©The Author(s) 2025.
World J Gastroenterol. Dec 7, 2025; 31(45): 112518
Published online Dec 7, 2025. doi: 10.3748/wjg.v31.i45.112518
Published online Dec 7, 2025. doi: 10.3748/wjg.v31.i45.112518
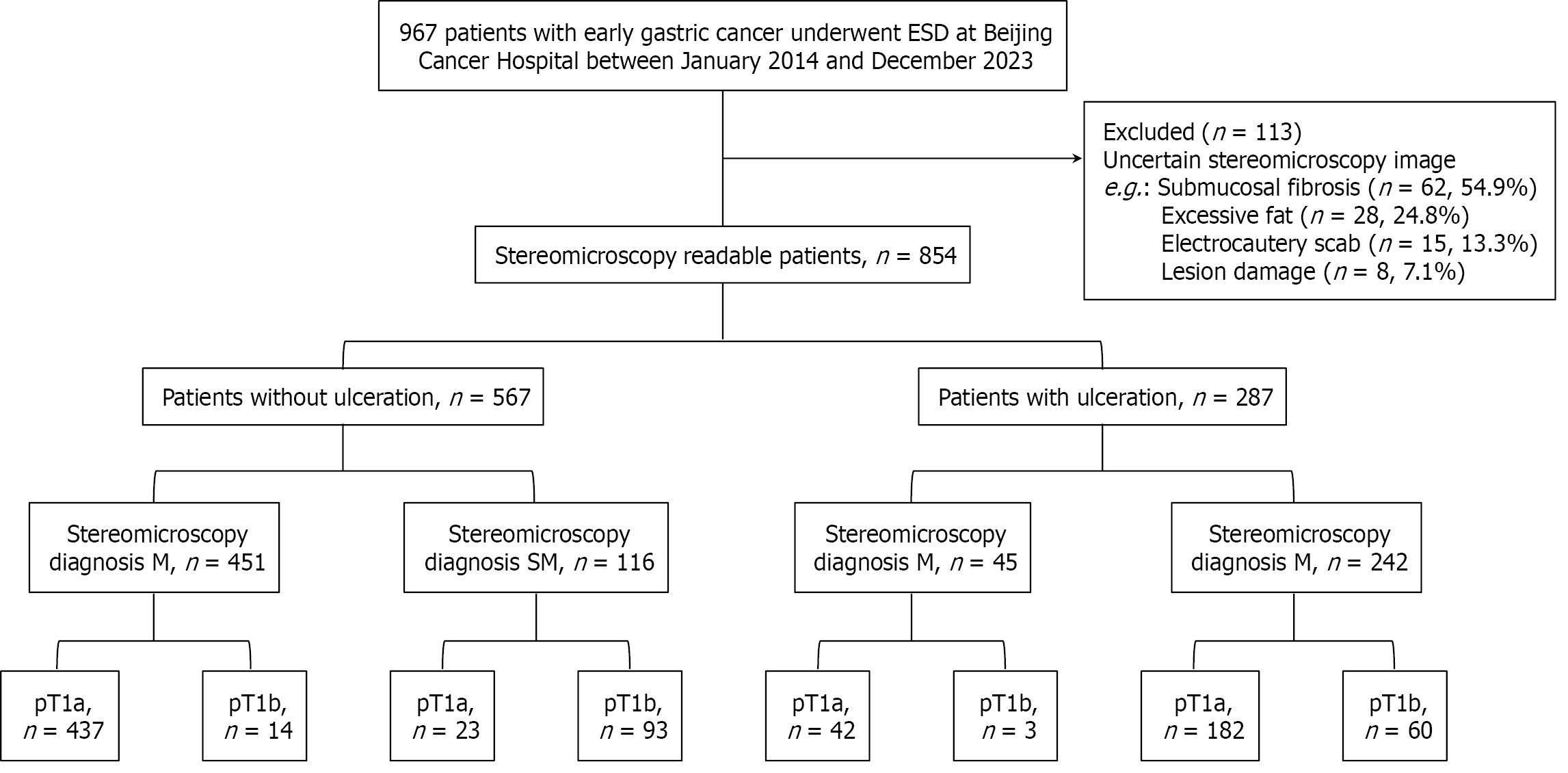
Figure 1 A flow diagram of patients with early gastric cancer included in this study.
ESD: Endoscopic submucosal dissection; M: Mucosa; SM: Submucosa.
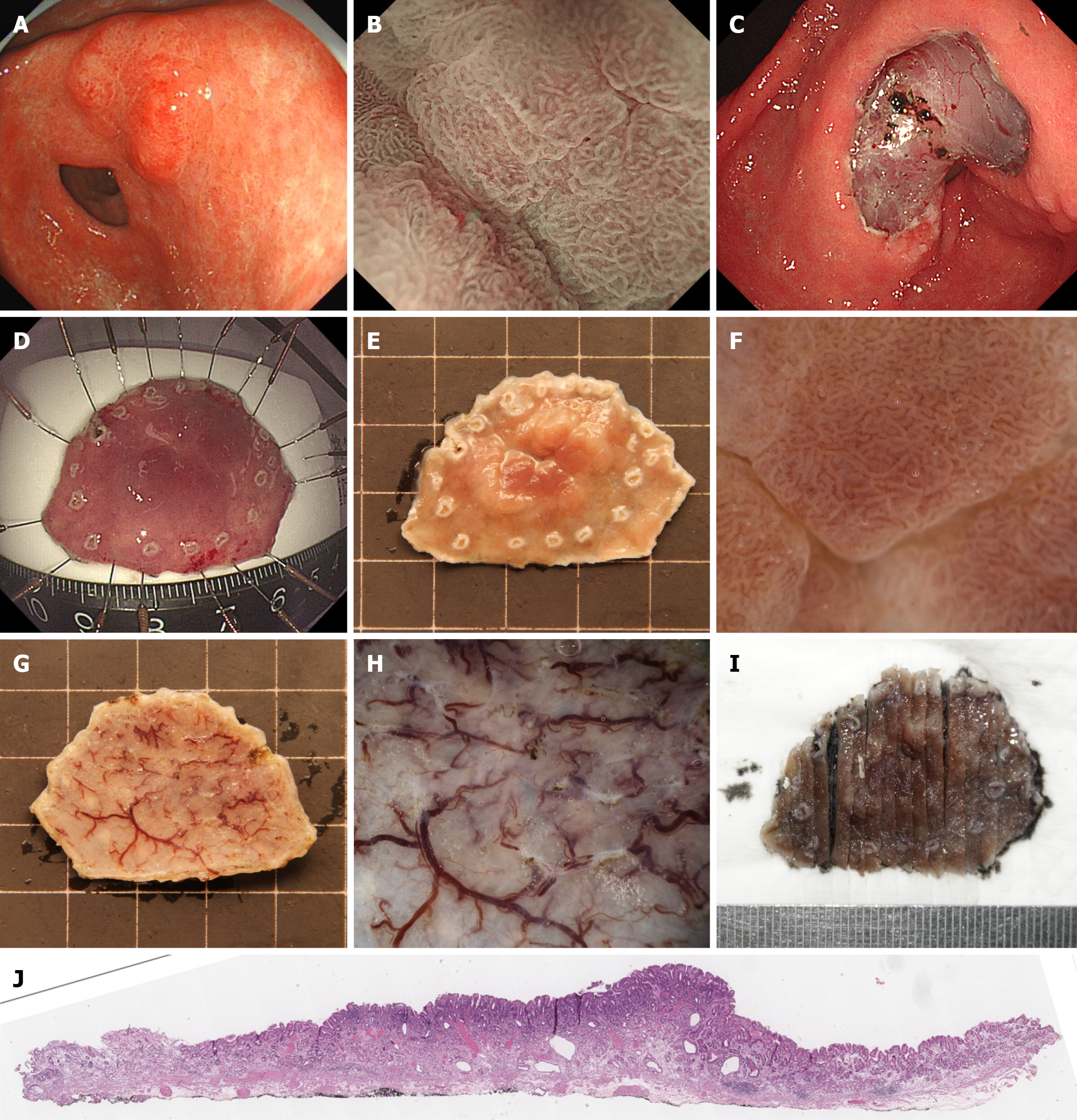
Figure 2 Workflow for preoperative assessment and postoperative management of stereomicroscopy-confirmed mucosal lesions pathologically diagnosed as mucosal.
A: White light imaging of a 0-IIa + IIc lesion in the gastric antrum; B: Magnifying endoscopy with narrow-band imaging of the lesion, demonstrating irregular microsurface and microvascular patterns; C: Post-endoscopic submucosal dissection mucosal defect with visible submucosal vasculature; D: The endoscopic submucosal dissection specimen was spread and pinned on a fixation board for formalin fixation; E: Stereomicroscopic evaluation of the specimen after 24-hour formalin fixation; F: High-magnification stereomicroscopy of the lesion surface, correlating with magnifying endoscopy with narrow-band imaging findings in B, showing irregular microsurface and microvascular architecture; G: Basal surface of the resected specimen under stereomicroscopy; H: High-magnification stereomicroscopy of the basal surface, revealing intact and homogeneous submucosal connective tissue architecture; I: Systematic vertical sectioning of the specimen at 2- to 3-mm intervals, ensuring accurate histopathologic evaluation of margins; J: Histopathological images confirming mucosal (M) diagnosis and margin status.
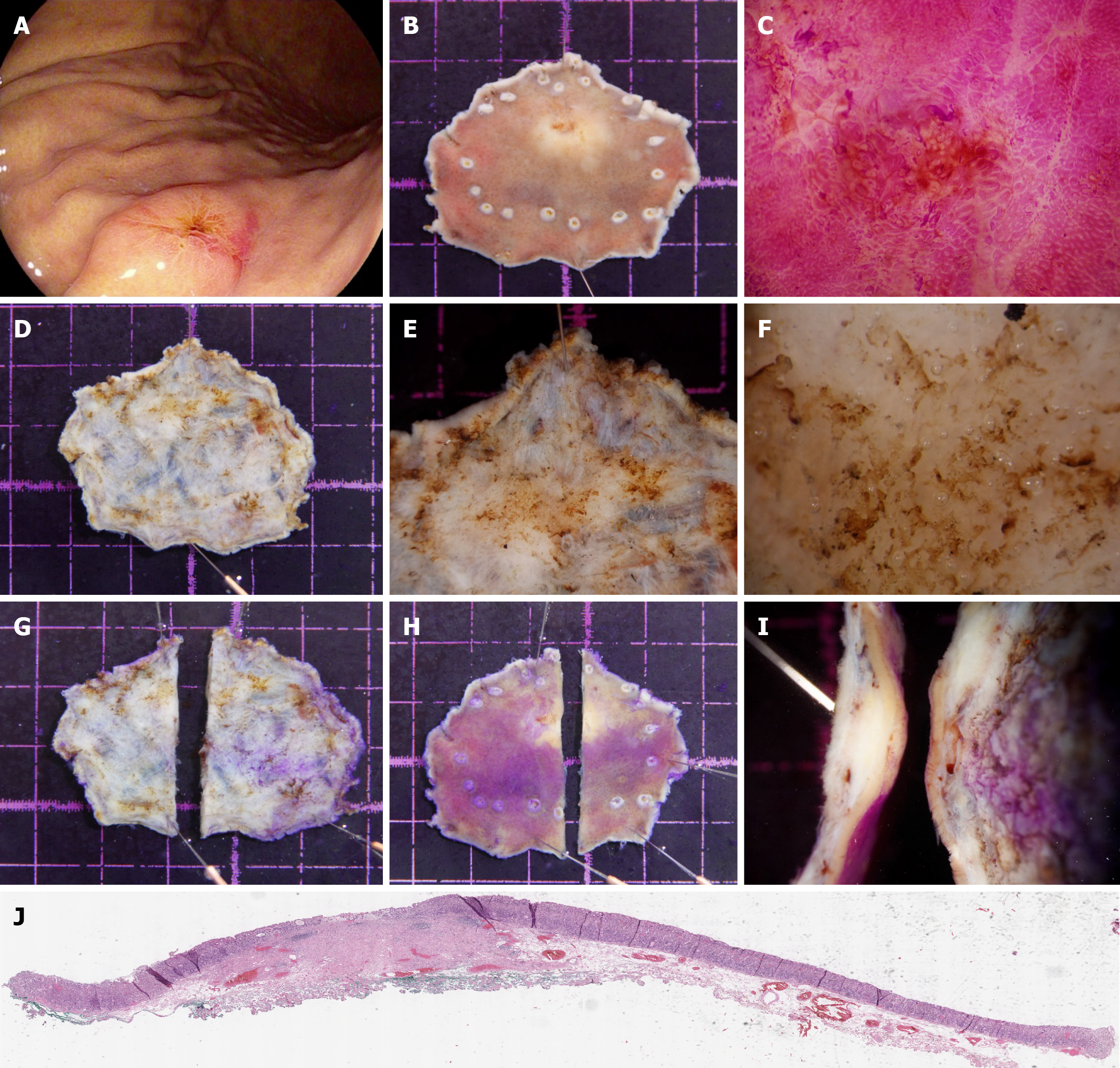
Figure 3 Workflow for preoperative assessment and postoperative management of stereomicroscopy-confirmed submucosal lesions pathologically diagnosed as submucosal.
A: White light imaging of a 0-IIa + IIc lesion located on the posterior wall of the proximal gastric body, exhibiting a central depression; B: Stereomicroscopic evaluation of the specimen after 24-hour formalin fixation; C: High-magnification stereomicroscopy of the central depressed area after eosin staining, demonstrating irregular microsurface patterns; D: Stereomicroscopic overview of the basal surface of the specimen; E: Medium-magnification stereomicroscopy of the basal surface, revealing a thickened submucosal layer with a yellowish-white discoloration; F: High-magnification stereomicroscopy of the basal surface, showing loss of submucosal connective tissue architecture, indicative of tumor invasion into the submucosa; G: The initial incision of the specimen was performed at a distance from the suspected submucosal invasion site on the basal surface to avoid disrupting the area of interest; H: The specimen was inverted to expose the mucosal surface, followed by systematic sampling at 2-mm to 3-mm intervals; I: Lateral view highlighting the deepest point of submucosal invasion; J: Histopathological images confirming the submucosal diagnosis and margin status.
Figure 4 Misdiagnosed case 1 stereomicroscopic overestimation (stereomicroscopy-submucosal vs pathology-T1a).
A: White light imaging of the lesion; B: Stereomicroscopic overview of the formalin-fixed specimen (mucosal surface); C: Stereomicroscopic view of the specimen’s vertical (basal) margin, the central part of the lesion shows localized, non-transparent submucosal tissue with whitish discoloration (diameter > 5 mm), leading to an erroneous diagnosis of submucosal invasion (stereomicroscopy-submucosal). Final histopathology confirmed the lesion was confined to the mucosa (pT1a).
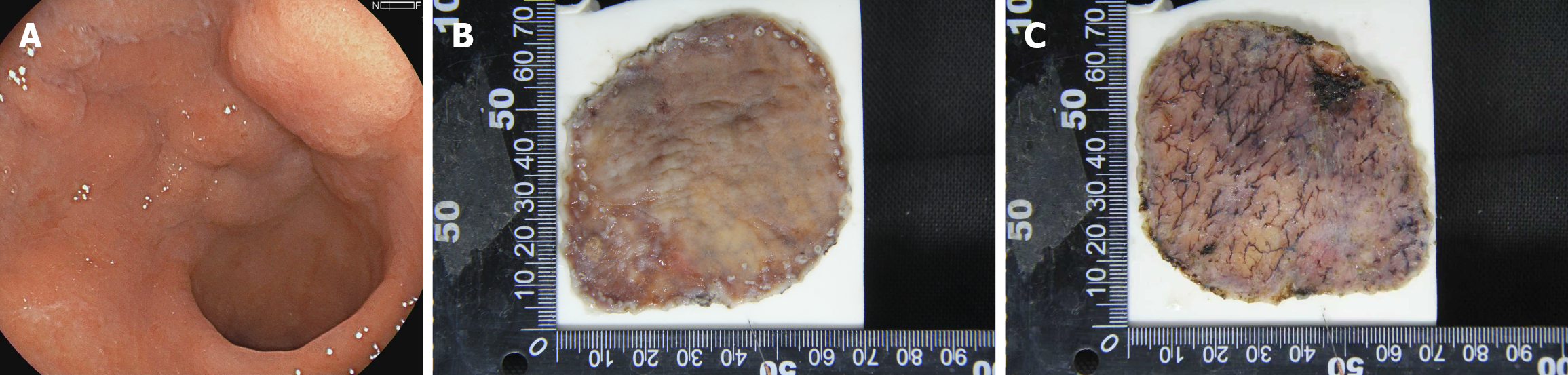
Figure 5 Misdiagnosed case 2 stereomicroscopic underestimation (stereomicroscopy-mucosa vs pathology-T1b).
A: White light imaging of the lesion; B: Stereomicroscopic overview of the formalin-fixed specimen (mucosal surface); C: Stereomicroscopic view of the specimen’s vertical (basal) margin, the submucosa presents with uniformly thick, transparent connective tissue without significant whitish discoloration (individual foci diameter < 5 mm), leading to an erroneous diagnosis of a mucosal lesion (stereomicroscopy-mucosa). Final histopathology confirmed submucosal invasion to a depth of 100 μm (pT1b).
- Citation: Wang J, Chang L, Niu DF, Yan Y, Cao CQ, Li SJ, Wu Q. Diagnostic accuracy of stereomicroscopy assessment of invasion depth in ex vivo specimens of early gastric cancer. World J Gastroenterol 2025; 31(45): 112518
- URL: https://www.wjgnet.com/1007-9327/full/v31/i45/112518.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i45.112518