Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9917
Peer-review started: July 5, 2021
First decision: August 9, 2021
Revised: August 25, 2021
Accepted: September 26, 2021
Article in press: September 26, 2021
Published online: November 16, 2021
Processing time: 127 Days and 22.7 Hours
Colorectal cancer (CRC) is one of the most common malignant tumors of the digestive tract. Lymphatic metastases of this tumor are mostly confined to the regional lymph nodes, and distant supraclavicular lymph node metastases are very rare.
In this report, we describe a patient with sigmoid carcinoma and isolated synchronous supraclavicular lymph node metastases. A 56-year-old male presented with a left cervical mass that was confirmed as a lymph node metastasis from sigmoid cancer by several auxiliary examinations. After 6 cycles of chemotherapy with the 5-fluorouracil, leucovorin and oxaliplatin + cetuximab regimen, the sigmoid colon tumor and Virchow’s lymph node metastasis were significantly smaller than before treatment, and no new metastatic sites were observed. Considering the effects of chemotherapy on quality of life, resection of the primary tumor was performed followed by 4 cycles of chemotherapy with the original chemotherapy regimen. Virchow’s lymph node dissection was selected by mutual consultation between the patient and us. After the second surgery, the patient received capecitabine and cetuximab chemotherapy and did not experience recurrence or metastasis during follow-up.
In conclusion, supraclavicular lymph node metastasis without any other solid organ metastasis is a potential metastatic pathway for CRC. In addition, after resection of the primary lesion, postoperative chemotherapy combined with supraclavicular lymph node dissection is feasible for the treatment of patients with CRC and isolated synchronous Virchow’s lymph node metastases.
Core Tip: A 56-year-old male presented with Virchow lymph node metastasis of sigmoid cancer. We treated the primary tumor and metastatic lymph nodes with chemotherapy combined with surgery. No recurrence or metastasis occurred during the follow-up period. According to our findings, supraclavicular lymph node metastasis without any other solid organ metastasis may be a potential metastatic pathway for colorectal cancer (CRC). In addition, after resection of the primary lesion, postoperative chemotherapy combined with supraclavicular lymph node dissection is feasible in the treatment of patients with CRC and isolated synchronous Virchow lymph node metastases.
- Citation: Yang JQ, Shang L, Li LP, Jing HY, Dong KD, Jiao J, Ye CS, Ren HC, Xu QF, Huang P, Liu J. Isolated synchronous Virchow lymph node metastasis of sigmoid cancer: A case report. World J Clin Cases 2021; 9(32): 9917-9925
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9917.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9917
Colorectal cancer (CRC) is one of the most common malignant tumors of the digestive tract[1]. CRC frequently metastasizes to the regional lymph nodes, liver, lung, and peritoneum[2]. CRC with distant lymph node site metastasis is rare, and synchronous distant lymph node metastasis from CRC without any other solid organ metastasis is extremely rare. Therefore, we report the case of a patient with sigmoid colon cancer who presented with isolated simultaneous Virchow’s lymph node metastasis.
A 56-year-old male presented with a left cervical mass that had been present for one month.
The patient's left cervical mass was incidentally discovered and no other clinical manifestations.
The patient was previously diagnosed with diabetes and took oral hypoglycemic drugs for control of blood glucose level.
The patient lived in Jining, China. He did not smoke and was not addicted to alcohol. No relevant family history was reported.
Physical examination revealed a solid small peanut-sized mass in the left supraclavicular region.
The laboratory assessment revealed that carcinoembryonic antigen (CEA), CA199, and CA724 serum levels were moderately elevated.
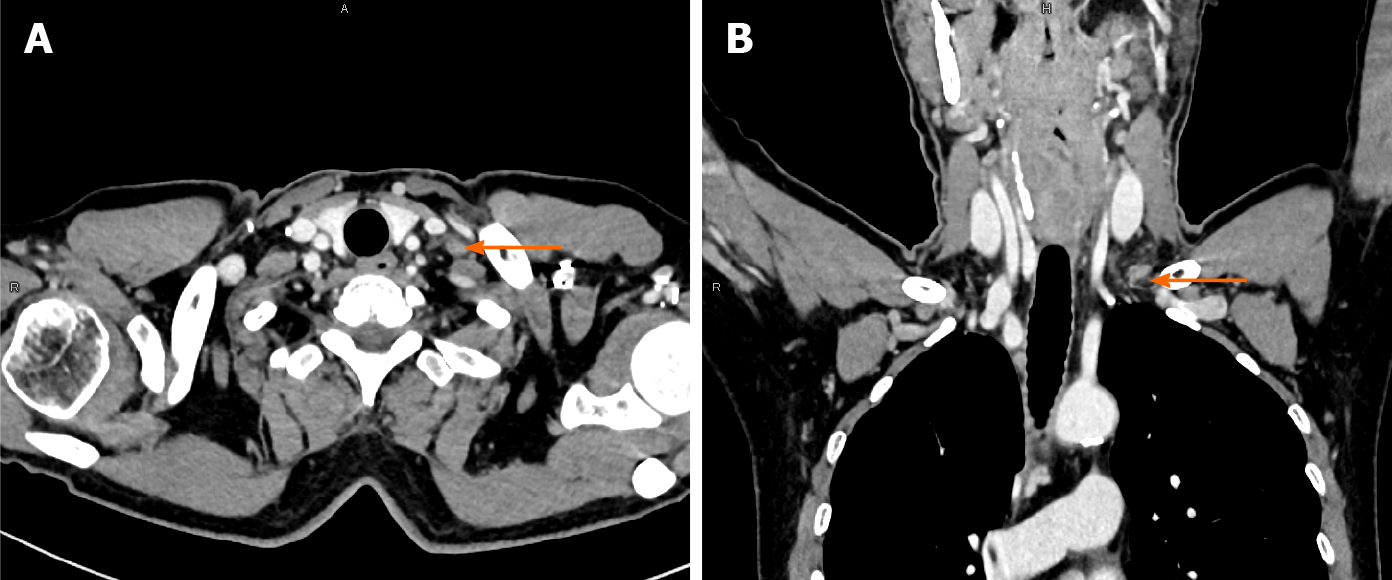
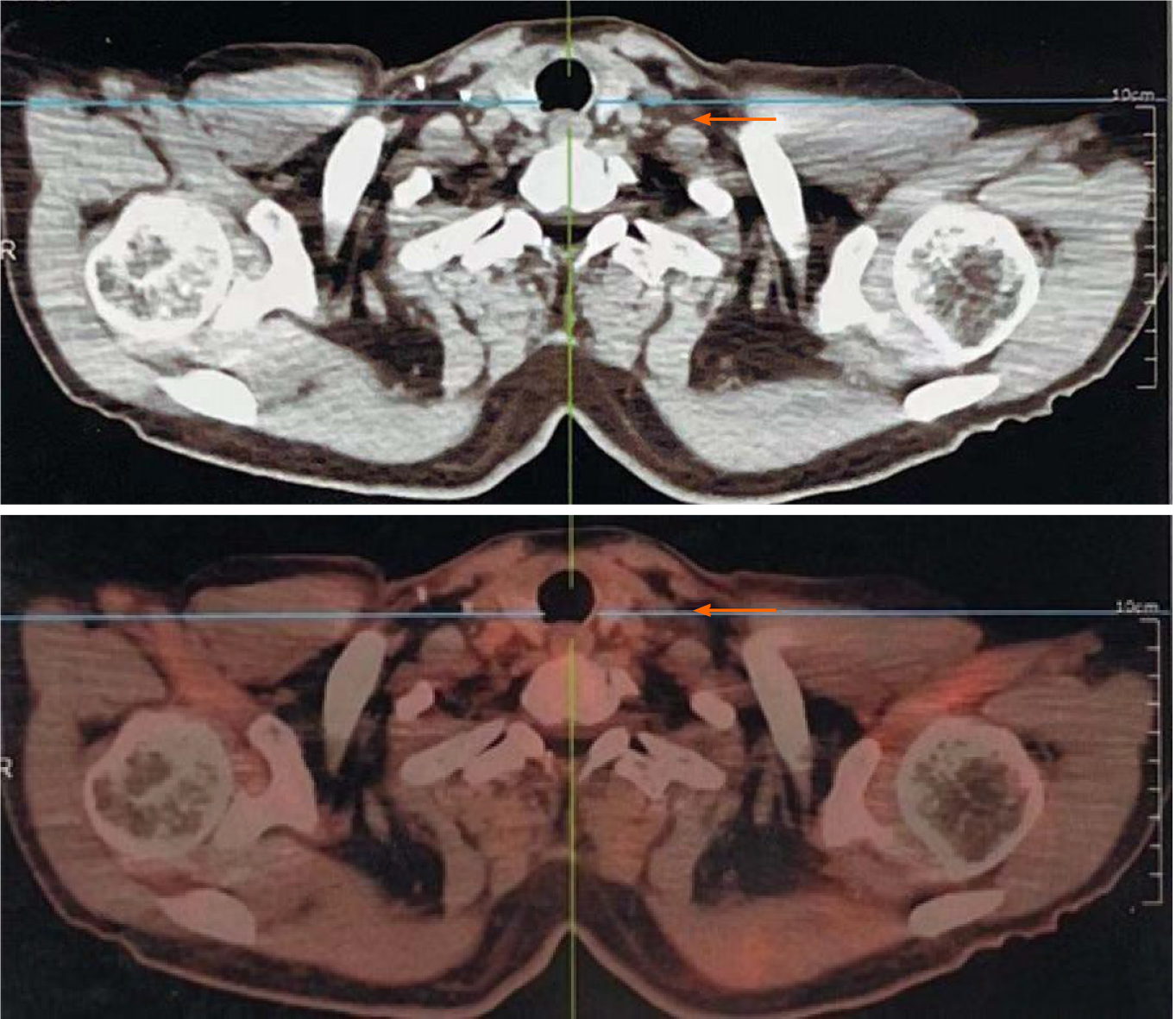
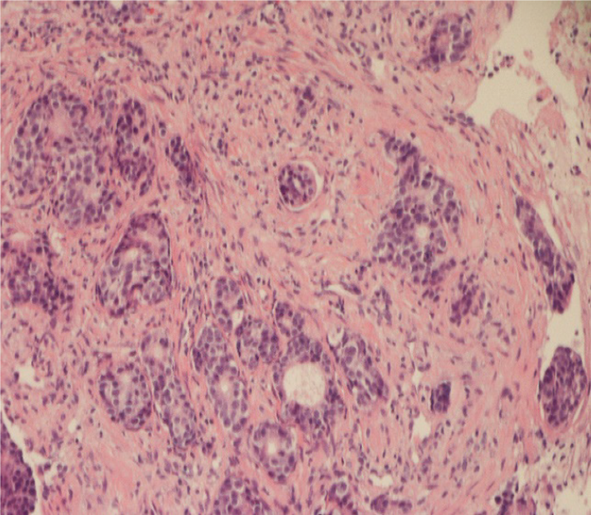
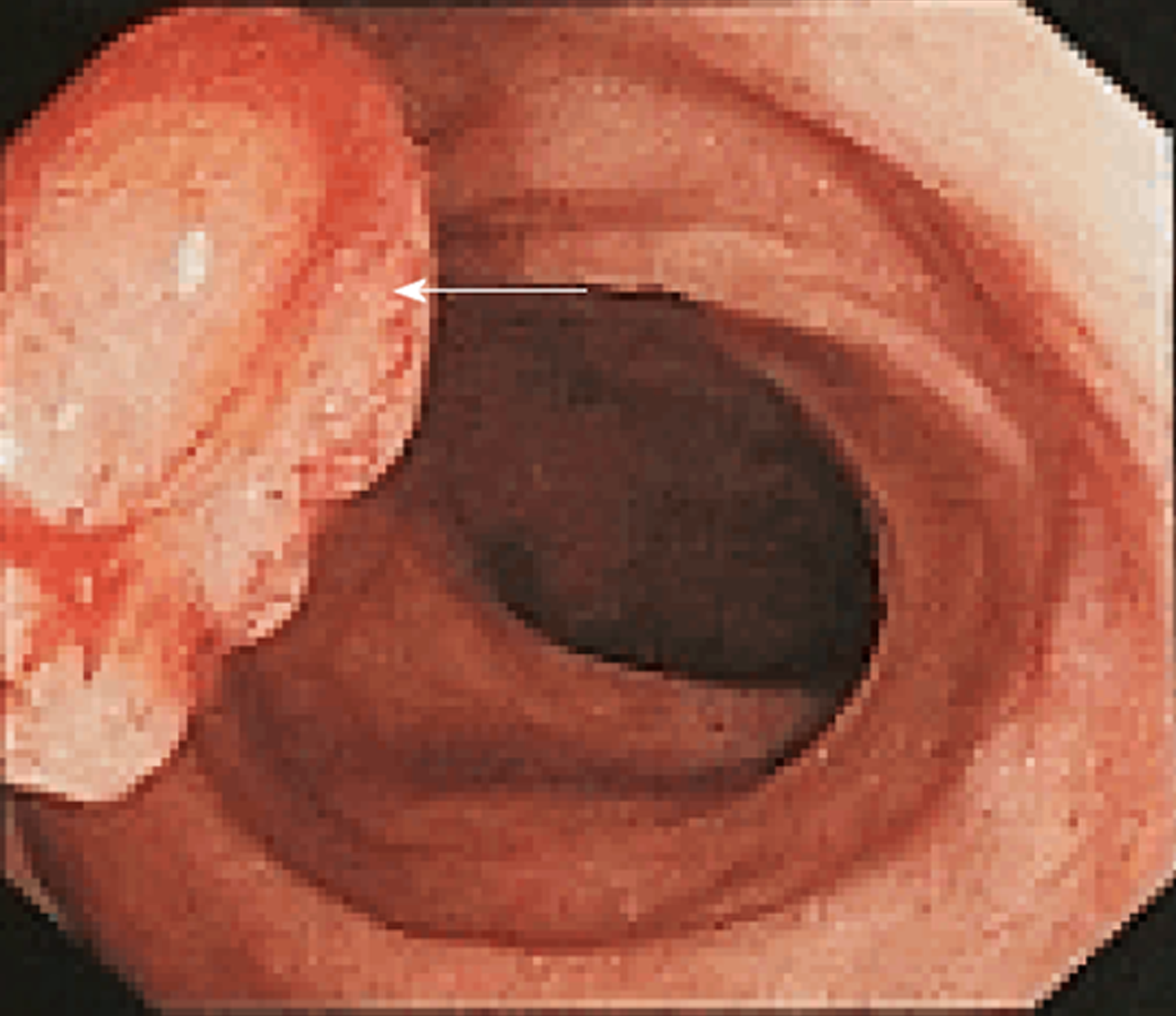
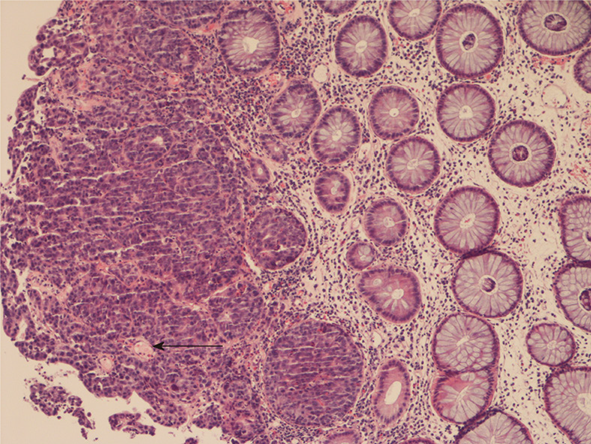
Ultrasonography of the cervical mass showed that multiple hypoechoic masses were present in the left supraclavicular fossa, and the larger mass measuring 0.9 cm × 0.5 cm had a clear border and unclear internal structure. This mass was mildly enhanced on contrast-enhanced computed tomography (CT) (Figure 1). Positron emission tomography/CT (PET/CT) scan demonstrated that no significant fluorodeoxyglucose (FDG) uptake was observed in the left supraclavicular region (Figure 2). To determine the nature of the enlarged lymph nodes, lymph node biopsy was performed, and histopathological examination revealed metastatic adenocarcinoma (Figure 3). In the immunohistochemical analysis, the biopsied tissue was positive for SP-B, CK8/18, CK20, CDX-2 and P504S expression with a Ki-67 index of 80%; the tissue was negative for CK5/6, CgA, P40, P63, CK7, TTF-1, Napsin A, SPA and Syn expression. The laboratory assessment revealed that CEA, CA199, and CA724 serum levels were elevated. To further clarify the diagnosis, the patient underwent gastroenteroscopy, and the results revealed one pedunculated polyp with mucosal erosion in the sigmoid colon, measuring 2.0 cm in diameter (Figure 4). Histological examination with hematoxylin-eosin staining revealed adenocarcinoma was in the intramucosal tissue (Figure 5). Immunohistochemical analysis revealed that the polyp was positive for CDX-2 and CK20 expression, negative for CgA, Syn and CD56 expression, and the Ki-67 index was 70%. In addition, high-throughput gene sequencing showed wild type K-Ras.
According to the results of the auxiliary examination, this patient was diagnosed with late-stage sigmoid colon cancer with distant lymph node metastasis.
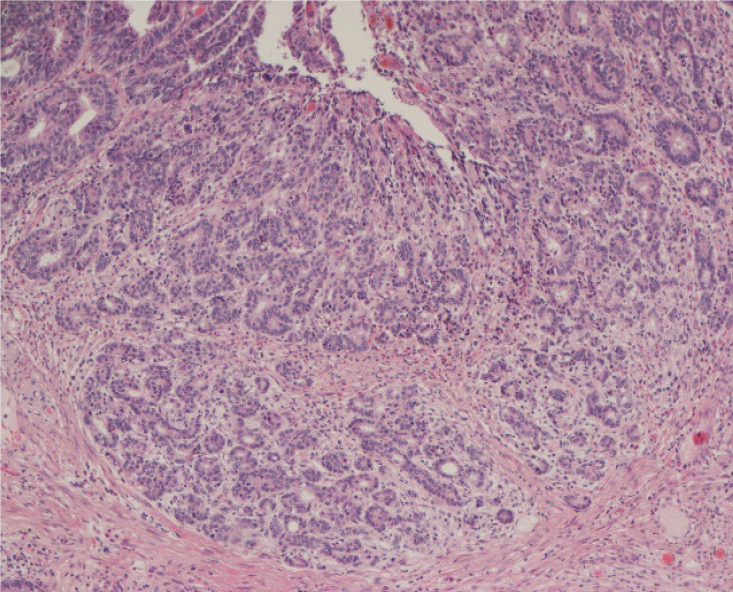
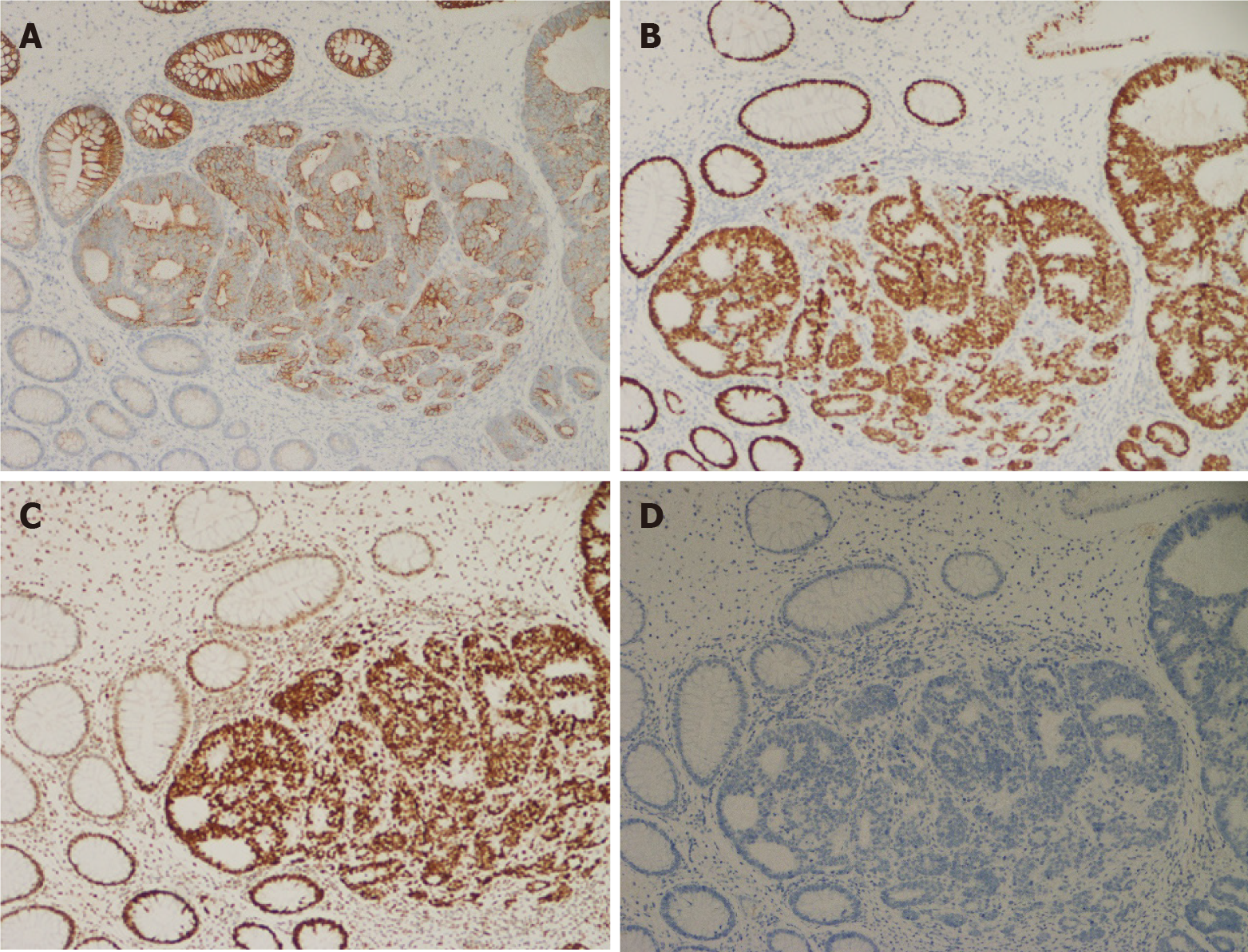
The patient received chemotherapy with the 5-fluorouracil, leucovorin and oxaliplatin (FOLFOX) + cetuximab regimen. After 6 cycles of chemotherapy, the patient was reexamined with CT and ultrasonography, and the results showed that the sigmoid colon tumor and Virchow’s lymph node were significantly smaller than before treatment and no new metastatic sites were found. Considering the effects of chemotherapy on quality of life, the patient and his family members strongly requested surgery after receiving education on the risks and benefits of surgery and other therapeutic regimens. Therefore, sigmoid carcinoma resection and mesenteric lymph node dissection were performed. Histological examination (Figure 6) showed moderately differentiated adenocarcinoma localized in the mucosa, and one of five paracolic lymph nodes contained metastatic carcinoma (pT1N1M1). Immunohistochemically, the excised tissues were positive for CK20, MSH2 and SATB2 and negative for CK7 (Figure 7). After surgery, the patient received the same chemotherapy regimen as before. After undergoing 4 cycles of chemotherapy, Virchow’s lymph node dissection was selected by mutual consultation between the patient and us. We removed the lymph nodes in the triangle bounded by the lower abdomen of the omohyoid, the posterior margin of the sternocleidomastoid and the superior clavicle (the level IV and VB lymph nodes of the neck). Histological examination revealed that five of the eight dissected cervical lymph nodes contained metastatic carcinoma. Immunohistochemically, these lymph nodes were positive for CDX2, SATB2, CK20, KIAA1429 and RBM15 and negative for IC3H13, CK7, TTF1 and P40. Histopathologic examination and immunohistochemistry staining again confirmed sigmoid metastasis. During the dissection of the enlarged left supraclavicular lymph node, there was clear fluid outflow from the left venous angle, which suggested lymphatic leakage. We immediately sutured the site with silk thread and pressed it with a gelatin sponge; subsequently, the fluid outflow stopped. On the second day after surgery, the left cervical drainage tube drained approximately 2000 mL milky white fluid. After the diagnosis of postoperative lymphatic leakage, the patient was treated with diet restriction, total parenteral nutrition, local wound compression, and somatostatin pumping. From the 4th to 7th day after surgery, approximately 500-100 mL of clear liquid was drained from the left cervical drainage tube per day. On the 10th day after surgery, 2 mL Pseudomonas aeruginosa (1.8 × 109/mL, Beijing Wanteer Biopharmaceutical Co. Ltd) was injected near the left venous corner under the guidance of ultrasonography, and the drainage tube was clamped. Thirty minutes after the injection, the patient developed chills and high fever, with the highest body temperature recorded at 39 ℃. After a large amount of fluid infusion, anti-inflammatory and other symptomatic treatments, the patient's symptoms gradually improved, and no further lymphatic fluid drainage was observed. Considering the patient has reached the predetermined number of cycles of chemotherapy after sigmoid tumor resection, the patient received a maintenance chemotherapy regimen with capecitabine and cetuximab after the second surgery.
At half of a year after the surgery, the patient was asymptomatic, and there were no signs of tumor recurrence or progression.
CRC can spread by lymphatic, hematogenous, and transperitoneal dissemination as well as direct extension. Regional lymph nodes (52%), liver (78%), lung (20%), and peritoneum (29%) are frequently observed metastatic sites of CRC[2]. CRC with distant lymph node metastasis is very rare. Although a few cases[3-6] of synchronous supraclavicular lymph node metastases from colorectal carcinoma have been reported (Table 1), most were complicated with multiple metastases or treated exclusively with chemotherapy. To the best of our knowledge, this is the first case of lymph node dissection combined with chemotherapy to treat isolated synchronous Virchow’s lymph node metastasis from sigmoid cancer (Table 2).
| No. | Ref. | Year | Age/gender | Primary location | Metastasis of another organ | Resection of Virchow LN | Postoperative chemotherapy | Disease free survival time | Overall survival time |
| 1 | Watanabe et al[3] | 2009 | 73/Male | Cecum | Paraaortic lymph nodes; Lung | - | 5-fluorouracil, Leucovorin, FOLFOX, FOLFIRI | - | 3 yr |
| 2 | Hirose et al[4] | 2010 | 57/Male | Rectum | - | - | FOLFOX, FOLFIRI | - | 3 yr |
| 3 | Ando et al[5] | 2013 | 63/Male | Sigmoid colon | - | - | FOLFOX, FOLFIRI | - | 5 yr |
| 4 | Suliman et al[6] | 2019 | 54/Male | Transverse colon | - | + | FOLFOX, FOLFIRI | - | - |
| 5 | Our case | 2020 | 56/Male | Sigmoid colon | - | + | FOLFOX, capecitabine, cetuximab | So far | So far |
| Time lane | Events |
| June 3, 2020 | The male presented with a left cervical mass for one month |
| June 9, 2020 | Lymph node biopsy was performed and histopathological examination revealed that the metastatic adenocarcinoma was found in the tissue |
| June 18, 2020 | The patient underwent gastroenteroscopy and the results revealed that one pedunculated polyp with mucosal erosion was observed in sigmoid colon, and histological examination revealed that adenocarcinoma was found in the intramucosal tissue |
| June 30, 2020 to September 30, 2020 | Undergoing 6 cycles of chemotherapy with FOLFOX + cetuximab regimen |
| October 22, 2020 | The resection of sigmoid carcinoma and mesenteric lymph node dissection were performed. Histological examination showed moderately differentiated adenocarcinoma localized in the mucosa, and one of five paracolic lymph nodes contained metastatic carcinoma (ypT1N1M1) |
| November 30, 2020 to January 30, 2021 | Undergoing 4 cycles of chemotherapy with FOLFOX + capecitabine regimen |
| February 24, 2021 | Virchow lymph node dissection was selected by mutual consultation between the patient and us |
| February 25, 2021 to March 5, 2021 | Postoperative lymphatic leakage |
| March 24, 2021-So far | The patient received chemotherapy with capecitabine and cetuximab. At nearly half of a year following the surgery, the patient was asymptomatic, and there were no signs of tumor recurrence or progression |
An enlarged Virchow’s lymph node located near the junction of the thoracic duct and the left subclavian vein is often considered a sign of gastric and esophageal cancer metastasis[7]. The specific mechanism of distant lymph node metastasis from CRC, such as metastasis to the Virchow lymph node, has not been reported. One possible metastatic mechanism is that this patient developed intraperitoneal micrometastases prior to systemic chemotherapy. Lymph from intraperitoneal metastatic lymph nodes enters the thoracic duct through lymphatic drainage, resulting in left supraclavicular lymph node enlargement[8].
The surgical indications for colorectal tumors with distant lymph node metastases remain controversial[9]. Traditionally, supraclavicular lymph node metastasis is considered a relative contraindication to surgery. CRC with supraclavicular lymph node metastasis is typically diagnosed as stage IV and indicates poor prognosis[10-12]. However, some CRC patients with supraclavicular lymph node metastasis achieve a good response and better prognosis after chemotherapy[3-6]. Therefore, preoperative chemotherapy combined with surgical resection has been reconsidered for this indication given the development of increasingly effective chemotherapy regimens[13]. In our case, because genetic sequencing of the patient's sigmoid tumor revealed at wild type K-Ras gene, the patient was administered six cycles of chemotherapy with the FOLFOX + cetuximab regimen. Due to the timely intervention with an appropriate systemic chemotherapy regimen, the patient did not develop systemic organ metastasis, and the primary tumor and metastatic lymph nodes showed a good response. This notion was further confirmed by postoperative pathology showing a retraction of sigmoid tumor invasion and fewer paracolic lymph node metastases. After resection of the primary site and 4 cycles of postoperative chemotherapy with the original regimen, this patient underwent left supraclavicular region lymph node dissection followed by chemotherapy with capecitabine + cetuximab. During the follow-up period, no signs of tumor recurrence or progression were observed. Therefore, we suggest that preoperative chemotherapy combined with surgical resection may be used to extend the survival interval of patients with CRC, especially patients who respond well to chemotherapy and have a strong desire to undergo surgery.
Previous literature has reported that PET/CT offers value in predicting distant tumor metastases[14]. In our case, however, no significant FDG uptake was observed in the patients' left supraclavicular lymph nodes on PET/CT. The false negative PET/CT results of this patient may be related to the smaller diameter of the supraclavicular lymph nodes. The standard uptake value (SUV) of the lesion is generally proportional to its size, so the SUV of smaller metastatic lymph nodes is often low and more difficult to detect by PET/CT[15]. In other words, PET/CT has lower sensitivity and higher specificity for distant metastatic lymph nodes than contrast-enhanced CT.
Pseudomonas aeruginosa injection is performed using attenuated Pseudomonas aeruginosa. Previous studies have confirmed that injection of Pseudomonas aeruginosa has a significant effect on improving postoperative lymphatic leakage of thyroid cancer[16]. The possible mechanism is as follows: Pseudomonas aeruginosa can penetrate into the subcutaneous space and produce aseptic inflammation, which promotes the closure of lymphatic vessels and reduces lymphatic leakage. In our case, the patient developed a lymphatic fistula after supraclavicular lymph node dissection. After the failure of a series of conservative treatments, we attempted to inject Pseudomonas aeruginosa from the left venous angle to reduce lymphatic leakage and achieved good results.
In summary, isolated Virchow’s lymph node metastasis is a potential metastatic route of CRC. In addition, when supraclavicular lymph node metastases are controlled by chemotherapeutic drugs, radical resection of both the primary site and the metastatic lesion is feasible. However, there is a need for further research to determine the optimum duration of preoperative chemotherapy and to further perfect surgical interventions.
We wish to thank the patient and Jining First People's Hospital for giving the consent and providing the data to report this case.
| 1. | Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359-E386. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20108] [Cited by in RCA: 20722] [Article Influence: 1883.8] [Reference Citation Analysis (23)] |
| 2. | Byun JH, Ahn JB, Kim SY, Kang JH, Zang DY, Kang SY, Kang MJ, Shim BY, Baek SK, Kim BS, Lee KH, Lee SI, Cho SH, Sohn BS, Kim S, Hwang IG, Nam EM, Seo BG, Oh SC, Lee MA, Lee SC, Hong JH, Park YS. The impact of primary tumor location in patients with metastatic colorectal cancer: a Korean Cancer Study Group CO12-04 study. Korean J Intern Med. 2019;34:165-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 23] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 3. | Takahashi S, Iiai T, Shimada Y, Kobayashi Y, Suda K, Iwaya A, Maruyama S, Tani T, Hatakeyama K. [A long-term survival case of far-advanced colon cancer with Virchow's lymph node and lung metastasis that responded to multidisciplinary therapy]. Gan To Kagaku Ryoho. 2009;36:127-129. [PubMed] |
| 4. | Hirose H, Ikeda M, Miyoshi N, Kim HM, Okano M, Uemura M, Yamashita S, Takemasa I, Mizushima T, Yamamoto H, Ishii H, Sekimoto M, Doki Y, Mori M. [A long-term survival case of rectal cancer with Virchow's lymph node metastasis by multimodality therapy]. Gan To Kagaku Ryoho. 2010;37:2545-2547. [PubMed] |
| 5. | Ando M, Fujiya K, Kamikozuru H, Ganno H, Amagasa H, Takeuchi S, Kawai Y, Fukuda A, Nagahama T, Ami K, Aoki N, Arai K, Tei S, Okada Y, Miura K. [Long-term survival of a case with advanced sigmoid colon cancer and Virchow's lymph node metastasis]. Gan To Kagaku Ryoho. 2013;40:2083-2085. [PubMed] |
| 6. | Suliman MS, Singh M, Ajmeri AN, Stuart DL, Teka ST. Virchow's node: a case report of an extremely rare presentation of metastasis of adenocarcinoma with mucinous features from the colon. Int J Gen Med. 2019;12:137-140. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 7. | Achmad H, Hanifa R. Supraclavicular Lymphnodes: Unusual Manifestation of Metastase Adenocarcinoma Colon. Acta Med Indones. 2015;47:333-339. [PubMed] |
| 8. | Das S, Ladell DS, Podgrabinska S, Ponomarev V, Nagi C, Fallon JT, Skobe M. Vascular endothelial growth factor-C induces lymphangitic carcinomatosis, an extremely aggressive form of lung metastases. Cancer Res. 2010;70:1814-1824. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Min BS, Kim JS, Kim NK, Lim JS, Lee KY, Cho CH, Sohn SK. Extended lymph node dissection for rectal cancer with radiologically diagnosed extramesenteric lymph node metastasis. Ann Surg Oncol. 2009;16:3271-3278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 52] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Aghili M, Izadi S, Madani H, Mortazavi H. Clinical and pathological evaluation of patients with early and late recurrence of colorectal cancer. Asia Pac J Clin Oncol. 2010;6:35-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 11. | Weitz J, Koch M, Debus J, Höhler T, Galle PR, Büchler MW. Colorectal cancer. Lancet. 2005;365:153-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 862] [Cited by in RCA: 956] [Article Influence: 45.5] [Reference Citation Analysis (0)] |
| 12. | Siegel R, DeSantis C, Virgo K, Stein K, Mariotto A, Smith T, Cooper D, Gansler T, Lerro C, Fedewa S, Lin C, Leach C, Cannady RS, Cho H, Scoppa S, Hachey M, Kirch R, Jemal A, Ward E. Cancer treatment and survivorship statistics, 2012. CA Cancer J Clin. 2012;62:220-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1973] [Cited by in RCA: 2085] [Article Influence: 148.9] [Reference Citation Analysis (3)] |
| 13. | Watanabe M, Otake R, Kozuki R, Toihata T, Takahashi K, Okamura A, Imamura Y. Recent progress in multidisciplinary treatment for patients with esophageal cancer. Surg Today. 2020;50:12-20. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 191] [Cited by in RCA: 323] [Article Influence: 53.8] [Reference Citation Analysis (0)] |
| 14. | Blodgett TM, Meltzer CC, Townsend DW. PET/CT: form and function. Radiology. 2007;242:360-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 285] [Cited by in RCA: 246] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 15. | Kwak JY, Kim JS, Kim HJ, Ha HK, Yu CS, Kim JC. Diagnostic value of FDG-PET/CT for lymph node metastasis of colorectal cancer. World J Surg. 2012;36:1898-1905. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 49] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 16. | Chen Q, Chen Y, Su A, Ma Y, Yu B, Zou X, Peng D, Zhu J. Ultrasound-guided percutaneous injection of Pseudomonas aeruginosa-mannose sensitive hemagglutinin for treatment of chyle fistula following neck dissection: Two case reports. Medicine (Baltimore). 2020;99:e18816. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Elkady N, Sacdalan DL, Sato Y S-Editor: Yan JP L-Editor: A P-Editor: Yan JP