©The Author(s) 2026.
World J Gastroenterol. Feb 14, 2026; 32(6): 115232
Published online Feb 14, 2026. doi: 10.3748/wjg.v32.i6.115232
Published online Feb 14, 2026. doi: 10.3748/wjg.v32.i6.115232
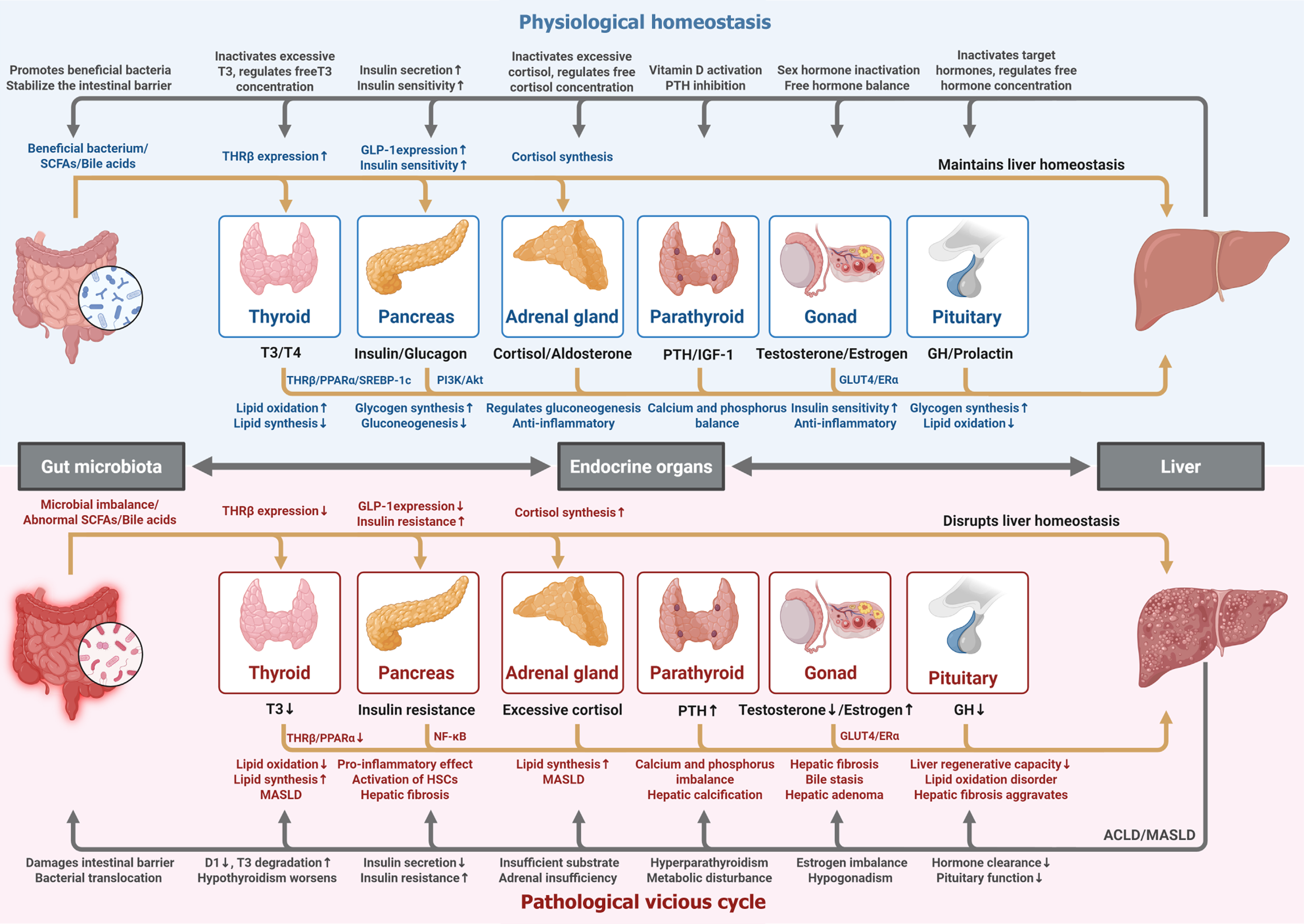
Figure 1 Gut microbiota-endocrine-liver axis: Bidirectional regulation in physiological homeostasis and pathological vicious cycle.
There exists dynamic bidirectional crosstalk among the gut microbiota, endocrine organs (thyroid, pancreas, adrenal gland, parathyroid, gonad, pituitary), and the liver, and this figure depicts their regulatory networks in physiological homeostasis (upper light blue section) and pathological vicious cycle (lower red section). In physiological homeostasis, the gut microbiota fosters beneficial bacteria and stable short-chain fatty acids/bile acids, collaborating with endocrine organs. The thyroid regulates hepatic lipid metabolism via T3-thyroid hormone receptor β-peroxisome proliferator-activated receptor α/sterol regulatory element-binding protein 1c; pancreas maintains glucose homeostasis through insulin/phosphoinositide 3-kinase/Akt pathway; adrenal gland modulates gluconeogenesis and anti-inflammation via cortisol, parathyroid balances calcium/phosphorus, gonad regulates insulin sensitivity and inflammation via sex hormones, and pituitary orchestrates downstream axes. While the liver sustains this balance by inactivating excess hormones, synthesizing binding globulins, and supporting metabolic processes. In the pathological vicious cycle, microbial imbalance and endocrine disorders trigger a cascading loop. The thyroid dysfunction (triiodothyronine↓) worsens lipid accumulation in metabolic dysfunction-associated steatotic liver disease (MASLD), pancreatic insulin resistance activates nuclear factor-κB and hepatic stellate cells to drive hepatic fibrosis, excessive adrenal cortisol promotes MASLD, parathyroid hyperfunction (parathyroid hormone↑) causes calcium/phosphorus imbalance and hepatic calcification, gonadal hormone imbalance (testosterone↓/estrogen↑) induces insulin resistance, bile stasis, and hepatic adenoma, and pituitary dysfunction (growth hormone↓) impairs liver regeneration. While the liver amplifies this cycle through impaired hormone clearance, disrupted gut barrier (bacterial translocation), and metabolic disturbance, ultimately progressing to advanced chronic liver disease or severe MASLD. The figures in the manuscript were created with BioRender.com. ACLD: Advanced chronic liver disease; D1: Type 1 deiodinase; ERα: Estrogen receptor α; GH: Growth hormone; GLUT-4: Glucose transporter type 4; HSCs: Hepatic stellate cells; IGF-1: Insulin-like growth factor 1; MASLD: Metabolic dysfunction-associated steatotic liver disease; NF-κB: Nuclear factor-κB; PI3K/Akt: Phos
- Citation: Wan KR, Qian C, Liu LM. Bidirectional regulation between the endocrine system and liver: From mechanisms to multidisciplinary clinical care. World J Gastroenterol 2026; 32(6): 115232
- URL: https://www.wjgnet.com/1007-9327/full/v32/i6/115232.htm
- DOI: https://dx.doi.org/10.3748/wjg.v32.i6.115232