Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.9752
Peer-review started: May 12, 2021
First decision: June 15, 2021
Revised: June 28, 2021
Accepted: August 24, 2021
Article in press: August 24, 2021
Published online: November 16, 2021
Processing time: 181 Days and 18.3 Hours
In most elderly patients with intertrochanteric fractures, satisfactory fracture reduction can be achieved by closed reduction using a traction table. However, intertrochanteric fractures cannot achieve satisfactory reduction in a few patients, which is called irreducible intertrochanteric fractures. Especially for type 31A3 irreducible intertrochanteric fractures, limited open reduction of the broken end with different intraoperative reduction methods is required to achieve satisfactory reduction and fixation.
To discuss clinical efficacy of intracortical screw insertion plus limited open reduction in type 31A3 irreducible intertrochanteric fractures in the elderly.
A retrospective analysis was performed on 23 elderly patients with type 31A3 irreducible intertrochanteric fractures (12 males and 11 females, aged 65-89-years-old) who received treatment at the orthopedics department. After type 31A3 irreducible intertrochanteric fractures were confirmed by intraoperative C-arm, all of these cases received intracortical screw insertion plus limited open reduction in the broken end with intramedullary screw internal fixation. The basic information of surgery, reduction effects, and functional recovery scores of the hip joint were assessed.
All patients were followed up for 13.8 mo on average. The operation time was 53.8 ± 13.6 min (40-95 min). The intraoperative blood loss was 218.5 ± 28.6 mL (170-320 mL). The average number of intraoperative X-rays was 22.8 ± 4.6 (18-33). The average time to fracture union was 4.8 ± 0.7 mo. The reduction effect was assessed using Kim’s fracture reduction evaluation. Twenty cases achieved grade I fracture reduction and three cases grade II fracture reduction. All of them achieved excellent or good fracture reduction. Upon the last follow-up, the functional recovery scores score was 83.6 ± 9.8, which was not significantly different from the functional recovery scores score (84.8 ± 10.7) before the fracture (t = 0.397, P = 0.694).
With careful preoperative preparation, intracortical screw insertion plus limited open reduction contributed to high-quality fracture reduction and fixation. Good clinical outcomes were achieved without increasing operation time and intraoperative blood loss.
Core Tip: Intertrochanteric fractures are common hip fractures in elderly patients with osteoporosis. Most of them achieve satisfactory fracture reduction with closed reduction using a traction table. However, for type 31A3 fractures, limited open reduction of the broken end with different intraoperative reduction methods is usually required to achieve satisfactory reduction and fixation. Here a retrospective analysis was performed on 23 elderly cases with 31A3 type irreducible intertrochanteric fractures, who were treated by intracortical screw insertion plus limited open reduction at our hospital in the past 2 years. The clinical efficacy of this treatment approach was assessed.
- Citation: Huang XW, Hong GQ, Zuo Q, Chen Q. Intracortical screw insertion plus limited open reduction in treating type 31A3 irreducible intertrochanteric fractures in the elderly. World J Clin Cases 2021; 9(32): 9752-9761
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/9752.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.9752
Intertrochanteric fractures are common hip fractures in the elderly, which usually affect osteoporotic patients of advanced age. Intertrochanteric fractures account for about 1.4%-3.0% of all fractures[1-3]. Given the high mortality associated with conservative treatment, early surgical treatment is generally preferred in recent years. Satisfactory fracture reduction can be achieved in most elderly patients with intertrochanteric fractures by closed reduction using a traction table. However, the reduction may still be unsatisfactory in a few patients receiving closed reduction using a traction table. These patients are known as irreducible intertrochanteric fractures[4-7], accounting for about 3%-17% of all fractures. Irreducible intertrochanteric fractures are divided into several types, including 31A1.3, 31A2 and 31A3 fractures. Generally speaking, reduction and fixation can be done using bucking bars and poking under closed traction in the first two types of fractures. But for type 31A3 fractures, limited open reduction of the broken end with different intraoperative reduction methods is usually required to achieve satisfactory reduction and fixation. Here a retrospective analysis was performed on 23 elderly cases with 31A3 type irreducible inter
Inclusion criteria: (1) Fresh type 31A3 irreducible intertrochanteric fractures; (2) Age above 65-years-old; (3) Unilateral fractures; (4) Ineffective treatment by closed manipulation using a traction table and confirmed as irreducible intraoperatively; and (5) Willingness of the patients and relatives to cooperate with the treatment and follow-up. Exclusion criteria: (1) Combined with severe internal medicine diseases or mental illnesses or contraindicated for surgery; (2) History of hip surgery; (3) Hip diseases, including local infection, tumors and autoimmune rheumatic diseases; (4) Open fractures; (5) Old fractures; (6) Pathological fractures; and (7) Poor compliance or uncooperative with follow-up.
We retrospectively analyzed 23 elderly patients with type 31A3 irreducible in
Causes of fractures: The fractures were induced by low-energy falls in 22 patients and a car accident in 1 patient. They were admitted through the emergency department and the fast admission channel for elderly hip fractures. The average preoperative wait time was 37.5 ± 6.3 h.
Concurrent internal medicine diseases: Eighteen cases were combined with hyper
Internal fixation: Proximal femoral nail antirotation (PFNA)-II was used for internal fixation in 20 cases and META-TAN in 3 cases.
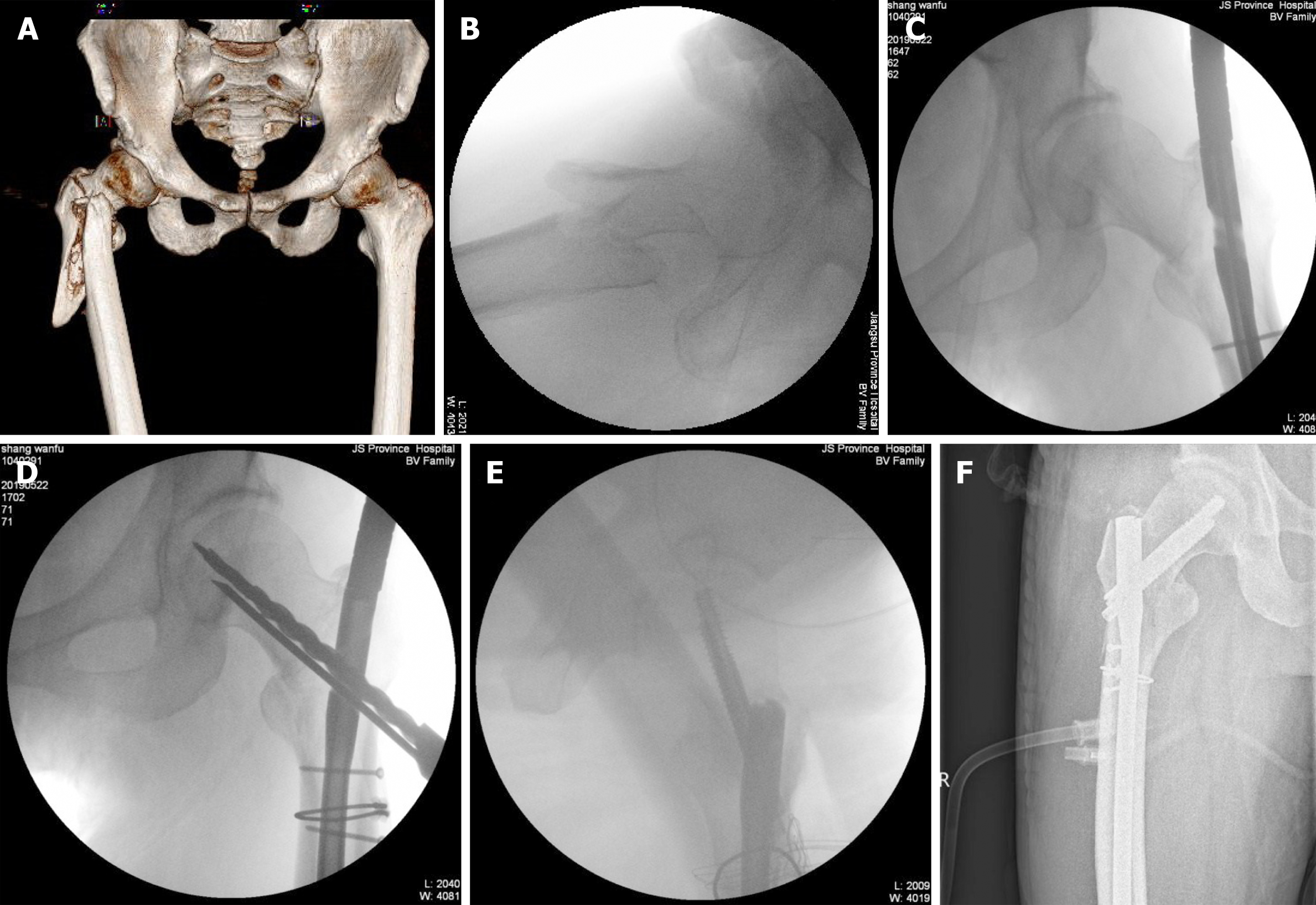
Preoperative preparation: All cases received emergency plain film X-rays of the pelvis and 3D computed tomography scans of the hip joint for radiographic assessment. These cases received supracondylar skeletal traction in the affected limbs immediately after admission. The traction weight was 1/10 of the body weight. Health education was offered to patients and relatives along with comprehensive routine preoperative examinations. The patients also received bedside breathing training and injection of low-molecular-weight heparin. A calf venous pump was used to prevent deep venous thrombosis of lower extremities. Blood glucose and blood pressure levels were controlled according to the examination results. Anesthesiology consultation was held through the fast channel for elderly hip fractures.
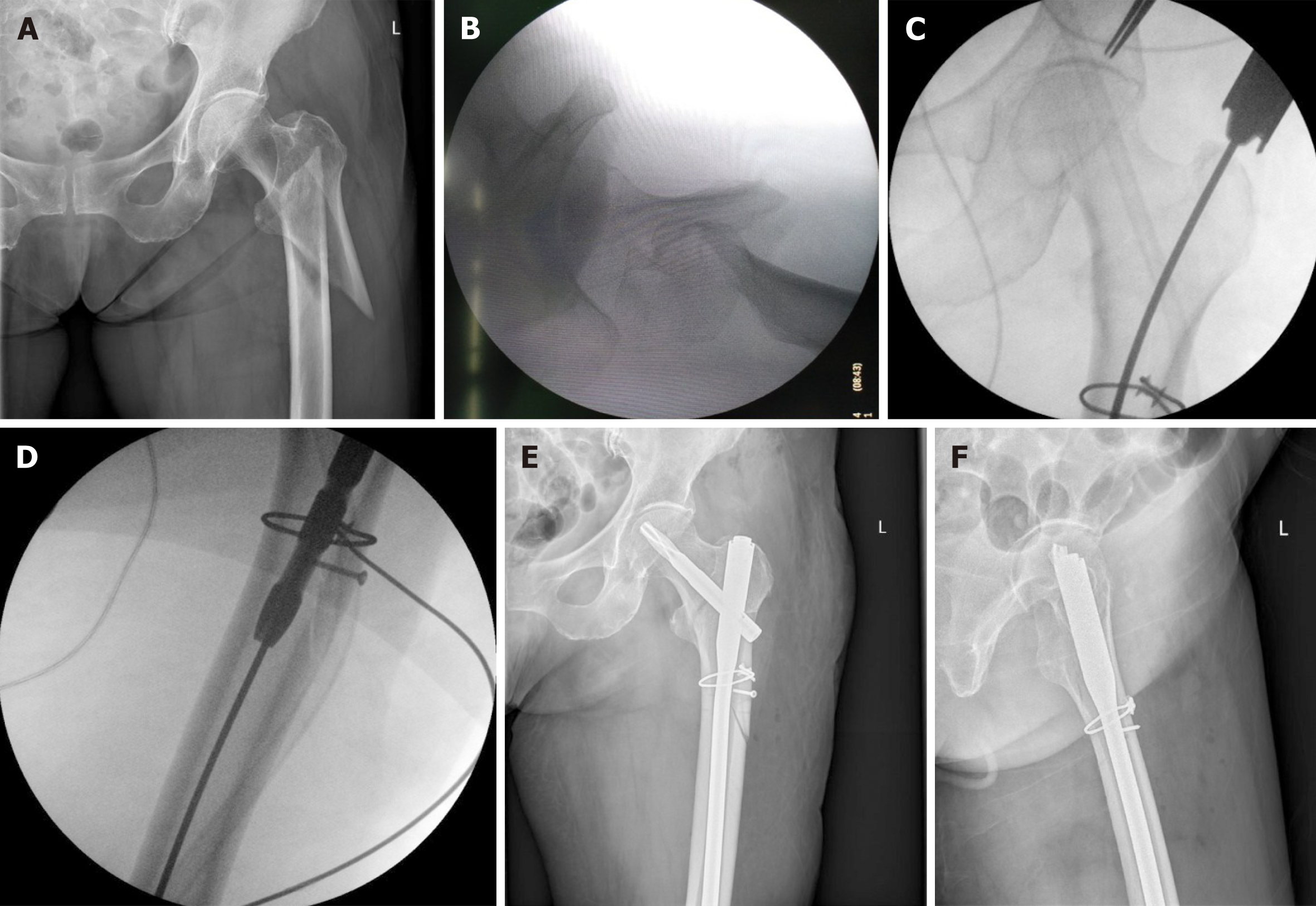
Intraoperative manipulations: All patients underwent tracheal intubation and general anesthesia with peripheral nerve block in the hip joint. After anesthesia, the patients took a supine position on the traction table, with the contralateral limb in flexion and abduction and the upper body slightly inclining towards the healthy side. Closed reduction was first attempted. Longitudinal traction was administered through abduction and external rotation of the affected limb, followed by internal rotation and adduction. However, C-arm X-rays revealed the failure to achieve satisfactory reduction. The proximal end of the fracture was found to be dislocated laterally on the anteroposterior view and towards the anterosuperior direction on the lateral view; the distal end of the fracture was dislocated towards the posteroinferior direction. The traction table was removed after confirming that the intertrochanteric fracture was irreducible.
The patient was then changed to a lateral position, with routine disinfection and draping. After the fracture line was located by intraoperative X-ray, limited resection was performed on the inferolateral aspect of the greater trochanter of the femur, with the incision running for a length of about 4-5 cm. The fascia lata was cut open. The broken end was exposed along the gap between the vastus lateralis muscle and the rectus femoris muscle. If difficulty was encountered during the exposure, blunt dissection of the vastus lateralis muscle was performed. Two or three Hoffman draw hooks were placed near the broken end to reveal the fracture. Longitudinal traction and internal rotation were applied through this incision for approximate reduction. Various reduction instruments were used for precision reduction and temporary fixation of the fractures (e.g., Kirschner wires and pointed reduction forceps).
Under the direct view, a position with intact cortex on the lateral or anterolateral aspect of the femur was chosen. The direction of the screw channel was predicted. It was preferable that the entrance and exit of the screw channel were both inside the cortex. The assistant marked the direction of the screw channel using a 2.0 mm Kirschner wire. Then the surgeon drilled along the predicted direction of the screw channel using a 2.0 mm drill bit. The drill bit was inside the cortex throughout the process. The surgeon could track the advance of the drill bit from the cortex surface. Meanwhile, the assistant performed dripping of normal saline onto the surgical area for cooling and keeping a clear visual field. Caution was taken to prevent the entry of the drill bit into the medullary cavity.
After that, the periphery of the screw channel was inspected with a sensor to ensure that the channel was entirely inside the cortex. The channel length was measured, and the 2.7 mm cortex screws were placed. However, if the insertion angle was too large, the drill bit might partly enter the medullary cavity, and an in-out-in-channel was formed. In that case, it should be checked whether the main part of the channel was still inside the channel and that the insertion of the screws would not influence the subsequent insertion of the intramedullary screws. The channel was retained if it met the above criteria. Each inserted screw had a stabilizing effect on 3-4 cm of the fracture line. Thus, a varying number of intracortical screws were chosen depending on the length of the fracture line, the position of fracture and stability after the reduction.
After the intracortical screws were placed at the optimal positions in some patients, more intracortical screws were inserted without using the channel (for instance, the channel entered spongy bone). Circumferential wiring was performed using one AO titanium cable to achieve synergistic fixation and to increase the stability of the broken end. Next, all Kirschner wires for temporary fixation and other reduction instruments were removed. It was checked whether the broken end was dislocated and tightly fixed. With the manual longitudinal traction preserved, intramedullary screws were inserted into the femur’s proximal end following conventional procedures. A 2-3 cm incision was made with the intersection between the vertical line of the anterior superior iliac spine and the femoral axis as the center. Blunt dissection of the gluteus medius muscle was performed. The apex of the greater trochanter was located and the guide pin was inserted under the X-ray.
In the meantime, the proximal end was opened and reamed to insert PFNA-II to the proper position. A diopter was placed, and the guide pin was inserted into the femoral head and neck under the X-ray until reaching the proper position (1/3 mid-lower portion of the femoral head and neck on the anteroposterior view, and right in the middle of the femoral head and neck on the lateral view). PFNA with a proper length was gently knocked to 5-10 mm below the cartilage. The distal nails were locked. Reduction and fixation were confirmed again under the X-ray. After thorough hemostasis, the incision was closed in layers. No drainage tube was inserted. META-TAN nails were placed using a similar method. More details of the manipulation can be found in the operating manual. The need for intraoperative blood transfusion was assessed based on blood gas analysis. The tracheal tube was removed after surgery. After the respiration and the hemodynamics were stabilized, the patients were transferred to the intensive care unit for postoperative monitoring. They were transferred to the general orthopedic ward when their conditions were stabilized on the second day after surgery.
Postoperative treatment and follow-up: After transferred to the general orthopedic ward on the second day after surgery, the patients received antibiotics to prevent infection and low-molecular-weight heparin against deep venous thrombosis. The patients began to take in-bed exercises under instructions from the rehabilitation department, such as isometric quadriceps exercise and ankle flexion and extension exercise. The patients were discharged or transferred to a rehabilitation hospital if no incision abnormalities were found 3-5 d later. The patients began partial weight-bearing exercise with walking aid and protection from specialized staffs 1-2 wk later. The time to ambulation was prolonged for patients of advanced age and those with comminuted fractures. Full weight-bearing was not allowed until the patients achieved fracture union.
All patients were told to pay regular return visits at 1, 2, 3, 6 and 12 mo after sur
Efficacy evaluation: (1) General indicators: the operation time, intraoperative blood loss, number of intraoperative X-rays, the average length of hospital stay, time to fracture union and complications (incision infection, non-union, failure of internal fixation, hypostatic pneumonia, bedsore and deep venous thrombosis) were recorded in all patients. Reoperation rate and cases lost to follow-up were recorded; (2) Evaluation of reduction outcomes: the reduction of intertrochanteric fractures was assessed using Kim’s fracture evaluation[8]: Grade I: excellent, cortical displacement < 1 cortical thickness in both anteroposterior and lateral views; grade II: fairly good (acceptable), cortical displacement < 1 cortical thickness in either anteroposterior and lateral views; grade III: poor, cortical displacement > 1 cortical thickness in both anteroposterior and lateral views; and (3) Evaluation of clinical efficacy: The function of the hip joint during activities of daily living was evaluated in all patients upon the last outpatient follow-up visit. The evaluation results were standardized based on the functional recovery score (FRS).
All statistical analyses were performed using STATA 15.0 software. Numerical variables were expressed as mean ± SD, and Kolmogorov-Smirnov test was used if they obeyed a normal distribution. FRS scores were compared before the injury and during the follow-up after surgery by paired t-test. The significance level was α = 0.05 (two-sided).
All patients were followed up for 10-23 mo, with an average of 13.8 mo. One case died of acute myocardial infarction at 16 mo of follow-up. The operation time, the intraoperative blood loss and the average number of intraoperative X-rays were 53.8 ± 13.6 min (40-95 min), 218.5 ± 28.6 mL (170-320 mL) and 22.8 ± 4.6 (18-33), respectively. The average length of hospital stay was 7.3 ± 1.5 d, and the average time to union was 4.8 ± 0.7 mo.
None of the patients had coxa vara. Two patients with diabetes had superficial incision infection and received intensive glucose control. Their conditions were improved after incision dressing changes and antibiotic therapy. Hypostatic pneumonia or deep venous thrombosis did not occur postoperatively. Neither nail withdrawal nor breaking of internal fixation occurred.
The reduction effect was assessed using Kim’s fracture reduction evaluation. Twenty cases achieved grade I fracture reduction and three cases grade II fracture reduction. All cases achieved excellent or fairly good fracture reduction. The FRS scores before surgery and at 1, 2, 3 and 6 mo after surgery were all significantly lower than those before the injury. The hip joint function had basically recovered to the pre-injury level at 6 and 12 mo after surgery, without significant differences in FRS scores (Table 1).
| Before injury | At 1 mo after surgery | At 2 mo after surgery | At 3 mo after surgery | At 6 mo after surgery | At 12 mo after surgery | |
| FRS scores | 84.8 ± 10.7 | 51.9 ± 6.2 | 57.1 ± 6.4 | 66.3 ± 7.5 | 81.9 ± 8.1 | 83.6 ± 9.8 |
| t value | 12.759 | 10.655 | 6.790 | 1.036 | 0.397 | |
| P value | < 0.001 | < 0.001 | < 0.001 | 0.306 | 0.694 |
The clinical information of typical cases is shown in Figure 1 and 2.
Intertrochanteric fracture is a common type of hip fracture in the elderly, accounting for about 36%. The majority of intertrochanteric fractures can be treated by closed reduction and internal fixation. PFNA and InterTan nail are the preferred intramedullary fixation systems for most intertrochanteric fractures[2,3,9]. Irreducible intertrochanteric fractures refer to fractures that cannot be effectively reduced by conventional closed traction. Radiographically, the proximal broken end is dislocated in the anterosuperior direction upon traction and the distal broken end in the posteroinferior direction. Besides, these fractures can hardly be corrected by increasing the traction weight. Type 31A1.3, 31A2 and 31A3 are irreducible intertrochanteric fractures[4-7,10,11]. In 2017, Chinese researchers[10] proposed the classification and treatment principles for irreducible intertrochanteric fractures. Type I and II fractures (irreducible either on the sagittal or coronary plane) are usually reducible with closed reduction and fixation using bucking bars and poking manipulation. They are mostly type 31A1.3 and type 31A2 fractures. However, type III fractures (irreducible on both sagittal and coronary planes) are hardly reducible by closed reduction using bucking bars and poking manipulation. There have been no targeted therapies for this type of fracture so far. According to the existing research, the overall failure rate of surgery is higher for these fractures. Therefore, limited open reduction is recommended if closed reduction is ineffective for irreducible intertrochanteric fractures[5,11-16], typically type 31A3 fractures as discussed in the present study.
The reasons for the difficult reduction in type 31A3 fractures can be summarized as follows. First, the fracture line runs in an opposite direction as the intertrochanteric line. The load transfer pattern along the fracture line results in the slip and instability of the distal fracture fragments. Second, the fracture line runs obliquely on the coronary plane from the posteroinferior to the anteromedial. Hence, the soft tissue hinge damage is serious in the front, and the femoral head floats. As a result, no immobilizing effect is exerted on the fracture fragments during closed reduction. Third, the proximal broken end is subjected to the action of short external rotator muscles, gluteus medius muscle and gluteus minimus muscle and therefore is in abduction and dislocation. Furthermore, the proximal broken end is subjected to the joint action of the iliofemoral ligament and iliopsoas muscle and therefore is in an upward dislocation. The joint action of the two muscle groups results in the dislocation of the proximal broken end in a three-dimensional space, that is, forward, upward and outward simultaneously. However, the distal broken end is dislocated downwards due to the gravitational pull. Given the three reasons above, type 31A3 fractures are usually presented as dislocations on two planes, sagittal and coronary, in the elderly. Such fractures are hardly reducible under closed traction, so limited open reduction is needed.
However, during limited open reduction, the assistant may find it hard to maintain the reduction due to the more developed muscles in the proximal femur in type 31A3 fractures. In that case, the reduction should be assisted with Kirschner wires for temporary fixation or other instruments. When several Kirschner wires are used for temporary fixation, the contralateral cortex may displace due to the improper anterior or posterior position of the Kirschner wires, leading to the loss of reduction. If several Kirschner wires are inserted at different angles, they may mistakenly enter the medullary cavity, which affects the subsequent placement of intramedullary screws. Besides, the Kirschner wires generally have low holding power. The broken end is likely to dislocate as the intramedullary screws are inserted subsequently, leading to the loss of reduction. Some researchers tried to use titanium cables alone to assist reduction and fixation. However, there was still an average dislocation of 3 mm in the broken end postoperatively[15]. This is because the proximal femur has a conical structure tapering downwards. The use of titanium cables alone for circumferential wiring can hardly give robust support. Moreover, the broken end may undergo micromovement during the nailing process, leading to downward slippage of the titanium cable and another loss of reduction.
For the reasons above, surgical procedures that can achieve and maintain reduction without causing too much trauma are needed. We innovatively combined intracortical screw technology and limited open reduction for irreducible intertrochanteric fractures in the elderly. Since osteoporosis is prevalent in elderly patients, greater importance should be attached to reduction. Forcible screw insertion with poor reduction will finally lead to a dramatic increase in the risk of internal fixation[4,10,14]. Therefore, the authors abandoned closed reduction and performed limited open reduction instead to expose the broken end directly. The high-quality precision reduction was then achieved using minimally invasive reduction instruments. Intracortical screw technology was employed for fixation and reduction maintenance only after precision reduction and temporary fixation with Kirschner wires. The screw channel was made where the cortex was intact, and it was ensured that the channel was entirely inside the cortex. The reduction was strictly maintained due to the holding power of the screws, and another loss of reduction was avoided by this method. If the fracture line is too long or if there is no suitable site for the insertion of multiple intracortical screws, the minimally invasive titanium cables can be used to assist fixation. In this way, the screws and the cables work synergistically to increase the holding power. With satisfactory reduction achieved, all reduction instruments and the Kirschner wires for temporary fixation are safely withdrawn. By taking these measures, improper anterior or posterior insertion of the Kirschner wires can be prevented, avoiding insufficient temporary fixation and loss of reduction during the subsequent screw placement. This method can also prevent the entry of the Kirschner wires into the medullary cavity, which will affect the subsequent intramedullary nail placement. As demonstrated by our study, limited open reduction allows for effective reduction and fixation and reduction maintenance. This method prevents flask-shaped soft tissue damage that may be otherwise caused by repeated ineffective closed reduction using bucking bars, forceps holder and poking manipulation.
For patients of advanced age, operation time and intraoperative blood loss have a direct bearing on patient survival. As compared with the existing research, our method did not prolong the operation time or increase intraoperative blood loss[17,18]. This is because the quickly performed limited open reduction can reduce time consumption and potential soft tissue damage and bleeding that are usually associated with repeated attempts of closed reduction. Besides, intracortical screws can effectively maintain reduction and reduce bleeding at the broken end.
For patients of advanced age, the reduction effect directly influences survival and prognosis and the complications associated with internal fixation. In the present study, the reduction effect was assessed using Kim’s indicators. The excellent and good rate was 100% among our cases. This result fully demonstrated the safety and reliability of intracortical screw technology combined with limited open reduction. All of the elderly patients achieved satisfactory reduction, with reduction loss less than 1 cortical thickness, which was far superior to the standard of less than 4 mm[8].
This technology has some defects. First of all, limited resection and exposure of the proximal femur raise higher requirements on surgical instruments and assistant’s skills. Secondly, precision reduction and intracortical screw placement entirely within the cortex are to be performed via a small incision. Therefore, the learning curve may be steeper and longer for some surgeons. It is noteworthy that in recent years, with the development of 3D-printing technology, young doctors can shorten the learning curve by simulating surgery on 3D models to become familiar with the surgical skill[19].
Our study had certain limitations, including a small sample size and short duration of follow-up. Our research findings remain to be verified through studies with a longer follow-up and a larger sample size.
For elderly patients with type 31A3 irreducible intertrochanteric fractures, intracortical screw technology plus limited open reduction is a novel surgical treatment modality and meaningful clinical attempt, which could achieve high-quality fracture reduction and fixation. A good clinical efficacy was attained without increasing operation time and intraoperative blood loss. This technology is worthy of further promotion and research.
For elderly patients with type 31A3 irreducible intertrochanteric fractures, intracortical screw technology plus limited open reduction is a novel surgical treatment modality and meaningful clinical attempt, which could achieve high-quality fracture reduction and fixation.
For type 31A3 irreducible intertrochanteric fractures, traditional intraoperative reduction methods are more traumatic, and it is difficult to maintain fracture reduction. Therefore, surgical procedures that can achieve and maintain reduction without causing too much trauma are needed. We innovatively combined intracortical screw technology and limited open reduction for irreducible intertrochanteric fractures in the elderly.
To explore and discuss clinical efficacy of intracortical screw insertion plus limited open reduction in type 31A3 irreducible intertrochanteric fractures in elder patients.
A retrospective analysis was performed on 23 elderly patients with type 31A3 irreducible intertrochanteric fractures who received intracortical screw insertion plus limited open reduction treatment at our orthopedics department. The operation time, intraoperative blood loss, intraoperative X-ray dose, fracture union time, reduction effects and functional recovery scores of the hip joint were evaluated.
The operation time was 53.8 ± 13.6 min. The intraoperative blood loss was 218.5 ± 28.6 mL. The average number of intraoperative X-rays was 22.8 ± 4.6. The average time to fracture union was 4.8 ± 0.7 mo. The reduction effects revealed by Kim’s fracture reduction evaluation was assessed as grade I in 20 cases and grade II in 3 cases, with an excellent to good rate of 100%. The functional recovery scores score in the last follow-up was not significantly different from the functional recovery scores score before the fracture.
Good clinical outcomes and high-quality fracture reduction were achieved by using intracortical screw technology and limited open reduction in patients with type 31A3 irreducible intertrochanteric fractures without increasing operation time and intraoperative blood loss.
Intracortical screw technology requires continual improvement and optimization. More randomized clinical trials are required to verify our findings.
| 1. | Chesser TJS, Handley R. Update of NICE guidance for hip fractures in adults. Hip Int. 2017;27:413-414. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Members of the Writing and Voting Panels of the AUC on the Treatment of Hip Fractures in the Elderly and the AUC on Postoperative Rehabilitation of Low Energy Hip Fractures in the Elderly, Quinn RH, Murray JN, Pezold R. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria for Management of Hip Fractures in the Elderly. J Bone Joint Surg Am. 2016;98:1222-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Ftouh S, Morga A, Swift C; Guideline Development Group. Management of hip fracture in adults: summary of NICE guidance. BMJ. 2011;342:d3304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 4. | Hao Y, Zhang Z, Zhou F, Ji H, Tian Y, Guo Y, Lv Y, Yang Z, Hou G. Risk factors for implant failure in reverse oblique and transverse intertrochanteric fractures treated with proximal femoral nail antirotation (PFNA). J Orthop Surg Res. 2019;14:350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 53] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 5. | Hao YL, Zhang ZS, Zhou F, Ji HQ, Tian Y, Guo Y, Lyu Y, Yang ZW, Hou GJ. Predictors and reduction techniques for irreducible reverse intertrochanteric fractures. Chin Med J (Engl). 2019;132:2534-2542. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Zhao P, Li DL, Yang F, Xu XJ. [Imaging characteristics and the operative effect of the irreducible femoral intertrochanteric fractures]. Zhongguo Gu Shang. 2016;29:693-696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Tan BY, Lau AC, Kwek EB. Morphology and fixation pitfalls of a highly unstable intertrochanteric fracture variant. J Orthop Surg (Hong Kong). 2015;23:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 8. | Kim Y, Dheep K, Lee J, Yoon YC, Shon WY, Oh CW, Oh JK. Hook leverage technique for reduction of intertrochanteric fracture. Injury. 2014;45:1006-1010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 44] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 9. | Socci AR, Casemyr NE, Leslie MP, Baumgaertner MR. Implant options for the treatment of intertrochanteric fractures of the hip: rationale, evidence, and recommendations. Bone Joint J. 2017;99-B:128-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 180] [Article Influence: 20.0] [Reference Citation Analysis (0)] |
| 10. | Hu J, He C, Liu F, Wen F. [Application of wire reduction technique guided by minimally invasive wire introducer in treatment of difficult-reducing intertrochanteric fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2019;33:1245-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Bo Y, Qin Y, Zang Y, Yang H. The suitable fixation for unstable intertrochanteric fractures: A protocol of comparative clinical study. Medicine (Baltimore). 2020;99:e23046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Mallya S, Kamath SU, Madegowda A, Krishnamurthy SL, Jain MK, Holla R. Comparison of radiological and functional outcome of unstable intertrochanteric femur fractures treated using PFN and PFNA-2 in patients with osteoporosis. Eur J Orthop Surg Traumatol. 2019;29:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Yu X, Wang H, Duan X, Liu M, Xiang Z. Intramedullary vs extramedullary internal fixation for unstable intertrochanteric fracture, a meta-analysis. Acta Orthop Traumatol Turc. 2018;52:299-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 58] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 14. | Karakus O, Ozdemir G, Karaca S, Cetin M, Saygi B. The relationship between the type of unstable intertrochanteric femur fracture and mobility in the elderly. J Orthop Surg Res. 2018;13:207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Wang R, Zhang H, Wei Q, Ding C, Cao L, Yi M, Tong D, Li D, Fan Z, Wu D, Ji F, Tang H. Intramedullary nails in combination with reconstruction plate in the treatment of unstable intertrochanteric femoral fractures with lateral wall damage. Int Orthop. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 16. | Shu WB, Zhang XB, Lu HY, Wang HH, Lan GH. Comparison of effects of four treatment methods for unstable intertrochanteric fractures: A network meta-analysis. Int J Surg. 2018;60:173-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Liu W, Liu J, Ji G. Comparison of clinical outcomes with proximal femoral nail anti-rotation vs InterTAN nail for intertrochanteric femoral fractures: a meta-analysis. J Orthop Surg Res. 2020;15:500. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Zheng H, Zhang Y, Wang H, Sun T, Sun Q. Comparison of perioperative hidden blood loss for intertrochanteric fractures in the elderly by different intramedullary fixations: A randomized controlled study protocol. Medicine (Baltimore). 2020;99:e21666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 19. | Calvo-Haro JA, Pascau J, Mediavilla-Santos L, Sanz-Ruiz P, Sánchez-Pérez C, Vaquero-Martín J, Perez-Mañanes R. Conceptual evolution of 3D printing in orthopedic surgery and traumatology: from "do it yourself" to "point of care manufacturing". BMC Musculoskelet Disord. 2021;22:360. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ulici A S-Editor: Zhang H L-Editor: Filipodia P-Editor: Zhang YL