©The Author(s) 2025.
World J Gastroenterol. Oct 14, 2025; 31(38): 109528
Published online Oct 14, 2025. doi: 10.3748/wjg.v31.i38.109528
Published online Oct 14, 2025. doi: 10.3748/wjg.v31.i38.109528
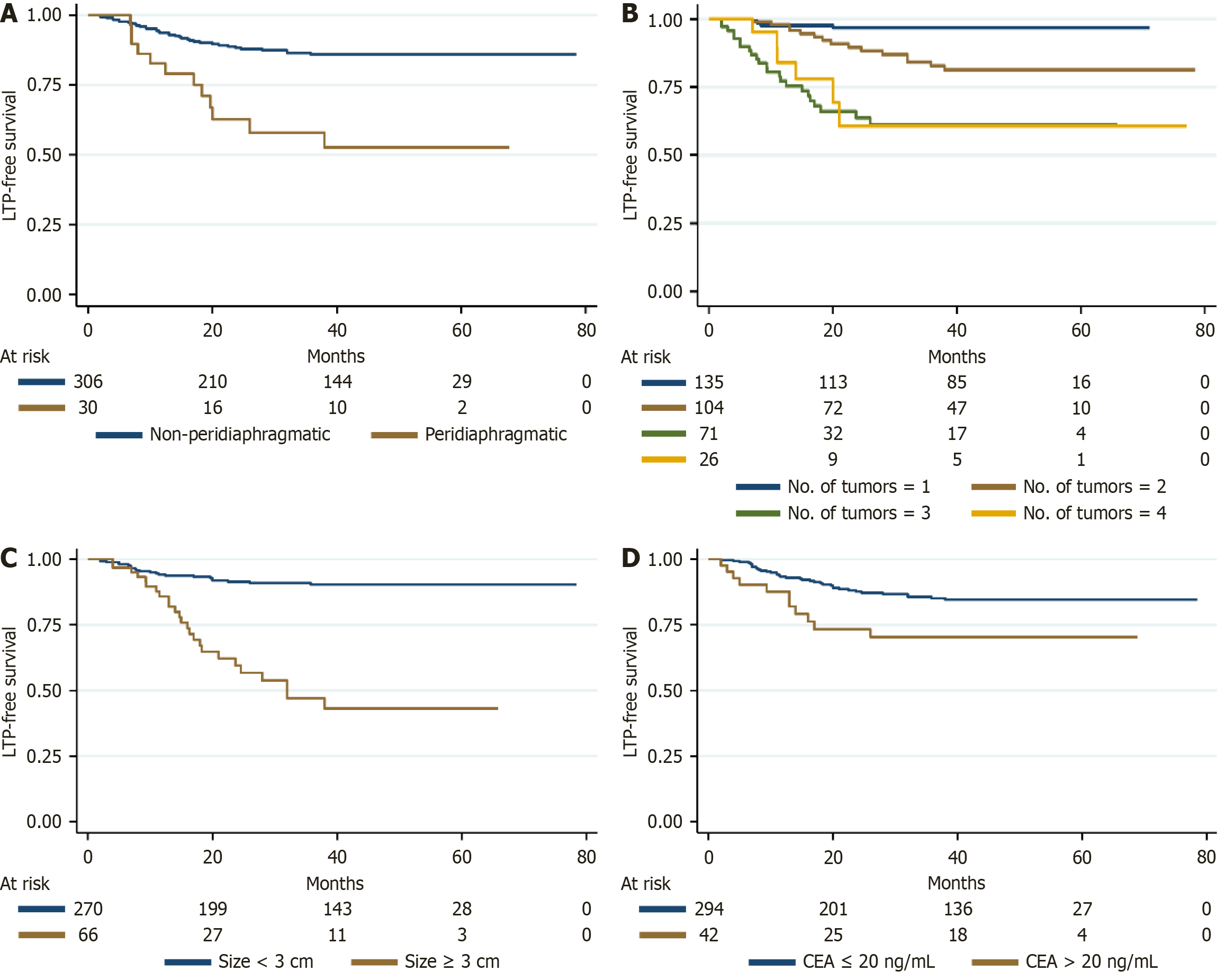
Figure 1 Kaplan-Meier survival curves for local tumor progression-free survival according to anatomical and biological risk factors.
A: Peridiaphragmatic lesion location was significantly associated with increased local progression risk, with a hazard ratio (HR) of 4.447, suggesting anatomical proximity to the diaphragm may compromise ablative efficacy; B: Tumor number was a strong predictor of local tumor progression-free survival (LTPFS). Compared with patients who had a single tumor, those with 2, 3, and 4 tumors showed markedly increased risk of local progression, with HRs of 4.419, 9.607, and 11.140, respectively; C: Tumor size ≥ 3 cm significantly predicted reduced LTPFS (HR = 3.367), indicating that larger lesions may be more challenging to fully ablate; D: Elevated pre-procedural carcinoembryonic antigen levels (> 20 ng/mL) independently correlated with shorter LTPFS (HR = 2.184), reflecting a potential marker of biologically aggressive disease. LTP: Local tumor progression; CEA: Carcinoembryonic antigen. A higher hazard ratio indicates greater risk of local recurrence following ablation.
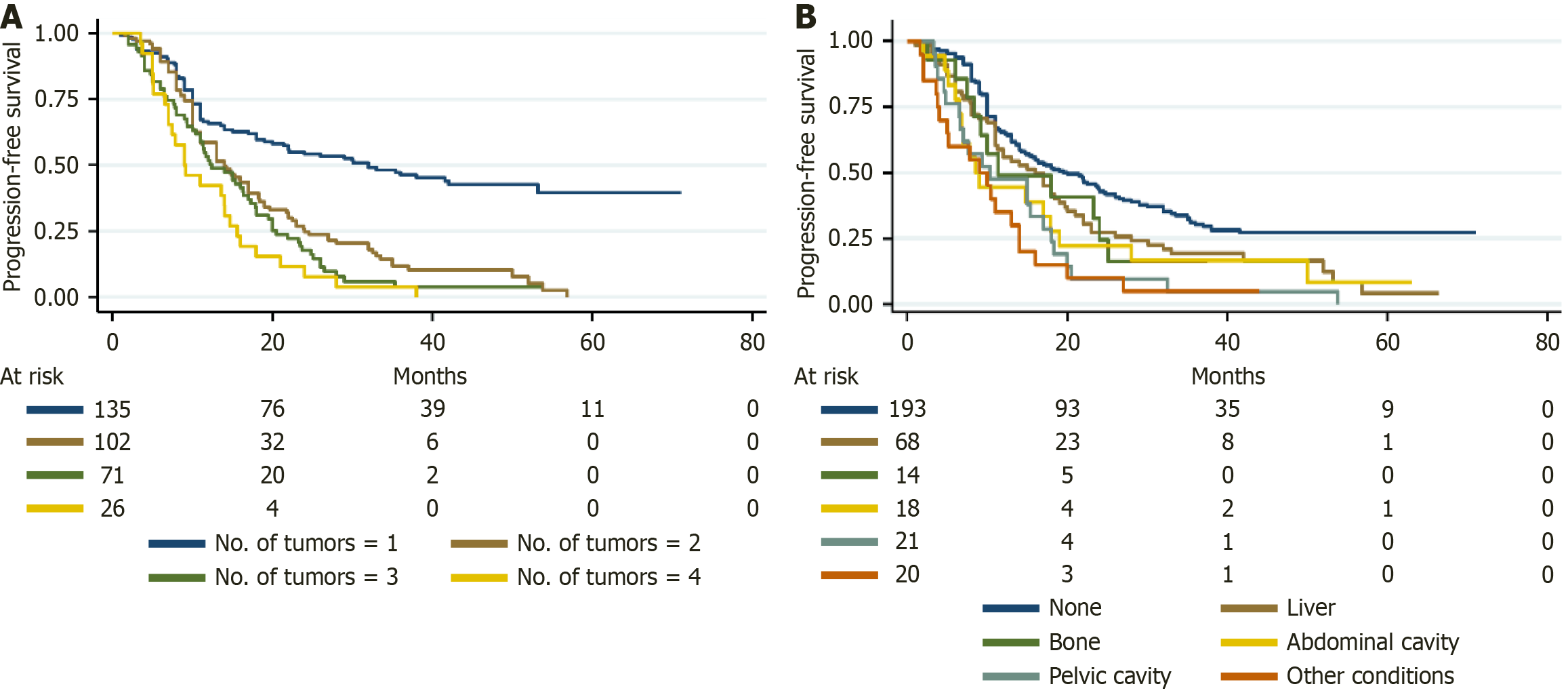
Figure 2 Kaplan-Meier survival curves for progression-free survival stratified by tumor burden and extrapulmonary metastasis patterns.
A: Tumor number was significantly associated with shorter progression-free survival (PFS). Compared to patients with a single tumor, those with 2, 3, and 4 tumors showed progressively increased risks of disease progression, with hazard ratios (HRs) of 2.235, 2.723, and 4.117, respectively; B: Presence and site of extrapulmonary metastases adversely impacted PFS. Patients with liver (HR = 1.449), bone (HR = 1.256), abdominal cavity (HR = 1.864), pelvic cavity (HR = 1.546), and other extrapulmonary metastases (HR = 2.730) had a higher risk of progression compared to those without extrapulmonary disease. A higher hazard ratio reflects a greater risk of progression.
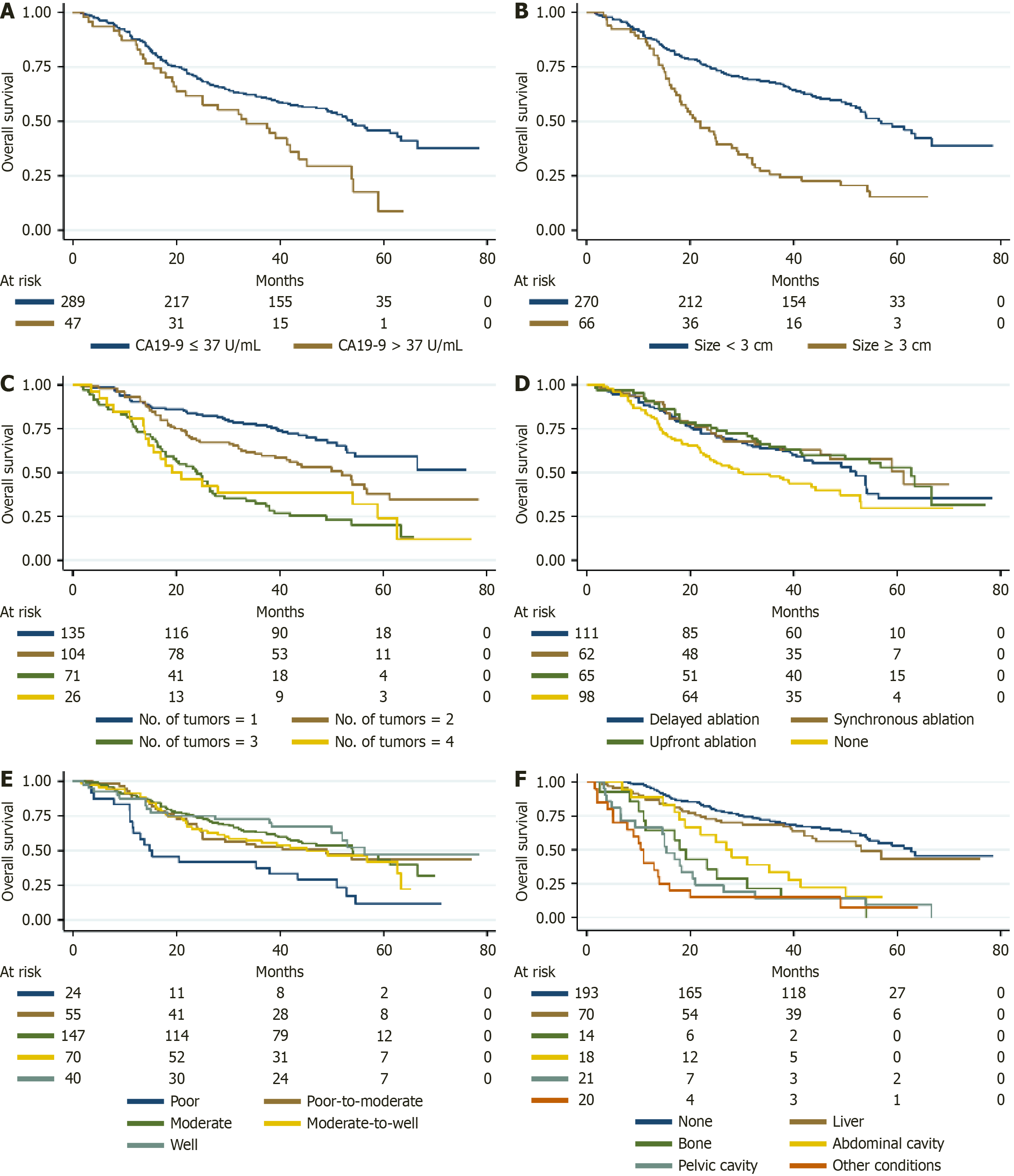
Figure 3 Kaplan-Meier survival curves for overall survival stratified by prognostic factors.
Survival curves illustrate the impact of various clinical and tumor-related factors on overall survival (OS) in patients with colorectal cancer lung metastases undergoing image-guided thermal ablation. A: Elevated carbohydrate antigen 19-9 (> 37 U/mL) was associated with significantly worse OS [hazard ratio (HR) = 1.592]; B: Tumor size ≥ 3 cm correlated with poorer OS compared to tumors < 3 cm (HR = 1.446); C: Increasing tumor number independently predicted worse outcomes, with hazard ratios of 1.446, 2.561, and 2.137 for 2, 3, and 4 tumors, respectively, relative to a single tumor; D: Systemic therapy and its timing were important predictors of OS. Lack of systemic therapy was associated with poorer prognosis, whereas delayed (HR = 0.670), synchronous (HR = 0.551), and upfront ablation (HR = 0.546) improved OS compared to no systemic therapy; E: Tumor differentiation significantly influenced survival; Poorly differentiated tumors (HR = 2.769) had worse outcomes compared to well-differentiated tumors, while other differentiation grades had variable impact; F: Presence and site of extrapulmonary metastasis markedly reduced OS, particularly in bone (HR = 4.538), abdominal cavity (HR = 4.813), pelvic cavity (HR = 3.105), and other sites (HR = 5.230), when compared to patients without extrapulmonary metastases. CA: Carbohydrate antigen. A higher hazard ratio indicates a greater risk of mortality.
- Citation: Hu XF, Dong XJ, Gu XY, Hu JH, Li XH, Zhao FH, Xia XW, Fan HJ, Xu SF. Extrapulmonary metastases impact survival outcomes of thermal ablation for colorectal lung oligometastases: A multicenter study. World J Gastroenterol 2025; 31(38): 109528
- URL: https://www.wjgnet.com/1007-9327/full/v31/i38/109528.htm
- DOI: https://dx.doi.org/10.3748/wjg.v31.i38.109528