] | 1 | Pancreatic carcinoma | Duodenal obstruction | 1 (100) | 1 (100) | N/D | Dilator | PS | None |
| Ramírez-Luna et al[31] | 9 | Pancreatic carcinoma (4), cholangiocarcinoma (2), metastases (1), | Faild EBD | 8 (89) | 8 (100) | 19 G FNA needle | Needle knife, 6, 7, 10 Fr dilator | 7, 8, 10 Fr PS | Biloma (1) |
| ampulla carcinoma (1), neuroendocrine (1) | |||||||||
| Park do et al[32] | 26 | N/D | Faild EBD | 24 (92) | 22 (92.9) | 19 G FNA needle | 4 Fr ERCP cannula, 6, 7 Fr dilator, needle knife | PS, MS | Bile peritonitis (2), unknown (3) |
| Artifon et al[33] | 13 | Unresectable malignant biliary obstruction | Faild EBD | 13 (100) | 13 (100) | 19 G FNA needle | Needle knife | 10 mm MS | Biloma (1), bleeding (1) |
| Attasaranya et al[34] | 9 | N/D | Faild EBD | 5 (56) | N/D | 19 G FNA needle | ERCP catheter, 6, 7 Fr dilator, 8 mm balloon, needle knife | N/D | Unknown (4) |
| Katanuma et al[35] | 1 | Chronic pancreatitis | Relapsing cholangitis, | 1 (100) | 1 (100) | 19 G FNA needle | Needle knife, dilator | 7 Fr PS | None |
| duodena stenosis | |||||||||
| kawakubo et al[36] | 2 | Pancreatic carcinoma (2) | Duodenal obstruction | 2 (100) | 2 (100) | 19 G FNA needle | 7 Fr dilator, 4 mm balloon | 7 Fr PS | None |
| Khashab et al[37] | 2 | Pancreatic carcinoma (2) | Duodenal obstruction | 2 (100) | 2 (100) | 19 G FNA needle | Needle knife, 7 Fr dilator | 10 mm MS | None |
| Kim et al[38] | 9 | Pancreatic carcinoma (5), cholangiocarcinoma (4) | Faild EBD | 9 (100) | 9 (100) | 19 G FNA needle | ERCP catheter, cystostome, needle knife, dilator | 10 mm MS | Bile peritonitis (1) |
| Song et al[39] | 15 | Pancreatic carcinoma (9), ampulla carcinoma (2), renal cell carcinoma (1), | Faild EBD | 13 (87) | 13 (100) | 19 G FNA needle | 6, 7 Fr dilator, needle knife | 8, 10 mm MS | Pneumoperitoneum (2), cholngitis (1) |
| lymphoma (1), gastric carcinoma (1), duodenal carcinoma (1) | |||||||||
| Vila et al[40] | 26 | Malignant (22), benign (4) | NA | 19 (86) | NA | NA | NA | NA | Biloma (1), bleeding (1), |
| pancreatitis (1), | |||||||||
| cholangitis (1) | |||||||||
| Maluf-Filho et al[41] | 5 | Pancreatic carcinoma (3), colonic carcinoma (1), cervix carcinoma (1) | Duodenal obstruction | 3 (60) | 5 (100) | 19 G FNA needle | Diathermic sheath | 10 mm MS | Biliary fistula (1), |
| cardiogenic shock (1) | |||||||||
| Itoi et al[42] | 1 | Pancreatic carcinoma (1) | Duodenal obstruction | 1 (100) | 1 (100) | 19 G FNA needle | ERCP catheter, 4 mm balloon | 10 mm MS | None |
| Tonozuka et al[43] | 4 | Pancreatic carcinoma (4) | Duodenal obstruction | 4 (100) | 4 (100) | 19 G FNA needle | Dilator, balloon, diathermic sheath | MS | None |
| Hara et al[44] | 18 | Pancreatic carcinoma (17), ampulla carcinoma (1) | Lower biliary obstruction | 17 (94) | 17 (100) | 22G FNA needle, needle knife | 6, 7, 9 Fr dilator | 10 mm MS, 8.5 Fr PS | Peritonitis (2) |
| Khashab et al[45] | 20 | Malignant (15) | NA | 20 (100) | 19 (95) | 19 G FNA needle | Dilator, balloon | PS, MS | NA |
| Kawakubo et al[46] | 44 | Pancreatic carcinoma (31), ampullary carcinoma (8), cholangiocarcinoma (2), metastatic lymph nodes (3) | Periampullary tumor invasion, failed EBS | 42 (95) | NA | 19 G FNA needle, needle knife | Dilator, balloon | PS, MS | Bile leak (3), stent misplacement (1), bleeding (1), pneumoperitoneum (1), perforation (1) |
EUS-CDS is mainly performed for patients with failed EBS excluded prospective clinical trial, as was previously described by Hara et al[26] and Itoi et al[42]. This procedure can be performed for obstructions in the middle and lower bile duct.
The primary diseases in patients who underwent EUS-CDS were pancreatic carcinoma (n = 98), ampullary carcinoma (n = 14), and cholangiocarcinoma (n = 13). This indicates that pancreato-biliary carcinoma is the main indication for EUS-CDS. On the other hand, EUS-CDS for benign biliary stricture was only performed in 2 patients, as previously reported.
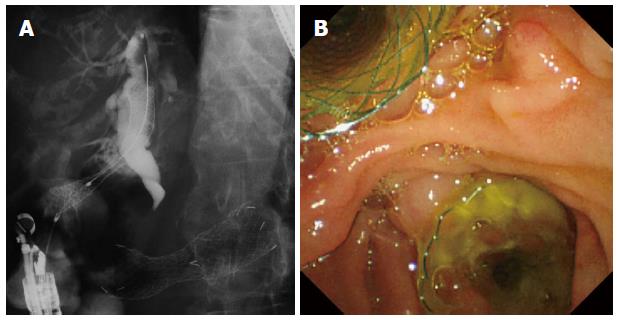
EUS-CDS is contraindicated in patients with surgically altered anatomy, such as a Roux-en-Y anastomosis or duodenal obstruction caused by tumor invasion, through which an endoscope cannot be passed. In such cases, EUS-guided hepaticogastrostomy may be indicated. However, if the duodenal bulb is not involved, EUS-CDS can be performed in combination with duodenal stenting (Figure 1).
The indications for EUS-CDS vs ERCP for benign disease are still not completely known. Therefore, prospective randomized controlled trials comparing EUS-CDS with ERCP are needed to assess the clinical efficacy of the procedure.
Hence, the following are the indications for EUS-CDS: (1) failed EBS; (2) inaccessibility of the ampulla of Vater, such as due to duodenal invasion by the tumor; (3) contraindications for percutaneous transhepatic biliary drainage (PTBD); and (4) middle or lower bile duct obstruction.
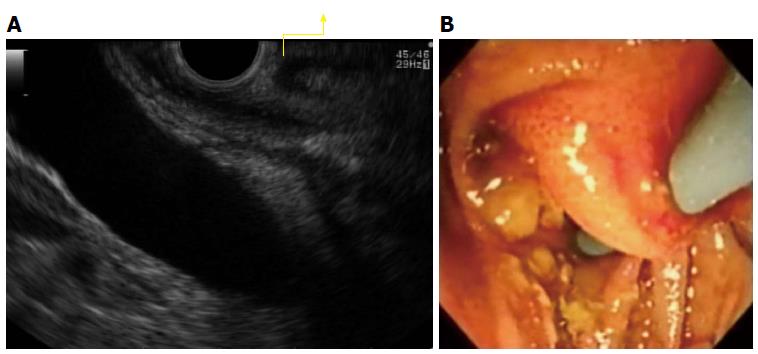
To visualize the CBD on EUS, the EUS scope is advanced into the duodenum, turned slightly to the left and angled downwards. The CBD is punctured using a 19-G needle under Doppler visualization, to avoid any intervening vessels. Bile juice is aspirated and a small amount of contrast medium is injected. During this step, it is important to avoid puncturing the duodenal mucosa and cystic duct. As shown in Figure 2, when a double duodenal mucosal line is visualized on EUS, the CBD should not be punctured to avoid puncture and stenting through double duodenal mucosa.
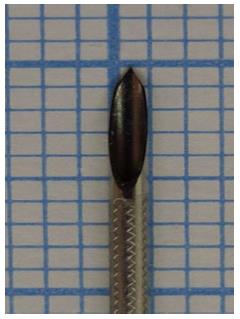
According to previous reports, a 19G or 22G FNA needle or needle knife is used to puncture the CBD. As of now, there are no randomized controlled trials comparing the outcomes of various FNA needles in EUS-CDS. Recently, a novel FNA needle (Sono Tip Pro Control 19G needle, Medi-Globe GmbH, Rosenheim, Germany) (Figure 3) has become available. The cut surface of this FNA needle is 5 mm long, and is believed to be extremely sharp. Therefore, we think this needle is appropriate for use in interventional EUS.
After the contrast is injected into the CBD, the guidewire is placed deep in the intrahepatic bile duct. On EUS imaging, when the CBD is aligned parallel to the FNA needle, the guidewire can be easily advanced toward the hepatic hilum.
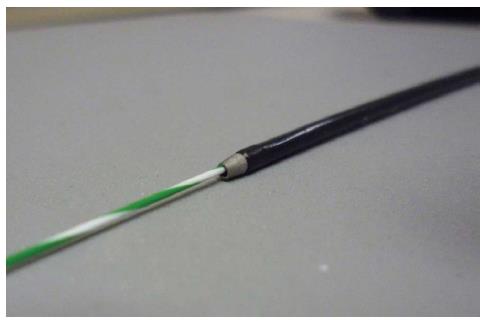
To enable passage of a 0.035 inch stiff guidewire into the needle, a 19-gauge needle should be selected. A 0.025 inch guidewire with a highly flexible tip, sufficient stiffness, and easily seeking ability (VisiGlide; Olympus Medical Systems, Tokyo, Japan) is preferable. To avoid wire sharing, a novel guidewire which top formation is coil (Cyst-wire, Medi-Globe) (Figure 4) is also useful.
When the guidewire is inserted along with other devices, it is important to be able to view the devices under both EUS and fluoroscopic guidance, to ensure that they fit the axis.
Various devices have been previously described for dilatation of the fistula after puncturing the CBD. The most common devices for transmural tract dilation are the dilator (6 to 10 Fr; Soehendra biliary dilation catheters, Cook Medical), balloon catheter (4-8 mm; MaxForce or Hurricane RX; Boston Scientific), or needle knife (Microtome, Boston Scientific). Park reported that the overall adverse event rate of EUS-BD, including EUS-CDS and EUS-HGS, was 27% (15/55)[32]. They also described the use of a needle knife for fistula dilation as the single risk factor for adverse procedural events after EUS-BD (P = 0.01, HR = 12.4, 95%CI: 1.83-83.5). Due to the acute angulation of the EUS scope, following deployment of the catheter at the duodenal bulb, the needle knife, when deployed, points tangentially, which can lead to accidental incision with a chance of pneumoperitoneum or bleeding. Therefore, they concluded that fistula dilation should be avoided if possible.
However, it is true that fistula dilation is easier if a needle knife is used. Recently, a diathermic dilator (Cysto Gastro Set; Endoflex, GmbH, Voerde, Germany) has become available. This device is always coaxial with the guidewire (Figure 5). Hence, its use for fistula dilation may reduce the incidence of EUS-BD-related adverse events compared with those using a needle knife. Studies comparing these devices are, therefore, warranted.
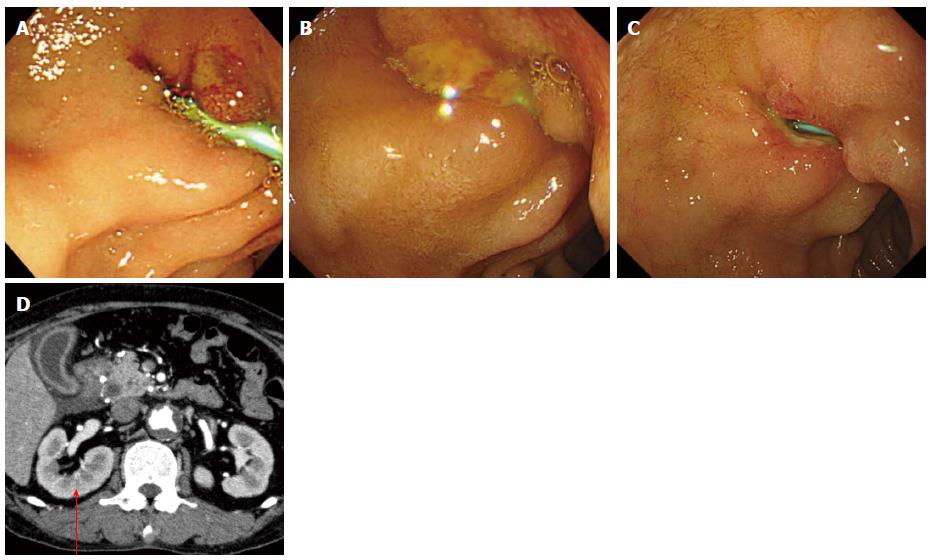
Both plastic and metallic stents have been used during EUS-CDS. Previously, plastic stents with diameters ranging from 5 to 10 Fr were used. Generally, because the diameter of the working channel of the EUS is 3.7 mm, a 7 or 8.5 Fr plastic stent is used. However, as shown in Figure 6, bile leak can occur with plastic stent placement. This patient had abdominal pain and fever for up to 3 d after EUS-CDS, and computed tomography and duodenoscopy showed bile leakage. If a large fistula is created during stent placement, bile leakage from the gap between the stent and the fistula is likely to occur because of the fine gauge of the plastic stent.
On the other hand, although no comparative studies exist, metallic stents are expected to offer several clinical benefits. First, because of their large diameter, metallic stents have a longer patency than plastic stents. Second, due to the close proximity between the metallic stent and the duodenal wall and bile duct, bile leak is less likely to occur. Use of an uncovered metallic stent, however, can easily cause bile leakage, which is sometimes fatal[43]. Therefore, partially or fully covered self-expandable metal stents (SEMS) should be selected. However, although these SEMS have the advantage of preventing bile leakage, they also have the disadvantage of causing occlusion of the side branch of the bile duct. This suggests that if the distance between the site of the puncture and the hepatic hilar portion is short, a partially covered SEMS should be selected to prevent occlusion of the intrahepatic bile duct. Unfortunately, when a partially covered SEMS is used, bile leak can occur from the uncovered part, particularly between the bile duct and the gastrointestinal tract.
Stent migration is also usually a challenging complication of EUS-BD. With the use of the standard metallic stent, some authors described that a double pigtail plastic stent can be placed inside the metal stent, with the pigtail functioning as an anchor[47]. Among standard metallic stents, metallic stents with a wide flange should be selected, and stent shortening to a length of 60 mm may be preferable in order to avoid stent migration.
Recently, a novel SEMS has been developed. The NAGI-Stent (Taewoong-Medical Co., Seoul, South Korea) is delivered through a 10.5 Fr catheter, and consists of a fully covered 20 mm long and 16 mm diameter stent with bilateral anchor flanges. The AXIOS stent (Xlumena Inc., Mountain View, CA, United States) is a fully covered, 10 mm diameter, 10 mm long, braided stent with bilateral 20 mm diameter anchor flanges. These novel SEMSs are used for EUS-guided pseudocystic drainage and EUS-guided cholecystogastrostomy[48-50]. This SEMS seems to be useful for EUS-CDS as well, although clinical trials are needed to confirm its utility.
According to previous reports, the mean stent patency in EUS-CDS was similar to PTBD (198 d vs 184 d, P = 0.86)[51]. Although there were no reports of comparison between EUS-CDS and EBS, stent patency of EBS (covered metallic stent; 585 d, uncovered metallic stent; 314 d) may be longer than EUS-CDS according to previously described report[52]. Randomized clinical trials are needed with standardizing kinds of biliary stents.
The reported technical success rate of EUS-CDS ranges from 50% to 100%, and the clinical success rate ranges from 92% to 100%. Further, the over-all technical success rate was 93% (199/213), and clinical success rate was 98% (183/187). This is a relatively high success rate compared with ERCP. Therefore, if EUS-CDS is associated with a low rate of adverse events and long stent patency, it has the potential to be the bile drainage method of choice instead of EBS. A prospective randomized clinical trial is needed to compare endoscopic biliary drainage and EUS-CDS.
Based on the currently available literature, the overall adverse event rate for EUS-CDS is 16% (34/213). EUS-CDS has the potential to cause several adverse events, including: (1) infection (peritonitis, cholangitis, cholecystitis); (2) pneumoperitoneum; (3) bile leakage, biloma; (4) bleeding; (5) abdominal pain; (6) perforation; and (7) stent migration.
Based on previous reports, the most frequent adverse events were pneumoperitoneum (28%, 9/34). In most EUS-CDS cases, if adverse events do occur, they can be treated conservatively. However, two deaths related to EUS-CDS, due to cardiogenic shock and bile leakage, were also reported by Maluf-Filho et al[41]. In both these patients, the bile leak occurred because of use of an uncovered SEMS. However, even if a fully covered SEMS is selected, the risk of bile peritonitis still remains. This adverse event may occur because of bile or air leak during dilation of the fistula while inserting the stent delivery system. Therefore, to avoid these adverse events, more developed devices that would enable one-step stent placement (without dilation of the fistula) are strongly needed. To avoid bleeding, use of color Doppler ultrasound to detect vascular structures can decrease the risk of bleeding.
SEM stents should be selected during EUS-CDS to avoid several adverse events, although the possibility of stent migration still remains. The data on the cumulative technical and clinical success rate for EUS-CDS is promising. EUS-CDS may become the first choice of the biliary tract drainage procedure in the local cases such as poor prognosis, the contraindication of PTBD.
| 1. | Fogel EL, Sherman S, Devereaux BM, Lehman GA. Therapeutic biliary endoscopy. Endoscopy. 2001;33:31-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 2. | Williams EJ, Taylor S, Fairclough P, Hamlyn A, Logan RF, Martin D, Riley SA, Veitch P, Wilkinson M, Williamson PJ. Are we meeting the standards set for endoscopy? Results of a large-scale prospective survey of endoscopic retrograde cholangio-pancreatograph practice. Gut. 2007;56:821-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 183] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 3. | Oh HC, Lee SK, Lee TY, Kwon S, Lee SS, Seo DW, Kim MH. Analysis of percutaneous transhepatic cholangioscopy-related complications and the risk factors for those complications. Endoscopy. 2007;39:731-736. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 112] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 4. | Winick AB, Waybill PN, Venbrux AC. Complications of percutaneous transhepatic biliary interventions. Tech Vasc Interv Radiol. 2001;4:200-206. [PubMed] |
| 5. | Carrasco CH, Zornoza J, Bechtel WJ. Malignant biliary obstruction: complications of percutaneous biliary drainage. Radiology. 1984;152:343-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 83] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Günther RW, Schild H, Thelen M. Percutaneous transhepatic biliary drainage: experience with 311 procedures. Cardiovasc Intervent Radiol. 1988;11:65-71. [PubMed] |
| 7. | Giovannini M, Dotti M, Bories E, Moutardier V, Pesenti C, Danisi C, Delpero JR. Hepaticogastrostomy by echo-endoscopy as a palliative treatment in a patient with metastatic biliary obstruction. Endoscopy. 2003;35:1076-1078. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 108] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 8. | Itoi T, Itokawa F, Kurihara T. Endoscopic ultrasonography-guided gallbladder drainage: actual technical presentations and review of the literature (with videos). J Hepatobiliary Pancreat Sci. 2011;18:282-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 46] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 9. | Kim YS, Gupta K, Mallery S, Li R, Kinney T, Freeman ML. Endoscopic ultrasound rendezvous for bile duct access using a transduodenal approach: cumulative experience at a single center. A case series. Endoscopy. 2010;42:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 10. | Giovannini M, Moutardier V, Pesenti C, Bories E, Lelong B, Delpero JR. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001;33:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 446] [Cited by in RCA: 489] [Article Influence: 19.6] [Reference Citation Analysis (0)] |
| 11. | Burmester E, Niehaus J, Leineweber T, Huetteroth T. EUS-cholangio-drainage of the bile duct: report of 4 cases. Gastrointest Endosc. 2003;57:246-251. [PubMed] |
| 12. | Püspök A, Lomoschitz F, Dejaco C, Hejna M, Sautner T, Gangl A. Endoscopic ultrasound guided therapy of benign and malignant biliary obstruction: a case series. Am J Gastroenterol. 2005;100:1743-1747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 13. | Kahaleh M, Hernandez AJ, Tokar J, Adams RB, Shami VM, Yeaton P. Interventional EUS-guided cholangiography: evaluation of a technique in evolution. Gastrointest Endosc. 2006;64:52-59. [PubMed] |
| 14. | Yamao K, Sawaki A, Takahashi K, Imaoka H, Ashida R, Mizuno N. EUS-guided choledochoduodenostomy for palliative biliary drainage in case of papillary obstruction: report of 2 cases. Gastrointest Endosc. 2006;64:663-667. [PubMed] |
| 15. | Yamao K, Bhatia V, Mizuno N, Sawaki A, Ishikawa H, Tajika M, Hoki N, Shimizu Y, Ashida R, Fukami N. EUS-guided choledochoduodenostomy for palliative biliary drainage in patients with malignant biliary obstruction: results of long-term follow-up. Endoscopy. 2008;40:340-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 101] [Article Influence: 5.6] [Reference Citation Analysis (2)] |
| 16. | Ang TL, Teo EK, Fock KM. EUS-guided transduodenal biliary drainage in unresectable pancreatic cancer with obstructive jaundice. JOP. 2007;8:438-443. [PubMed] |
| 17. | Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Horaguchi J, Takasawa O, Nakahara K. Histological changes at an endosonography-guided biliary drainage site: a case report. World J Gastroenterol. 2007;13:5512-5515. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 48] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Tarantino I, Barresi L, Repici A, Traina M. EUS-guided biliary drainage: a case series. Endoscopy. 2008;40:336-339. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (2)] |
| 19. | Itoi T, Itokawa F, Sofuni A, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N, Moriyasu F. Endoscopic ultrasound-guided choledochoduodenostomy in patients with failed endoscopic retrograde cholangiopancreatography. World J Gastroenterol. 2008;14:6078-6082. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 86] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (3)] |
| 20. | Brauer BC, Chen YK, Fukami N, Shah RJ. Single-operator EUS-guided cholangiopancreatography for difficult pancreaticobiliary access (with video). Gastrointest Endosc. 2009;70:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 21. | Horaguchi J, Fujita N, Noda Y, Kobayashi G, Ito K, Obana T, Takasawa O, Koshita S, Kanno Y. Endosonography-guided biliary drainage in cases with difficult transpapillary endoscopic biliary drainage. Dig Endosc. 2009;21:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 22. | Hanada K, Iiboshi T, Ishii Y. Endoscopic ultrasound-guided choledochoduodenostomy for palliative biliary drainage in cases with inoperable pancreas head carcinoma. Dig Endosc. 2009;21 Suppl 1:S75-S78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 38] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 23. | Iwamuro M, Kawamoto H, Harada R, Kato H, Hirao K, Mizuno O, Ishida E, Ogawa T, Okada H, Yamamoto K. Combined duodenal stent placement and endoscopic ultrasonography-guided biliary drainage for malignant duodenal obstruction with biliary stricture. Dig Endosc. 2010;22:236-240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 42] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Artifon EL, Takada J, Okawa L, Moura EG, Sakai P. EUS-guided choledochoduodenostomy for biliary drainage in unresectable pancreatic cancer: a case series. JOP. 2010;11:597-600. [PubMed] |
| 25. | Belletrutti PJ, Gerdes H, Schattner MA. Successful endoscopic ultrasound-guided transduodenal biliary drainage through a pre-existing duodenal stent. JOP. 2010;11:234-236. [PubMed] |
| 26. | Hara K, Yamao K, Niwa Y, Sawaki A, Mizuno N, Hijioka S, Tajika M, Kawai H, Kondo S, Kobayashi Y. Prospective clinical study of EUS-guided choledochoduodenostomy for malignant lower biliary tract obstruction. Am J Gastroenterol. 2011;106:1239-1245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 127] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 27. | Siddiqui AA, Sreenarasimhaiah J, Lara LF, Harford W, Lee C, Eloubeidi MA. Endoscopic ultrasound-guided transduodenal placement of a fully covered metal stent for palliative biliary drainage in patients with malignant biliary obstruction. Surg Endosc. 2011;25:549-555. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 50] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 28. | Fabbri C, Luigiano C, Fuccio L, Polifemo AM, Ferrara F, Ghersi S, Bassi M, Billi P, Maimone A, Cennamo V. EUS-guided biliary drainage with placement of a new partially covered biliary stent for palliation of malignant biliary obstruction: a case series. Endoscopy. 2011;43:438-441. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 52] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 29. | Komaki T, Kitano M, Sakamoto H, Kudo M. Endoscopic ultrasonography-guided biliary drainage: evaluation of a choledochoduodenostomy technique. Pancreatology. 2011;11 Suppl 2:47-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 30. | Prachayakul V, Aswakul P, Kachintorn U. EUS-guided choledochoduodenostomy for biliary drainage using tapered-tip plastic stent with multiple fangs. Endoscopy. 2011;43 Suppl 2 UCTN:E109-E110. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 31. | Ramírez-Luna MA, Téllez-Ávila FI, Giovannini M, Valdovinos-Andraca F, Guerrero-Hernández I, Herrera-Esquivel J. Endoscopic ultrasound-guided biliodigestive drainage is a good alternative in patients with unresectable cancer. Endoscopy. 2011;43:826-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 32. | Park do H, Jang JW, Lee SS, Seo DW, Lee SK, Kim MH. EUS-guided biliary drainage with transluminal stenting after failed ERCP: predictors of adverse events and long-term results. Gastrointest Endosc. 2011;74:1276-1284. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 248] [Article Influence: 16.5] [Reference Citation Analysis (0)] |
| 33. | Artifon EL, Aparicio D, Paione JB, Lo SK, Bordini A, Rabello C, Otoch JP, Gupta K. Biliary drainage in patients with unresectable, malignant obstruction where ERCP fails: endoscopic ultrasonography-guided choledochoduodenostomy versus percutaneous drainage. J Clin Gastroenterol. 2012;46:768-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 153] [Cited by in RCA: 180] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 34. | Attasaranya S, Netinasunton N, Jongboonyanuparp T, Sottisuporn J, Witeerungrot T, Pirathvisuth T, Ovartlarnporn B. The Spectrum of Endoscopic Ultrasound Intervention in Biliary Diseases: A Single Center’s Experience in 31 Cases. Gastroenterol Res Pract. 2012;2012:680753. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 35. | Katanuma A, Maguchi H, Osanai M, Takahashi K. Endoscopic ultrasound-guided biliary drainage performed for refractory bile duct stenosis due to chronic pancreatitis: a case report. Dig Endosc. 2012;24 Suppl 1:34-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 36. | Kawakubo K, Isayama H, Nakai Y, Sasahira N, Kogure H, Sasaki T, Hirano K, Tada M, Koike K. Simultaneous Duodenal Metal Stent Placement and EUS-Guided Choledochoduodenostomy for Unresectable Pancreatic Cancer. Gut Liver. 2012;6:399-402. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 37. | Khashab MA, Fujii LL, Baron TH, Canto MI, Gostout CJ, Petersen BT, Okolo PI, Topazian MD, Levy MJ. EUS-guided biliary drainage for patients with malignant biliary obstruction with an indwelling duodenal stent (with videos). Gastrointest Endosc. 2012;76:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 38. | Kim TH, Kim SH, Oh HJ, Sohn YW, Lee SO. Endoscopic ultrasound-guided biliary drainage with placement of a fully covered metal stent for malignant biliary obstruction. World J Gastroenterol. 2012;18:2526-2532. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 44] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 39. | Song TJ, Hyun YS, Lee SS, Park do H, Seo DW, Lee SK, Kim MH. Endoscopic ultrasound-guided choledochoduodenostomies with fully covered self-expandable metallic stents. World J Gastroenterol. 2012;18:4435-4440. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 46] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 40. | Vila JJ, Pérez-Miranda M, Vazquez-Sequeiros E, Abadia MA, Pérez-Millán A, González-Huix F, Gornals J, Iglesias-Garcia J, De la Serna C, Aparicio JR. Initial experience with EUS-guided cholangiopancreatography for biliary and pancreatic duct drainage: a Spanish national survey. Gastrointest Endosc. 2012;76:1133-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 164] [Cited by in RCA: 208] [Article Influence: 14.9] [Reference Citation Analysis (0)] |
| 41. | Maluf-Filho F, Retes FA, Neves CZ, Sato CF, Kawaguti FS, Jureidini R, Ribeiro U, Bacchella T. Transduodenal endosonography-guided biliary drainage and duodenal stenting for palliation of malignant obstructive jaundice and duodenal obstruction. JOP. 2012;13:210-214. [PubMed] |
| 42. | Itoi T, Itokawa F, Tsuchiya T, Tsuji S, Tonozuka R. Endoscopic ultrasound-guided choledochoantrostomy as an alternative extrahepatic bile duct drainage method in pancreatic cancer with duodenal invasion. Dig Endosc. 2013;25 Suppl 2:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 43. | Tonozuka R, Itoi T, Sofuni A, Itokawa F, Moriyasu F. Endoscopic double stenting for the treatment of malignant biliary and duodenal obstruction due to pancreatic cancer. Dig Endosc. 2013;25 Suppl 2:100-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 44. | Hara K, Yamao K, Hijioka S, Mizuno N, Imaoka H, Tajika M, Kondo S, Tanaka T, Haba S, Takeshi O. Prospective clinical study of endoscopic ultrasound-guided choledochoduodenostomy with direct metallic stent placement using a forward-viewing echoendoscope. Endoscopy. 2013;45:392-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 94] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 45. | Khashab MA, Valeshabad AK, Modayil R, Widmer J, Saxena P, Idrees M, Iqbal S, Kalloo AN, Stavropoulos SN. EUS-guided biliary drainage by using a standardized approach for malignant biliary obstruction: rendezvous versus direct transluminal techniques (with videos). Gastrointest Endosc. 2013;78:734-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 103] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 46. | Kawakubo K, Isayama H, Kato H, Itoi T, Kawakami H, Hanada K, Ishiwatari H, Yasuda I, Kawamoto H, Itokawa F. Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci. 2014;21:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 189] [Cited by in RCA: 177] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 47. | Sarkaria S, Lee HS, Gaidhane M, Kahaleh M. Advances in endoscopic ultrasound-guided biliary drainage: a comprehensive review. Gut Liver. 2013;7:129-136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 48. | Itoi T, Binmoeller KF, Shah J, Sofuni A, Itokawa F, Kurihara T, Tsuchiya T, Ishii K, Tsuji S, Ikeuchi N. Clinical evaluation of a novel lumen-apposing metal stent for endosonography-guided pancreatic pseudocyst and gallbladder drainage (with videos). Gastrointest Endosc. 2012;75:870-876. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 299] [Cited by in RCA: 320] [Article Influence: 22.9] [Reference Citation Analysis (0)] |
| 49. | Itoi T, Nageshwar Reddy D, Yasuda I. New fully-covered self-expandable metal stent for endoscopic ultrasonography-guided intervention in infectious walled-off pancreatic necrosis (with video). J Hepatobiliary Pancreat Sci. 2013;20:403-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 56] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 50. | Binmoeller KF, Shah J. A novel lumen-apposing stent for transluminal drainage of nonadherent extraintestinal fluid collections. Endoscopy. 2011;43:337-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 172] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 51. | Khashab MA, Valeshabad AK, Afghani E, Singh VK, Kumbhari V, Messallam A, Saxena P, El Zein M, Lennon AM, Canto MI. A Comparative Evaluation of EUS-Guided Biliary Drainage and Percutaneous Drainage in Patients with Distal Malignant Biliary Obstruction and Failed ERCP. Dig Dis Sci. 2014;Epub ahead of print. [PubMed] |
| 52. | Kitano M, Yamashita Y, Tanaka K, Konishi H, Yazumi S, Nakai Y, Nishiyama O, Uehara H, Mitoro A, Sanuki T. Covered self-expandable metal stents with an anti-migration system improve patency duration without increased complications compared with uncovered stents for distal biliary obstruction caused by pancreatic carcinoma: a randomized multicenter trial. Am J Gastroenterol. 2013;108:1713-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 177] [Article Influence: 13.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Matsumoto K, Mentes O, Tsai HH S- Editor: Gou SX L- Editor: A E- Editor: Liu XM