©The Author(s) 2026.
World J Gastroenterol. Jan 14, 2026; 32(2): 114222
Published online Jan 14, 2026. doi: 10.3748/wjg.v32.i2.114222
Published online Jan 14, 2026. doi: 10.3748/wjg.v32.i2.114222
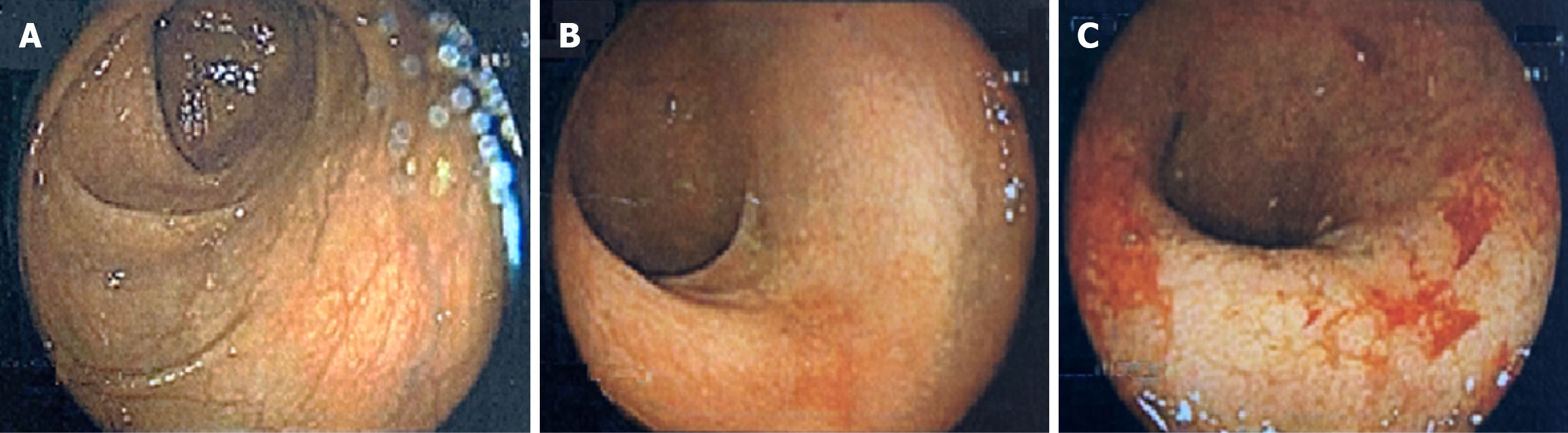
Figure 1 Colonoscopy images (colonoscopy performed at age 40 while managing ulcerative colitis with only oral corticosteroids).
A: Proximal left colon with normal vascular pattern and no mucosal lesions; B: Sigmoid colon with erythema and mucosal friability; C: Rectum with erythema, mucosal friability, erosions, and ulceration.
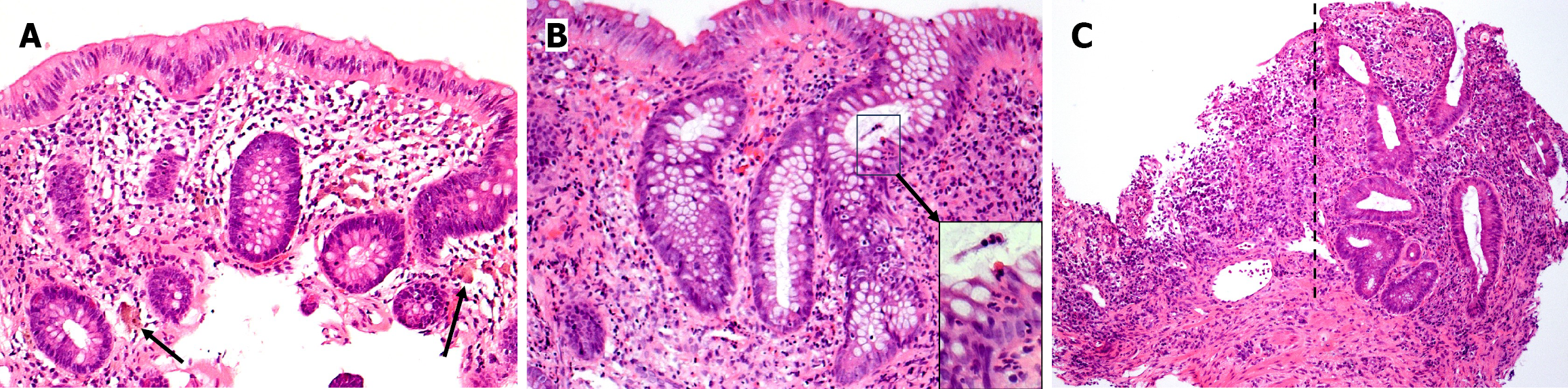
Figure 2 Microscopic photographs of endoscopic biopsies (obtained at age 40 while managing ulcerative colitis with only oral corticosteroids), hematoxylin and eosin stained histologic sections.
A: Right colon biopsy (medium power microscopic view photographed at 100 × magnification) reveals colonic mucosa with occasional plump macrophages with pigmented cytoplasmic accumulation (arrows) within the lamina propria. Colonic mucosa is, otherwise, histologically unremarkable; B: Left colon biopsy (medium power microscopic view photographed at 100 × magnification) reveals mildly active chronic colitis with crypt architectural distortion and a mild increase in mononuclear inflammatory cells within the lamina propria. The epithelium in the crypt on the far right is infiltrated by several neutrophils (“cryptitis”) with modest infiltration into the crypt of Lieberkühn (insert: High power microscopic view); C: Rectal biopsy (low power microscopic view photographed at 40 × magnification) reveals active chronic colitis with crypt architectural distortion and ulceration. The mucosa on the right (of the dotted line) contains a moderate increase in mononuclear inflammatory cells within the lamina propria, basal plasmacytosis, and crypt architectural distortion; whereas, the mucosa on the left (of the dotted line) is ulcerated, comprised of inflamed granulation tissue without crypts.
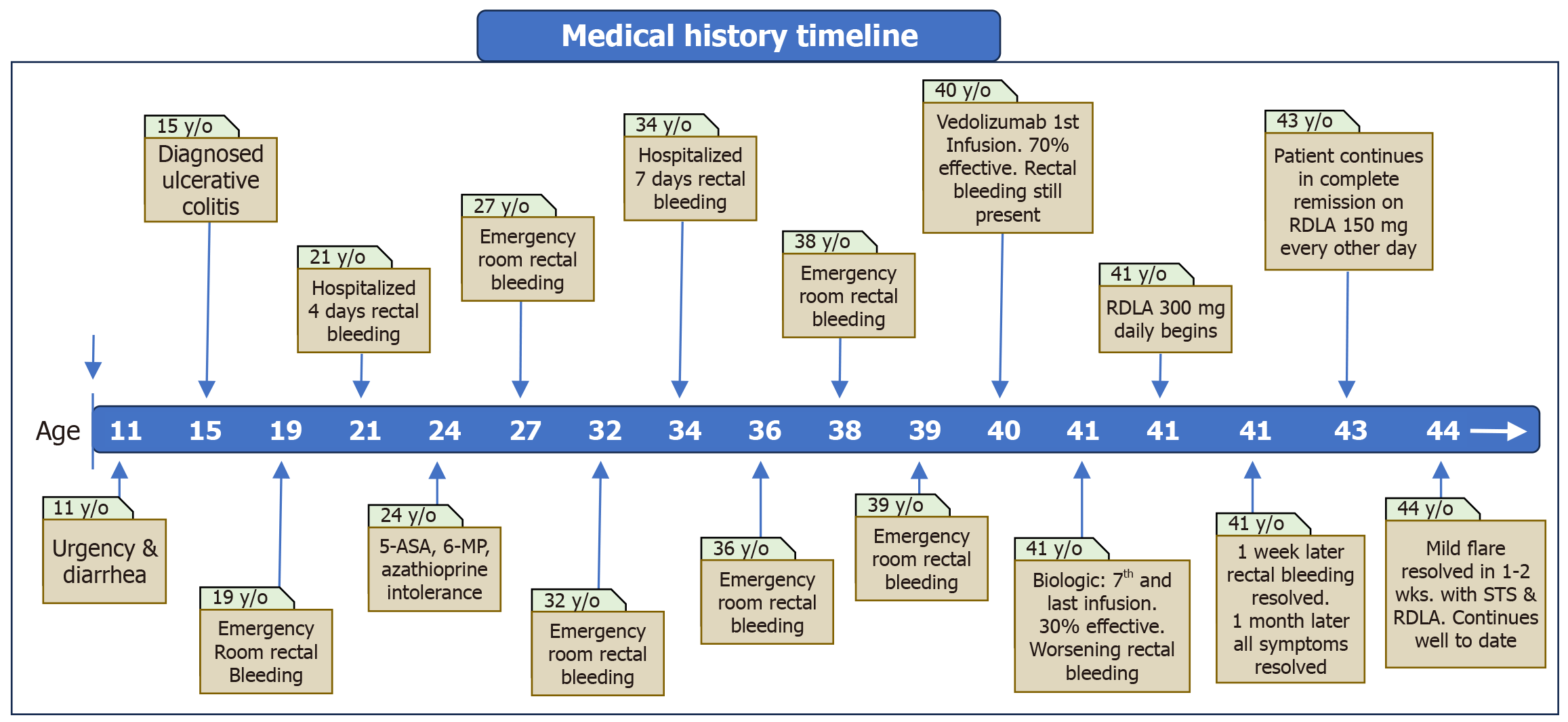
Figure 3 Visual timeline summary of patient’s medical history of ulcerative colitis.
Note the onset of symptoms beginning at 11 years of age. A diagnosis of ulcerative colitis was established at age 15, followed by multiple visits to the emergency department and hospitalizations. After failing treatment with multiple agents, the patient achieved sustained remission at 41 years of age with R-dihydrolipoic acid. Three years later, an ulcerative colitis flare occurring during a highly stressful event was successfully treated with a short course of sodium thiosulfate pentahydrate, followed by resumption of R-dihydrolipoic acid regimen. RDLA: R-dihydrolipoic acid; STS: Sodium thiosulfate pentahydrate.
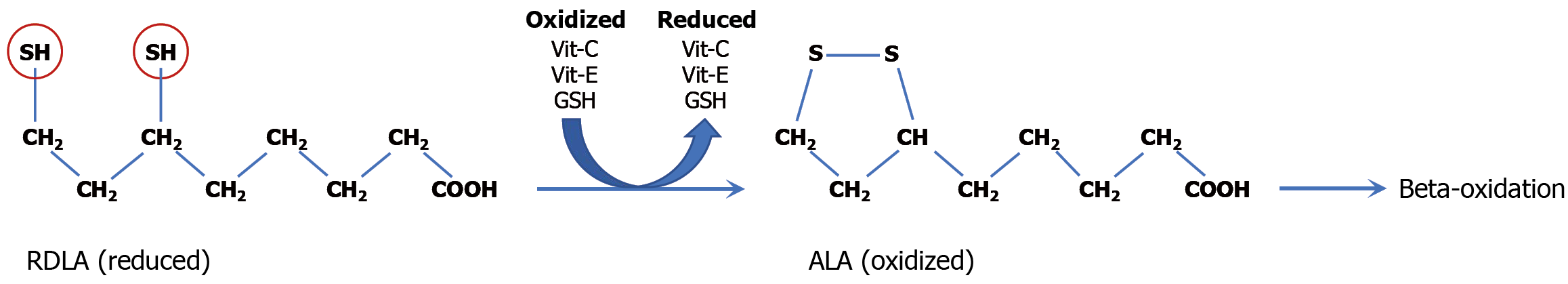
Figure 4 Antioxidant mechanism of R-dihydrolipoic acid: The principal role of R-dihydrolipoic acid is to function as a biological reducing agent that enhances the body’s intrinsic reductive (antioxidant) defenses.
The thiol groups (SH, circled) are responsible for the electron donating (antioxidant) capacity of R-dihydrolipoic acid and the regeneration of other cellular antioxidants (as depicted) - including vitamin C, vitamin E, glutathione, and thioredoxin - following their utilization in neutralizing intracellular and intramitochondrial hydrogen peroxide. Alpha lipoic acid may be recycled back to R-dihydrolipoic acid but is eventually metabolized via mitochondrial beta-oxidation. RDLA: R-dihydrolipoic acid; Vit-C: Vitamin C; Vit-E: Vitamin E; GSH: Glutathione; ALA: Alpha lipoic acid.
- Citation: Sylvestre PB. Reducing agents for induction and maintenance therapy achieve long-term remission of refractory ulcerative colitis: A case report and review of literature. World J Gastroenterol 2026; 32(2): 114222
- URL: https://www.wjgnet.com/1007-9327/full/v32/i2/114222.htm
- DOI: https://dx.doi.org/10.3748/wjg.v32.i2.114222