Published online Jan 21, 2015. doi: 10.3748/wjg.v21.i3.815
Peer-review started: July 29, 2014
First decision: August 15, 2014
Revised: August 29, 2014
Accepted: October 15, 2014
Article in press: October 15, 2014
Published online: January 21, 2015
Processing time: 175 Days and 21.9 Hours
The association of gastroesophageal reflux disease (GERD) and esophageal cancer is well known. The carcinogenic properties of the gastroduodenal contents may also lead to cancer in target organs for GERD especially considering that they do not have intrinsic protective mechanisms as found in the esophagus. This review focuses on the putative relation between GERD and non-esophageal cancer. Most of the papers reviewed are far from ideal to prove the relationship of extra-esophageal cancer and GERD since a small number of patients is presented, most do not control cases based on tobacco usage and obesity, and the diagnosis of GERD is variable, not always from an objective measurement such as pH monitoring but relying on symptoms in most reports. Nevertheless, head and neck and lung cancer have a growing incidence parallel to GERD and a shift towards non-smoking, female gender and adenocarcinoma (compared to squamous cell carcinoma) is arising, similar to the example of esophageal cancer with the exception of the female gender.
Core tip: Gastroesophageal reflux disease (GERD) is a very prevalent disease with a rising incidence. The disease is certainly linked to the pathogenesis of esophageal adenocarcinoma originated in the Barrett’s esophagus. The carcinogenic properties of the gastroduodenal contents may also lead to cancer in target organs for GERD, especially considering that they do not have intrinsic protective mechanisms as found in the esophagus. Although strong conclusions cannot be drawn due to lack of good quality published studies, GERD may also be linked to the pathogenesis of head and neck and lung cancers.
- Citation: Herbella FA, Neto SP, Santoro IL, Figueiredo LC. Gastroesophageal reflux disease and non-esophageal cancer. World J Gastroenterol 2015; 21(3): 815-819
- URL: https://www.wjgnet.com/1007-9327/full/v21/i3/815.htm
- DOI: https://dx.doi.org/10.3748/wjg.v21.i3.815
Gastroesophageal reflux disease (GERD) is a very prevalent disease, affecting 18%-27% of the population in North America, 9%-25% in Europe, 2%-8% in East Asia, 9%-33% in the Middle East, 11% in Australia and 23% in South America[1]. Moreover, the incidence of GERD seems to be increasing with time[2]. It accounts for almost 9000000 outpatient visits, 65000 hospitalizations and costs of over US $9000000000 per year only in the United States[3,4]. The association of GERD and esophageal cancer is well known, with a metaplasia-dysplasia-carcinoma sequence leading ultimately to esophageal adenocarcinoma[5]. Esophageal adenocarcinoma also showed a significant increase in incidence in the last decades[6].
Virtually all adjacent organs to the esophagus may be affected by the gastric refluxate and new discoveries are made on a regular basis showing that even distant organs may be affected by GERD. It seems logical that the carcinogenic properties of the gastroduodenal contents may also lead to cancer in target organs for GERD especially considering that they do not have intrinsic protective mechanisms as found in the esophagus.
This review focuses on the putative relation between GERD and non-esophageal cancer.
Esophageal adenocarcinoma originated in a Barrett’s esophagus is the most studied cancer linked to GERD; however, its cellular origins and molecular mechanisms are still not fully understood[7]. GERD induces esophageal inflammation and consequent oxidative stress leading to DNA damage. Both acid and bile are active on oncogenic pathways. Acid induces DNA damage, decreases proliferation, and increases apoptosis. Bile salts induce DNA damage, affect proliferation in a pH-dependent manner, and cause resistance to apoptosis[7,8]. More detailed molecular mechanisms are available in recent reviews[7-9].
Apart from the direct effect of gastric refluxate, other variables link GERD and cancer. Obesity is a risk factor for different cancers, including esophageal adenocarcinoma[10]. Fat tissue increases the release of proinflammatory molecules and induces insulin resistance, all of them linked to carcinogenesis[7,11]. GERD is strongly associated to obesity as well[12]. It has been shown that for each 5-point increase in body mass index, the DeMeester GERD score increases by 3 units[13]. Parallel to GERD, the prevalence of obesity more than doubled between 1980 and 2009 in the United States, as indicated by Centers for Disease Control and Prevention Surveys.
Smoking is also linked to esophageal[14], head and neck[15] and lung cancer[16] and, again, is a risk factor for GERD[17].
Gastric contents reach the larynx/pharynx in healthy volunteers and in patients with GERD[18]. This has been proven by different methods, such as dual probe pH monitoring[18], multichannel intraluminal impedance[19], and aerosolized reflux detection[20]. In fact, refluxate may reach up to the mouth and GERD is thought to cause tooth wearing[21].
GERD has long been considered a risk factor for laryngeal/pharyngeal cancer[22]. Few studies did not show GERD as an independent risk factor for cancer in multivariate analysis when tobacco and alcohol consumption are considered[23]; however, other studies, including a meta-analysis, do show GERD as an independent risk factor especially in non-smokers[24-27]. Also, the incidence of these tumors is increasing parallel to GERD.
Another piece of evidence that links GERD and laryngeal/pharyngeal cancer is the putative higher risk in patients with heterotopic acid-producing gastric mucosa in the proximal esophagus (inlet patch)[28].
The literature on oral cancer and GERD is scarce even though they also may be associated[29].
Similar to the proximal respiratory organs, duodenogastric contents may also reflux to the lungs. Pepsin and biliary salts can be recovered from the lungs in patients with end-stage pulmonary diseases[30]. GERD is associated with different lung diseases[31]; however, the association of GERD and lung cancer is unknown. A single preliminary report showed significant GERD in lung cancer patients irrespective of histology[32].
The link between GERD and lung cancer seems plausible based on the following facts: (1) Lung adenocarcinoma has a growing incidence with a trend to surpass squamous cell carcinoma[33,34], similar to esophageal cancer; (2) Lung adenocarcinoma is the most frequent histologic type in non-smokers and a clear risk factor has not been attributed to it[35]; (3) Connective tissue diseases are common risk factors for lung adenocarcinoma[36] and GERD[37]; and (4) Centrally located lung adenocarcinoma (area of the lung closer to the esophagus and more prone to aspirate gastrodudodenal refluxate) is likely to arise from the glandular epithelium (superficial layer more susceptible to contact with refluxate). In contrast, peripheral adenocarcinoma is likely to originate in type II pneumocytes and Clara cells[38].
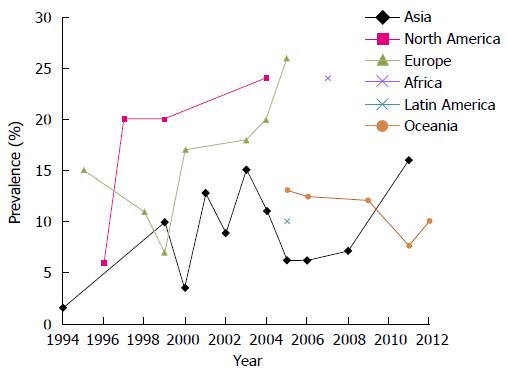
GERD is a common and costly disease; however, despite great achievements in the understanding of the pathophysiology and treatment of the disease, medicine is not winning the battle against GERD. The incidence of GERD is escalating (Figure 1)[39-59] and, even though old complications attributed to this illness, such as esophageal stenosis and ulceration, have almost disappeared, a new spectrum of the disease is surging with extra-esophageal manifestations and cancer. Thus, esophageal cancer should also be added to the burden of GERD and probably head and neck and lung cancers as well.
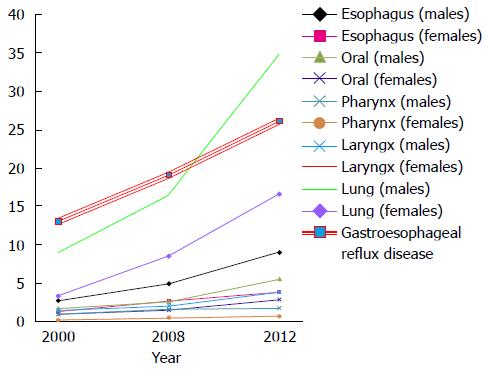
Head and neck and lung cancer both have smoking as the main etiologic factor. Even though the prevalence of smokers is decreasing[60], the incidence of the aforementioned tumors is not (Figure 2). Obviously, a proportional increase in the incidences of two separate diseases does not necessarily indicate an etiological relationship but more than that, a shift towards non-smoking, female gender and adenocarcinoma (compared to squamous cell carcinoma) is arising[61], similar to the example of the esophageal cancer with the exception of the female gender[62-64].
It must be said that most of the papers reviewed are far from ideal to prove the relationship of extra-esophageal cancer and GERD. A single study addressed the association of lung cancer and GERD. Not all studies showed a relationship between GERD and head and neck cancer, and even in studies showing positive association this is not too strong. Some present with a small number of patients, most do not control cases based on tobacco usage and obesity. Moreover, the diagnosis of GERD is variable, not always from an objective measurement such as pH monitoring but relying on symptoms that has been shown not to be a trustworthy method for correct GERD diagnosis. Different previous publications showed that symptoms are unreliable for the diagnosis of GERD[65,66] although the labeling of patients as refluxers based on symptom questionnaires is still a common practice, in spite of the fact that most of these questionnaires were not validated in comparison to esophageal ambulatory pH monitoring[67].
In conclusion, laryngeal and pharyngeal tumors are highly associated to GERD. Oral and lung cancers probably are also connected to GERD.
| 1. | El-Serag HB, Sweet S, Winchester CC, Dent J. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63:871-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Rubenstein JH, Chen JW. Epidemiology of gastroesophageal reflux disease. Gastroenterol Clin North Am. 2014;43:1-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 69] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Sandler RS, Everhart JE, Donowitz M, Adams E, Cronin K, Goodman C, Gemmen E, Shah S, Avdic A, Rubin R. The burden of selected digestive diseases in the United States. Gastroenterology. 2002;122:1500-1511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1062] [Cited by in RCA: 1043] [Article Influence: 43.5] [Reference Citation Analysis (0)] |
| 4. | Peery AF, Dellon ES, Lund J, Crockett SD, McGowan CE, Bulsiewicz WJ, Gangarosa LM, Thiny MT, Stizenberg K, Morgan DR. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179-1187.e1-e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1355] [Cited by in RCA: 1489] [Article Influence: 106.4] [Reference Citation Analysis (1)] |
| 5. | Oh DS, Demeester SR. Pathophysiology and treatment of Barrett’s esophagus. World J Gastroenterol. 2010;16:3762-3772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 42] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Hur C, Miller M, Kong CY, Dowling EC, Nattinger KJ, Dunn M, Feuer EJ. Trends in esophageal adenocarcinoma incidence and mortality. Cancer. 2013;119:1149-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 359] [Cited by in RCA: 400] [Article Influence: 28.6] [Reference Citation Analysis (0)] |
| 7. | Fang Y, Chen X, Bajpai M, Verma A, Das KM, Souza RF, Garman KS, Donohoe CL, O’Farrell NJ, Reynolds JV. Cellular origins and molecular mechanisms of Barrett’s esophagus and esophageal adenocarcinoma. Ann N Y Acad Sci. 2013;1300:187-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Denlinger CE, Thompson RK. Molecular basis of esophageal cancer development and progression. Surg Clin North Am. 2012;92:1089-1103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 28] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Wang DH, Souza RF. Biology of Barrett’s esophagus and esophageal adenocarcinoma. Gastrointest Endosc Clin N Am. 2011;21:25-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 10. | Donohoe CL, Pidgeon GP, Lysaght J, Reynolds JV. Obesity and gastrointestinal cancer. Br J Surg. 2010;97:628-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 86] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 11. | Alemán JO, Eusebi LH, Ricciardiello L, Patidar K, Sanyal AJ, Holt PR. Mechanisms of obesity-induced gastrointestinal neoplasia. Gastroenterology. 2014;146:357-373. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 128] [Cited by in RCA: 154] [Article Influence: 12.8] [Reference Citation Analysis (0)] |
| 12. | Fisichella PM, Patti MG. Gastroesophageal reflux disease and morbid obesity: is there a relation? World J Surg. 2009;33:2034-2038. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 20] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Herbella FA, Sweet MP, Tedesco P, Nipomnick I, Patti MG. Gastroesophageal reflux disease and obesity. Pathophysiology and implications for treatment. J Gastrointest Surg. 2007;11:286-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Navarro Silvera SA, Mayne ST, Gammon MD, Vaughan TL, Chow WH, Dubin JA, Dubrow R, Stanford JL, West AB, Rotterdam H. Diet and lifestyle factors and risk of subtypes of esophageal and gastric cancers: classification tree analysis. Ann Epidemiol. 2014;24:50-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Maasland DH, van den Brandt PA, Kremer B, Goldbohm RA, Schouten LJ. Alcohol consumption, cigarette smoking and the risk of subtypes of head-neck cancer: results from the Netherlands Cohort Study. BMC Cancer. 2014;14:187. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 127] [Cited by in RCA: 143] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 16. | Samet JM. Tobacco smoking: the leading cause of preventable disease worldwide. Thorac Surg Clin. 2013;23:103-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 207] [Article Influence: 15.9] [Reference Citation Analysis (0)] |
| 17. | Pandolfino JE, Kahrilas PJ. Smoking and gastro-oesophageal reflux disease. Eur J Gastroenterol Hepatol. 2000;12:837-842. [PubMed] |
| 18. | Neto SC, Herbella FA, Silva LC, Patti MG. Ratio between proximal/distal gastroesophageal reflux does not discriminate abnormal proximal reflux. World J Surg. 2014;38:890-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Oelschlager BK, Quiroga E, Isch JA, Cuenca-Abente F. Gastroesophageal and pharyngeal reflux detection using impedance and 24-hour pH monitoring in asymptomatic subjects: defining the normal environment. J Gastrointest Surg. 2006;10:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 69] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 20. | Sun G, Muddana S, Slaughter JC, Casey S, Hill E, Farrokhi F, Garrett CG, Vaezi MF. A new pH catheter for laryngopharyngeal reflux: Normal values. Laryngoscope. 2009;119:1639-1643. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 21. | Holbrook WP, Furuholm J, Gudmundsson K, Theodórs A, Meurman JH. Gastric reflux is a significant causative factor of tooth erosion. J Dent Res. 2009;88:422-426. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 74] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 22. | Ward PH, Hanson DG. Reflux as an etiological factor of carcinoma of the laryngopharynx. Laryngoscope. 1988;98:1195-1199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 86] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 23. | Francis DO, Maynard C, Weymuller EA, Reiber G, Merati AL, Yueh B. Reevaluation of gastroesophageal reflux disease as a risk factor for laryngeal cancer. Laryngoscope. 2011;121:102-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Langevin SM, Michaud DS, Marsit CJ, Nelson HH, Birnbaum AE, Eliot M, Christensen BC, McClean MD, Kelsey KT. Gastric reflux is an independent risk factor for laryngopharyngeal carcinoma. Cancer Epidemiol Biomarkers Prev. 2013;22:1061-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 55] [Article Influence: 4.2] [Reference Citation Analysis (1)] |
| 25. | Qadeer MA, Colabianchi N, Vaezi MF. Is GERD a risk factor for laryngeal cancer? Laryngoscope. 2005;115:486-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 44] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 26. | Vaezi MF, Qadeer MA, Lopez R, Colabianchi N. Laryngeal cancer and gastroesophageal reflux disease: a case-control study. Am J Med. 2006;119:768-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 27. | Bacciu A, Mercante G, Ingegnoli A, Ferri T, Muzzetto P, Leandro G, Di Mario F, Bacciu S. Effects of gastroesophageal reflux disease in laryngeal carcinoma. Clin Otolaryngol Allied Sci. 2004;29:545-548. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 28. | Chong VH. Clinical significance of heterotopic gastric mucosal patch of the proximal esophagus. World J Gastroenterol. 2013;19:331-338. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 55] [Cited by in RCA: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 29. | Mercante G, Bacciu A, Ferri T, Bacciu S. Gastroesophageal reflux as a possible co-promoting factor in the development of the squamous-cell carcinoma of the oral cavity, of the larynx and of the pharynx. Acta Otorhinolaryngol Belg. 2003;57:113-117. [PubMed] |
| 30. | Reder NP, Davis CS, Kovacs EJ, Fisichella PM. The diagnostic value of gastroesophageal reflux disease (GERD) symptoms and detection of pepsin and bile acids in bronchoalveolar lavage fluid and exhaled breath condensate for identifying lung transplantation patients with GERD-induced aspiration. Surg Endosc. 2014;28:1794-1800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 29] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 31. | Sweet MP, Patti MG, Hoopes C, Hays SR, Golden JA. Gastro-oesophageal reflux and aspiration in patients with advanced lung disease. Thorax. 2009;64:167-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 81] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 32. | Vereczkei A, Horvath OP, Varga G, Molnar TF. Gastroesophageal reflux disease and non-small cell lung cancer. Results of a pilot study. Dis Esophagus. 2008;21:457-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 33. | Etzel CJ, Lu M, Merriman K, Liu M, Vaporciyan A, Spitz MR. An epidemiologic study of early onset lung cancer. Lung Cancer. 2006;52:129-134. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 42] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 34. | Liam CK, Pang YK, Leow CH, Poosparajah S, Menon A. Changes in the distribution of lung cancer cell types and patient demography in a developing multiracial Asian country: experience of a university teaching hospital. Lung Cancer. 2006;53:23-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 35. | Couraud S, Zalcman G, Milleron B, Morin F, Souquet PJ. Lung cancer in never smokers--a review. Eur J Cancer. 2012;48:1299-1311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 353] [Article Influence: 25.2] [Reference Citation Analysis (3)] |
| 36. | Yang Y, Fujita J, Tokuda M, Bandoh S, Ishida T. Lung cancer associated with several connective tissue diseases: with a review of literature. Rheumatol Int. 2001;21:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 44] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 37. | Patti MG, Gasper WJ, Fisichella PM, Nipomnick I, Palazzo F. Gastroesophageal reflux disease and connective tissue disorders: pathophysiology and implications for treatment. J Gastrointest Surg. 2008;12:1900-1906. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 38. | Fukui T, Shaykhiev R, Agosto-Perez F, Mezey JG, Downey RJ, Travis WD, Crystal RG. Lung adenocarcinoma subtypes based on expression of human airway basal cell genes. Eur Respir J. 2013;42:1332-1344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 35] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 39. | Goh KL. Gastroesophageal reflux disease in Asia: A historical perspective and present challenges. J Gastroenterol Hepatol. 2011;26 Suppl 1:2-10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 40. | Bhatia SJ, Reddy DN, Ghoshal UC, Jayanthi V, Abraham P, Choudhuri G, Broor SL, Ahuja V, Augustine P, Balakrishnan V. Epidemiology and symptom profile of gastroesophageal reflux in the Indian population: report of the Indian Society of Gastroenterology Task Force. Indian J Gastroenterol. 2011;30:118-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 61] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 41. | Hung LJ, Hsu PI, Yang CY, Wang EM, Lai KH. Prevalence of gastroesophageal reflux disease in a general population in Taiwan. J Gastroenterol Hepatol. 2011;26:1164-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 42. | El-Serag HB, Petersen NJ, Carter J, Graham DY, Richardson P, Genta RM, Rabeneck L. Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126:1692-1699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 191] [Cited by in RCA: 192] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 43. | Locke GR, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ. Risk factors associated with symptoms of gastroesophageal reflux. Am J Med. 1999;106:642-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 350] [Cited by in RCA: 342] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 44. | Frank L, Kleinman L, Ganoczy D, McQuaid K, Sloan S, Eggleston A, Tougas G, Farup C. Upper gastrointestinal symptoms in North America: prevalence and relationship to healthcare utilization and quality of life. Dig Dis Sci. 2000;45:809-818. [PubMed] |
| 45. | Diaz-Rubio M, Moreno-Elola-Olaso C, Rey E, Locke GR, Rodriguez-Artalejo F. Symptoms of gastro-oesophageal reflux: prevalence, severity, duration and associated factors in a Spanish population. Aliment Pharmacol Ther. 2004;19:95-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 46. | Louis E, DeLooze D, Deprez P, Hiele M, Urbain D, Pelckmans P, Devière J, Deltenre M. Heartburn in Belgium: prevalence, impact on daily life, and utilization of medical resources. Eur J Gastroenterol Hepatol. 2002;14:279-284. [PubMed] |
| 47. | Agréus L, Svärdsudd K, Talley NJ, Jones MP, Tibblin G. Natural history of gastroesophageal reflux disease and functional abdominal disorders: a population-based study. Am J Gastroenterol. 2001;96:2905-2914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 102] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 48. | Isolauri J, Laippala P. Prevalence of symptoms suggestive of gastro-oesophageal reflux disease in an adult population. Ann Med. 1995;27:67-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 214] [Cited by in RCA: 210] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 49. | Ronkainen J, Aro P, Storskrubb T, Johansson SE, Lind T, Bolling-Sternevald E, Graffner H, Vieth M, Stolte M, Engstrand L, Talley NJ, Agréus L. High prevalence of gastroesophageal reflux symptoms and esophagitis with or without symptoms in the general adult Swedish population: a Kalixanda study report. Scand J Gastroenterol. 2005;40:275-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 315] [Cited by in RCA: 318] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 50. | Valle C, Broglia F, Pistorio A, Tinelli C, Perego M. Prevalence and impact of symptoms suggestive of gastroesophageal reflux disease. Dig Dis Sci. 1999;44:1848-1852. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 53] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 51. | Terry P, Lagergren J, Wolk A, Nyrén O. Reflux-inducing dietary factors and risk of adenocarcinoma of the esophagus and gastric cardia. Nutr Cancer. 2000;38:186-191. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 74] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 52. | Mohammed I, Cherkas LF, Riley SA, Spector TD, Trudgill NJ. Genetic influences in gastro-oesophageal reflux disease: a twin study. Gut. 2003;52:1085-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 176] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 53. | Eslick GD, Talley NJ. Gastroesophageal reflux disease (GERD): risk factors, and impact on quality of life-a population-based study. J Clin Gastroenterol. 2009;43:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 70] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 54. | Pandeya N, Green AC, Whiteman DC; Australian Cancer Study. Prevalence and determinants of frequent gastroesophageal reflux symptoms in the Australian community. Dis Esophagus. 2012;25:573-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 55. | Ben Chaabane N, El Jeridi N, Ben Salem K, Hellara O, Loghmari H, Melki W, Bdioui F, Safer L, Soltani M, Saffar H. Prevalence of gastroesophageal reflux in a Tunisian primary care population determined by patient interview. Dis Esophagus. 2012;25:4-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 56. | Chen Z, Thompson SK, Jamieson GG, Devitt PG, Watson DI. Effect of sex on symptoms associated with gastroesophageal reflux. Arch Surg. 2011;146:1164-1169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 57. | Watson DI, Lally CJ. Prevalence of symptoms and use of medication for gastroesophageal reflux in an Australian community. World J Surg. 2009;33:88-94. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 58. | Knox SA, Harrison CM, Britt HC, Henderson JV. Estimating prevalence of common chronic morbidities in Australia. Med J Aust. 2008;189:66-70. [PubMed] |
| 59. | Chiocca JC, Olmos JA, Salis GB, Soifer LO, Higa R, Marcolongo M; Argentinean Gastro-oesophageal Reflux Study Group. Prevalence, clinical spectrum and atypical symptoms of gastro-oesophageal reflux in Argentina: a nationwide population-based study. Aliment Pharmacol Ther. 2005;22:331-342. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 97] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 60. | Center for Diseases Control. Trends in Current Cigarette Smoking Among High School Students and Adults, United States, 1965-2011. Available from: http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/ accessed 07-26-2014. |
| 61. | Lortet-Tieulent J, Renteria E, Sharp L, Weiderpass E, Comber H, Baas P, Bray F, Coebergh JW, Soerjomataram I. Convergence of decreasing male and increasing female incidence rates in major tobacco-related cancers in Europe in 1988-2010. Eur J Cancer. 2013;Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 122] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 62. | Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893-2917. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11128] [Cited by in RCA: 11886] [Article Influence: 792.4] [Reference Citation Analysis (6)] |
| 63. | Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001;94:153-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2651] [Cited by in RCA: 2604] [Article Influence: 104.2] [Reference Citation Analysis (1)] |
| 64. | Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11[Internet]. Lyon, France: International Agency for Research on Cancer 2013; Available from: http://globocan.iarc.fr. |
| 65. | Bello B, Zoccali M, Gullo R, Allaix ME, Herbella FA, Gasparaitis A, Patti MG. Lack of correlation between a self-administered subjective GERD questionnaire and pathologic GERD diagnosed by 24-h esophageal pH monitoringup? J Gastrointest Surg. 2013;14-20; discussion p. 20 . [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 45] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 66. | Chan K, Liu G, Miller L, Ma C, Xu W, Schlachta CM, Darling G. Lack of correlation between a self-administered subjective GERD questionnaire and pathologic GERD diagnosed by 24-h esophageal pH monitoring. J Gastrointest Surg. 2010;14:427-436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 67. | Vakil NB, Halling K, Becher A, Rydén A. Systematic review of patient-reported outcome instruments for gastroesophageal reflux disease symptoms. Eur J Gastroenterol Hepatol. 2013;25:2-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
P- Reviewer: Ding GQ, Mickevicius A, Thomopoulos KC S- Editor: Gou SX L- Editor: O’Neill M E- Editor: Wang CH