Published online Feb 6, 2021. doi: 10.12998/wjcc.v9.i4.935
Peer-review started: October 6, 2020
First decision: November 8, 2020
Revised: November 17, 2020
Accepted: December 16, 2020
Article in press: December 16, 2020
Published online: February 6, 2021
Processing time: 110 Days and 19.1 Hours
Primary retroperitoneal tumor is a rare type of tumor with insidious onset, large tumor size at the time of diagnosis, and often extensive involvement of surrounding tissues and blood vessels in the retroperitoneum. Surgery for primary retroperitoneal tumors is technically challenging. Preoperative imaging evaluation is critical for the selection of the optimal surgical approach and can influence complete resection and recurrence rates. Three-dimensional model reconstruction combined with virtual reality is useful for preoperative assessment.
A 17-year-old female patient was admitted for abdominal pain lasting for half a year that had been worsening for half a month. Abdominopelvic enhanced helical computed tomography revealed a retroperitoneal space-occupying lesion about 11.3 cm × 9.1 cm in size, with well-defined borders in the upper left quadrant of the abdomen. The lesion compressed the left renal artery and vein resulting in vascular displacement and deformation. A multidisciplinary team decided on the optimal treatment approach. Preoperative three-dimensional visualization and virtual reality technology were used to assess and simulate the surgical procedure. Then, retroperitoneal tumor resection along with renal artery reconstruction was decided as the treatment. Complete resection of the retroperitoneal tumor was performed. Stable blood flow was established after renal artery reconstruction. The tumor was diagnosed as mature cystic teratoma (retroperitoneal tumor) by postoperative pathologic analysis. The patient, who recovered well, was discharged after 2 wk and maintains regular follow-ups.
A combination of three-dimensional reconstruction and virtual reality technology before surgery improves the rate of complete resection of retroperitoneal teratoma.
Core Tip: Primary retroperitoneal tumors are a rare type of tumor. In this case report, we describe a patient with a giant retroperitoneal tumor who was preoperatively assessed using a combination of three-dimensional reconstruction and virtual reality technology. Complete removal of the tumor was performed, and there were no complications. The combination of these technologies provides a tool for simulating the operation, which can shorten the operation time, decrease the amount of bleeding, and improve the rate of complete tumor resection.
- Citation: Liu T, Chen K, Xia RM, Li WG. Retroperitoneal teratoma resection assisted by 3-dimensional visualization and virtual reality: A case report. World J Clin Cases 2021; 9(4): 935-942
- URL: https://www.wjgnet.com/2307-8960/full/v9/i4/935.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i4.935
Primary retroperitoneal tumors are a rare type of tumor with insidious onset, large tumor size at the time of diagnosis, and often extensive involvement of surrounding tissues and blood vessels in the retroperitoneum[1]. As these tumors are unresponsive to radiotherapy and chemotherapy, surgical resection is the treatment of choice[2]; however, the surgery is technically difficult. Because of the low rate of complete resection, it is associated with a high rate of postoperative recurrence[3]. Preoperative imaging evaluation[4] has a major impact on the choice of surgical approach as well as rates of complete resection and recurrence. Conventional imaging modalities such as ultrasound (US), computed tomography (CT), magnetic resonance imaging, and angiography have their advantages and disadvantages. Three-dimensional (3D) reconstruction of two-dimensional CT images using software allows visualization of structures from multiple angles and accurate determination of the relationship between tumors, blood vessels, and surrounding organs[5]. Virtual reality (VR) technology makes it possible for the surgeon to formulate an optimal surgical plan based on simulations using the 3D reconstructed model[6].
In this study, we report the case of a patient with a giant retroperitoneal tumor who was preoperatively evaluated using 3D reconstruction combined with VR technology, which facilitated the complete removal of the tumor without complications.
A 17-year-old female patient was admitted to the hospital on September 9, 2019 with abdominal pain that had lasted for half a year and had been worsening for half a month.
On September 8, 2019, the patient visited Xiamen Third Hospital for an abdominal US. A homogeneous mass with fluid echo was detected in the left middle abdomen that was suspected as being a retroperitoneal tumor. The patient came to our hospital for further diagnosis and treatment.
The patient was in good health with no history of infectious disease, allergy, or surgery.
The patient has no family or genetic history of disease.
A standard physical examination was performed. The abdomen was flat and soft; there was tenderness on the left side but no rebound tenderness and no Murphy’s sign. The mass in the left middle abdomen was about 8 cm × 10 cm in size, with an intact capsule but without a distinct boundary; the mass showed poor mobility with tenderness elicited in the palpation test. The liver and spleen were impalpable under the ribs, and there were no obvious gallbladder abnormalities. Further physical examination revealed drum sounds on percussion, negative shifting dullness, and normal bowel sounds on auscultation.
No abnormalities were found in the routine blood, urine and stool analysis, or liver and kidney function.
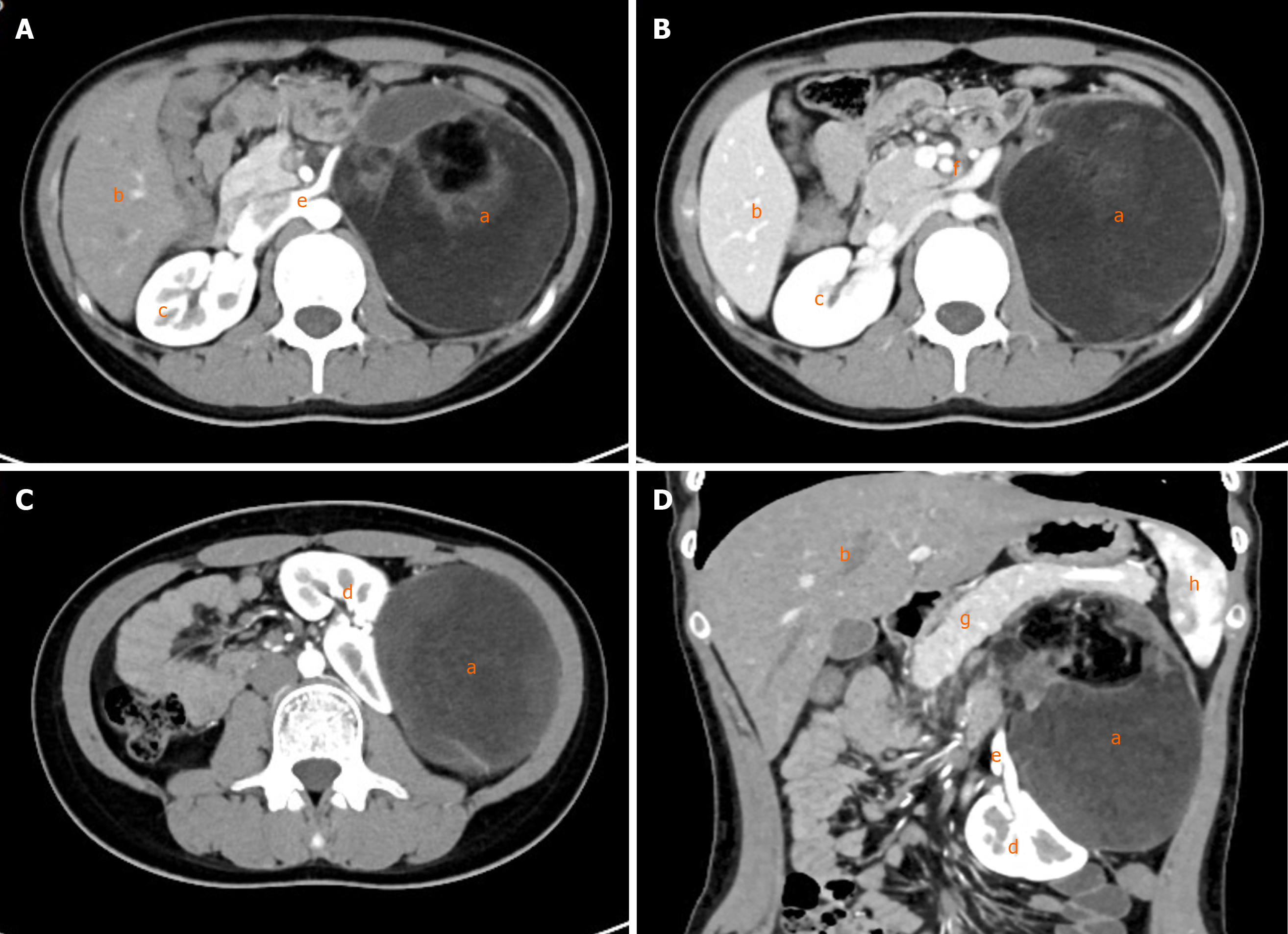
A clinical examination after admission on September 9, 2019 revealed sinus arrhythmia by electrocardiography, and a pulmonary nodule in the right lower lobe by helical CT that may have been an old pulmonary lesion. Abdominopelvic enhanced helical CT showed a retroperitoneal space-occupying lesion in the upper left quadrant of the abdomen that was presumed to be retroperitoneal liposarcoma or teratoma (Figure 1).
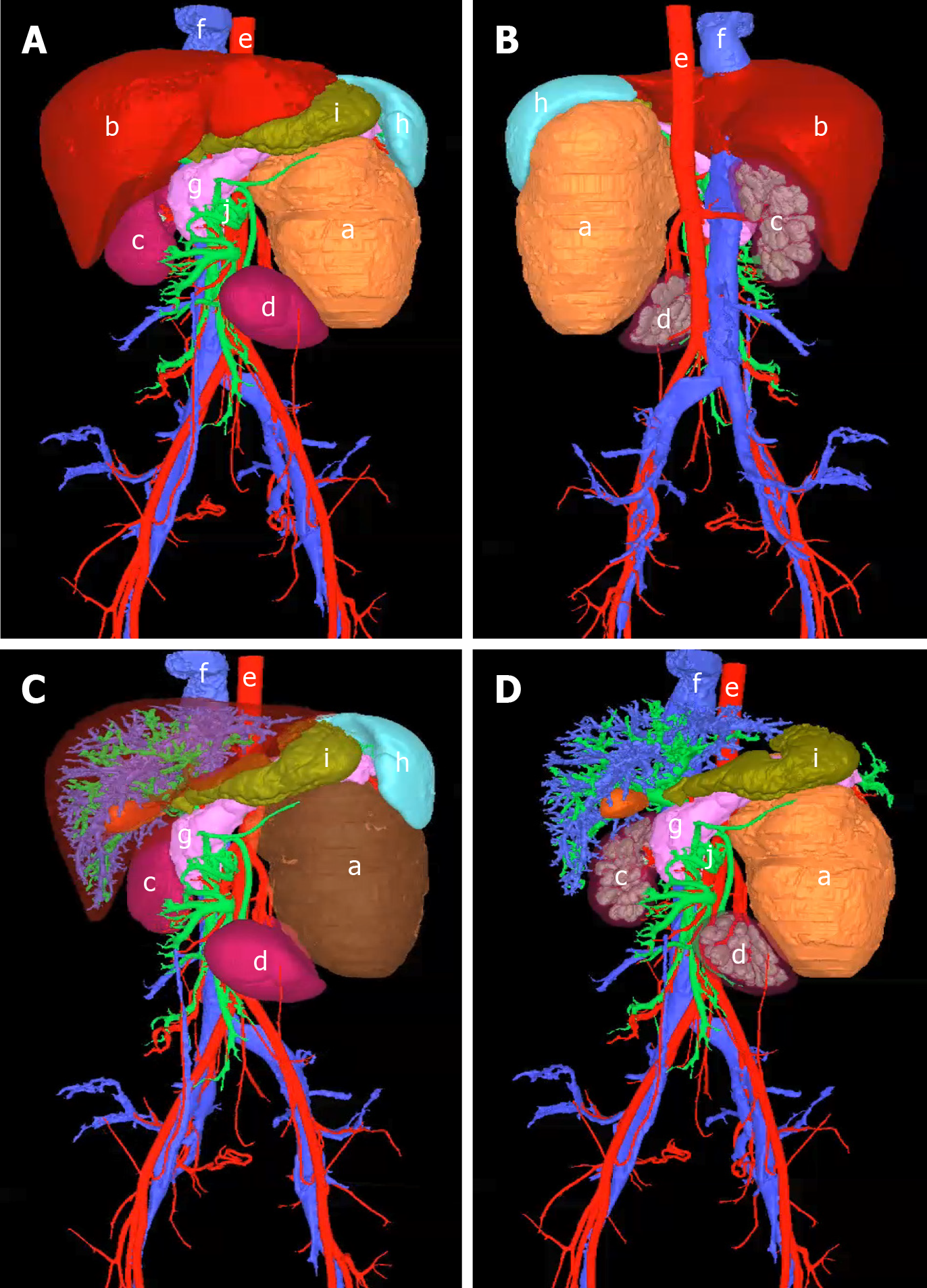
We used the proprietary XMQB-Liver software (Xiamen Qiangben Technology Co, Xiamen, China) for 3D reconstruction of CT images. The software allowed rotation, blurring, and elimination of elements in the 3D model (Figure 2), provided omnidirectional views (Figure 2A and B), and allowed tumor virtualization (Figure 2C), removal of normal organs, and observation of the relationship between the tumor, blood vessels, and surrounding organs (Figure 2D). The tumor was located in the upper left retroperitoneum and was about 11.3 cm × 9.1 cm in size with well-defined borders; it compressed the left renal artery and vein, resulting in vascular displacement and deformation. The inferior vena cava and abdominal aorta were unaffected. The left kidney and adrenal gland were shifted forward and downward under pressure; there was no visible invasion of the liver, spleen, pancreas, or stomach. The intestines could not be reconstructed.
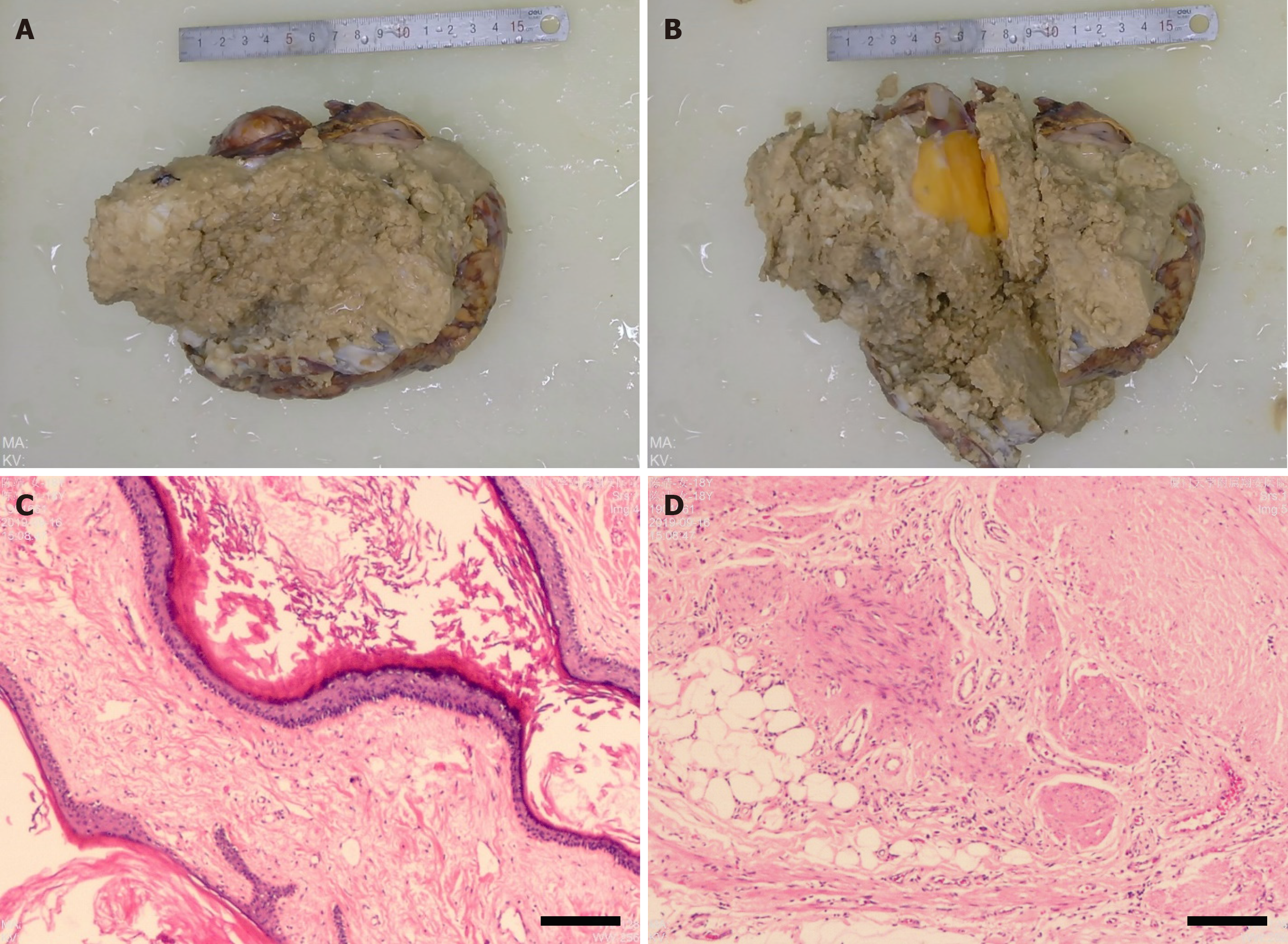
The samples were diagnosed as mature cystic teratoma (retroperitoneal tumor) by postoperative pathologic analysis, with a tumor size of 17 cm × 14 cm × 7 cm. A small amount of adrenal tissue was seen on the lateral side of the tumor.
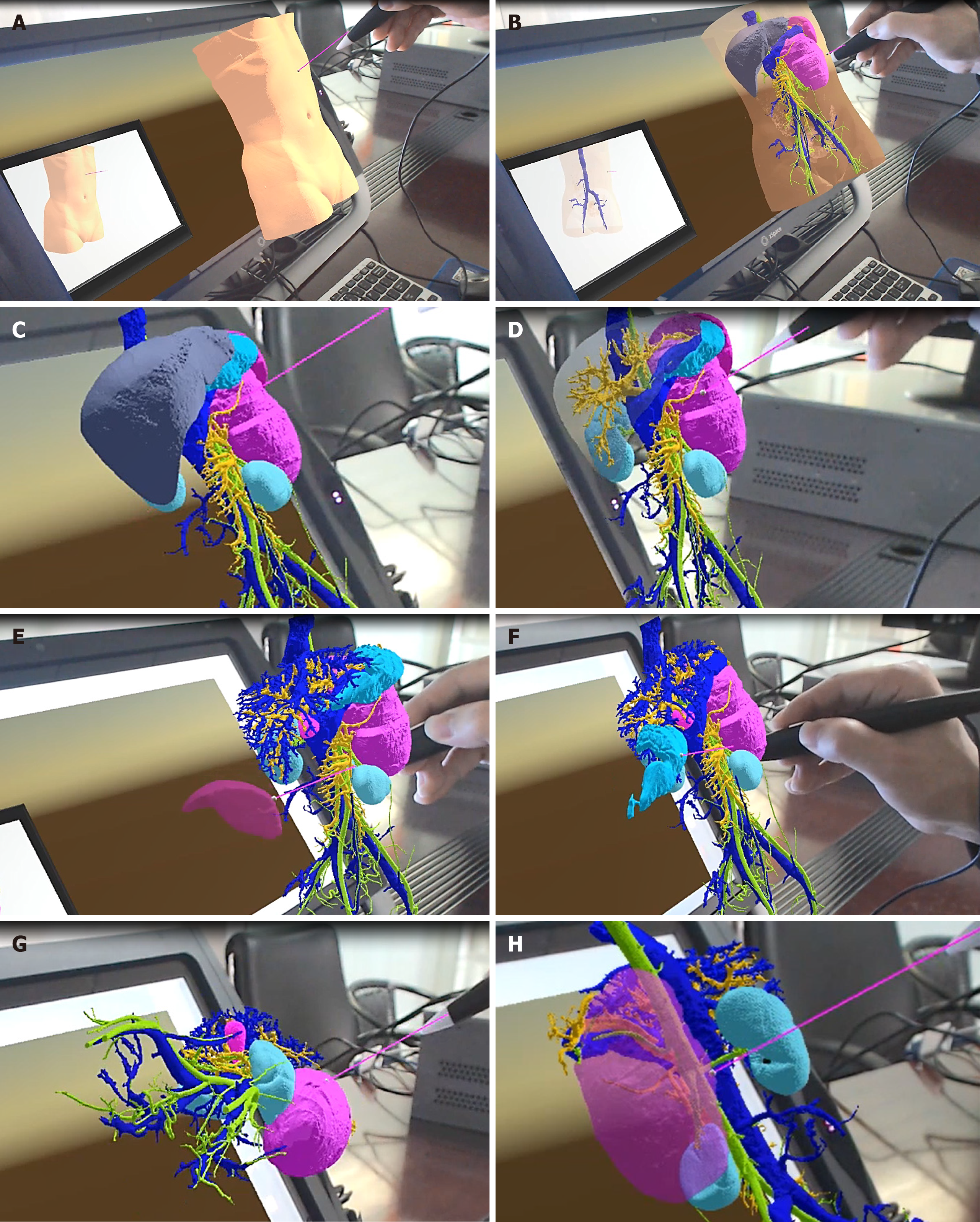
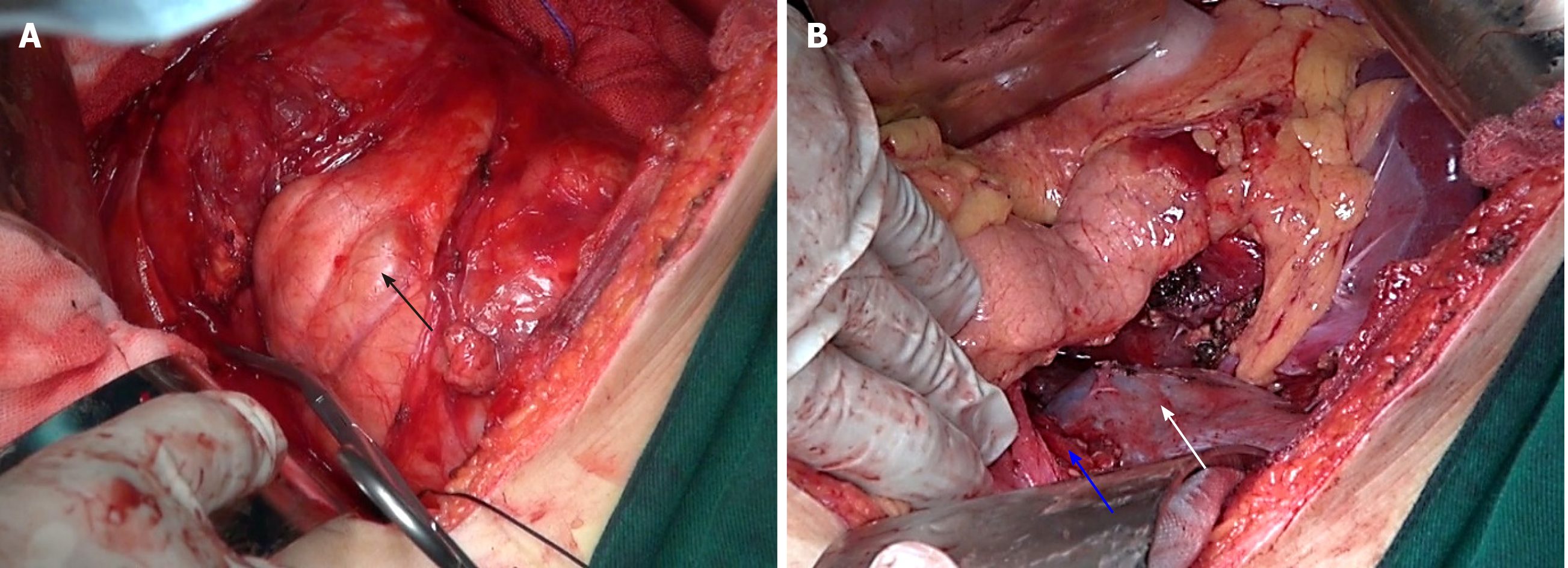
A multidisciplinary team decided on the optimal treatment approach. The 3D model was imported into the VR simulation system. To simulate the surgical resection procedure, the operator wearing the VR helmet directly operated on virtual tissues and organs using a stylus. By VR imaging with multiview observation (Figure 3), we were able to visualize tissues and blood vessels (Figure 3A-C) and removed the normal organs and tumors, simulating the surgical resection process (Figure 3D-H). Retroperitoneal tumor resection along with renal artery reconstruction was decided as the treatment; these were performed on September 12, 2019. After anesthesia and routine skin disinfection, an approximately 20 cm long incision was made around the umbilicus in the middle of the abdomen. The abdominal cavity was thoroughly inspected and was found to be without ascites, while a huge mass about 16 cm × 10 cm in size that could be palpated was found in the upper left abdomen (Figure 4A). The mass adhered to the small intestine and left colon. The upper boundary of the mass was located below the pancreas, the lower boundary was flush with the lower edge of the left kidney, the right side showed clear adhesion to the renal artery and vein, and the left side was bonded to the descending colon. The adhesions were separated using an US knife. The tumor could not be completely separated from the renal artery, which it blocked (Figure 4B). Part of the renal artery was removed and reconstructed with 6-0 stitches. The reconstructed artery had good pulsation. The mass was completely resected from the bottom up (Figure 5A and B). After all surgical instruments and materials were accounted for, the surgical incision was sutured shut. The total surgical time was 120 min. The operation was uneventful, and the volume of blood loss was about 200 mL.
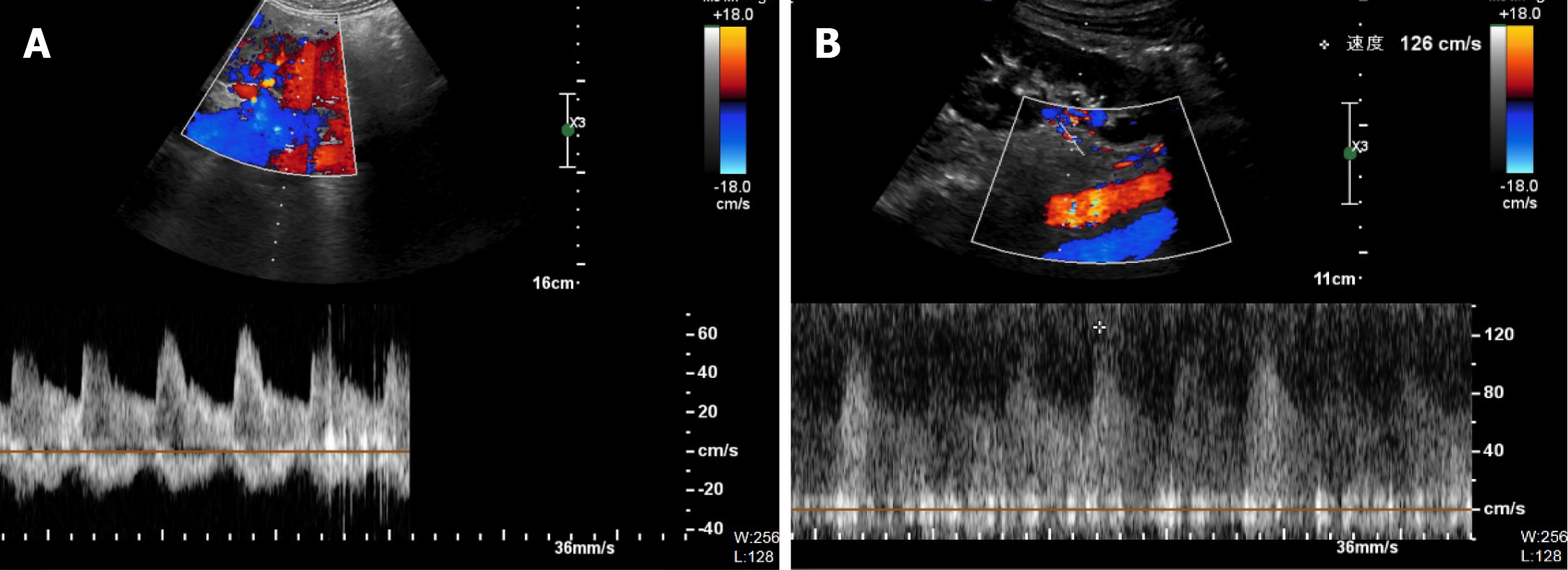
Color Doppler US reexamination showed renal artery patency without blood flow abnormalities (Figure 6A and B). The patient was discharged on September 27, 2019 and is followed up regularly.
Current imaging assessment of retroperitoneal tumors is based on a two-dimensional image that does not show the spatial relationship between the tumor, blood vessels, and other tissues and is therefore not useful for preoperative planning. Exploratory laparotomy is commonly carried out in conventional surgery. However, the procedure mostly relies on the surgeon’s clinical judgments made by naked eye, while superior surgical skills are required in order to avoid hemorrhage or incomplete tumor removal. A 3D model can be constructed on a computer and observed from any angle to determine the relative positions of the tumor, blood vessels, and surrounding organs, thereby enabling more effective surgical preplanning. However, this approach still has limitations because the model can only be examined on a flat monitor. In contrast, VR technology creates a virtual space by importing image data into a simulation system on a computer[7]. Using VR equipment (e.g., a helmet), the surgeon can examine each organ and make virtual contact with the tumor, vessels, and organs. Additionally, tumor removal, combined evisceration, vascular reconstruction, and other operative procedures can be stimulated within the VR environment. Thus, VR technology is an important navigation tool for surgical simulation[8].
3D reconstruction and VR simulation are based on CT images. In each image, different organs are distinguished according to their CT value, and images in each layer are superimposed to generate the 3D model. Therefore, the quality of CT images is very important. Small tissues such as adrenal glands, ureters, and small nerves are more readily visible in high-resolution CT images. Thin-slice CT scanning, which obtains images of multiple sections through the tissue, can also provide a higher resolution view of small tissues. Additionally, enhanced CT allows differentiation of tissues from each organ through comparisons of images obtained at different time points.
VR technology allows simulation of the surgery, but this still differs in many respects from the actual surgery. For instance, the boundary between the tumor and other tissues is relatively clear in the simulation, while in reality the surgery is complicated by limitations of the surgical field, intraoperative hemorrhage, tissue adhesion, and other factors. Additionally, the VR simulation can clearly show relationships between larger tissues but is less accurate for smaller tissues; the latter can only be confirmed in the actual surgery. Finally, blood vessels are static in the VR simulation; during real surgery, separating the tumor from blood vessels is difficult because of the pulsation of large vessels.
A multidisciplinary team[9] can offer different perspectives on the risks associated with the surgery and enhance preoperative preparation, especially when using conventional imaging evaluation assisted by 3D visual reconstruction and VR technology. In our patient, the tumor compressed the left renal artery and vein, resulting in displacement and deformation of the vessels. Using a combination of 3D visual reconstruction and VR technology, the multidisciplinary team was able to determine preoperatively that the renal artery would be challenging to isolate but that reconstruction was possible. Based on these observations and associated analysis, the surgical team prepared for vessel revascularization and prevention of massive hemorrhage in the preoperative planning. During the separation of the renal artery, there was adhesion between the artery and tumor that prevented their clean separation. Renal artery reconstruction was subsequently performed[10]. Our observations during the surgery were generally consistent with the preoperative assessment, and our team achieved complete tumor excision and renal artery reconstruction. The patient recovered well after the operation.
The combination of three-dimensional visualization and virtual reality technology can be used to accurately assess the relationship between the tumor, blood vessels, and surrounding organs. The three-dimensional model was consistent with intraoperative findings. This approach provides a means for simulating the operation before the actual procedure, which can shorten the operation time, reduce the amount of bleeding, and improve the rate of complete tumor resection.
The authors thank Feng-Lin Miao for proposing this investigation; Xue-Min Cai for useful discussions; and Xiao-Cong Chen for carefully proofreading the manuscript.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hussein R, Park BK S-Editor: Zhang H L-Editor: Filipodia P-Editor: Li JH
| 1. | Murez T, Fléchon A, Rocher L, Camparo P, Morel-Journel N, Savoie PH, Ferretti L, Sèbe P, Méjean A, Durand X. [CCAFU french national guidelines 2016-2018 on retroperitoneal sarcoma]. Prog Urol. 2016;27 Suppl 1:S183-S190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Fairweather M, Gonzalez RJ, Strauss D, Raut CP. Current principles of surgery for retroperitoneal sarcomas. J Surg Oncol. 2018;117:33-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 3. | MacNeill AJ, Miceli R, Strauss DC, Bonvalot S, Hohenberger P, Van Coevorden F, Rutkowski P, Callegaro D, Hayes AJ, Honoré C, Fairweather M, Cannell A, Jakob J, Haas RL, Szacht M, Fiore M, Casali PG, Pollock RE, Raut CP, Gronchi A, Swallow CJ. Post-relapse outcomes after primary extended resection of retroperitoneal sarcoma: A report from the Trans-Atlantic RPS Working Group. Cancer. 2017;123:1971-1978. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 105] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 4. | Tzanis D, Bouhadiba T, Gaignard E, Bonvalot S. Major vascular resections in retroperitoneal sarcoma. J Surg Oncol. 2018;117:42-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 5. | Su ZJ, Li WG, Huang JL, Xiao LF, Chen FZ, Wang BL. Pancreaticoduodenectomy assisted by 3-D visualization reconstruction and portal vein arterialization: A case report (a CARE-compliant article). Medicine (Baltimore). 2016;95:e4697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Li C, Cai Y, Wang W, Sun Y, Li G, Dimachkieh AL, Tian W, Sun R. Combined application of virtual surgery and 3D printing technology in postoperative reconstruction of head and neck cancers. BMC Surg. 2019;19:182. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Del Pozo Jiménez G, Rodríguez Monsalve M, Carballido Rodríguez J, Castillón Vela I. Virtual reality and intracorporeal navigation in urology. Arch Esp Urol. 2019;72:867-881. [PubMed] |
| 8. | Mikhail M, Mithani K, Ibrahim GM. Presurgical and Intraoperative Augmented Reality in Neuro-Oncologic Surgery: Clinical Experiences and Limitations. World Neurosurg. 2019;128:268-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 45] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Tseng WW, Seo HJ, Pollock RE, Gronchi A. Historical perspectives and future directions in the surgical management of retroperitoneal sarcoma. J Surg Oncol. 2018;117:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 10. | Radaelli S, Fiore M, Colombo C, Ford S, Palassini E, Sanfilippo R, Stacchiotti S, Sangalli C, Morosi C, Casali PG, Gronchi A. Vascular resection en-bloc with tumor removal and graft reconstruction is safe and effective in soft tissue sarcoma (STS) of the extremities and retroperitoneum. Surg Oncol. 2016;25:125-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |