Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9911
Peer-review started: June 11, 2021
First decision: June 25, 2021
Revised: July 2, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: November 16, 2021
Processing time: 153 Days and 19.5 Hours
In this case report we describe an extremely rare case of cerebral air embolism following transbronchial lung biopsy (TBLB). Only a few cases of this rare complication were described previously. Every bronchologist should recognize this severe adverse event. Prompt recognition of this complication is mandatory in order to initiate supportive measures and consider hyperbaric oxygen therapy.
In this case report we describe an extremely rare case of cerebral air embolism following TBLB. Only a few cases of this rare complication were described previously. Our patient had an incidental finding of lung tumour and pulmonary emphysema. Cerebral air embolism developed during bronchoscopy procedure, immediately after the third trans-bronchial lung biopsy sample and caused cerebral ischaemia of the right hemisphere and severe left-sided hemiplegia. Despite timely initiation of hyperbaric oxygen therapy hemiplegia didn´t resolve and the patient died several weeks later. Cerebral air embolism is an extremely rare complication of TBLB. This condition should be considered in case the patient remains unresponsive or presents with acute neurological symptoms in the post-intervention period since early recognition, diagnosis and hyperbaric oxygen therapy initiation are key factors determining the patient´s outcome.
Within this report, we conclude that air/gas embolism is an extremely rare complication after TBLB, which should be considered in case the patient remains unresponsive or presents with acute neurological symptoms in the post-intervention period after bronchoscopy. The current gold standard for diagnosis is computed tomography scan of the head. After recognition of this complication we suggest immediate hyperbaric oxygen therapy, if available.
Core Tip: Cerebral air embolism is an extremely rare complication of transbronchial lung biopsy. This condition should be considered in case the patient remains unresponsive or presents with acute neurological symptoms in the post-intervention period since early recognition, diagnosis and hyperbaric oxygen therapy initiation are key factors determining the patient´s outcome.
- Citation: Herout V, Brat K, Richter S, Cundrle Jr I. Cerebral air embolism complicating transbronchial lung biopsy: A case report. World J Clin Cases 2021; 9(32): 9911-9916
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9911.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9911
Transbronchial lung biopsy (TBLB) is a bronchoscopy procedure performed with the use of biopsy forceps. The most frequent indications for TBLB are peripheral nodular lesions of the lungs, suspect sarcoidosis or interstitial lung disease[1]. Despite the diagnostic yield is rather lower and differs by various lung pathologies, the diagnostic performance when seeking lung nodules can be improved with the use of fluoroscopy or radial ultrasound[1].
The most common complications of TBLB include pneumothorax and bleeding, occurring with a frequency of a few per cents across different cohorts[2,3]. Air embolism was described in literature as an extremely rare complication of TBLB[4-6] or transbronchial needle aspiration[7] as well as computed tomography-guided transthoracic biopsy[8-11]. Hereby we describe a near-fatal case of cerebral air embolism after TBLB in a patient who had lung cancer.
A 70-year-old man collapsed during flexible bronchoscopy after third TBLB.
A flexible bronchoscopy procedure was performed using standard light sedation with alprazolam and topical anaesthesia with lidocaine and trimecaine. The macroscopic appearance of the lower airways was about normal. The TBLB procedure was initiated. Following the successful completion of two TBLB samples, the third TBLB was complicated by haemorrhage. The medium-intensity bleeding was stopped with topical use of etamsylate and terlipressin.
Shortly after the third TBLB sample the patient collapsed. His pulse rate dropped to 30-50 b.p.m. and his systolic blood pressure fell under 90 mmHg. After i.v. administration of 1 mg of atropin, bradycardia and hypotension retreated. The patient was unresponsive, had right-sided mydriasis, with hemi-facial cyanosis on the right side.
Irrelevant.
Shortly after the third TBLB sample the patient collapsed. His pulse rate dropped to 30-50 b.p.m. and his systolic blood pressure fell under 90 mmHg. After i.v. administration of 1 mg of atropin, bradycardia and hypotension retreated. The patient was unresponsive, had right-sided mydriasis, with hemi-facial cyanosis on the right side.
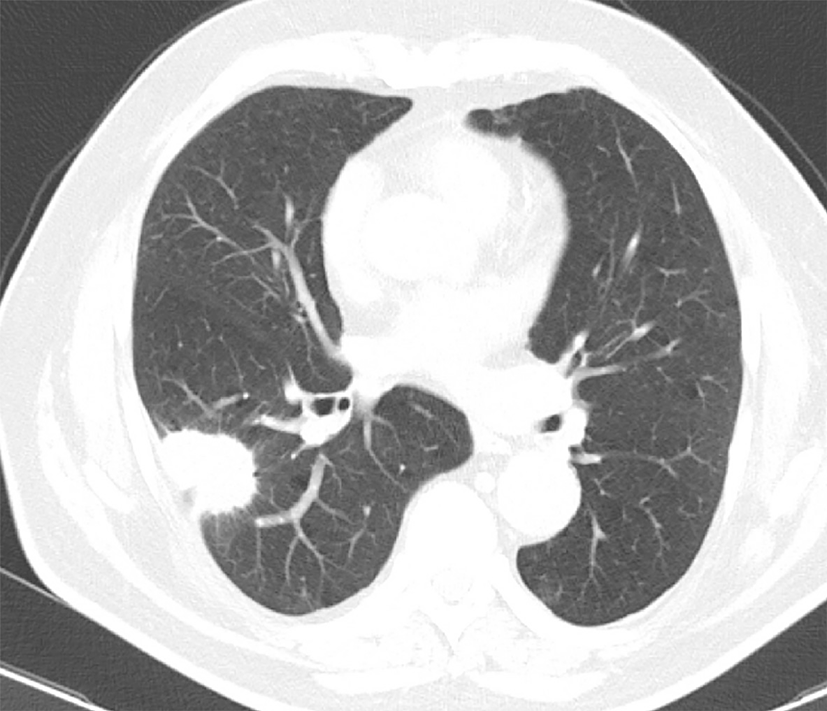
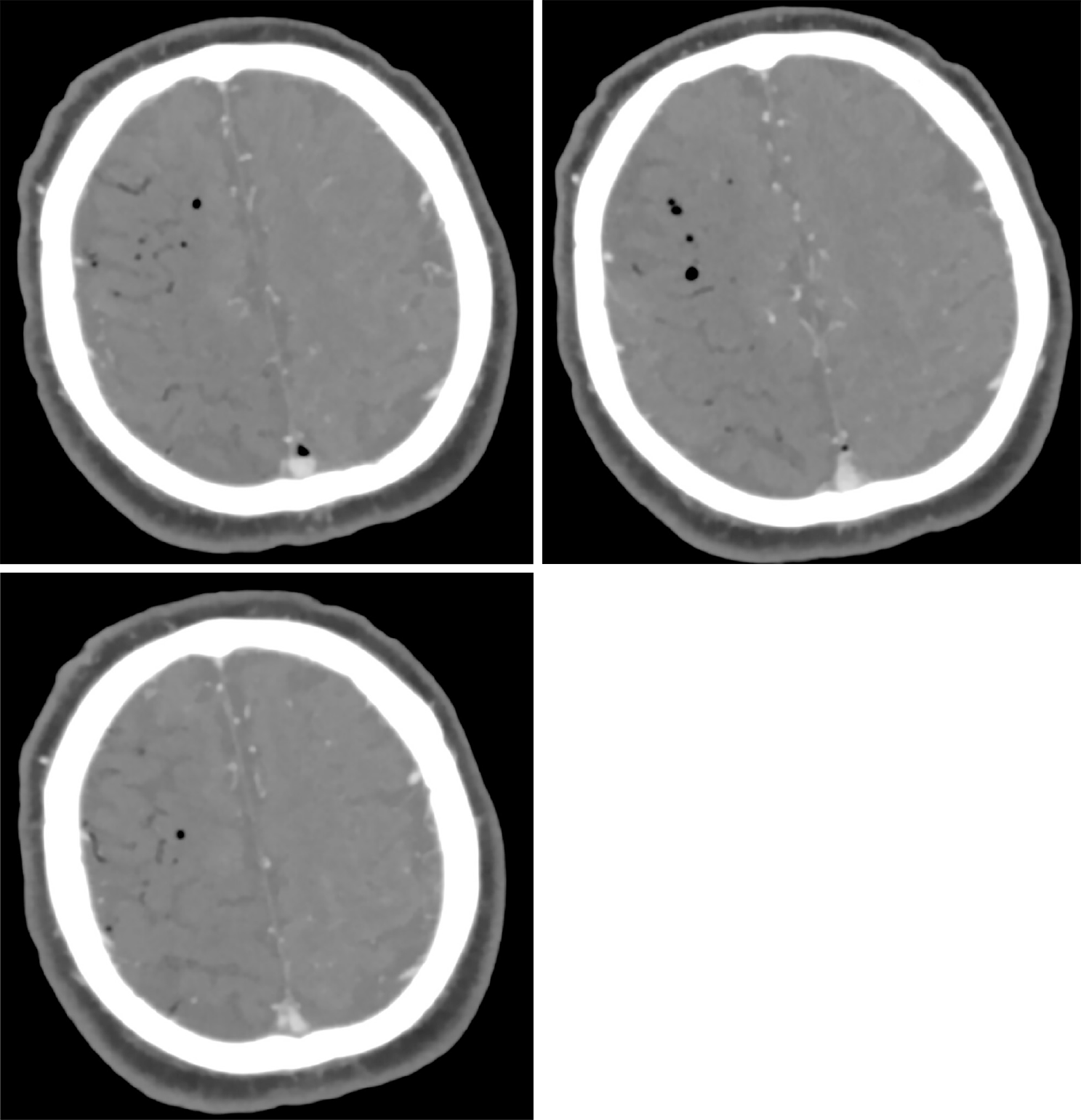
He was immediately transported to emergency unit. On neurological examination left side hemiplegia with right rotation of the head were found. Chest computed tomography (CT) showed spiculating lung tumour in S6 of the right lung (Figure 1). A CT scan of the brain performed 30 min after the event revealed air in the venous system of right cerebral hemisphere, suggesting air embolism (Figure 2).
The final diagnosis of the presented case is cerebral air embolism in the venous system of the right cerebral hemisphere.
The patient was immediately transferred by helicopter air ambulance to Na Homolce Hospital (Prague, distance ca 200 km) where hyperbaric oxygen therapy was initiated.
A follow-up CT scan performed 3 d later showed right cerebral hemisphere watershed ischaemia with foci of acute infarction. It was consistent with the persistent severe left-sided hemiparesis. Intensive stroke rehabilitation was performed for 14 d, but there was no tendency towards recovery. The patient´s poor prognosis was discussed with the family and it was decided to transfer the patient to a hospice where he died several days later.
Around 270 to 300 patients annually undergo TBLB at our university-type respiratory department, but this was the first ever documented case of cerebral air embolism. Unfortunately, the case was fatal and the patient died within a few weeks after the event.
Transbronchial lung biopsy rarely causes life-threatening complications. An extremely rare complication after bronchoscopy can be cerebral air embolism. A small number of air emboli cases were mentioned in the literature. Those are arterial as well as venous air emboli[4,6]. The exact mechanism of air embolism during TBLB is not clear. It seems probable that a combination of venous trauma together with increased airway pressure and predisposing patient-related factors (e.g. lung fibrosis, lung tumours) may play a role[12].
In the first published case report, Erickson et al[13] speculated that exhalation against wedged bronchoscope might have caused increase in airway pressure distal from the bronchoscope and thereby contributed to the air embolism development. Wedged bronchoscope as a possible cause of increased airway pressure was described also in the case report of Dhillon et al[4]. Air trapping in patients with severe chronic obstructive pulmonary disease and coughing may be another factor that could increase airway pressure and contribute to air embolism development during transbronchial biopsy[4,12,14] and also during bronchial curette cytology, which is considered a less invasive procedure than bronchial biopsy or needle aspiration[14]. Finally, positive-pressure ventilation was used in some of the reported patients[5,6,15]; however this might have aggravated the air embolism but not caused it primarily, as all of the patients had symptoms prior to being intubated.
Although a few cases of air embolism without venous trauma were documented[16,17], it is unlikely that the increased airway pressure alone would be sufficient to cause air embolism during transbronchial biopsy as the pressures used in both above cited studies were unphysiologically high (bronchoscopic expanding of atelectatic lobe [16] and in canine experiment[17]). Indeed, postmortem finding of a patent broncho-venous fistula, as an origin of cerebral air embolism, was described by Strange et al[5]. Therefore, it appears that both broncho-venous communication and increased airway pressure predispose to cause air embolism.
Moreover, in the Strange et al[5] case report, the patient was diagnosed with amyloidosis and the authors speculated the amyloid infiltration of pulmonary vessels might have prevented vasoconstriction and the immediate closure of the broncho-venous fistula. Similarly, lung fibrosis might have caused the same effect in the report of Shetty et al[6] and tuberculosis in the report of Erikson et al[13]. Also tumor associated lung consolidations (which may cause loss of lung elasticity, and may thereby allow abnormal communications to stay open for a longer time) was speculated as a risk factor for air embolism during bronchoscopic tumour ablation[18]. However, in this case Nd:YAG laser was used and the reason for air embolism was probably the coolant air stream entering the tumor and pulmonary venous circulation[18].
Taken together, it appears that the combination of broncho-venous communication, patient factors not allowing immediate closure of the artificial communication and high airway pressure increasing the amount of air entering the blood stream are needed to cause clinically significant air embolism. Probably a combination of all these factors was the cause of air embolism also in our patient.
Depending on the air volume, signs of low cardiac output (hypotension, tachy
In our case, the hyperbaric oxygen treatment was largely unsuccessful, probably due to the relative remoteness of the nearest hyperbaric chamber (ca 200 km distance from University Hospital Brno). We also speculate that the air emboli were partly treatment-resistant to hyperbaric oxygen therapy due to normal (21%) oxygen content. Higher oxygen content in the emboli (e.g. with oxygen inhalation during bronchoscopy) could probably resolve better and the residual neurological disorder would be more limited.
Within this report, we conclude that air/gas embolism is an extremely rare complication after TBLB, which should be considered in case the patient remains unresponsive or presents with acute neurological symptoms in the post-intervention period after bronchoscopy. The current gold standard for diagnosis is CT scan of the head. After recognition of this complication we suggest immediate hyperbaric oxygen therapy, if available.
| 1. | Herout V, Heroutova M, Merta Z, Cundrle I Jr, Brat K. Transbronchial biopsy from the upper pulmonary lobes is associated with increased risk of pneumothorax - a retrospective study. BMC Pulm Med. 2019;19:56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 2. | Milman N, Faurschou P, Munch EP, Grode G. Transbronchial lung biopsy through the fibre optic bronchoscope. Results and complications in 452 examinations. Respir Med. 1994;88:749-753. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 48] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Du Rand IA, Blaikley J, Booton R, Chaudhuri N, Gupta V, Khalid S, Mandal S, Martin J, Mills J, Navani N, Rahman NM, Wrightson JM, Munavvar M; British Thoracic Society Bronchoscopy Guideline Group. British Thoracic Society guideline for diagnostic flexible bronchoscopy in adults: accredited by NICE. Thorax. 2013;68 Suppl 1:i1-i44. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 410] [Cited by in RCA: 598] [Article Influence: 46.0] [Reference Citation Analysis (0)] |
| 4. | Dhillon SS, Agrawal A, Gorin AB. Cerebral Arterial Air Embolism After Transbronchial Lung Biopsy: A Case Report and Review of Literature. J Bronchology Interv Pulmonol. 2004;11:125-127. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Strange C, Heffner JE, Collins BS, Brown FM, Sahn SA. Pulmonary hemorrhage and air embolism complicating transbronchial biopsy in pulmonary amyloidosis. Chest. 1987;92:367-369. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 37] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | Shetty PG, Fatterpekar GM, Manohar S, Sujit V, Varsha J, Zarir U. Fatal cerebral air embolism as a complication of transbronchoscopic lung biopsy: a case report. Australas Radiol. 2001;45:215-217. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Almas ET, Casserly B. Air embolism following bronchoscopy with fine needle aspiration: An unexpected complication. Respir Med Case Rep. 2018;25:228-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Richardson CM, Pointon KS, Manhire AR, Macfarlane JT. Percutaneous lung biopsies: a survey of UK practice based on 5444 biopsies. Br J Radiol. 2002;75:731-735. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 144] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 9. | Tomiyama N, Yasuhara Y, Nakajima Y, Adachi S, Arai Y, Kusumoto M, Eguchi K, Kuriyama K, Sakai F, Noguchi M, Murata K, Murayama S, Mochizuki T, Mori K, Yamada K. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. 2006;59:60-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 293] [Cited by in RCA: 355] [Article Influence: 17.8] [Reference Citation Analysis (0)] |
| 10. | Ohashi S, Endoh H, Honda T, Komura N, Satoh K. Cerebral air embolism complicating percutaneous thin-needle biopsy of the lung: complete neurological recovery after hyperbaric oxygen therapy. J Anesth. 2001;15:233-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Ghafoori M, Varedi P. Systemic air embolism after percutaneous transthorasic needle biopsy of the lung. Emerg Radiol. 2008;15:353-356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Perinel Ragey S, Garnier P, Vergnon JM. Complete resolution of cerebral air embolism secondary to a transbronchial needle aspiration. Respiration. 2013;86:504-507. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Erickson AD, Irwin RS, Teplitz C, Corrao WM, Tarpey JT. Cerebral air embolism complicating transbronchoscopic lung biopsy. Ann Intern Med. 1979;90:937-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Maemura K, Kage H, Isago H, Takeshima H, Makita K, Amano Y, Takai D, Ohishi N, Nagase T. Cerebral Arterial Air Embolism after Diagnostic Flexible Fiberoptic Bronchoscopy: A Case Report and Review of the Literature. Case Rep Pulmonol. 2018;2018:7108215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Azzola A, von Garnier C, Chhajed PN, Schirp U, Tamm M. Fatal cerebral air embolism following uneventful flexible bronchoscopy. Respiration. 2010;80:569-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Wherrett CG, Mehran RJ, Beaulieu MA. Cerebral arterial gas embolism following diagnostic bronchoscopy: delayed treatment with hyperbaric oxygen. Can J Anaesth. 2002;49:96-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 17. | Meier GH, Wood WJ, Symbas PN. Systemic air embolization from penetrating lung injury. Ann Thorac Surg. 1979;27:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Peachey T, Eason J, Moxham J, Jarvis D, Driver M. Systemic air embolism during laser bronchoscopy. Anaesthesia. 1988;43:872-875. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 19. | Muth CM, Shank ES. Gas embolism. N Engl J Med. 2000;342:476-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 602] [Cited by in RCA: 617] [Article Influence: 23.7] [Reference Citation Analysis (0)] |
| 20. | Hiraki T, Fujiwara H, Sakurai J, Iguchi T, Gobara H, Tajiri N, Mimura H, Kanazawa S. Nonfatal systemic air embolism complicating percutaneous CT-guided transthoracic needle biopsy: four cases from a single institution. Chest. 2007;132:684-690. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Corresponding Author's Membership in Professional Societies: European Respiratory Society, No. 245031; Czech Respiratory Society.
Specialty type: Respiratory System
Country/Territory of origin: Czech Republic
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Wang H S-Editor: Wang JL L-Editor: A P-Editor: Guo X