Published online Nov 16, 2021. doi: 10.12998/wjcc.v9.i32.10006
Peer-review started: July 2, 2021
First decision: July 16, 2021
Revised: July 19, 2021
Accepted: September 8, 2021
Article in press: September 8, 2021
Published online: November 16, 2021
Processing time: 130 Days and 21.3 Hours
Postoperative pain following total hip arthroplasty (THA) may occur in a few patients but may pose a significant challenge to surgeons if the etiology is not identified. Herein, we report the case of a patient who developed late-onset pain following THA due to screw penetration of the iliopsoas tendon.
We report the case of a 77-year-old man who developed inguinal pain 7 years after THA. While the symptoms resembled that of iliopsoas impingement by the acetabular cup, the pain resolved only when the supplementary acetabular screw protruding through the ilium was decompressed. Decompression was performed using the pararectus approach. The patient was able to ambulate pain-free immediately after surgery.
A protruded screw through the ilium may penetrate the iliopsoas muscle, causing pain following THA. Pain may resolve with the decompression of the protruded screw.
Core Tip: The acetabular screws are mostly positioned in the posterolateral quadrant and rarely protrude through the anterior ilium. However, when supplementary screw is protruded anteriorly and penetrate through iliopsoas muscle, the symptom may resemble that of the iliopsoas impingement by acetabular cup. Instead of removing the entire screw, which would require dislocation of the hip and disassembly of the ceramic liner, flatten the protruded portion of the screw with the para-rectus approach may relieve the symptom.
- Citation: Park HS, Lee SH, Cho HM, Choi HB, Jo S. Screw penetration of the iliopsoas muscle causing late-onset pain after total hip arthroplasty: A case report. World J Clin Cases 2021; 9(32): 10006-10012
- URL: https://www.wjgnet.com/2307-8960/full/v9/i32/10006.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i32.10006
Primary total hip arthroplasty (THA) is recognized as a safe and satisfactory intervention; however, postoperative pain may occur in some patients. Pain may be attributed to various etiologies, including periprosthetic infection, implant loosening, or irritation from various causes1]. Conversely, several patients develop pain after THA due to unidentified reasons. These patients may undergo extensive spine evaluation or psychological assessment, and in some cases, the pain may require revision surgery even when mechanical complications of the prosthesis are not confirmed[2]. Herein, we report a case in which a supplemental screw on the acetabular cup initiated iliopsoas irritation. We suggest that this may be a potential cause of late-onset pain in patients who undergo THA.
A 77-year-old man was referred to our institution because of right inguinal pain.
The patient’s symptoms developed a month ago without any trauma to the hip joint. The pain worsened over 1 mo before the patient decided to visit our clinic.
The patient did not have any relevant past illness since the index THA was performed.
The patient had undergone THA due to post-traumatic osteoarthritis 7 years prior and had no discomfort following the surgery. The index surgery was performed using a direct lateral (modified Hardinge) approach with a non-cemented prosthesis (Delta PF cup, C2 stem; Lima, Italy) and ceramic-on-ceramic bearings and two supplementary screws were used for fixation of the acetabular cup.
At the time of the visit, the patient was unable to walk because of pain, with a visual analog scale (VAS) score of 9. The pain was localized in the inguinal region with mild tenderness at the site, which was exacerbated by hip extension.
All results from routine laboratory tests, which included serum erythrocyte sedimentation rate and C-reactive protein levels for the detection of periprosthetic infection, were within the normal range.
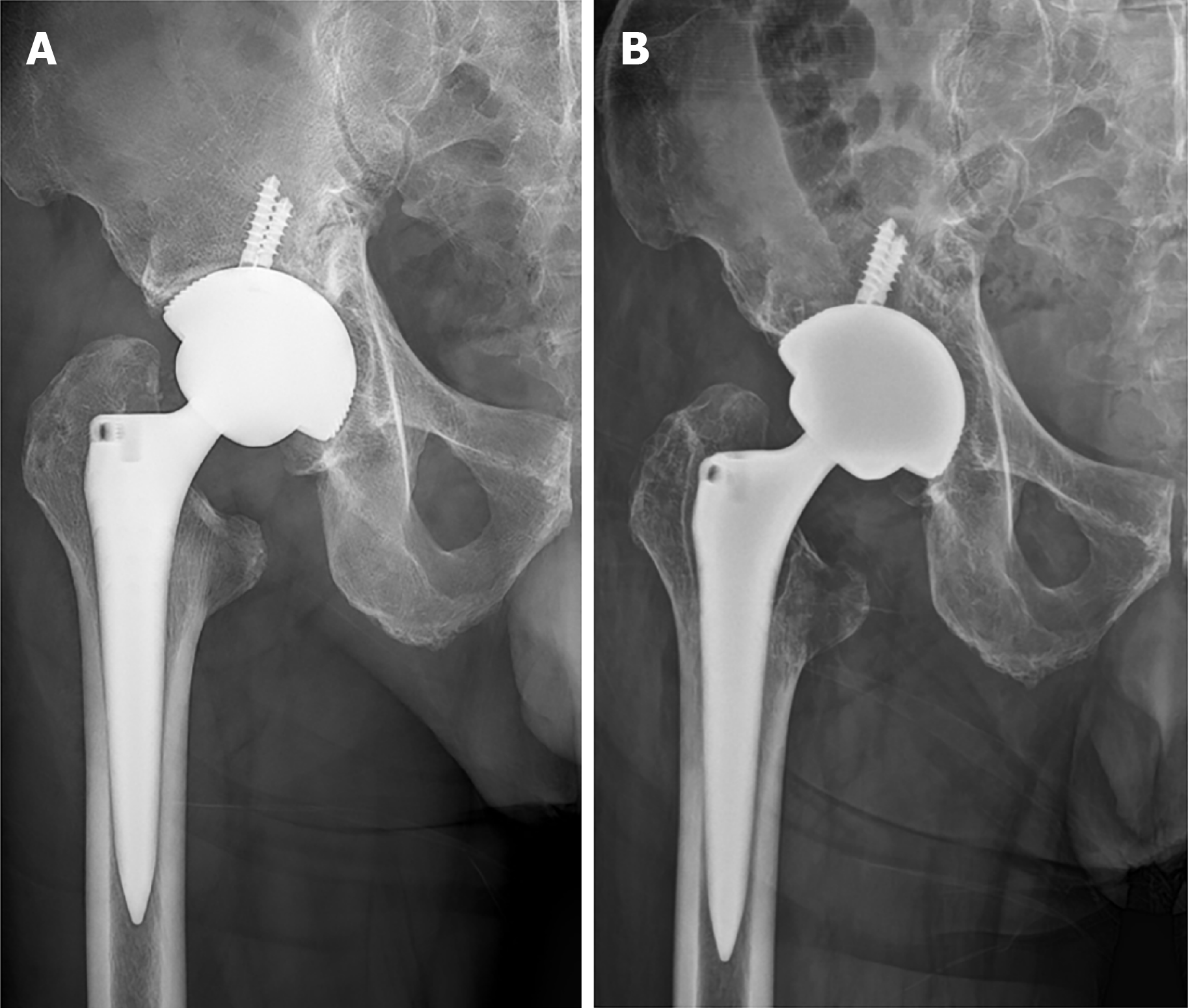
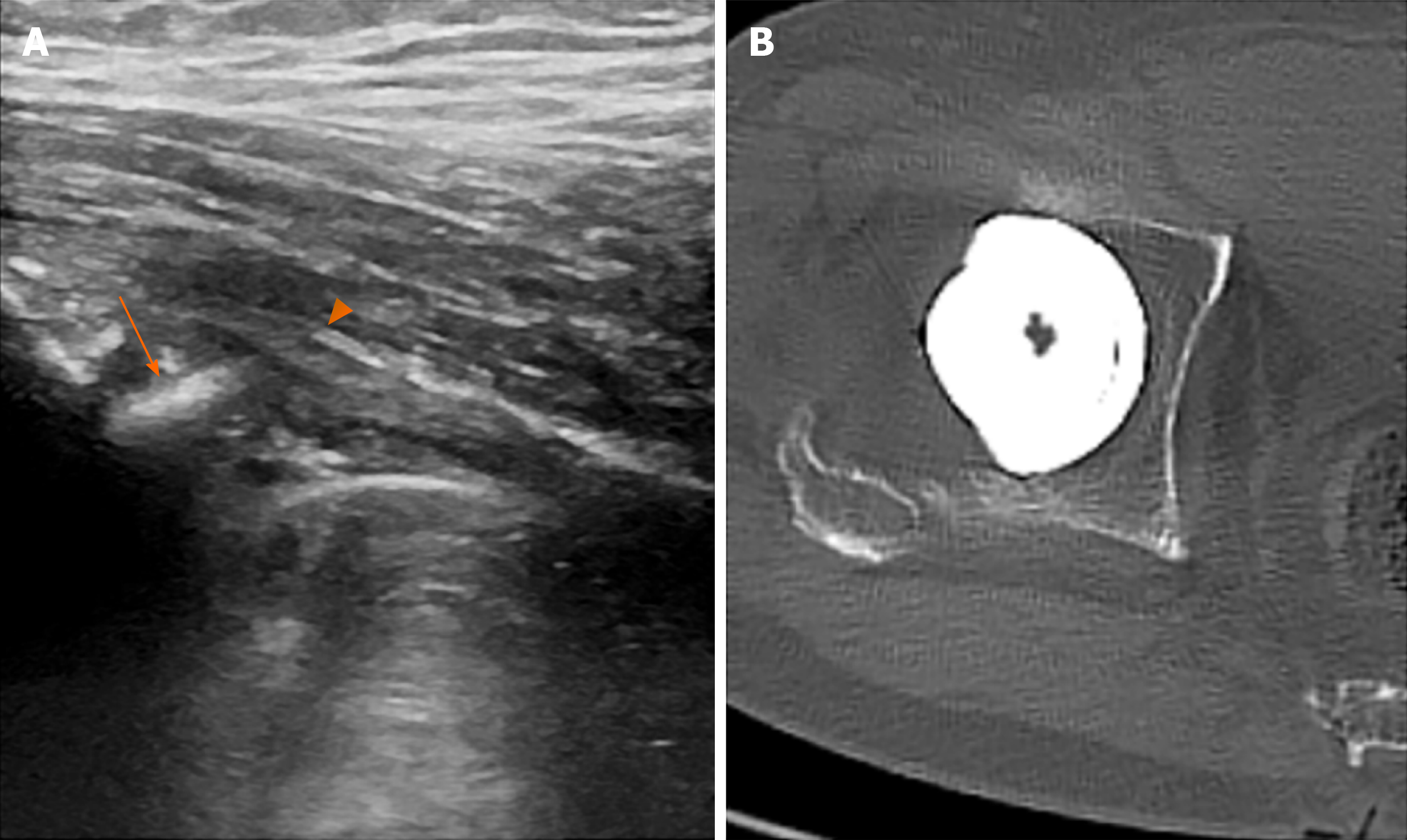
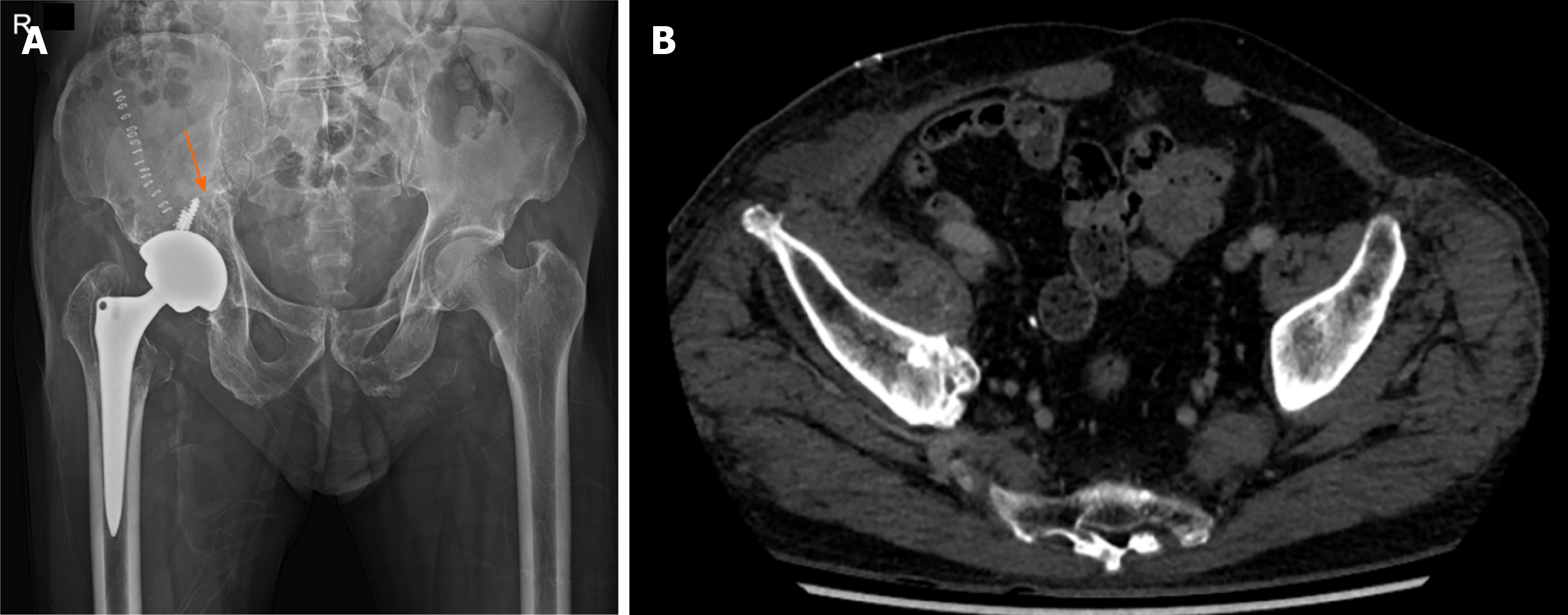
The immediate postoperative radiograph following the index THA was compared with a simple radiograph taken at the time of the visit. On the femoral side, bone resorption in the Charnley and Gruen zones[3,4] 1 and 7 were observed, and in the acetabular side, slight bone resorption was observed in zone 2 (Figure 1). A bone scan with WBC-marrow imaging showed no evidence of infection[5]. Thorough lumbar spine inspection, including magnetic resonance imaging (MRI), showed mild disc bulging at L4-5. On sonography of the hip joint, no joint fluid was observed near the prosthesis; however, a slight protrusion of the anterior rim of the acetabular cup was observed. The cup was placed at 39° of abduction, and the anteversion was - 9° (Figure 2).
While low-grade infection was suspected, psoas impingement due to acetabular retroversion was suggested to be a potential cause of pain. Ultrasound-guided injection of an analgesic was performed at the insertion of the iliopsoas tendon (IPT), and the pain subsided immediately. With the given information, the diagnosis of iliopsoas impingement due to the acetabular cup was established. The patient underwent 3 mo of conservative treatment without improvement, and the decision to perform arthroscopic iliopsoas release was made.
Arthroscopic iliopsoas release was performed using the established method[6] using the anterolateral and mid-anterior portals. Before fluid was loaded into the joint, capsule samples were retrieved for tissue culture, which later confirmed the absence of bacteria. During surgery, thickening of the anterior capsule was observed, which was decompressed along with the tendinous portion of the IPT. The patient’s pain improved to VAS 2 after the surgery; pain during walking persisted but was endurable. The patient was followed up at 3-mo intervals, with the pain persisting and ranging between VAS 2 and 3.
Fourteen months after the surgery, the patient developed the same pain that occurred prior to the iliopsoas release surgery. The patient was unable to walk, and the range of motion of the hip was unattainable due to pain. The patient’s pain was limited to the inguinal region but also somehow radiated to the anterior thigh.
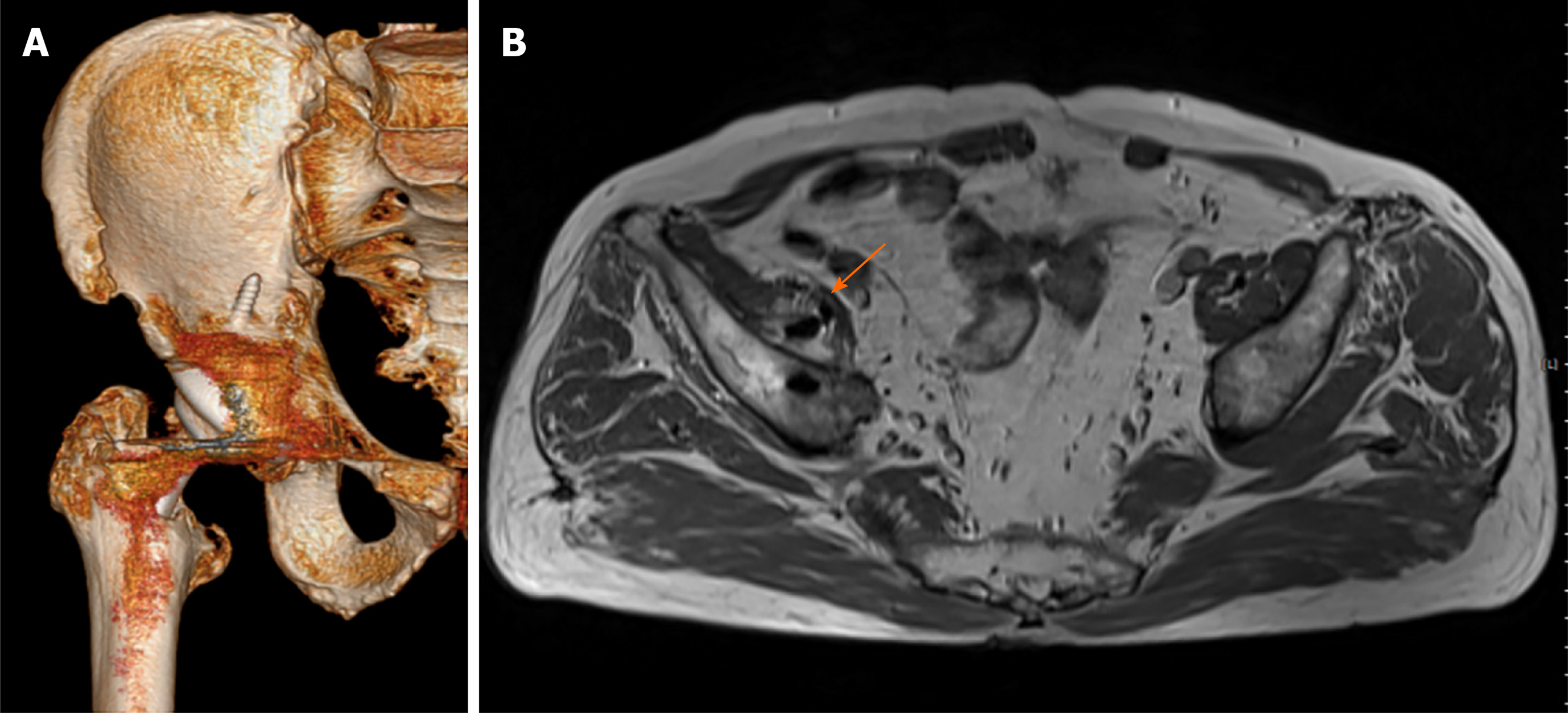
The simple radiograph showed no difference from the radiograph taken at the time of the first visit to our institution; again, there was no sign of infection. Ultrasound-guided injection of an analgesic to the IPT again resulted in complete resolution of pain for 2 days. At this time, Computed tomography (CT) with three-dimensional reconstruction and MRI with a metal suppression sequence were performed. CT revealed that the tip of the screw used for the acetabular cup fixation protruded out of the anterior ilium. The MRI revealed fluid collection in the iliopsoas muscle adjacent to the screw tip (Figure 3).
We concluded that the patient’s inguinal pain was due to iliopsoas muscle penetration by the screw.
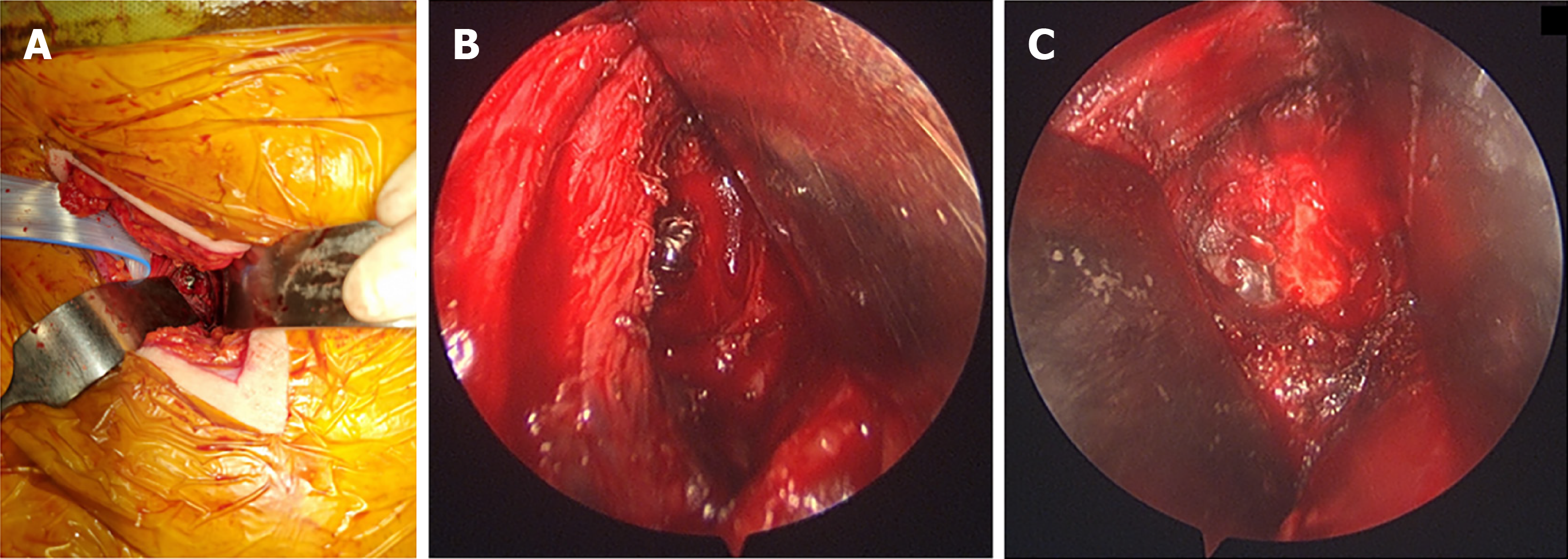
Instead of removing the entire screw, which would require dislocation of the hip and disassembly of the ceramic liner, we decided to flatten the protruded portion of the screw. The pararectus approach[7] was used for exposure. On exploration of the iliopsoas, we observed a hematoma where the screw tip protruded. Tissue culture was performed to differentiate potential infections and was found to be negative. The protruded tip of the screw was approximately 1.8 mm long and was flattened to the ilium surface using a high-speed burr (Legend Diamond ball burr; Medtronic, United States; Figure 4).
Complete resection of the protruded screw tip was observed on postoperative radiographs (Figure 5). The pain completely subsided when the patient recovered from general anesthesia, and the patient was able to walk pain-free the next day. The patient was followed up for a year without pain and no radiographic changes.
The results of THA are mostly satisfactory, and surgical interventions are often without complications. However, pain may persist in some patients for various reasons. The cause of the pain may be unidentified in a limited number of patients.
More recently, iliopsoas impingement has been suggested as a potential cause of postoperative pain and has been reported to occur in up to 4.3% of patients undergoing THA[8]. This impingement is suggested to be caused by a retroverted or large acetabular cup[9]. The acetabular cup was retroverted by 9 in our case, and since the patient’s pain improved following the iliopsoas injection, we initially suspected iliopsoas impingement from cup malposition. It is likely that our analgesic injection to the IPT may have spread along the IPT and may have anesthetized the muscular portion in which the screw was penetrating. Similarly, arthroscopic release of the IPT may have elongated the tendon, causing less stress to the muscle, resulting in decreased but persistent pain.
Reports of iliopsoas impingement by supplementary acetabular screws are extremely rare. The acetabular screws are mostly positioned in the posterolateral quadrant and rarely protrude through the anterior ilium[10]. The anteriorly placed acetabular screw may pass proximal to the external iliac vessels and should be avoided if possible. However, even when it protrudes in this region, it is often not taken seriously and is not considered a cause of pain. However, iliopsoas travels adjacent to the ilium, and if the screw is long enough, this may result in irritation of the iliopsoas muscle.
To the best of our knowledge, there is one case report that reported a similar pheno
The current case varies from the previous report in that late-onset pain following THA occurred due to an acetabular screw. It remains unknown why the pain did not begin immediately following surgery and started after 7 years. One assumption would be the patient’s change in the spinopelvic alignment; that is, if the patient developed pelvic anteversion, this may tighten the iliopsoas, making it more prone to irritation from the screw[12]. However, this theory remains unproven. Additionally, we could resolve the problem by simple decompression using the pararectus approach, which provides early ambulation and less economic burden for the patient. We believe this is the first case report that suggests that a supplementary screw penetrating the iliopsoas muscle may cause late-onset pain.
A supplementary screw penetrating the iliopsoas muscle after THA may cause late-onset pain. With advancements in surgical techniques, the problem can be solved simply by using the pararectus approach. We recommend using advanced imaging to confirm the relationship between the screw and iliopsoas muscle when the pain is unexplainable.
| 1. | Henderson RA, Lachiewicz PF. Groin pain after replacement of the hip: aetiology, evaluation and treatment. J Bone Joint Surg Br. 2012;94:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 67] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Classen T, Zaps D, Landgraeber S, Li X, Jäger M. Assessment and management of chronic pain in patients with stable total hip arthroplasty. Int Orthop. 2013;37:1-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Banaszkiewicz PA. "Modes of failure" of cemented stem-type femoral components: a radiographic analysis of loosening. In: Classic Papers in Orthopaedics. Springer, 2014: 35-38. [DOI] [Full Text] |
| 4. | Banaszkiewicz PA. Classic Papers in Orthopaedics. In: Radiological demarcation of cemented sockets in total hip replacement. Springer, 2014: 39-41. [DOI] [Full Text] |
| 5. | Palestro CJ, Love C, Tronco GG, Tomas MB, Rini JN. Combined labeled leukocyte and technetium 99m sulfur colloid bone marrow imaging for diagnosing musculoskeletal infection. Radiographics. 2006;26:859-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 106] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | May O. Arthroscopic techniques for treating ilio-psoas tendinopathy after hip arthroplasty. Orthop Traumatol Surg Res. 2019;105:S177-S185. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (1)] |
| 7. | Keel MJ, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Büchler L, Siebenrock KA, Bastian JD. The Pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012;94:405-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 128] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 8. | Dora C, Houweling M, Koch P, Sierra RJ. Iliopsoas impingement after total hip replacement: the results of non-operative management, tenotomy or acetabular revision. J Bone Joint Surg Br. 2007;89:1031-1035. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 156] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 9. | Batailler C, Bonin N, M Wettstein, Nogier A, Martres S, Ollier E, May O, Lustig S; French Arthroscopy Society (SFA). Outcomes of cup revision for ilio-psoas impingement after total hip arthroplasty: Retrospective study of 46 patients. Orthop Traumatol Surg Res. 2017;103:1147-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 43] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 10. | Wasielewski RC, Cooperstein LA, Kruger MP, Rubash HE. Acetabular anatomy and the transacetabular fixation of screws in total hip arthroplasty. J Bone Joint Surg Am. 1990;72:501-508. [PubMed] |
| 11. | Mayne IP, Kosashvili Y, White LM, Backstein D. Iliopsoas tendonitis due to the protrusion of an acetabular component fixation screw after total hip arthroplasty. J Arthroplasty. 2010;25:659.e5-659.e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Asai H, Tsuchiyama H, Hatakeyama T, Inaoka PT, Murata K. Age-related Changes in Maximum Pelvic Anteversion and Retroversion Angles Measured in the Sitting Position. J Phys Ther Sci. 2014;26:1959-1961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Provenance and peer review: Unsolicited article; Externally peer reviewed
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Feng J S-Editor: Wang JJ L-Editor: A P-Editor: Yu HG