Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9977
Peer-review started: June 19, 2021
First decision: July 5, 2021
Revised: July 11, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: November 16, 2021
Processing time: 143 Days and 12.8 Hours
Focal nodular hyperplasia (FNH) commonly occurs in women; it is usually asymptomatic and sometimes difficult to differentiate from hepatocellular carcinoma (HCC).
A large space-occupying lesion in the right lobe of the liver was incidentally detected in an adult man and diagnosed as HCC. Transcatheter arterial chemoembolization was applied once monthly for 2 years, but the lesion did not decrease in size. It was revealed by biopsy to be FNH. Eleven years later, the patient underwent liver resection due to hemorrhage and the pathological examination confirmed FNH.
For a space-occupying lesion, it is prerequisite to pathologically confirm the diagnosis and the corresponding intervention can be effective.
Core Tip: We report a case of large focal nodular hyperplasia that was pre-emptively diagnosed by a physician as hepatocellular carcinoma. Consequently, the management was incorrect and ineffective, which raises an alert for all clinicians.
- Citation: Ren H, Gao YJ, Ma XM, Zhou ST. Large focal nodular hyperplasia is unresponsive to arterial embolization: A case report. World J Clin Cases 2021; 9(32): 9977-9981
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9977.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9977
Focal nodular hyperplasia (FNH) is defined by proliferating hepatocytes reinstituting 1–2-cell-thick plates with a multinodular pattern separated by stellate central fibrous scar surrounded with a dystrophic arteriole[1]. It is the second most frequent benign liver nodule after hemangioma and it has been reported to occur in about 3% of the general population and in women in their 30s and 40s. Its accurate etiology remains unknown. These lesions are usually asymptomatic and detected serendipitously on imaging examination, autopsy or surgery for unrelated symptoms[2,3]. Clinical recognition of FNH and FNH-like lesions is important for their management because they are sometimes difficult to differentiate from hepatic adenoma and hepatocellular carcinoma (HCC) with radiology or ultrasound, and FNH itself is not a premalignant disease[4]. In our case, FNH was present as a large lesion that was misdiagnosed and the patient underwent unwarranted intervention.
The patient felt discomfort in the right upper quadrant of the abdomen and received physical examination.
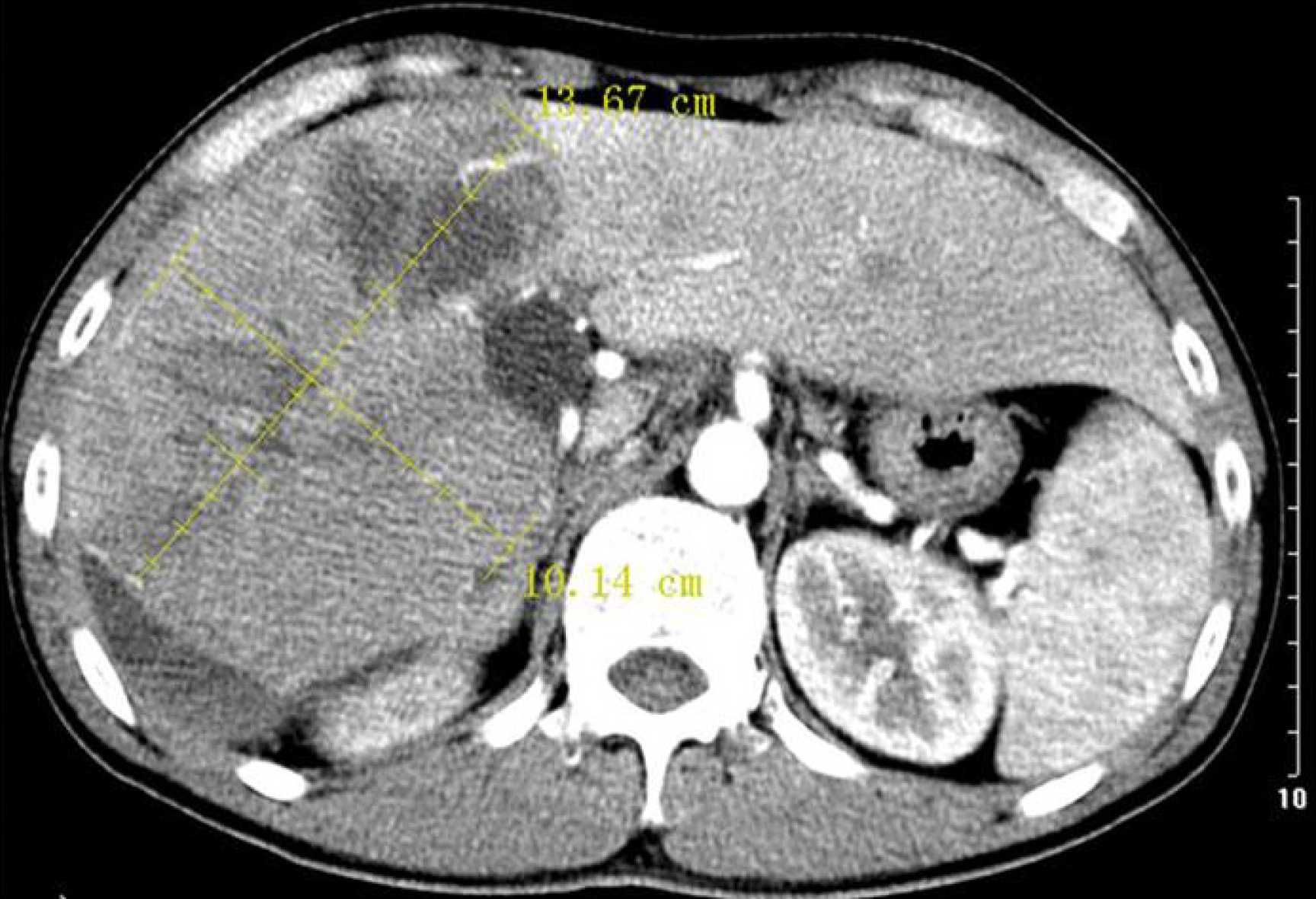
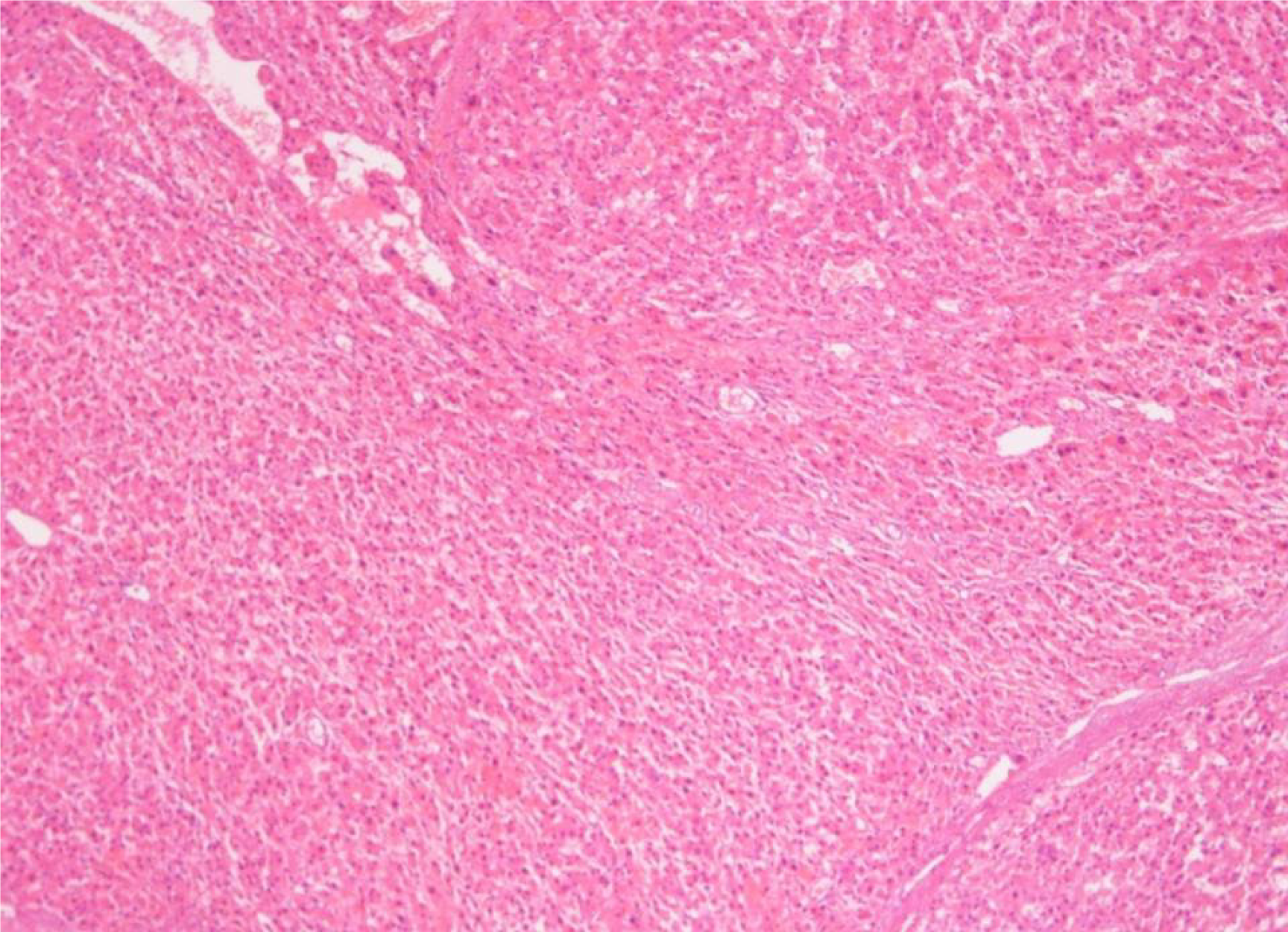
In 2005, a space-occupying lesion measuring 10.1 cm × 10.0 cm in the right lobe of the liver was detected in a 34-year-old man through multiphase computed tomography (CT) due to discomfort in the right upper quadrant of the abdomen. CT imaging showed multiple cystic low-density lesions heterogeneously enhanced in the arterial phase with delayed portal washout, and splenomegaly, which was confirmed by magnetic resonance imaging (MRI). Liver functions and α-fetoprotein level were within normal limits; all viral hepatitis and autoimmune biomarker panels were negative and no history of alcohol consumption was noted. HCC was then suspected preferably at the discretion of the first clinician. The patient visited many tertiary care units. Biopsy was denied for fear of tumor seeding along the needle track. Due to unexpected surgery and the large lesion, the patient received transcatheter arterial chemoembolization (TACE) once monthly, recommended by the first clinician, for a total 22 times within 2 years, but the size of the lesion was not changed. In 2008, liver biopsy revealed FNH but did not exclude well-differentiated HCC. Transarterial embolization is a feasible treatment strategy for FNH, which was unresponsive in this patient. In 2016, hepatectomy was performed due to hemorrhage in the lesion. Postoperative pathology determined low-grade FNH with a size of 13.6 cm × 10.5 cm (Figures 1 and 2).
No special history of past illness was reported.
No special personal and family history was reported.
No finding on physical examination was revealed.
Liver functions and α-fetoprotein level were within normal limits, and all viral hepatitis and autoimmune biomarker panels were negative.
CT and MRI showed multiple cystic low-density lesions heterogeneously enhanced in the arterial phase with delayed portal washout and splenomegaly.
HCC was diagnosed at the discretion of the first physician, but later FNH was confirmed.
TACE was applied once monthly, 22 times in total, and 11 years later, the patient underwent hepatectomy.
Currently, the patient has been well for 5 years on regular follow-up. This study was approved by the Ethics Committee of The Fifth Medical Center, Chinese People’s Liberation Army General Hospital and informed consent was received for publication of the case.
FNH is not a rare disease in the general population but its pathophysiology is still elusive[5]. In China, FNH is detected in adult men or children, and is solitary in most cases[2,6]. FNH lesions are generally asymptomatic and are therefore discovered fortuitously during autopsy, or imaging examinations for unrelated symptoms. It progresses insidiously and it is difficult to distinguish precisely between FNH and HCC, even with modern advanced imaging technology, especially for small lesions[7,8].
On evaluation of a solid hepatic tumor, a benign lesion must be taken into account when serum fetoprotein level is normal and viral hepatitis tests are negative. Final diagnosis of the space-occupying lesion must be made cautiously, and any pre-emptive decision will surely have a negative impact on subsequent management. Although CT or MRI allows accurate diagnosis in most cases, pathological confirm
Management of FNH is controversial because its etiology and pathophysiology are not fully understood[11]. It has been reported that transarterial embolization, preferably applied as a less-invasive tumor ablation technique, is a good option in the management of a variety of liver lesions since it is a hyperplastic response of the hepatic parenchyma to pre-existing arterial malformations, especially for small FNH[12,13]. When symptoms are continuously present or complications like hemorrhage occur due to the larger lesion or chronic course, the blood supply from the dual systems precludes transarterial embolization or TACE, surgery can be first-line treatment option. FNH itself is a benign disease and it does not require radical treatment unless symptoms persist or complications occur.
Pathologically confirmed diagnosis is prerequisite for space-occupying lesions and results in effective management.
| 1. | Nault JC, Bioulac-Sage P, Zucman-Rossi J. Hepatocellular benign tumors-from molecular classification to personalized clinical care. Gastroenterology. 2013;144:888-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 196] [Article Influence: 15.1] [Reference Citation Analysis (0)] |
| 2. | Cannella R, Rangaswamy B, Minervini MI, Borhani AA, Tsung A, Furlan A. Value of Texture Analysis on Gadoxetic Acid-Enhanced MRI for Differentiating Hepatocellular Adenoma From Focal Nodular Hyperplasia. AJR Am J Roentgenol. 2019;212:538-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Balabaud C, Al-Rabih WR, Chen PJ, Evason K, Ferrell L, Hernandez-Prera JC, Huang SF, Longerich T, Park YN, Quaglia A, Schirmacher P, Sempoux C, Thung SN, Torbenson M, Wee A, Yeh MM, Yeh SH, Le Bail B, Zucman-Rossi J, Bioulac-Sage P. Focal Nodular Hyperplasia and Hepatocellular Adenoma around the World Viewed through the Scope of the Immunopathological Classification. Int J Hepatol. 2013;2013:268625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 39] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Bonney GK, Gomez D, Al-Mukhtar A, Toogood GJ, Lodge JP, Prasad R. Indication for treatment and long-term outcome of focal nodular hyperplasia. HPB (Oxford). 2007;9:368-372. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Amesur N, Hammond JS, Zajko AB, Geller DA, Gamblin TC. Management of unresectable symptomatic focal nodular hyperplasia with arterial embolization. J Vasc Interv Radiol. 2009;20:543-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Jung JM, Hwang S, Kim KH, Ahn CS, Moon DB, Ha TY, Song GW, Jung DH. Surgical indications for focal nodular hyperplasia of the liver: Single-center experience of 48 adult cases. Ann Hepatobiliary Pancreat Surg. 2019;23:8-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Choi JY, Lee HC, Yim JH, Shim JH, Lim YS, Shin YM, Yu ES, Suh DJ. Focal nodular hyperplasia or focal nodular hyperplasia-like lesions of the liver: a special emphasis on diagnosis. J Gastroenterol Hepatol. 2011;26:1004-1009. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Chen YJ, Chen PJ, Lee MC, Yeh SH, Hsu MT, Lin CH. Chromosomal analysis of hepatic adenoma and focal nodular hyperplasia by comparative genomic hybridization. Genes Chromosomes Cancer. 2002;35:138-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 27] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Navarro AP, Gomez D, Lamb CM, Brooks A, Cameron IC. Focal nodular hyperplasia: a review of current indications for and outcomes of hepatic resection. HPB (Oxford). 2014;16:503-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Perrakis A, Vassos N, Grützmann R, Croner RS. What is Changing in Indications and Treatment of Focal Nodular Hyperplasia of the Liver. Is There Any Place for Surgery? Ann Hepatol. 2017;16:333-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Laxague F, Ramallo D, McCormack L. Near-Complete Disappearance of a Giant Focal Nodular Hyperplasia in the Liver. Clin Gastroenterol Hepatol. 2021;19:e34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Zhang G, Wang M, Duan F, Yuan K, Li K, Yan J, Chang Z. Transarterial embolization with bleomycin for symptomatic hepatic focal nodular hyperplasia. Diagn Interv Radiol. 2017;23:66-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Fukukura Y, Nakashima O, Kusaba A, Kage M, Kojiro M. Angioarchitecture and blood circulation in focal nodular hyperplasia of the liver. J Hepatol. 1998;29:470-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 63] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chen Y S-Editor: Chang KL L-Editor: Kerr C P-Editor: Li JH