©The Author(s) 2025.
World J Gastroenterol. Nov 14, 2025; 31(42): 110449
Published online Nov 14, 2025. doi: 10.3748/wjg.v31.i42.110449
Published online Nov 14, 2025. doi: 10.3748/wjg.v31.i42.110449
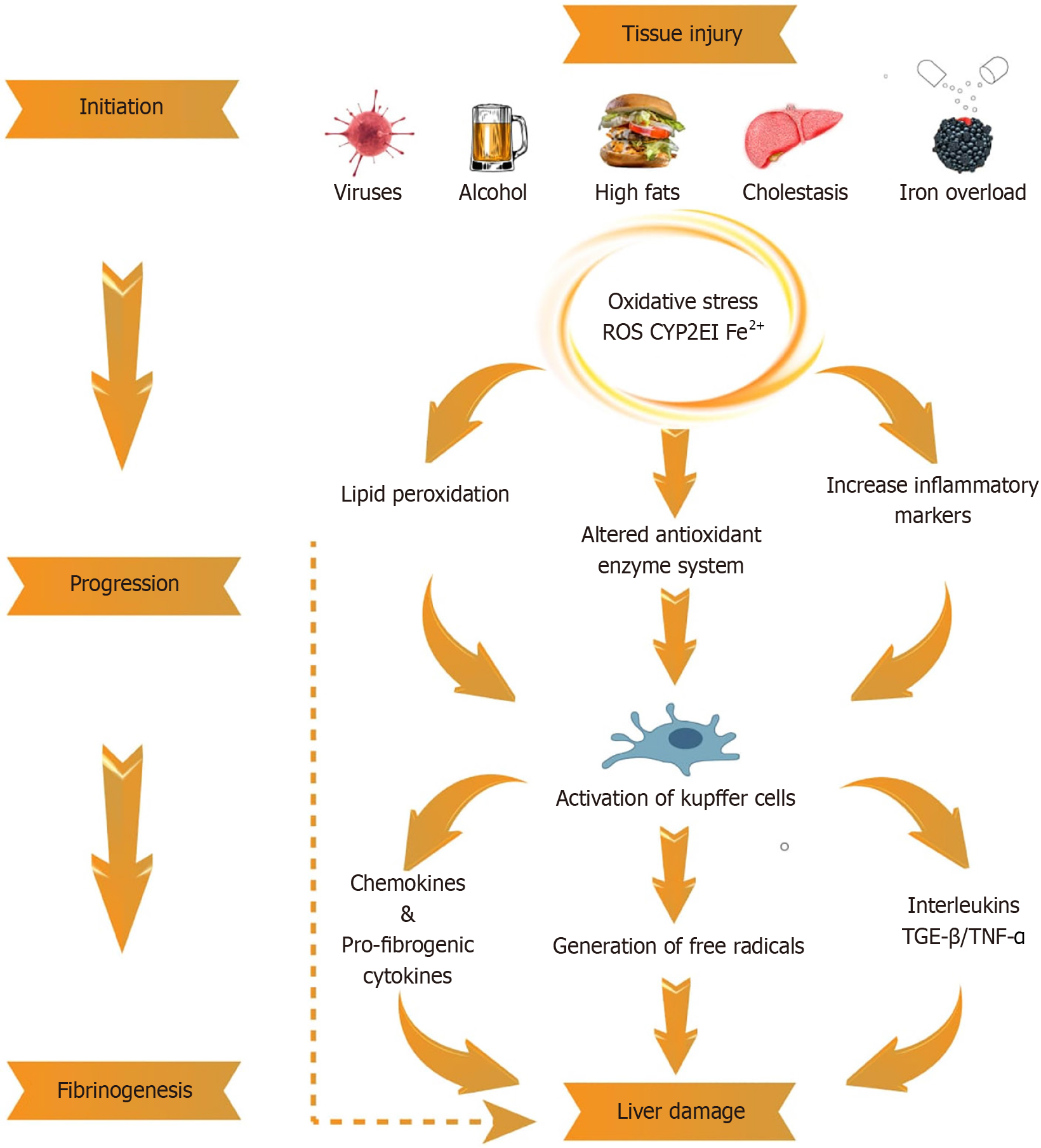
Figure 1 Pathophysiological mechanisms of liver injury leading to fibrogenesis.
This schematic illustrates the key mechanisms underlying chronic liver injury and the progression to liver fibrosis. Persistent liver damage due to viral infections, toxic insults, or metabolic disorders—induces oxidative stress, inflammation, and hepatocyte apoptosis. These insults activate Kupffer cells (liver-resident macrophages), which in turn release pro-inflammatory cytokines (e.g., tumor necrosis factor α, interleukin-6) and reactive oxygen species. These mediators stimulate hepatic stellate cells and drive extracellular matrix deposition, initiating fibrogenesis. Sustained activation of these pathways leads to scar tissue formation and, if unregulated, culminates in liver cirrhosis. TNF-α: Tumor necrosis factor α; ROS: Reactive oxygen species; TGF-β: Transforming growth factor-β.
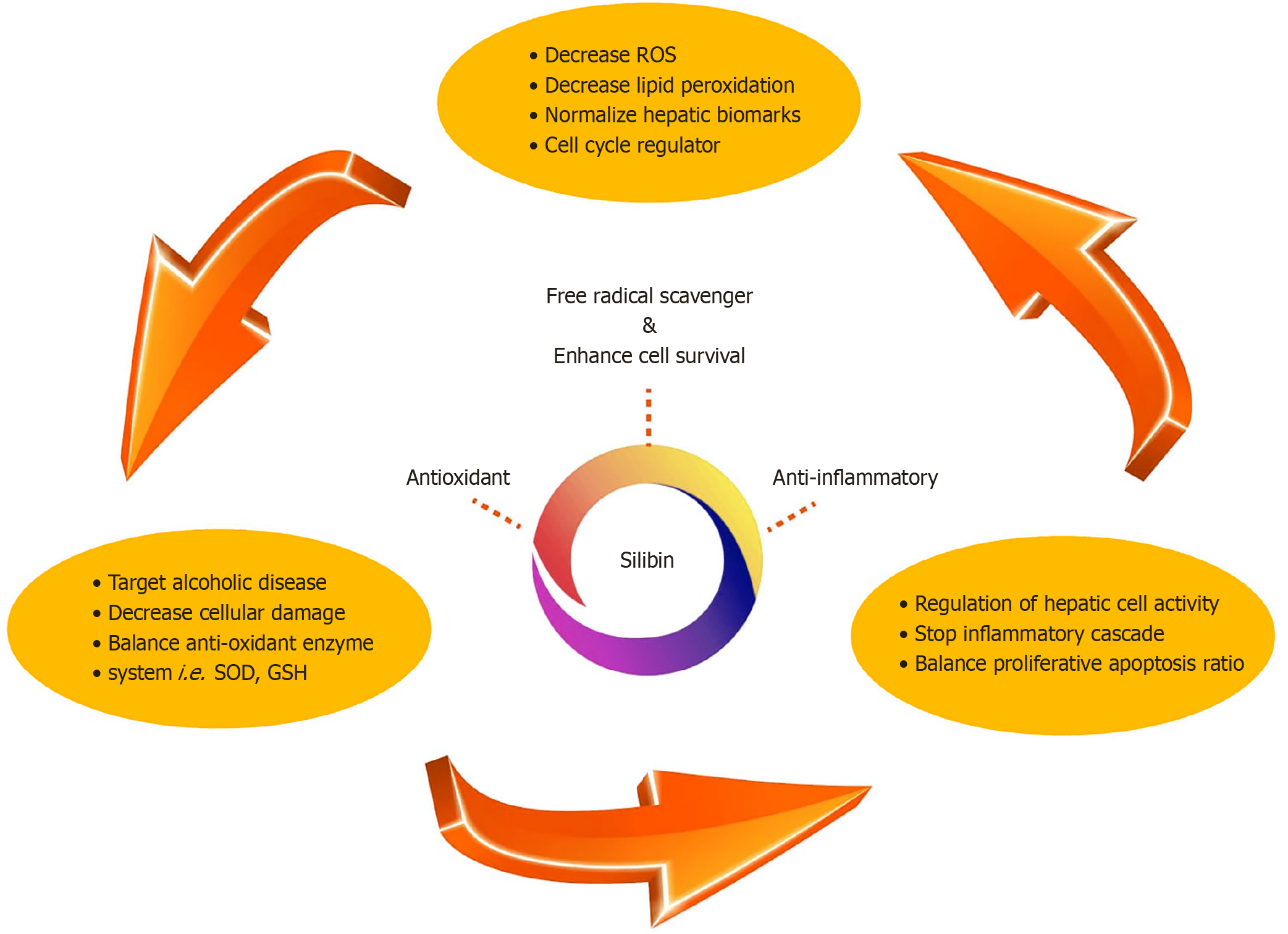
Figure 2 Key biological and pharmacological properties of silybin.
This figure highlights the major therapeutic properties of silybin, the principal active constituent of silymarin extracted from Silybum marianum (milk thistle). Silybin exerts strong antioxidant and anti-inflammatory effects, primarily through the modulation of oxidative stress, suppression of pro-inflammatory cytokines, regulation of apoptotic pathways, and inhibition of fibrogenic signaling. These multifaceted actions contribute to its hepatoprotective and antifibrotic potential. ROS: Reactive oxygen species; SOD: Superoxidedismutase.
- Citation: Liu XX, Hassan W, Ahmed H, Song SZ. Hepatoprotective effects of silybin in liver fibrosis. World J Gastroenterol 2025; 31(42): 110449
- URL: https://www.wjgnet.com/1007-9327/full/v31/i42/110449.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i42.110449