Published online Nov 21, 2013. doi: 10.3748/wjg.v19.i43.7494
Revised: September 10, 2013
Accepted: September 16, 2013
Published online: November 21, 2013
Processing time: 132 Days and 10.8 Hours
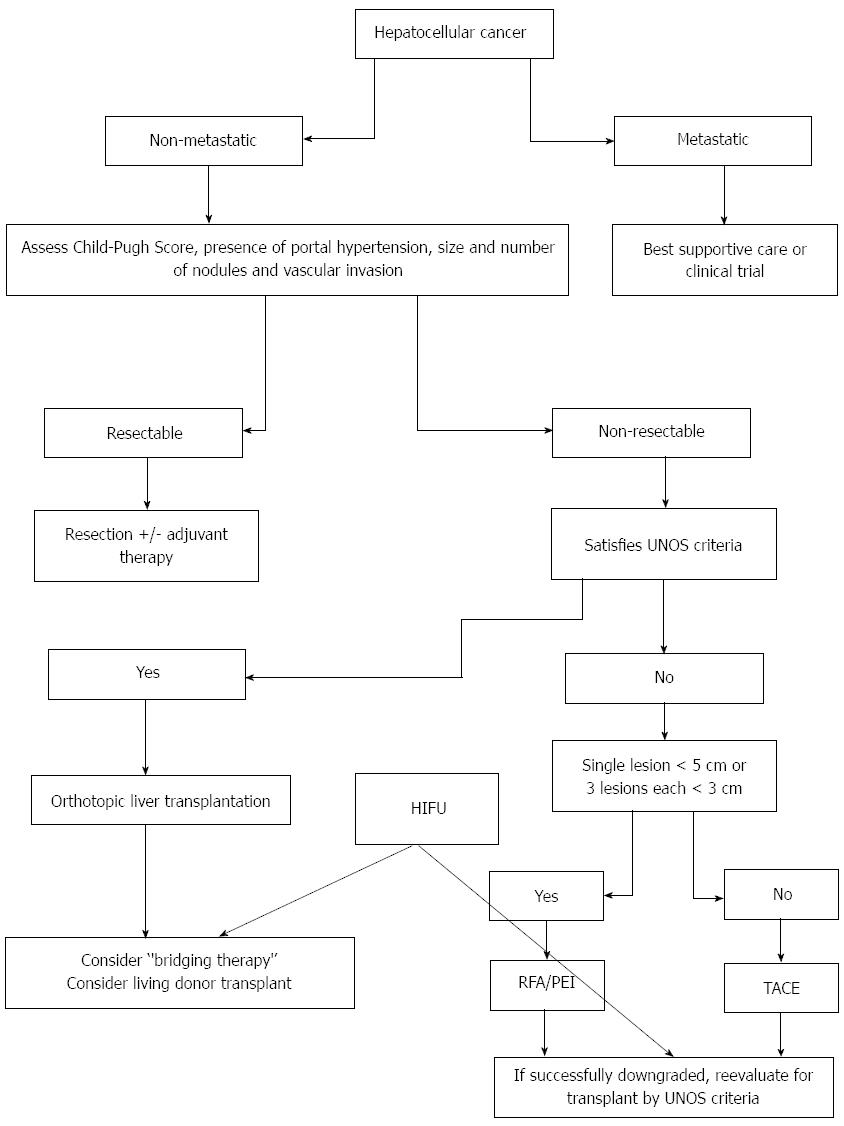
High-intensity focused ultrasound (HIFU) is a non-invasive modality that uses an extracorporeal source of focused ultrasound energy. This technique was introduced by Lynn et al and is able to induce coagulative necrosis in selected tissues without damaging adjacent structures. Although HIFU has been studied for 50 years, recent technological developments now allow its use for tumours of the liver, prostate and other sites. In liver disease, HIFU has been used to treat unresectable, advanced stages of hepatocellular carcinoma (HCC) and liver metastases. Hepatocellular carcinoma is a serious health problem worldwide and is endemic in some areas because of its association with hepatitis B and C viruses (in 20% of cases). Liver transplantation (LT) has become one of the best treatments available because it removes both the tumour and the underlying liver disease such as cirrhosis (which is present in approximately 80% of cases). The prerequisite for long-term transplant success depends on tumour load and strict selection criteria regarding the size and number of tumour nodules. The need to obtain the optimal benefit from the limited number of organs available has prompted strict selection criteria limited to only those patients with early HCC who have a better long-term outcome after LT. The so-called “bridging therapy” has the aim of controlling disease burden for patients who are on the organ transplant waiting list. Amongst various treatment options, transarterial chemoembolisation and radiofrequency ablation are the most popular treatment choices. Recently, Cheung et al demonstrated that HIFU ablation is a safe and effective method for the treatment of HCC patients with advanced cirrhosis as a bridging therapy and that it reduced the dropout rate from the liver transplant waiting list. In this commentary, we discuss the current value of HIFU in the treatment of liver disease, including its value as a bridging therapy, and examine the potential advantages of other therapeutic strategies.
Core tip: High-intensity focused ultrasound (HIFU) is a non-invasive modality used to destroy tissue. It has been used to treat unresectable advanced stages of hepatocellular carcinoma (HCC) and liver metastases. In some HCC cases, liver transplantation has become one of the best treatments because it removes the tumour and the underlying liver disease such as cirrhosis. The so-called “bridging therapy” has the aim of controlling disease burden for patients who are on the organ transplant waiting list. Here, we discuss various treatment options including transarterial chemoembolisation and radiofrequency ablation, and we examine the utility of HIFU as a safe and effective method of bridging therapy that can reduce the dropout rate of patients who are on the liver transplant waiting list.
- Citation: Mearini L. High intensity focused ultrasound, liver disease and bridging therapy. World J Gastroenterol 2013; 19(43): 7494-7499
- URL: https://www.wjgnet.com/1007-9327/full/v19/i43/7494.htm
- DOI: https://dx.doi.org/10.3748/wjg.v19.i43.7494
I have read with great interest the recent article by Cheung et al[1] reporting their experience in the use of high-intensity focused ultrasound (HIFU) in patients with hepatocellular carcinoma (HCC) and cirrhosis who are waiting for liver transplant. The study aim was to determine whether HIFU could reduce the patient dropout rate.
HIFU is a non-invasive modality that uses an extracorporeal source of focused ultrasound energy. The technique was introduced by Lynn et al[2], and it is able to induce coagulative necrosis in targeted tissues without damaging overlying and surrounding vital structures.
Although HIFU has been studied for 50 years, recent technological developments have allowed its use in treating tumours of the liver[3], prostate[4] and other sites[5].
HIFU is a highly precise medical procedure that applies high-intensity focused energy to “heat” and “destroy” diseased tissues. Its precision is under investigation for a possible application as “focal” therapy in case of prostate cancer, where whole gland therapy has a negative impact in terms of incontinence and impotence[6].
HIFU is a hyperthermia therapy, which is a class of clinical therapies [including radiofrequency ablation (RFA)] that use high temperature to treat diseases.
HIFU is also a modality of therapeutic ultrasound, involving minimally invasive or non-invasive methods to direct acoustic energy into the body. In addition to HIFU, other modalities include ultrasound-assisted drug delivery, ultrasound haemostasis, ultrasound lithotripsy and ultrasound-assisted thrombolysis.
A clinical HIFU procedure is typically performed in conjunction with an imaging procedure to enable treatment planning and targeting before applying any therapeutic or ablative levels of ultrasound energy. When diagnostic sonography is used, the technique is termed ultrasound-guided focused ultrasound (USgHIFU or USgFUS). Magnetic resonance imaging is also used for guidance; thus, the technique is sometimes called magnetic resonance-guided focused ultrasound, which is often shortened to MRgHIFU or MRgFUS.
Currently, USgHIFU is approved for use in Bulgaria, China, Hong Kong, Italy, Japan, Korea, Malaysia, Mexico, Russia, Romania, Spain and the United Kingdom. MRgHIFU is an approved therapeutic procedure to treat uterine fibroids in Asia, Australia, Canada, Europe, Israel and the United States (Food and Drug Administration, FDA approved). Research on other indications is actively underway, including clinical trials evaluating the effectiveness of HIFU for the treatment of cancers of the brain, breast, liver, bone, and prostate.
From a technical point of view, the ultrasound waves of high-intensity focused ultrasound are generated by high frequency (0.5 to 10 MHz) vibration of a piezoelectric or piezo-ceramic transducer. The ultrasound beams are then focused by spherical arrangement using an acoustic lens or parabolic reflectors into a small, discrete region that corresponds to the focal point. For clinical applications, and similar to ultrasound imaging, an ultrasound probe is usually coupled by degassed water between the source and patient surface (skin, rectal wall). Because of the comparable acoustic properties of water and tissue, the sound waves should penetrate the surface and the pre-target tissue with only slight absorption, reflection and heating. This phenomenon occurs because the power density of the converging ultrasound increases as it approaches the focal point. The focal region is a 3-dimensional zone, whose area depends on the frequency and the geometry of the source. Generally, the focal area is approximately 10 to 50 mm in length and 1 to 5 mm in diameter.
Based on target volume, the tissue can be ablated by sequentially shifting the focal zone with incremental movements of the transducer. This approach is combined with adjustments of the focal length and is coupled with an immobile organ or with the complex real-time tracking of a moving target (such as liver). The extent of tissue ablation is approximately that of the physical focal zone, although in practice cold spots (cause by blood perfusion in the tissue), beam distortion and beam mis-registration are impediments to finely controlled treatments. However, by scanning the target using multiple pulses and multiple focal points, large tissue areas can be ablated.
The effect of acoustic cavitation induced by the ultrasound beam is complex, and acoustic impedance is sometimes unpredictable. However, the result is cell necrosis induced through a combination of mechanical stress and thermal injury.
The mechanical effect is induced by cavitation, a process in which bubbles develop and increase in size to the point at which resonance is achieved. The bubble formation is a consequence of the negative pressure of the ultrasound wave. As the bubbles expand and collapse, high pressures ranging from 20000 to 30000 bars develop and damage nearby cells. The popcorn effect is the typical example of cavitation.
The thermal effect is directly induced by the ultrasound beams, and due to the significant energy deposition at the focus the temperature within the tissue can rise from 65 to 85 °C. The temperature increase destroys tissue by coagulative necrosis. Higher temperatures are typically avoided to prevent boiling of liquids inside the tissue.
Because ultrasound destroys the diseased tissue non-invasively, it is also known as a non-invasive surgery. In liver disease, HIFU has been used for the treatment of unresectable, advanced stages of hepatocellular carcinoma or for the treatment of liver metastases.
Previous studies have shown that HIFU is safe and effective for patients with hepatocellular carcinoma[7] and can improve the quality of life of patients with HCC. In a study involving 145 patients with HCC, symptoms improved or pain was relieved in 84.8% of the 145 patients. Additionally, the size of the target tumour shrank by various degrees. The 2-year survival rate was 80% in patients with stage Ib HCC, 51.4% in stage IIa, and 46.5% in stage IIIa.
Ng et al[8] involving 49 patients receiving HIFU for unresectable HCC showed that the technique was effective in 79.5% of cases. The study found that only tumour size (≥ 3.0 cm) was a significant risk factor affecting the complete ablation rate. The 1- and 3-year overall survival rates were 87.7% and 62.4%, respectively. Moreover, HIFU is safe for the treatment of disease adjacent to or surrounding a major liver vessel. The study by Zhang et al[9] enrolled 39 patients with HCC. All of the treated tumours had a distance between the tumour and main blood vessel (inferior vena cava, main hepatic vein branches, portal vein) of less than 1 cm, and no major blood vessel injury was observed in any subject.
HIFU has been used in combination with transarterial chemoembolisation (TACE) in prior studies. Jin et al[10] reported their experience of HIFU and transraterial chemoembolisation in 73 patients with unresectable HCC. That study demonstrated that 45.2% patients achieved complete tumour ablation. By multivariate analysis, ablation response (P = 0.001) and tumour size (P = 0.013) were major prognostic factors in predicting response to therapy. In an interesting randomised trial comparing TACE alone vs TACE + HIFU, Li et al[11] showed that the total effective rate for tumour response was 72.8% in the TACE + HIFU group. This response was significantly higher than in the TACE group alone (44.5%, P < 0.05). The corresponding 1-, 2-, 3- and 5-year overall survival rates for the TACE-HIFU group were 72.7%, 50.0%, 31.8% and 11.4%, respectively. These rates were higher than in the TACE alone group (47.2%, 16.7%, 2.8% and 0%, respectively , P < 0.01).
HIFU ablation is well tolerated in HCC patients with cirrhosis. According to Cheung et al[12], 13% of 100 patients developed 18 complications. Morbidity was mainly caused by skin and subcutaneous tissue injuries in nine cases. Based on the Clavien classification of surgical complications, only four complications were grade 3a, while the other 14 were below this grade. By univariate analysis, only age was found to be an independent factor for poor HIFU tolerance.
HCC is a serious health problem worldwide because of its association with hepatitis B and C viruses. Liver transplantation has become one of the best HCC treatments available because it removes both the tumour and the underlying liver disease.
A prerequisite for the long-term success of a transplantation program depends on tumour load and selection criteria regarding size and number of tumour nodules. The need to obtain the optimal benefit from the limited number of available organs has prompted the use of careful selection criteria to list only those patients with early HCC who have a prediction of superior long-term outcome after LT.
Patients who fulfil the so-called Milan criteria (single tumour ≤ 5 cm; two or three tumours, none > 3 cm; no vascular invasion) or the expanded University of California San Francisco criteria (UCSF criteria: single tumour ≤ 4.5 cm; two or three tumours, none > 4.5 cm; or total tumour diameter ≤ 8 cm; no vascular invasion) may have a 3-year survival of up to 88%. However, the expansion of these criteria for transplantation is still a topic of discussion.
Other problems arise from the differential between the number of patients on the liver transplant waiting list and the number of available donors. Additionally, there is a time lag between patient inclusion on a waiting list and the available organ. For example, in the United States, more than 2000 candidates die each year while awaiting transplantation.
Some therapies for HCC, called “bridge therapy”, have the capacity to “fix” or suspend tumour progression and to allow HCC patients to maintain active candidacy as long as necessary to obtain a liver. Several techniques are employed as bridge therapies for HCC patients awaiting liver transplantation. Treatment options such as TACE and radio frequency ablasion (RFA) are the most popular treatment choices as pre-transplant locoregional therapy.
Moreover, other goals of locoregional therapy, e.g., alcohol injection, radiofrequency ablation, transarterial chemoembolisation, transarterial radioembolization, and liver resection, are intended to decrease tumour size and number in patients who initially present with tumours that do not meet locally acceptable criteria for liver transplantation.
The TACE principle is intra-arterial injection of cytotoxic drug combinations (doxorubicin and/or cisplatin and/or mitomycin into the hepatic artery), followed by lipiodol injection, gelfoam for vessel occlusion and degradable microspheres. An aggressive ablation therapy in association with a short transplant waiting time has the potential to optimise the curative intent of liver transplantation in selected cirrhotic patients. Based on the local extension of the disease and the hepatic functional reserve, TACE may be performed as a ‘‘complete’’, selective or superselective procedure through a microcatheter. Contraindications for TACE include Child-Pugh C liver cirrhosis, presence of multifocal bilobar tumour spread, presence of extrahepatic metastases, portal vein thrombosis or arterio-portal fistula.
TACE has shown excellent outcomes as a bridging therapy. However, only patients with preserved liver function and asymptomatic multinodular tumours without vascular invasion or extrahepatic spread are eligible for TACE because it avoids hepatic failure and severe adverse events[13]. TACE has been used as a selective/superselective procedure and has shown excellent results that are superior to a simple lobar approach[14]. As a bridging (or down-staging) therapy, selective/superselective TACE induces a histological necrosis in 91.8% of cases and was maximal for tumours > 3 cm.
RFA represents a widely applied method to treat HCC in a palliative intent, or as a ‘‘bridging’’ to liver transplantation. RFA may be performed under ultrasonography, Computed tomography guidance, or during laparoscopic and open surgical procedures. This procedure has more limitations than TACE, including the number of nodules that may be treated (up to three in most cases) or the maximal tumour diameter of the nodules (up to 5 cm). Effective treatment has been achieved[15] when 100% tumour necrosis is present. However, it is difficult to reach this goal with tumours exceeding the above-mentioned diameter or number of tumour nodules. Mazzaferro et al[16] showed that although the complete response rate was high (55%), tumour size (> 3 cm) and time from treatment (> 1 year) predict a high risk of tumour persistence in the targeted nodule.
As a bridging therapy, RFA showed some limitations. Schroeder et al[17] demonstrated that although the majority of treated patients (62%) had a solitary tumour at the beginning of treatment, tumour progression was observed in a large proportion (38%) of patients. These results limit the role of RFA as a bridging treatment prior to LT.
Yttrium-90 (Y90) microsphere radio-embolisation is a recently FDA-approved, non-surgical procedure used to treat inoperable HCC. This innovative procedure delivers targeted, internal radiation therapy directly to the tumour[18]. Some promising results have been reported for this technique either as a “bridging” option before other treatment modalities (partial hepatectomy, liver transplantation) or as a main therapy for patients with diffuse intrahepatic tumour spread. Treatment with Y90 microspheres has the advantage of being able to treat all intrahepatic HCC lesions, including otherwise undetected tumours. This treatment may also be the alternative to TACE in selected patients with contraindications for TACE.
In conclusion, with increases in waiting times for liver transplantation, it has become common practice to monitor patients to ensure that they remain within the acceptable criteria for liver transplantation. Moreover, the dropout of patients on the waiting list is common because of cancer progression or other medical reasons. Locoregional therapy as a bridging strategy for patients on the waiting list aims to decrease tumour-related dropout rates and to reduce the incidence of recurrent diseases after liver transplantation. Current available techniques show a dropout rate up to 35% for transarterial embolisation and up to 15% for radiofrequency ablation.
Cheung et al[12] must be congratulated for testing the utility of high-intensity focused ultrasound in this particular setting. The study examined 49 consecutive HCC patients listed for liver transplant by UCSF criteria. Twenty-nine patients received TACE as a bridging therapy, 16 patients received no treatment before liver transplantation, and five patients received HIFU as bridging therapy. The control group of five patients received HIFU but were not on the transplant list. TACE was performed using cisplatin as the chemotherapeutic agent, and it was delivered with Lipiodol, followed by gelfoam particle embolisation. Selective cannulation and embolisation of the feeding arteries of the tumours were performed whenever possible. All of the HIFU treatments were conducted by an experienced hepatobiliary surgeon and radiologist using the JC HIFU system (Chongqing Haifu Technology, Chongqing, China). The system is composed of a real-time diagnostic imaging unit, a therapeutic unit, a degassed water circulation unit, and a computer system. The real-time diagnostic imaging unit provides direct visualisation of the tumour. The therapeutic unit consists of an ultrasound energy transducer that focuses the ultrasound energy at a 12-cm focal point. The degassed water circulation unit provides a medium for ultrasound transmission outside the body. The computer system controls these three units.
Cheung demonstrated that 90% of patients receiving HIFU had complete tumour response, while 10% had partial response. There was no complete or partial tumour response in the TACE group. Fourteen (46%) patients had progressive disease, and 14 (46%) patients had stable disease. The overall dropout rate was 24.1%.
HIFU was shown to be a safe treatment, and none of the patients receiving HIFU as a bridging therapy developed complications due to intolerance after the procedure. The complication rate was 8.2%, and the complications involved mild skin oedema and injury due to energy accumulation at the ultrasound beam pathway.
HIFU ablation is an entirely extracorporeal non-invasive ablative treatment method using focused ultrasound energy. It is capable of causing coagulative necrosis of the targeted HCC via intact skin, without the need for surgical incision.
HIFU has been well demonstrated to be an effective ablation modality that is non-invasive. It can effectively reduce the dropout rate from the liver transplant waiting list by providing effective tumour control. The histological proof from the liver explants provides evidence that the necrosis is effective in an in vivo model.
Despite the low number of enrolled subjects, the preliminary study by Cheung et al[1] is interesting and suggests the need for more extensive clinical trials that focus on the use of HIFU as a bridging therapy (Figure 1).
| 1. | Cheung TT, Fan ST, Chan SC, Chok KS, Chu FS, Jenkins CR, Lo RC, Fung JY, Chan AC, Sharr WW. High-intensity focused ultrasound ablation: an effective bridging therapy for hepatocellular carcinoma patients. World J Gastroenterol. 2013;19:3083-3089. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 2. | Lynn JG, Zwemer RL, Chick AJ, Miller AE. A new method for the generation and use of focused ultrasound in experimental biology. J Gen Physiol. 1942;26:179-193. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 437] [Cited by in RCA: 411] [Article Influence: 25.7] [Reference Citation Analysis (0)] |
| 3. | Shen HP, Gong JP, Zuo GQ. Role of high-intensity focused ultrasound in treatment of hepatocellular carcinoma. Am Surg. 2011;77:1496-1501. [PubMed] |
| 4. | Mearini L, Porena M. Transrectal high-intensity focused ultrasound for the treatment of prostate cancer: past, present, and future. Indian J Urol. 2010;26:4-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Kennedy JE, Ter Haar GR, Cranston D. High intensity focused ultrasound: surgery of the future? Br J Radiol. 2003;76:590-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 555] [Cited by in RCA: 395] [Article Influence: 17.2] [Reference Citation Analysis (0)] |
| 6. | Mearini L, Porena M. Pros and cons of focal therapy for localised prostate cancer. Prostate Cancer. 2011;2011:584784. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Xu G, Luo G, He L, Li J, Shan H, Zhang R, Li Y, Gao X, Lin S, Wang G. Follow-up of high-intensity focused ultrasound treatment for patients with hepatocellular carcinoma. Ultrasound Med Biol. 2011;37:1993-1999. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Ng KK, Poon RT, Chan SC, Chok KS, Cheung TT, Tung H, Chu F, Tso WK, Yu WC, Lo CM. High-intensity focused ultrasound for hepatocellular carcinoma: a single-center experience. Ann Surg. 2011;253:981-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Zhang L, Zhu H, Jin C, Zhou K, Li K, Su H, Chen W, Bai J, Wang Z. High-intensity focused ultrasound (HIFU): effective and safe therapy for hepatocellular carcinoma adjacent to major hepatic veins. Eur Radiol. 2009;19:437-445. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 135] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 10. | Jin C, Zhu H, Wang Z, Wu F, Chen W, Li K, Su H, Zhou K, Gong W. High-intensity focused ultrasound combined with transarterial chemoembolization for unresectable hepatocellular carcinoma: long-term follow-up and clinical analysis. Eur J Radiol. 2011;80:662-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Li C, Zhang W, Zhang R, Zhang L, Wu P, Zhang F. Therapeutic effects and prognostic factors in high-intensity focused ultrasound combined with chemoembolisation for larger hepatocellular carcinoma. Eur J Cancer. 2010;46:2513-2521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Cheung TT, Chu FS, Jenkins CR, Tsang DS, Chok KS, Chan AC, Yau TC, Chan SC, Poon RT, Lo CM. Tolerance of high-intensity focused ultrasound ablation in patients with hepatocellular carcinoma. World J Surg. 2012;36:2420-2427. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Vogl TJ, Naguib NN, Nour-Eldin NE, Rao P, Emami AH, Zangos S, Nabil M, Abdelkader A. Review on transarterial chemoembolization in hepatocellular carcinoma: palliative, combined, neoadjuvant, bridging, and symptomatic indications. Eur J Radiol. 2009;72:505-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 108] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Golfieri R, Cappelli A, Cucchetti A, Piscaglia F, Carpenzano M, Peri E, Ravaioli M, D’Errico-Grigioni A, Pinna AD, Bolondi L. Efficacy of selective transarterial chemoembolization in inducing tumor necrosis in small (& lt; 5 cm) hepatocellular carcinomas. Hepatology. 2011;53:1580-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 188] [Cited by in RCA: 221] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 15. | Lu DS, Yu NC, Raman SS, Lassman C, Tong MJ, Britten C, Durazo F, Saab S, Han S, Finn R. Percutaneous radiofrequency ablation of hepatocellular carcinoma as a bridge to liver transplantation. Hepatology. 2005;41:1130-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 257] [Cited by in RCA: 271] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 16. | Mazzaferro V, Battiston C, Perrone S, Pulvirenti A, Regalia E, Romito R, Sarli D, Schiavo M, Garbagnati F, Marchianò A. Radiofrequency ablation of small hepatocellular carcinoma in cirrhotic patients awaiting liver transplantation: a prospective study. Ann Surg. 2004;240:900-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 380] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 17. | Schroeder T, Sotiropoulos GC, Molmenti EP, Kuehl H, Cicinnati VR, Schmitz KJ, Kóbori L, Paul A, Mathé Z. Changes in staging for hepatocellular carcinoma after radiofrequency ablation prior to liver transplantation as found in the explanted liver. Hepatogastroenterology. 2011;58:2029-2031. [PubMed] |
| 18. | Lau WY, Lai EC, Leung TW. Current role of selective internal irradiation with yttrium-90 microspheres in the management of hepatocellular carcinoma: a systematic review. Int J Radiat Oncol Biol Phys. 2011;81:460-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 19. | Parikh S, Hyman D. Hepatocellular cancer: a guide for the internist. Am J Med. 2007;120:194-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 119] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
P- Reviewers: Lin ZY, Maruyama H S- Editor: Gou SX L- Editor: A E- Editor: Wang CH