Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11482
Peer-review started: September 2, 2021
First decision: September 29, 2021
Revised: October 11, 2021
Accepted: November 18, 2021
Article in press: November 18, 2021
Published online: December 26, 2021
Processing time: 112 Days and 5.4 Hours
Fetus-in-fetu (FIF) is an extremely rare congenital abnormal mass, in which a normal fetus’s vertebral axis frequently connected with malformed fetus around this axis. Here, we report the case of a male infant aged 26 d presenting with retroperitoneal parasitic fetus.
In a prenatal examination, we first detected an abdominal mass measuring 7.8 cm × 5.1 cm × 6.8 cm in a mother’s abdomen at 25 gestational weeks and teratoma was suspected. After the fetal was born, we did a magnetic resonance imaging (MRI) and ultrasonography on him and saw a distinctive limb with five-toes. According to the result of MRI, ultrasonography and postoperative pathology, he finally was diagnosed with FIF.
A laparotomy was performed at 26 d of age with excision of the retroperitoneal cystic tumor, which measured about 10 cm in diameter. According to the result of imaging and histological test, FIF was confirmed.
Core Tip: Fetus-in-fetu (FIF) is a rare pediatric disease that many clinicians have not faced. In this case, we summarize the features and antidiastole of FIF with radiology, especially magnetic resonance imaging and ultrasound, cross-sectional ultrasonic imaging helps in differentiating it from teratoma. Clinicians’ preliminary understanding of FIF facilitates to achieve early discovery, early diagnosis, early treatment.
- Citation: Xia B, Li DD, Wei HX, Zhang XX, Li RM, Chen J. Retroperitoneal parasitic fetus: A case report. World J Clin Cases 2021; 9(36): 11482-11486
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11482.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11482
The fetus in fetu (FIF) is a rare congenital anomaly, with an incidence of approximately 1 in 500000 Live births[1]. Less than 190 cases have been reported worldwide (1/4 of them in Asia with an alleged prevalence in males). While the pathogenesis of the disease is not clear, most scholars believe that it is related to abnormal embryonic development, and the two embryos are very different in growth and development. The larger can continue to develop into normal because of adequate placental blood supply, while the smaller is arrested in development and attached to the larger. The most common site of parasitism is the retroperitoneum of the normally developing fetus[2]. However, it can be detected even in the sacral and gonadal regions (8% of cases), and within the skull (8%)[3,4]. The symptoms and signs caused by different parasitic sites are also different. Most FIF increase with the age of the host[5]. The main clinical manifestations of FIF were abdominal mass and compression symptoms such as vomit, dyspepsia, jaundice and urinary retention, as well as fatigue and irritability caused by its metabolites. Because of the low incidence of the disease, clinical and ultrasound doctors are not familiar with it at all.
A gravida came to hospital at 25 gestational weeks because of unusual distended abdomen.
The fetal, one pregnancy and one birth, was pregnant for 36 wk plus 1 d Prenatal ultrasound at 25 wk of gestation revealed an intraperitoneal cystic solid mass in fetal abdomen. After birth, the child was generally in good condition, with normal diet and stool, and no other treatment was performed for the abdominal mass. Later, the patient was admitted to the hospital, and abdominal B-mode ultrasound showed cystic solid mass on the right side of the abdomen.
The patient had no remarkable previous medical history.
The patient had no special personal and family history.
There were no abnormal sounds found through auscultated, no tenderness, no rebound pain and no muscle tension over the abdominal swelling where liver can be reached 1cm below the right rib and spleen is not reached.
The patient had no meaningful laboratory results throughout the examinations.
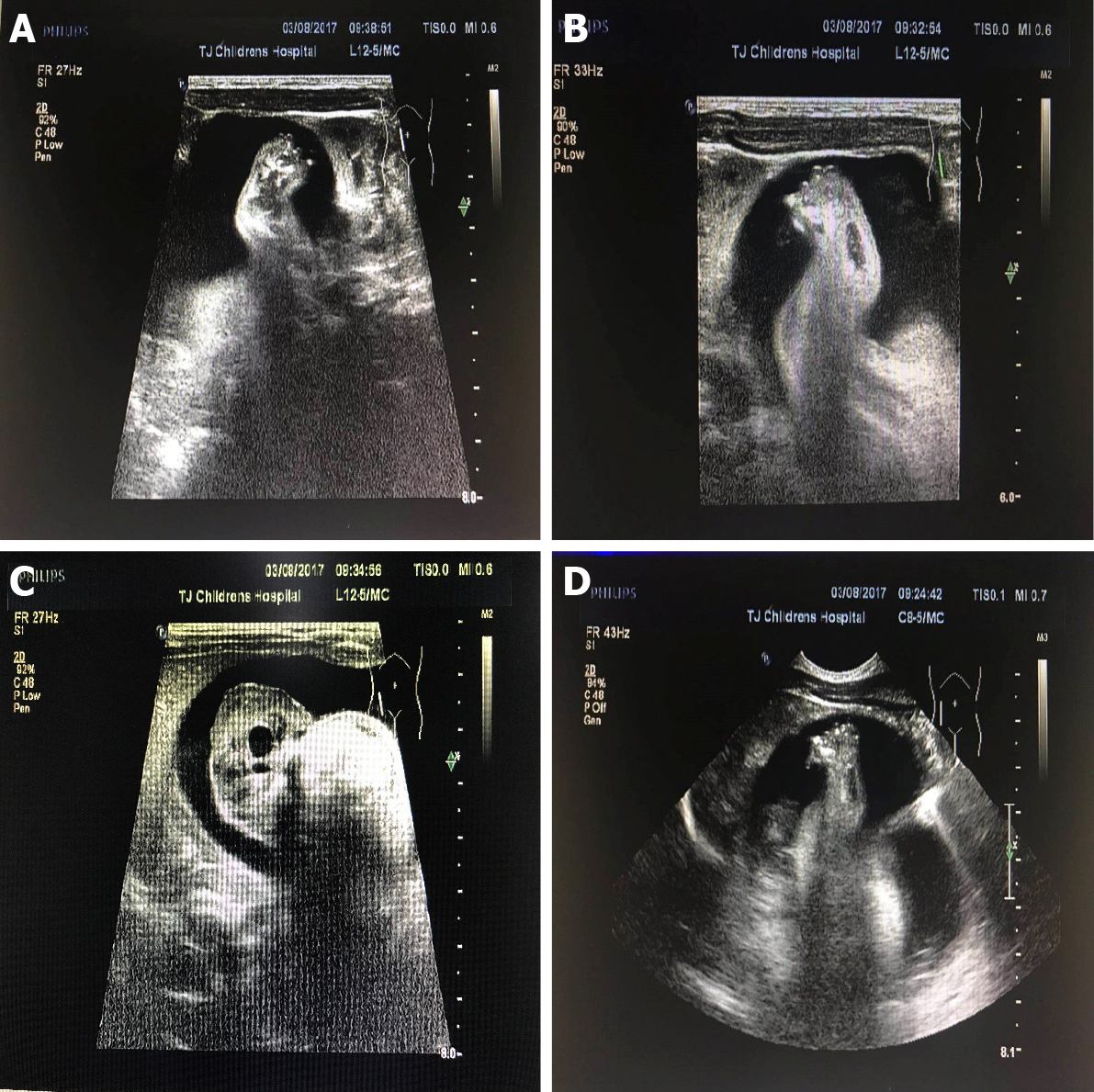
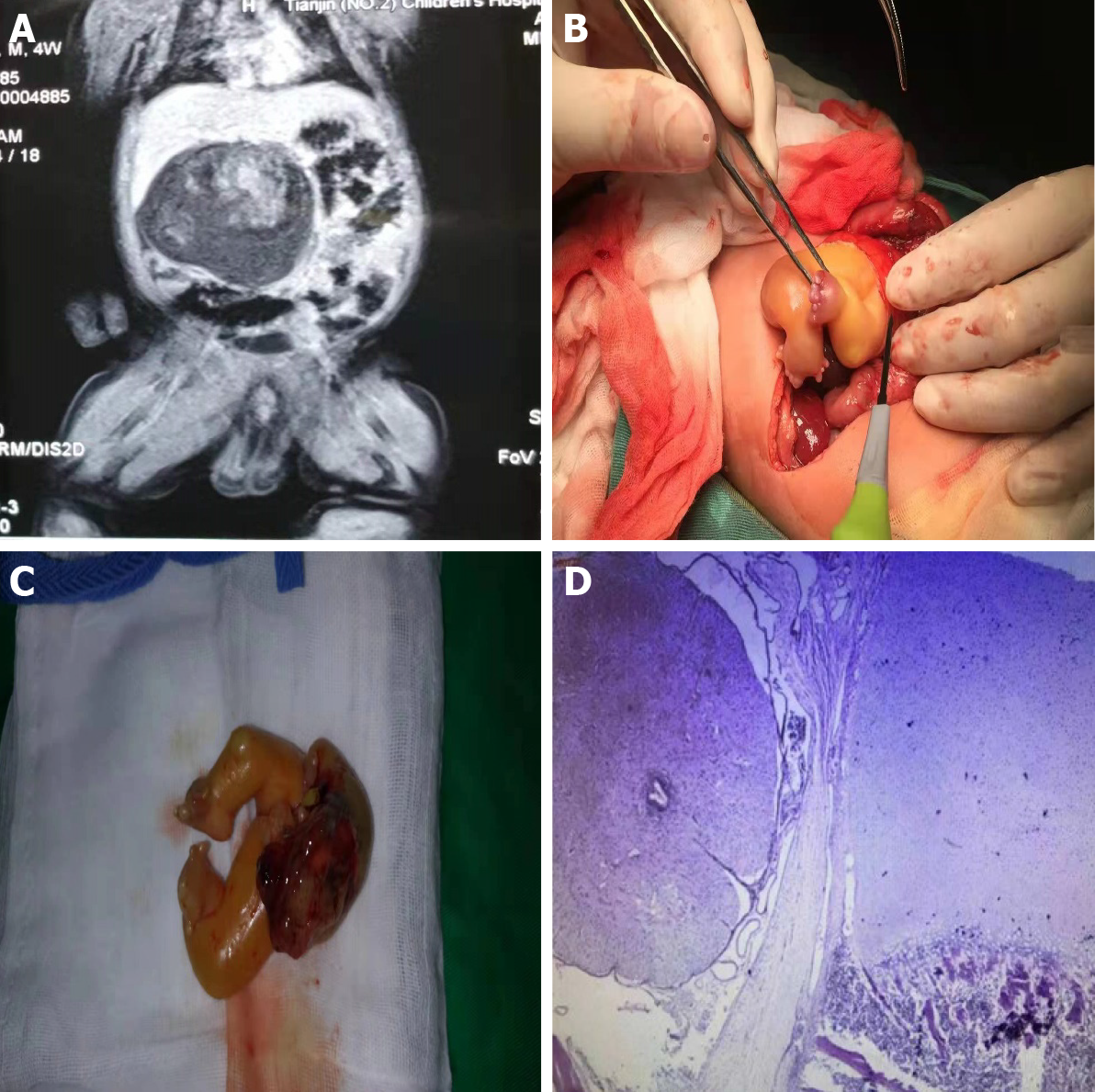
After ultrasonic testing, we found abdominal mass measuring 7.8 cm × 5.1 cm × 6.8 cm on ultrasound image. On imaging, the right midabdomen is dense, with multiple irregular high-density shadows, FIF was considered (Figure 1). On magnetic resonance imaging (MRI), the cystic components in the lesion showed slightly shorter T1 and long T2 signals. Soft tissue, fat signal and short T2 signal shadows were visible in the lesion. The abdominal bowel is compressed and displaced to the left abdominal cystic-solid are mixed signal mass, there was uneven enhancement of some solid components in the right mid-upper abdominal mass, but no enhancement was observed in the cystic part (Figure 2A).
A diagnosis of FIF was finally made.
On laparotomy, the mass that came from retroperitoneum was huge, about 10 cm × 8 cm × 8 cm (Figure 2B and C). There was a complete fetal-like mass with visible lower limbs in the cyst. The FIF has no obvious head or face, un-conspicuous chest and abdomen and no skin covering on the side of head, except bone, cartilage, a little subcutaneous fat and alimentary canal can be found.
Pathologically confirmed it FIF (Figure 2D), On the histopathological examination, the gross specimen showed creatine kinase (+), epithelial membrane antigen (+), desmin (+), glial fibrillary acidic protein (+), S-100 LCA a little (+). Postoperative ultrasound follow-up showed no obvious masses in the abdominal cavity and retroperitoneum.
Imaging plays a very important role in the diagnosis of FIF[6]. However, X-ray is difficult to distinguish the spinal and limb images of FIF, because of the low-density resolution. On computed tomography (CT), the FIF showed irregular shape, well-defined hybrid density, CT values -26.10-216.50 Hus, three-dimensional reconstruction can provide the most intuitive impression. But on CT, children, especially newborns, may bear radiation damage, and sedation is required for the operation, so it has poor reproducibility. MRI can also be used in the diagnosis of FIF[7], which presents a solid and cystic mixed signal mass, with enhancement of the solid portion during enhanced scanning, however, MRI needs long time, children have to take sedatives and further evidence-based medical verification about contrast medium and sedative are not clear, so it is not the first choice. Nicolini et al[8] used prenatal ultrasound examination for the first time in the diagnosis of FIF. Sonographic representation of typical FIF showed a recognizable skeleton echo in the amniotic-like structure in normal fetus’s retroperitoneum[9], partly or completely enveloped by the skin echo, it has a blood supply similar to the umbilical cord and the axial bone system is the most characteristic feature, there may be normal human tissue structure, and other bone structures are often found, such as ribs, limb bones, such as the degree of high differentiation, can even grow into complete organs or limbs. Ultrasound has the advantages of safety, convenience, inexpensive, high repeatability and real-time monitoring of FIF. Meanwhile, ultrasound is the first choice for postoperative follow-up.
From a radiological and surgical perspective, making a preoperative diagnosis and differentiating FIF from the usual and more common congenital mass, teratoma, is important. This is because of the fact that there is an associated 10% chance of malignancy developing in a teratoma whereas FIF is a benign condition. There has been only one report that showed malignant transformation of FIF, to our knowledge[10]. The ultrasonic image of teratoma shows the mixed echo and the boundary is clear, the shape is regular, the fat is contained in the tumor presents the high-level echo, partially or completely covers the cavity. When it has the hair, we can see the spherical or the hemispherical light mass, bone, tooth and cartilage showed high-level echo in the shape of strip, accompanied by acoustic shadow or sound attenuation, and teratoma showing abundant blood signals. As teratoma lacks axonal bone system, it generally can hardly form complete organs or limbs[11]. In addition, old intra-abdominal pregnancy may also present as heterogeneous intra-abdominal echo mass. Some well-developed intra-abdominal pregnancies may also show axial bone system and fetal images of intact limbs, but most of them are found in adult women with a history of menopause, so it can be distinguished by medical history. Generally speaking, when we are faced with abdominal mass, CT or MRI may be the first choice. But In this case we can diagnose it by ultrasound. The picture in ultrasound is very clear. Ultrasound is just a screening before, as the resolution of ultrasonic examination increases, more and more diseases can be diagnose by ultrasound. We even advise ultrasound as the first choice. Due to the lack of understanding of the disease, we want to remind the doctor that ultrasound play an important role in FIF, and a deep understanding of this disease will improve the diagnosis and treatment for clinicians.
To sum up, when we are faced with abdominal mass, firstly we must make sure the location of the mass, in the abdominal cavity or the retroperitoneum. There are some deviations in treatment, and the FIF is a rare congenital disease, which is harmful, especially to the newborn. It should be diagnosed as soon as possible, and totally resected after diagnosis then followed up for a long time.
| 1. | Grant P, Pearn JH. Foetus-in-foetu. Med J Aust. 1969;1:1016-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 2. | Sathe PA, Ghodke RK, Kandalkar BM. Fetus in fetu: an institutional experience. Pediatr Dev Pathol. 2014;17:243-249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Ruffo G, Di Meglio L, Sica C, Resta A, Cicatiello R. Fetus-in-fetu: two case reports. J Matern Fetal Neonatal Med. 2019;32:2812-2819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Hadhri R, Bellalah A. [Retroperitoneal fetus in fetu]. Pan Afr Med J. 2019;34:78. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Sharifah MI, Noryati M, Che Zubaidah CD, Zakaria Z. Foetus-in-Fetu. Med J Malaysia. 2010;65:150-151. [PubMed] |
| 6. | Sitharama SA, Jindal B, Vuriti MK, Naredi BK, Krishnamurthy S, Subramania DB. Fetus in Fetu: Case Report and Brief Review of Literature on Embryologic Origin, Clinical Presentation, Imaging and Differential Diagnosis. Pol J Radiol. 2017;82:46-49. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Parashari UC, Luthra G, Khanduri S, Bhadury S, Upadhyay D. Diagnostic dilemma in a neglected case of fetus-in-fetu solved with Magnetic Resonance Imaging and MDCT--a case report and review of literature. J Radiol Case Rep. 2011;5:29-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Nicolini U, Dell'Agnola CA, Ferrazzi E, Motta G. Ultrasonic prenatal diagnosis of fetus in fetu. J Clin Ultrasound. 1983;11:321-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Ji Y, Chen S, Zhong L, Jiang X, Jin S, Kong F, Wang Q, Li C, Xiang B. Fetus in fetu: two case reports and literature review. BMC Pediatr. 2014;14:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Harigovind D, Babu Sp H, Nair SV, Sangram N. Fetus in fetu - a rare developmental anomaly. Radiol Case Rep. 2019;14:333-336. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Pourang H, Sarmadi S, Mireskandari SM, Soleimani M, Mollaeian M, Alizadeh H, Alehosein SM. Twin fetus in fetu with immature teratoma: a case report and review of the literature. Arch Iran Med. 2009;12:507-510. [PubMed] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: https://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Pediatrics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Katsura D, Oria AP S-Editor: Wang JL L-Editor: A P-Editor: Wang JL