Published online Dec 26, 2021. doi: 10.12998/wjcc.v9.i36.11362
Peer-review started: May 12, 2021
First decision: June 15, 2021
Revised: June 26, 2021
Accepted: July 6, 2021
Article in press: July 6, 2021
Published online: December 26, 2021
Processing time: 209 Days and 23.8 Hours
Mediastinal bronchogenic cysts and pericardial defects are both rare. It is extremely rare that both occur simultaneously. To the best of our knowledge, this is the first case of a coexistent bronchogenic cyst and pericardial defect reported in China. We performed a literature review and found a relationship between bronchogenic cysts and pericardial defects, which further revealed the correlation between the bronchus and pericardium during embryonic development.
A 14-year-old boy attended a local hospital for ankylosing spondylitis. Chest radiography showed an enhanced circular-density shadow near the left mediastinum. The patient had no chest symptoms and the physical examination was normal. Because of the mediastinal occupation, the patient visited our department of chest surgery for further treatment. During surgery, a left pericardial defect was observed. The bronchogenic cyst was removed by thoracoscopic surgery, but the pericardial defect remained untreated, and a satisfactory outcome was achieved after the operation. The patient was diagnosed with a mediastinal tumor. The pathological diagnosis of the tumor was a bronchogenic cyst.
This case further reveals the correlation between the bronchus and pericardium during embryonic development.
Core Tip: Mediastinal bronchogenic cysts coexistent with pericardial defects are extremely rare. Our case revealed the correlation between the bronchus and pericardium during embryonic development. In the early stages of embryonic development, the primitive heart and lungs share a common chamber and are closely linked to each other. A fold is produced in the space between the future pericardium and the pleural cavity, which separates the pleural cavity from the pericardial cavity. If this process is abnormal, bronchogenic cysts or pericardial defects may occur, or both congenital developmental malformations may occur simultaneously.
- Citation: Zhu X, Zhang L, Tang Z, Xing FB, Gao X, Chen WB. Mature mediastinal bronchogenic cyst with left pericardial defect: A case report. World J Clin Cases 2021; 9(36): 11362-11368
- URL: https://www.wjgnet.com/2307-8960/full/v9/i36/11362.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i36.11362
Mediastinal bronchogenic cysts are rare in mediastinal masses. Bronchogenic cysts are mainly detected by chest X-ray or chest computed tomography (CT) scans during physical examinations, without obvious symptoms[1-3]. We here report a rare case of a bronchogenic cyst. The cartilage tissue inside the cyst is mature and structures similar to bronchial bifurcation can be seen. Pericardial defect in such patients is rare. Congenital pericardial defects associated with bronchogenic cysts are even rarer. To our knowledge, this is the first case of a left pericardial defect with a bronchogenic cyst reported in China. The relationship between them was also analyzed through a literature review. Databases including MEDLINE/PubMed and CENTRAL (The Cochrane Central Register of Controlled Trials) were systematically searched up until February 2021 for relevant papers. Search terms included bronchogenic cyst, pericardial defect, absence of pericardium, and mediastinal mass.
A 14-year-old boy attended a local hospital for ankylosing spondylitis. Chest radiography showed an enhanced circular-density shadow near the left mediastinum, which intersected with the mediastinum at an obtuse angle; the base was close to the mediastinum, the outer edge clear and smooth, and the mass density even. A benign lesion was considered. Because of the mediastinal occupation, the patient visited our department of chest surgery for further treatment.
The patient had no previous symptoms.
The patient had no major illness before, and mandatory spondylitis was discovered this time because of his left hip pain.
The patient had no previous symptoms.
The results of the physical examination were normal.
Blood analysis and the blood biochemistries, as well as urine analysis, were all normal. Electrocardiogram and arterial blood gas were also normal.
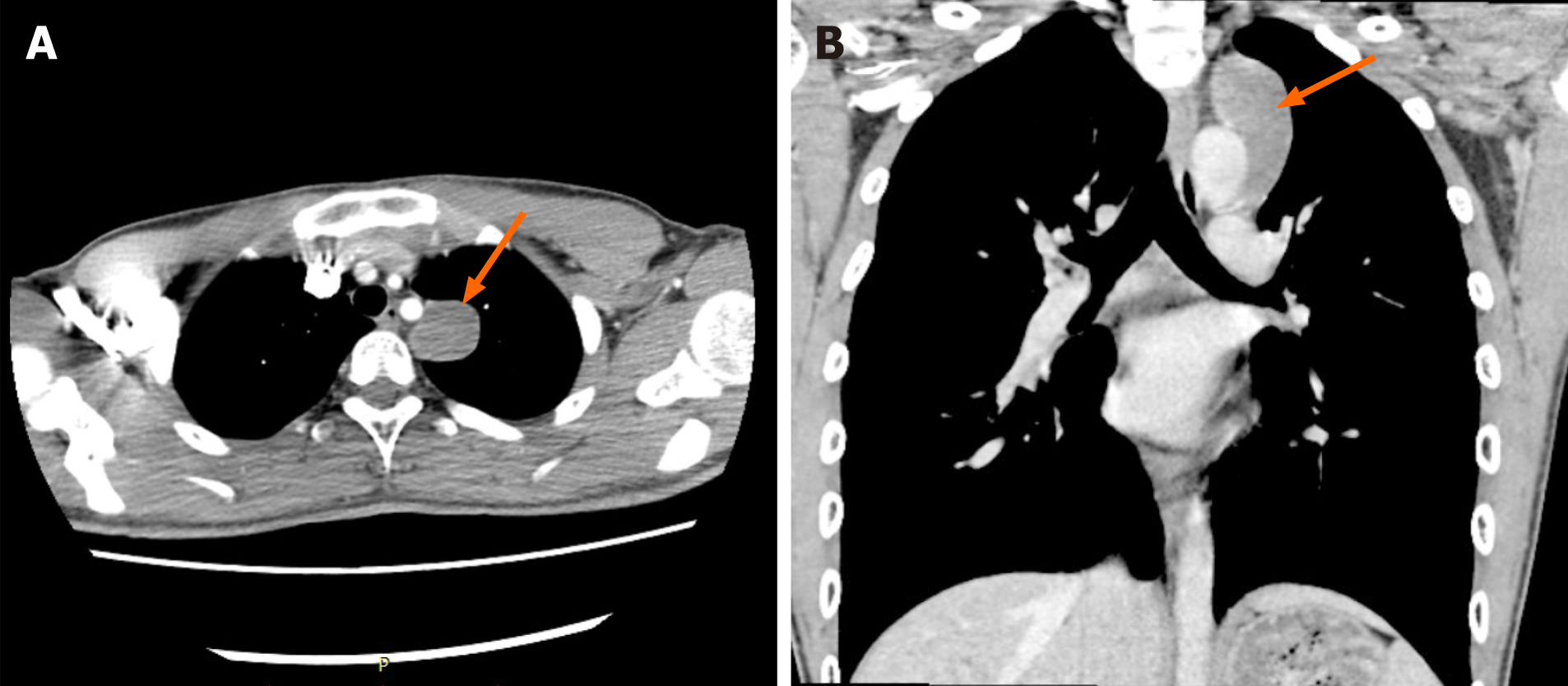
Enhanced chest CT suggested irregular soft tissue density above the left aortic arch with a clear boundary, about 5.5 cm × 3.2 cm × 2.8 cm in size (Figure 1).
The patient was diagnosed with a mediastinal tumor. The pathological diagnosis of the tumor after the operation was a bronchogenic cyst.
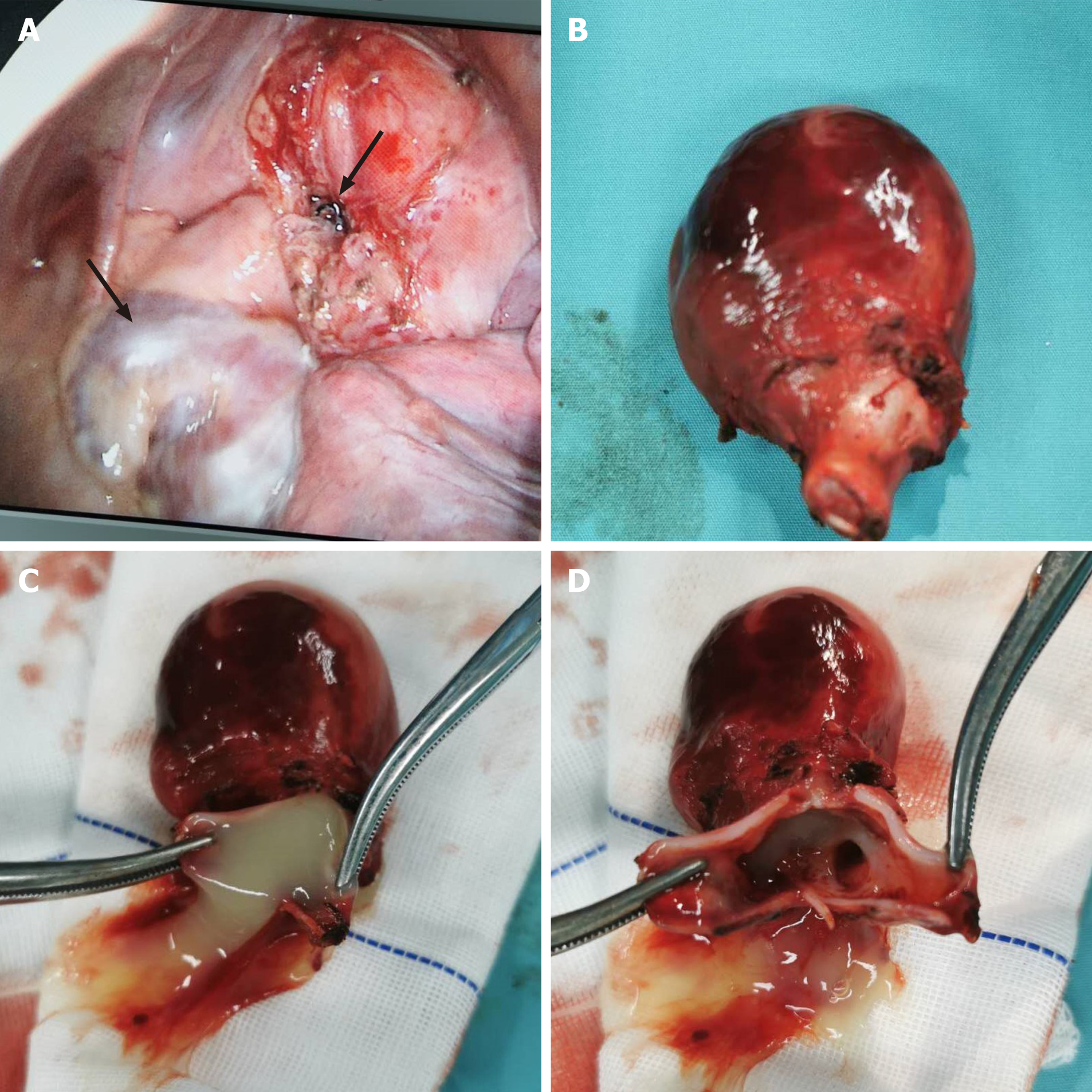
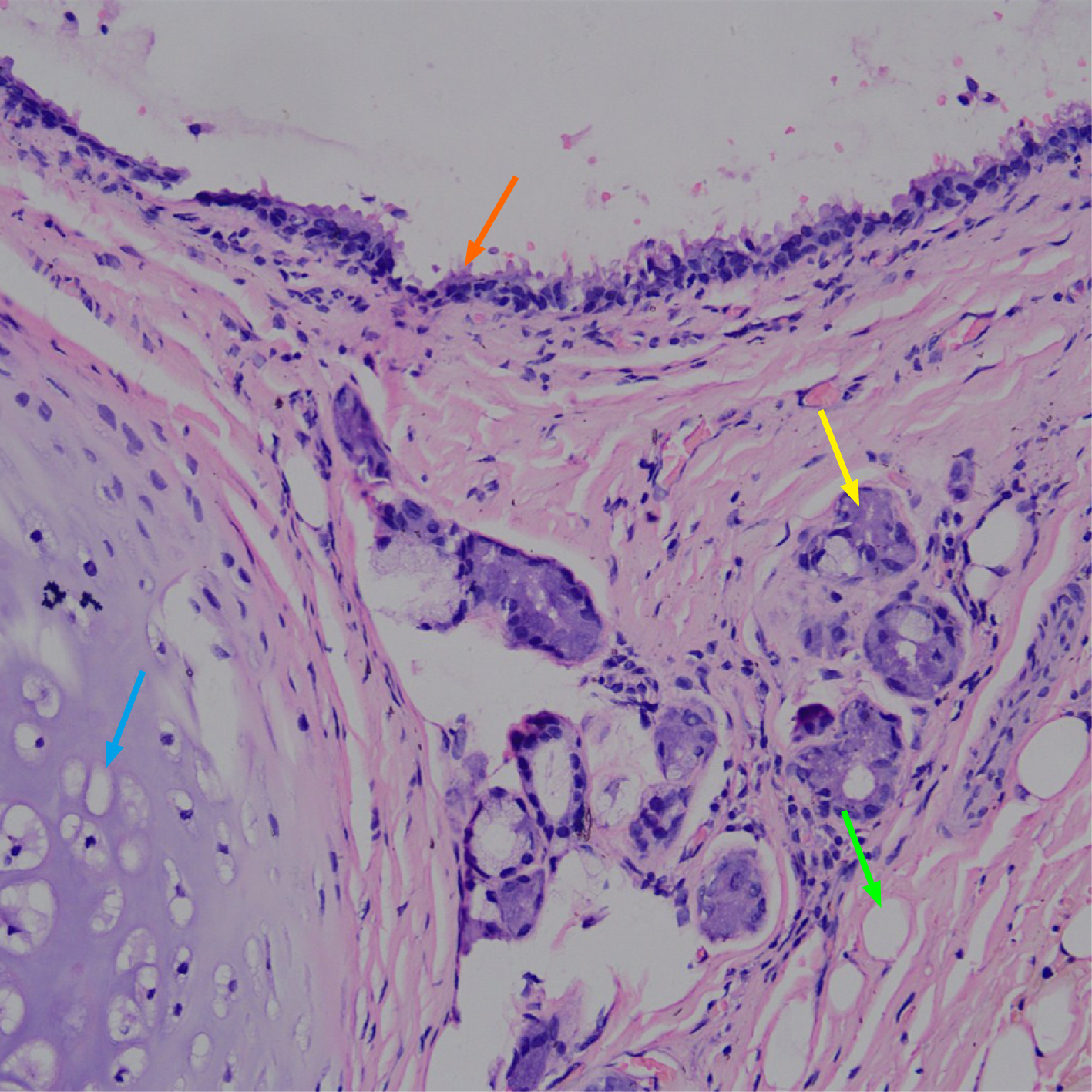
After excluding the contraindications, we performed a video-assisted thoracoscopic resection of the mediastinal mass. During surgery, no obvious adhesion in the left thoracic cavity was observed. The tumor was cystic; it was closely related to the aortic arch, about 4 cm × 4 cm × 4 cm in size. It had a complete envelope, with good activity. At the same time, the left pericardial defect was found, and the left atrium and left atrial appendage of the heart were completely exposed (Figure 2A). We used surgical instruments to lift the tumor and separate it along the lower edge of the tumor, and could see that the pedicle of the tumor was close to the main trachea. We continued to isolate the surrounding tissue of the tumor and lift the tumor outward so as to elongate the pedicle of the tumor. Finally, we used an ultrasound knife to cut the pedicle of the tumor and ligate the broken end of the pedicle. We removed the tumor, and the pedicle end turned out to be solid tissue rather than a lumen structure, and cartilage fragments could be seen from the pedicle (Figure 2B). The tumor contained a large amount of yellow, viscous fluid (Figure 2C), and there was a bronchial bifurcation-like structure inside the tumor (Figure 2D). The pericardial defect was not treated. The pathological diagnosis of the tumor was a bronchial cyst (Figure 3).
The patient recovered well after the operation. Echocardiography was performed 3 wk after the operation, indicating that there was no abnormality in the structure and function of the heart. There was no obvious abnormality in the chest radiography.
Bronchogenic cyst is a type of anterior intestinal cyst, which is known as congenital dysplasia[3]. With regard to the pathogenesis of bronchogenic cysts, the hypothesis of germ shedding and translocation proposed by Sumiyoshi and other scholars has been widely accepted[4]: Bronchogenic cysts are derived from the abnormal germ from the primitive foregut; because of the abnormal germ's different migration time, the location of the bronchogenic cyst formation is different. Bronchogenic cysts are classified into mediastinal, intrapulmonary, and rare ectopic types according to their locations[2,4,5].
The internal cavity of a bronchogenic cyst is irregular, and the ciliated columnar epithelium, smooth muscle, and cartilage can be seen under the microscope[6]. However, the bronchogenic cyst in our patient was dissected and showed an internal bronchial bifurcation-like structure (Figure 2D) rather than irregular sacs of varying sizes. This typical condition is caused by the further development of cartilage tissue in the bronchogenic cyst.
Mediastinal bronchogenic cysts are generally asymptomatic, and it is difficult to distinguish them from other types of mediastinal tumors on imaging grounds. Symptomatic bronchogenic cysts can be treated surgically, but it is not clear whether asymptomatic patients need surgical treatment. In most cases, thoracic surgeons recommend surgery for the following reasons: The growing bronchogenic cyst will increase the difficulty of surgery and lead to the possibility of rupture; complications such as compression symptoms and pleural effusion or infection may occur when the cyst is bleeding or infected[7,8]; on the other hand, the cysts may become malignant tumors[9]. The majority of patients with asymptomatic bronchogenic cysts are young and middle-aged. It can be clearly diagnosed by surgical resection and pathological examination. Thoracoscopic surgery is now the preferred procedure[2,7], which is less traumatic and has a definite effect.
Congenital pericardial defect is rare, with an incidence of about 1/10000-1/14000, usually found by chance in thoracic surgery, autopsy, and imaging studies[10-14]. Lack of part of the pericardium usually does not cause obvious symptoms. A few patients will have atypical chest pain, dyspnea, palpitations, and other manifestations[10-12,15]. There is no significant difference in the life expectancy between patients with congenital pericardial defect and the general population. But if there are critical complications, such as pericardial hernia and large vessel torsion[12,16], surgery is required[17].
At present, it is believed that the premature atrophy of the Cuvier tube at the eighth week of the embryo may lead to the lack of nourishment of the pleural pericardia, leading to developmental disorders[18]. Pericardial partial absence is more common in the left pericardia[19,20]. The same is true for our patient.
Congenital pericardial defect is associated with other congenital deformities of the heart and lung[12,14,16,19], which is not uncommon. These include congenital heart abnormalities such as patent ductus arteriosus, atrial septal defect, mitral stenosis, tetralogy of Fallot, and so on. In addition, there are congenital abnormalities outside the heart, such as bronchogenic cyst reported in this case, as well as pulmonary isolation, and diaphragmatic hernia. Congenital pericardial defect is also associated with abnormal pulmonary anatomy, such as the presence of pulmonary parenchyma between the pulmonary artery and aorta[21]. Imperatori et al[19] has reported 18 cases of bronchogenic cyst with congenital pericardial defect. A number of articles[13,22] suggest that congenital pericardial defects may be related to bronchial cysts. At the fifth week of embryonic development, the bronchial bud develops at the tail end of the larynx and grows into the pericardioperitoneal canal, which is the future pleural cavity; during this period, the primitive heart and lungs share a common chamber and are closely linked to each other[23]. In order to adapt to the growing lung buds, the pleural cavity will continue to grow and expand. A fold called pericardio-pleural membrane is produced in the space between the future pericardium and the pleural cavity, which fuse in the midline and separates the pleural cavity from the pericardial cavity[24]. If this process is abnormal, bronchogenic cysts or pericardial defects may occur, or both congenital developmental malformations may occur simultaneously.
There is a relationship between bronchogenic cysts and pericardial defects. This case further reveals the correlation between the bronchus and pericardium during embryonic development.
We thank all medical staff and technicians who participated in this study.
| 1. | Kozu Y, Suzuki K, Oh S, Matsunaga T, Tsushima Y, Takamochi K. Single institutional experience with primary mediastinal cysts: clinicopathological study of 108 resected cases. Ann Thorac Cardiovasc Surg. 2014;20:365-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Jung HS, Kim DK, Lee GD, Sim HJ, Choi SH, Kim HR, Kim YH, Park SI. Video-assisted thoracic surgery for bronchogenic cysts: is this the surgical approach of choice? Interact Cardiovasc Thorac Surg. 2014;19:824-829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Takeda S, Miyoshi S, Minami M, Ohta M, Masaoka A, Matsuda H. Clinical spectrum of mediastinal cysts. Chest. 2003;124:125-132. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 183] [Cited by in RCA: 155] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 5. | Maurin S, Hery G, Bourliere B, Potier A, Guys JM, Lagausie PD. Bronchogenic cyst: Clinical course from antenatal diagnosis to postnatal thoracoscopic resection. J Minim Access Surg. 2013;9:25-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Biyyam DR, Chapman T, Ferguson MR, Deutsch G, Dighe MK. Congenital lung abnormalities: embryologic features, prenatal diagnosis, and postnatal radiologic-pathologic correlation. Radiographics. 2010;30:1721-1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 145] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Guo C, Mei J, Liu C, Deng S, Pu Q, Lin F, Liu L. Video-assisted thoracic surgery compared with posterolateral thoracotomy for mediastinal bronchogenic cysts in adult patients. J Thorac Dis. 2016;8:2504-2511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Ueda K, Yanagawa M, Ueguchi T, Satoh Y, Kawai M, Gyobu T, Sumikawa H, Honda O, Tomiyama N. Paradoxical signal pattern of mediastinal cysts on T2-weighted MR imaging: phantom and clinical study. Eur J Radiol. 2014;83:1016-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Taira N, Kawasaki H, Atsumi E, Ichi T, Kawabata T, Saio M, Yoshimi N. Mucoepidermoid Carcinoma of Arising from a Bronchogenic Cyst of the Diaphragm. Ann Thorac Cardiovasc Surg. 2018;24:247-250. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Macaione F, Barison A, Pescetelli I, Pali F, Pizzino F, Terrizzi A, Di Lisi D, Novo G, Todiere G, Assennato P, Novo S, Aquaro GD. Quantitative criteria for the diagnosis of the congenital absence of pericardium by cardiac magnetic resonance. Eur J Radiol. 2016;85:616-624. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Steinberg C, Pelletier MJ, Perron J, Kumar A, Champagne J. Sudden cardiac arrest due to subtotal absence of left-sided pericardium--case report and review of the literature. Congenit Heart Dis. 2013;8:E92-E98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Shah AB, Kronzon I. Congenital defects of the pericardium: a review. Eur Heart J Cardiovasc Imaging. 2015;16:821-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 80] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 13. | Hiraoka K, Yamazaki S, Hosokawa M, Suzuki Y. Bronchogenic cyst associated with congenital absence of the pericardium. J Surg Case Rep. 2015;2015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Van Son JA, Danielson GK, Schaff HV, Mullany CJ, Julsrud PR, Breen JF. Congenital partial and complete absence of the pericardium. Mayo Clin Proc. 1993;68:743-747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 87] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 15. | Palau P, Domínguez E, García-González P, Gallego J, Bosch MJ, Sieso E. Isolated Partial Congenital Absence of the Pericardium: A Familial Presentation. Can J Cardiol. 2016;32:1039.e1-1039.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Verde F, Johnson PT, Jha S, Fishman EK, Zimmerman SL. Congenital absence of the pericardium and its mimics. J Cardiovasc Comput Tomogr. 2013;7:11-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | BRUNING EG. Congenital defect of the pericardium. J Clin Pathol. 1962;15:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 45] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Tubbs OS, Yacoub MH. Congenital pericardial defects. Thorax. 1968;23:598-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Imperatori A, Rotolo N, Nardecchia E, Mariscalco G, Spagnoletti M, Dominioni L. Bronchogenic cyst associated with pericardial defect: case report and review of the literature. J Cardiothorac Surg. 2011;6:85. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Rajiah P, Kanne JP. Computed tomography of the pericardium and pericardial disease. J Cardiovasc Comput Tomogr. 2010;4:3-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Sergio P, Bertella E, Muri M, Zangrandi I, Ceruti P, Fumagalli F, Bosio G. Congenital absence of pericardium: two cases and a comprehensive review of the literature. BJR Case Rep. 2019;5:20180117. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 22. | Kamata T, Yoshida S, Iwata T, Nakatani Y, Yoshino I. Giant bronchogenic cyst with pericardial defect: a case report & literature review in Japan. J Thorac Dis. 2016;8:E684-E688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Moore KL, Persaud TV. The Developing Human: clinically oriented embryology. 10th ed. Philadelphia: Elsevier, 2016: 200-201. |
| 24. | Eom DW, Kang GH, Kim JW, Ryu DS. Unusual bronchopulmonary foregut malformation associated with pericardial defect: bronchogenic cyst communicating with tubular esophageal duplication. J Korean Med Sci. 2007;22:564-567. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Respiratory system
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Exbrayat JM S-Editor: Yan JP L-Editor: Wang TQ P-Editor: Zhang YL