Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9244
Peer-review started: May 26, 2021
First decision: June 15, 2021
Revised: June 15, 2021
Accepted: July 28, 2021
Article in press: July 28, 2021
Published online: October 26, 2021
Processing time: 147 Days and 18.8 Hours
Pseudomonas aeruginosa (P. aeruginosa) is considered a common pathogenic bac
We describe the diagnostic and treatment processes of a case involving a complex choroidal space-occupying lesion. Our analyses of early clinical manifestations revealed a high possibility of choroidal melanoma, as indicated by the choroidal space-occupying lesion and uveitis. Further magnetic resonance imaging results revealed no positive evidence for the diagnosis of choroidal melanoma. The exact properties of the space-occupying lesion could not be ascertained prior to surgery. However, the lesion was subsequently confirmed as a metastatic abscess by diagnostic vitrectomy. The occupying lesion was found to occupy 75% of the vitreous cavity in the surgery. The entire white viscous tissue was completely removed, and the necrotic retina was cleaned up. After surgery, microbiological culture revealed mucoid P. aeruginosa, which was sensitive to a variety of antibiotics. The bacterial infection grew and disseminated towards the outside of the eye. After the fifth injection, the left eye was successfully retained.
This is a peculiar case because a huge, local, space-occupying lesion had formed due to the dissemination of low-toxic mucinous P. aeruginosa in the blood from the lungs to the choroid. After surgical removal, the bacteria were able to re-grow; thus, local infection re-spread following surgery. The patient lost vision, but we managed to retain the full structure of the eyeball and eliminated the focus of infection.
Core Tip: Pseudomonas aeruginosa (P. aeruginosa) is considered a common pa
- Citation: Li Z, Gao W, Tian YM, Xiao Y. Choroidal metastatic mucinous abscess caused by Pseudomonas aeruginosa: A case report. World J Clin Cases 2021; 9(30): 9244-9254
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9244.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9244
Pseudomonas aeruginosa (P. aeruginosa) is considered a common pathogenic bacterium. We present herein a rare case of choroidal metastatic mucinous abscess caused by P. aeruginosa.
A 52-year-old female patient of Han nationality was admitted to hospital on December 18, 2020 due to the primary symptom of pain in the left eye and loss of vision for over 2 wk (Table 1). The patient had felt pain in the left eye since the December 1, 2020 and experienced reduced levels of vision in this eye without any other predisposing factors or causes.
| Age | Sex | Occupation | Family history | Previous condition | |
| Patient information | 52 | Female | Farm worker | None | Hypertension |
The patient went to a local hospital and was diagnosed with iridocyclitis of the left eye. The patient’s symptoms eased after the administration of semi-retrobulbar triamcinolone acetonide injections and hormone eyedrops. However, the symptoms subsequently reappeared with an intensified headache. The acupuncture department of the local hospital performed acupuncture and moxibustion treatment while blo
Hypertension.
There was no personal and family history.
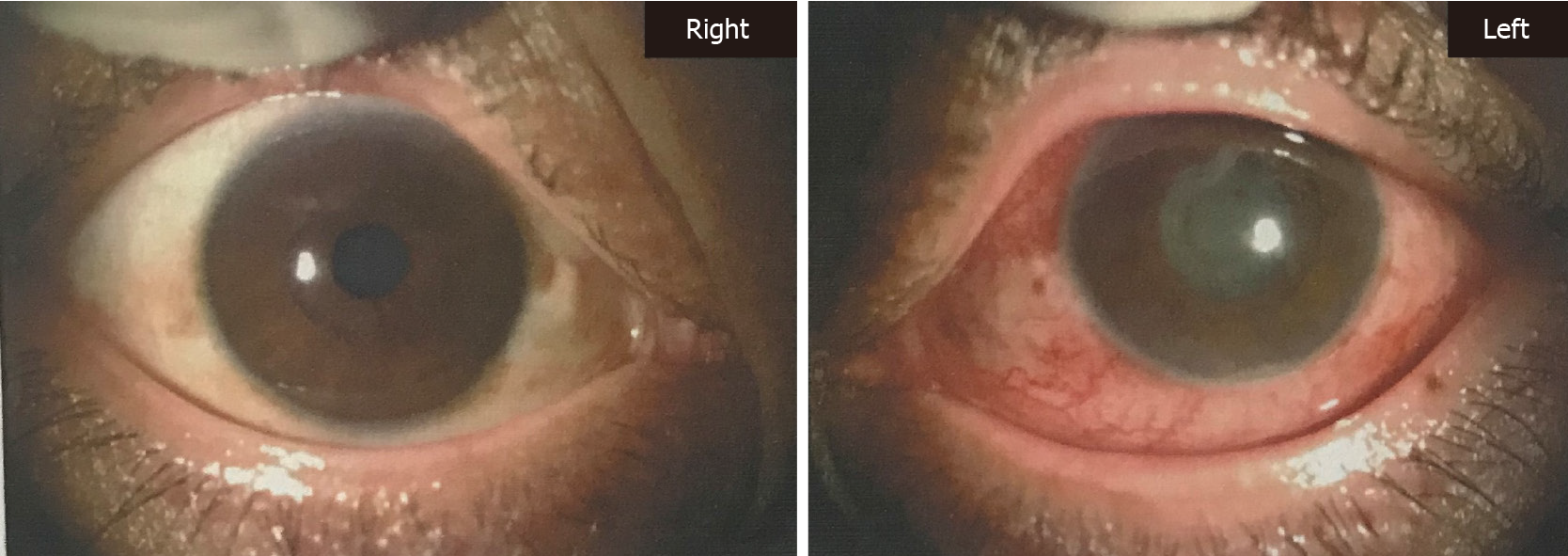
Physical examination revealed that the visual acuity in the right eye was 0.6; the left eye was reactive to light and the skin on the left upper eyelid was bruised. We also observed conjunctival congestion, a transparent cornea, visible floating cells in the anterior chamber with a small amount of empyema below, mydriasis (5 mm), ad
None.
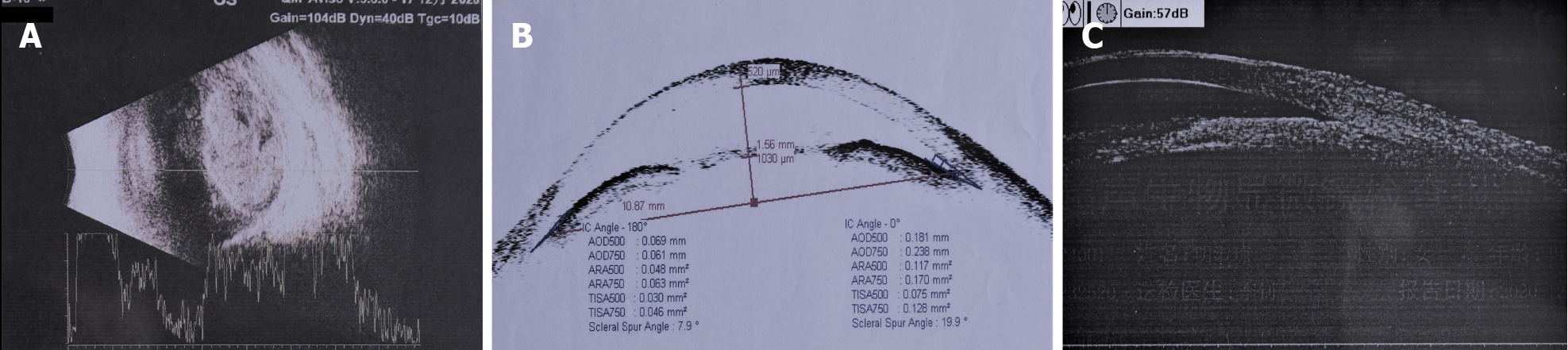
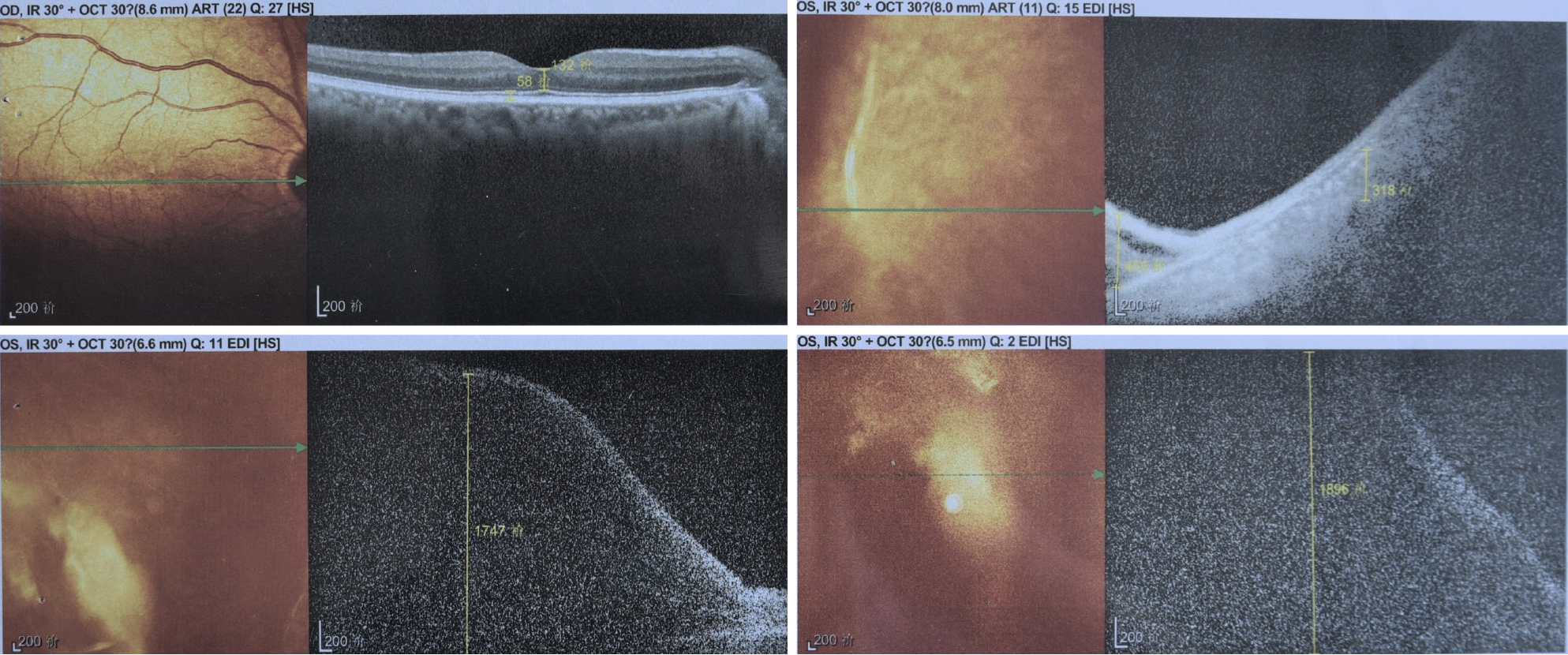
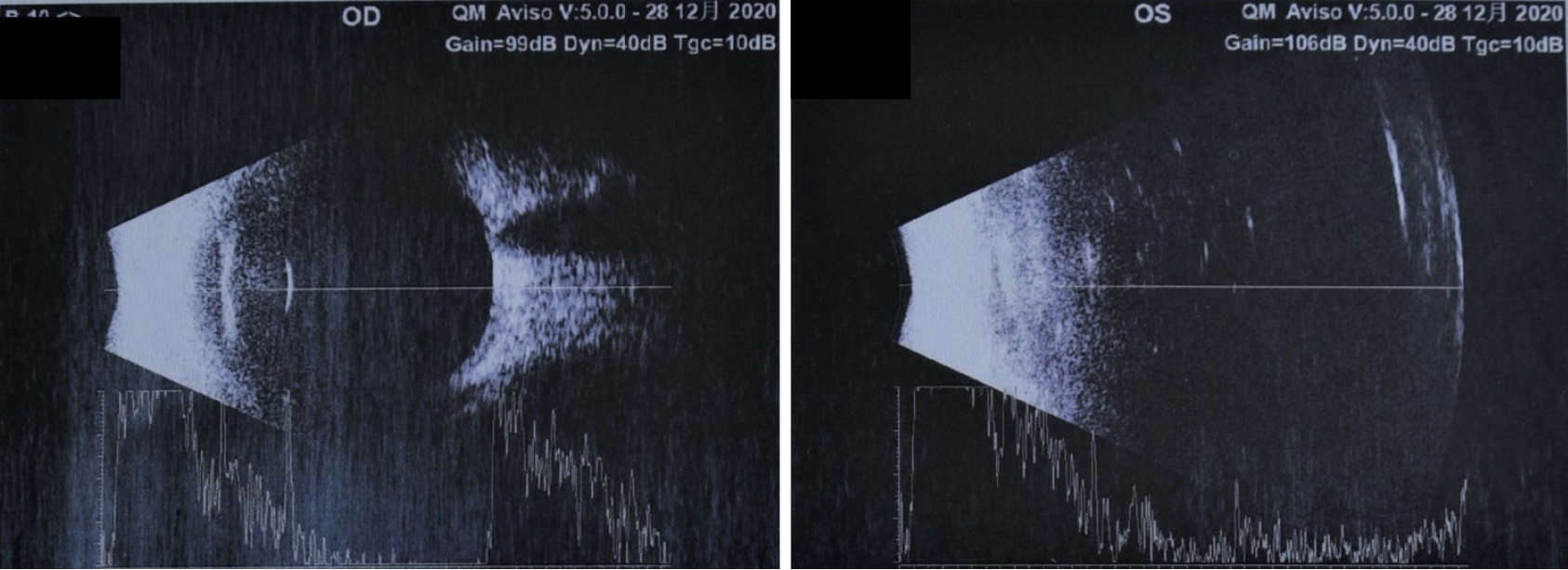
Ultrasonic biomicroscopy (UBM) examination revealed swelling of the iris root in both eyes, an expanded turbid anterior chamber in the left eye, shallow partial detachment of the ciliary body, and positive suprachoroidal effusion. Anterior segment optical coherence tomography (OCT) revealed closure of the left eye from 7 to 10 o’clock, along with edema and infiltration of cornea. Ultrasound revealed a normal optical axis in both eyes, vitreous opacity in the right eye, and vitreous turbidness in the left eye (potentially indicating hemorrhage). Ultrasound also revealed a choroidal lesion in the left eye. Color Doppler ultrasound revealed a normal optical axis in the left eye and a solid space-occupying lesion within the left eyeball. No valid data could be acquired from the corneal endothelium in the left eye (Figure 3).
Abdominal ultrasound further revealed a fatty liver and a frizzy gallbladder wall, although no abnormalities were detected in the spleen.
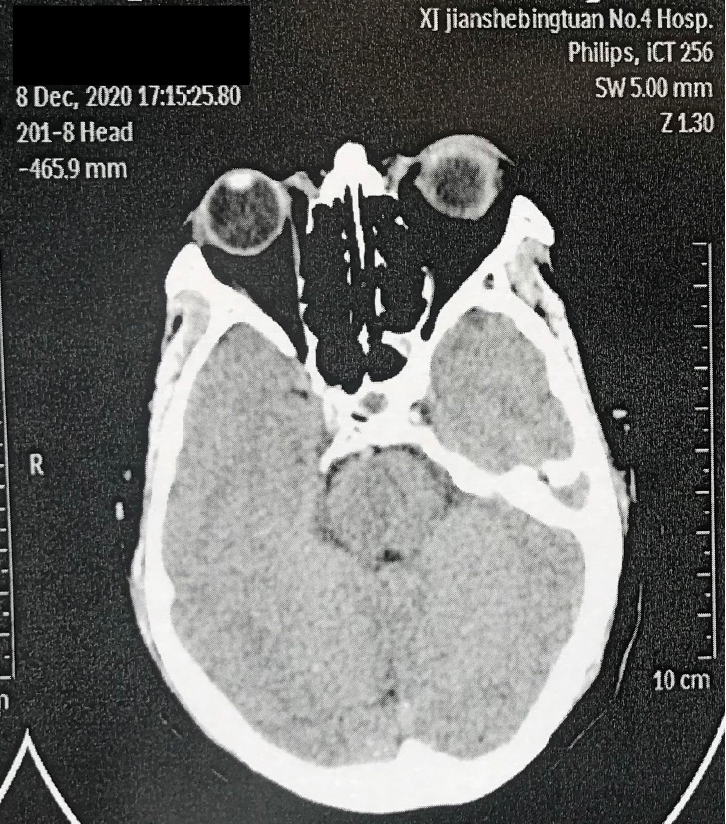
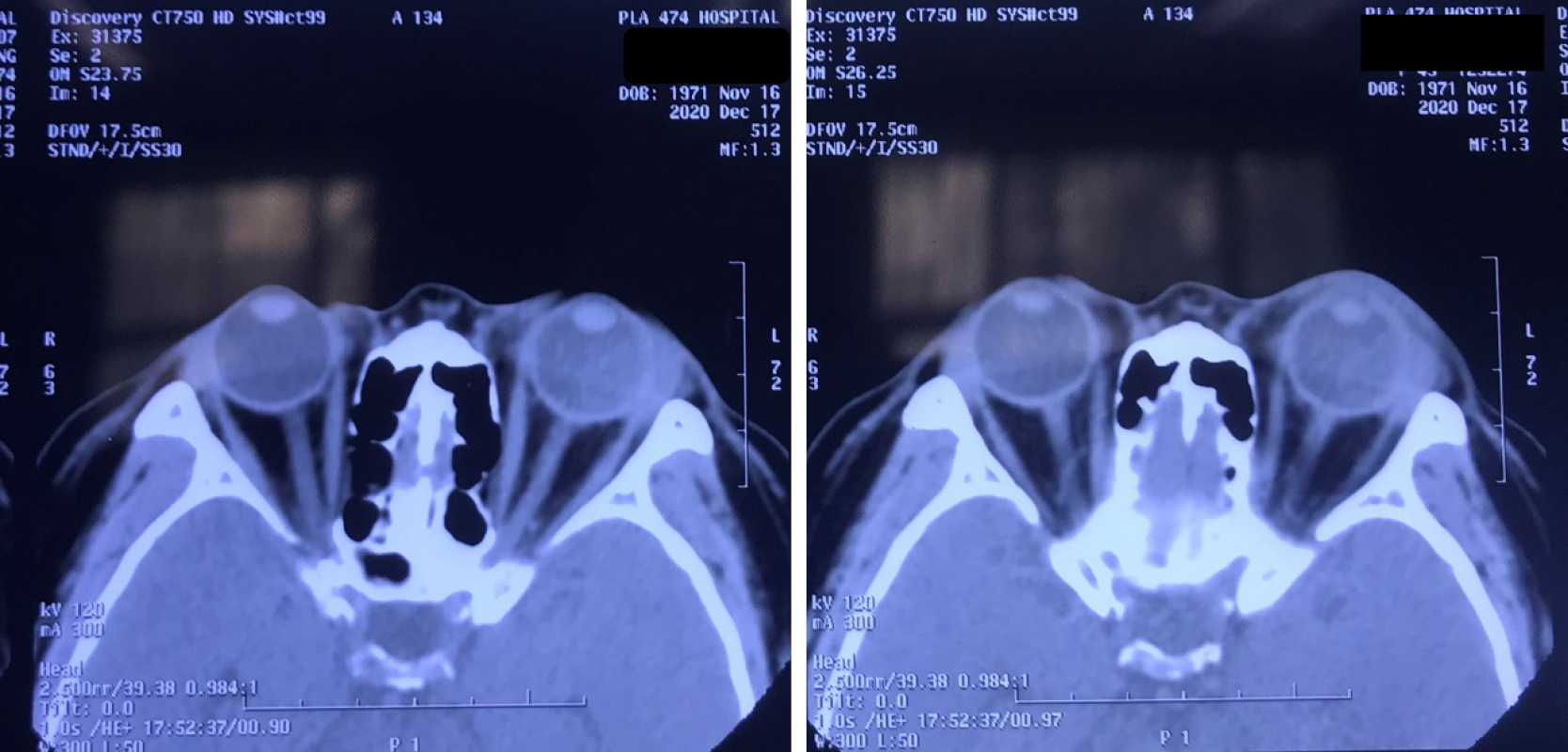
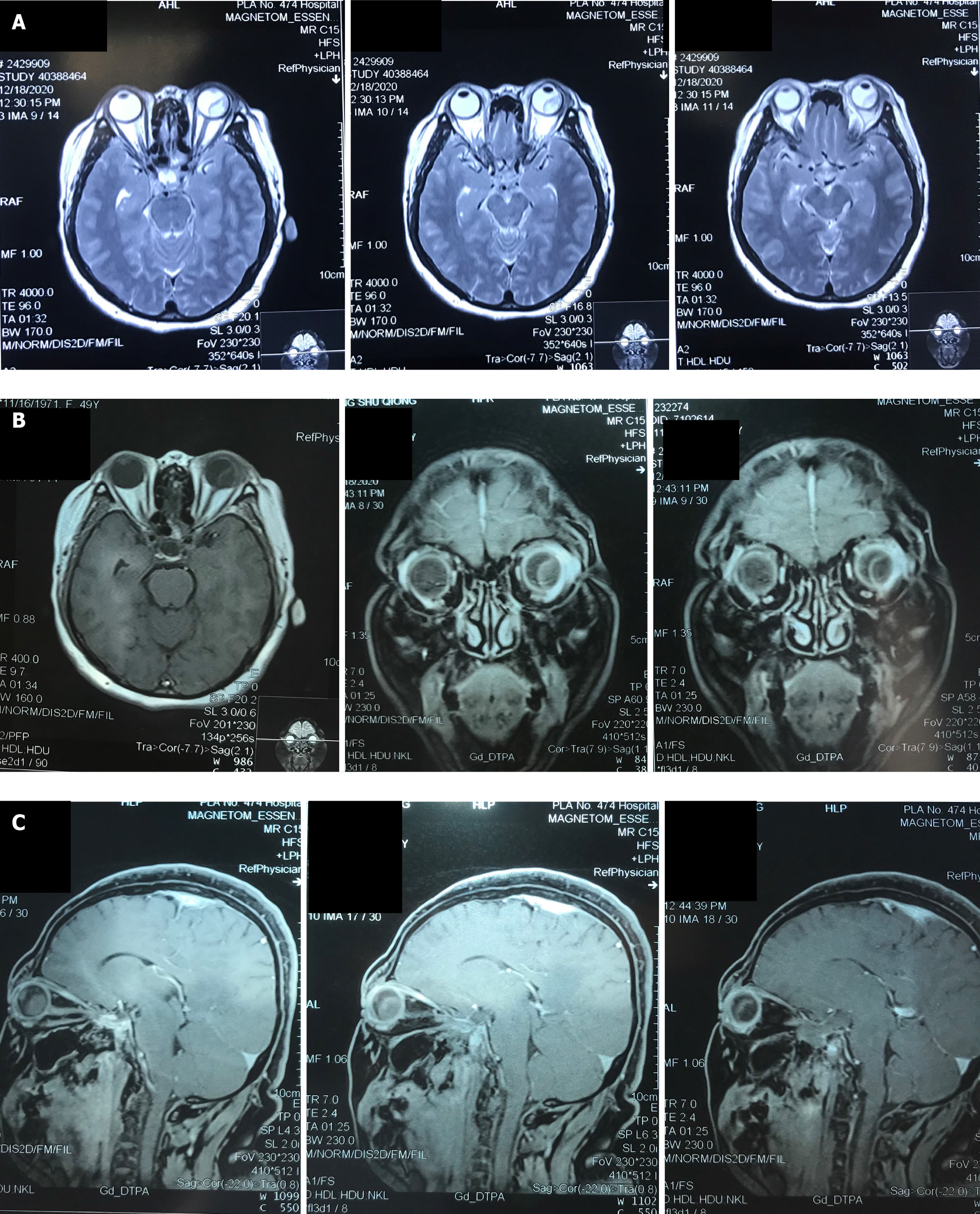
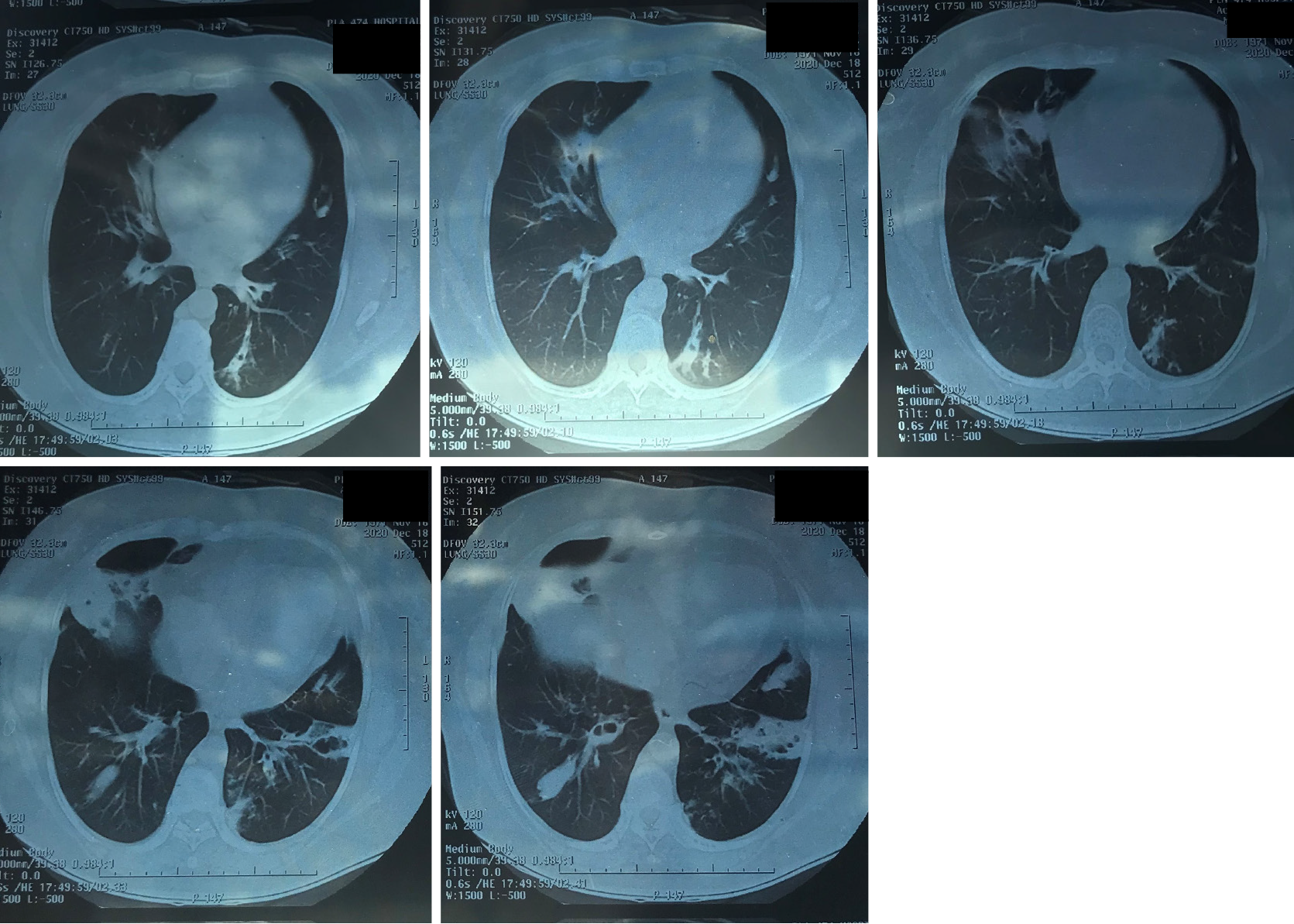
Eye CT (with enhancement) revealed slight enlargement as well as prolapse of the lacrimal gland in the left eye (Figure 4). Fusiform images showed a slightly higher density on the inner temporal side of the left eyeball when compared to the right eyeball. MRI examination revealed a thickened left eyelid, an enlarged and prolapsed lacrimal gland, a little oozing around the eyeball, and potential evidence for infectious disease. MRI also revealed a fusiform shadow of abnormal signals on the temporal side of the left eyeball, for which prolapse and hematoma of the choroid or retina were considered (Figure 5). Chest CT examinations revealed bronchiectasis and infection of both lungs, along with the formation of mucus plugs in the inferior lobe of the right lung (Video).
According to the diagnosis of uveitis and intraocular placeholder of the left eye and treatment in the local hospital, the conditions of the eye anterior segment, and the auxiliary examination results, our initial considerations for diagnosis were as follows: (1) Masquerade syndrome of the left eye; (2) a choroidal occupying lesion in the left eye[1] (indicating a high possibility of choroidal melanoma); (3) secondary glaucoma of the left eye; or (4) cataract of the left eye. The patient initially presented with uveitis and imaging results revealed choroidal occupation; these observations were in line with the diagnostic criteria for masquerade syndrome. There was a high possibility of a choroidal occupying melanoma. Typical manifestations of high T1 signals and low T2 signals in MRI images, with enhancement, can be used for the specific diagnosis of choroidal melanoma[2]. While preparing for the enucleation of the suspected cho
The final diagnosis of the presented case is as follows: (1) Choroidal metastatic mucinous abscess of the left eye caused by P. aeruginosa; (2) endophthalmitis of the left eye; (3) secondary glaucoma of the left eye; and (4) cataract of the left eye.
Further CT and MRI scans (with enhancement) were conducted to fully examine the eyes, brain, and lungs. We also performed eye ultrasound of the corneal endothelium, anterior OCT, UBM, and optometry, and measured the intraocular pressure.
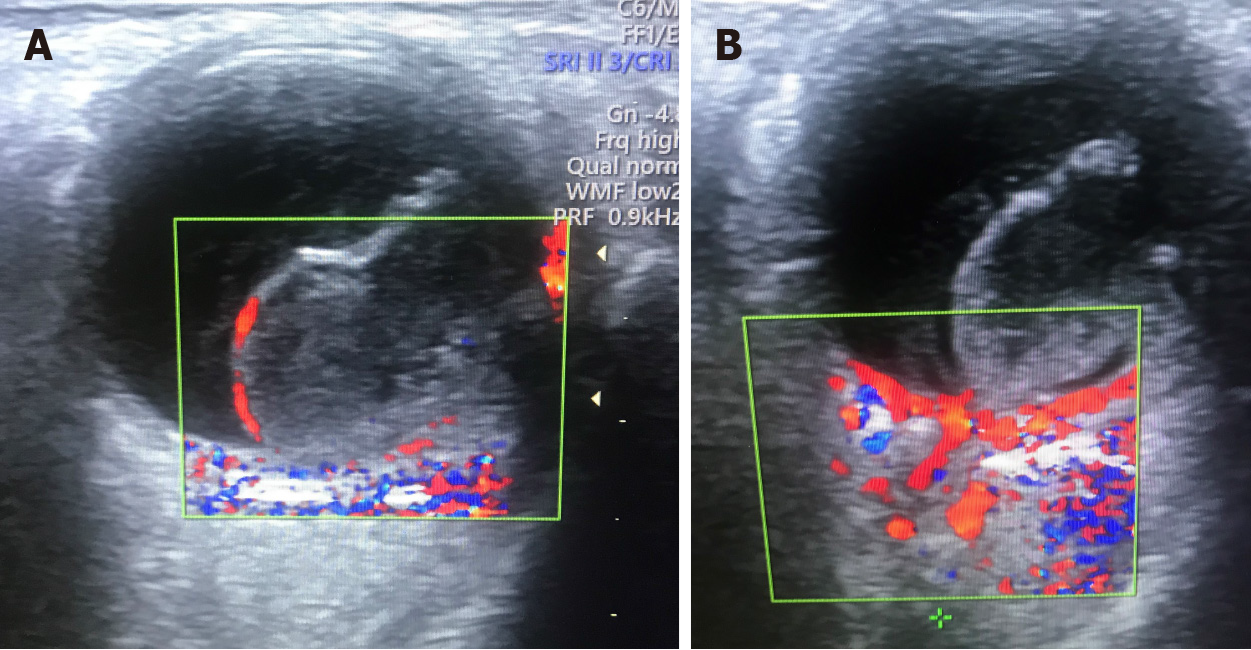
In order to further confirm the differential diagnosis responsible for the tumor and hemorrhage, we performed color Doppler ultrasound examination of the left eye[4]. Blood flow signals were seen in the entire periphery of the occupying lesion (Figure 6). However, there were no obvious blood flow signals in the solid portion in the middle of the lesion. This reduced the likelihood of the lesion being a tumor, although this could not be ruled out completely at this stage. It was not possible to visualize the vitreous cavity in the left eye due to the presence of a cataract. Consequently, we planned to observe the vitreous fundus following phacoemulsification of the cataract and subsequently analyze the nature of the occupying lesion and determine the appro
As the intraocular pressure increased and foggy edema appeared in the cornea of the left eye, it was considered that if the occupying lesion represented hemorrhagic disease, explosive suprachoroidal hemorrhage might occur if the anterior chamber was placed under pressure during phacoemulsification surgery. If the occupying lesion was a malignant tumor, there was also a risk that the phacoemulsification surgery might lead to the dissemination of tumor cells to the anterior chamber. Therefore, we considered it inappropriate to conduct phacoemulsification surgery.
After comprehensively analyzing the imaging results of the occupying lesion, and by considering the relative advantages and disadvantages, and obtaining the patient’s consent, we chose to remove the lens from the left eye and perform diagnostic vitrectomy supported by perfusion of the anterior chamber. This form of surgery could help us to remove the lens while maintaining a relatively safe status and offer opportunities to explore the possible nature of the occupying lesion. This would provide doctors with critical evidence to formulate subsequent decision-making. In addition, this form of surgery could also help us to detect whether the occupying lesion is a tumor or not. As soon as the results were confirmed, it would be possible for us to perform an immediate optical enucleation so as to minimize the risk of tumor cell dissemination.
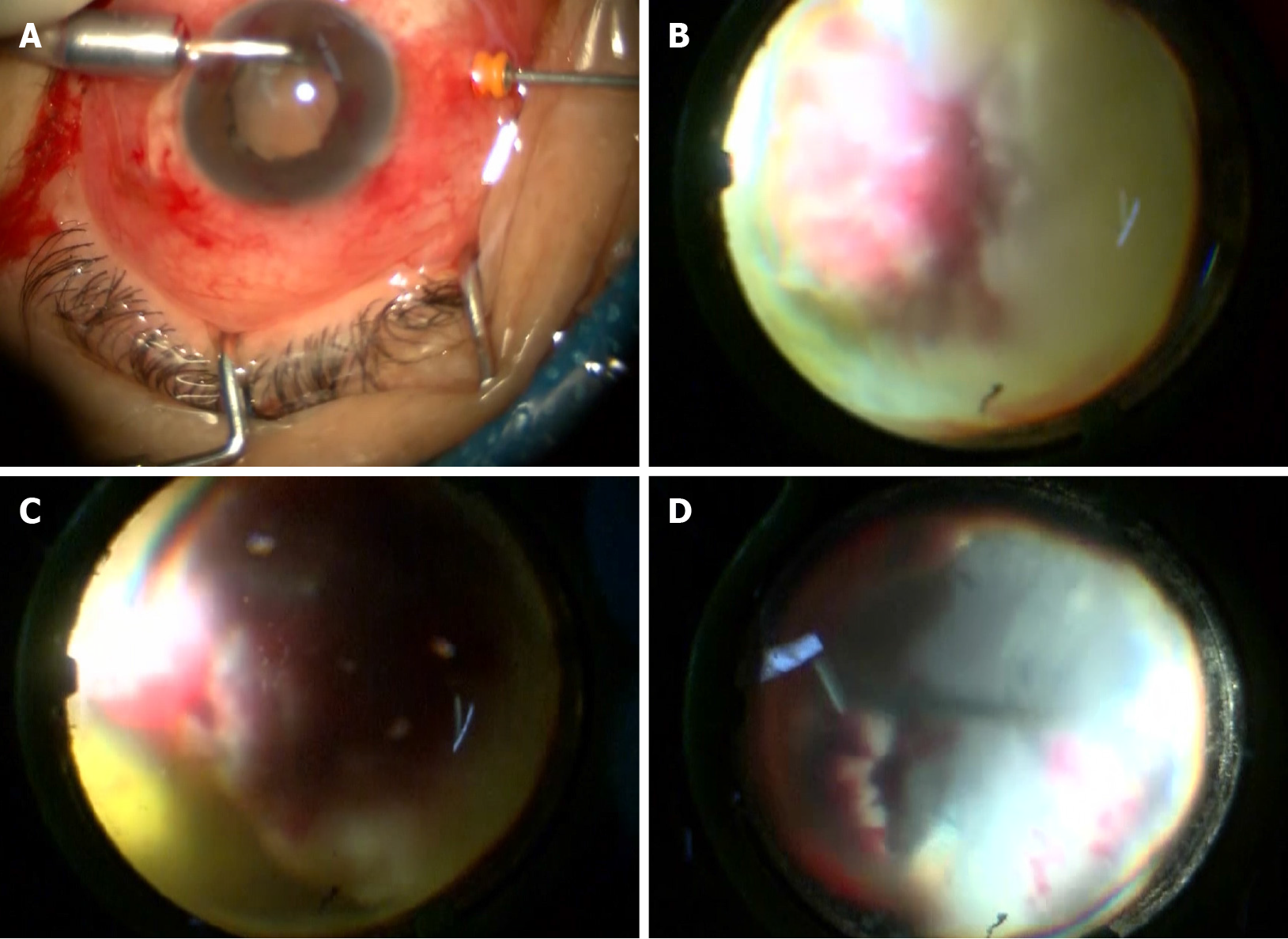
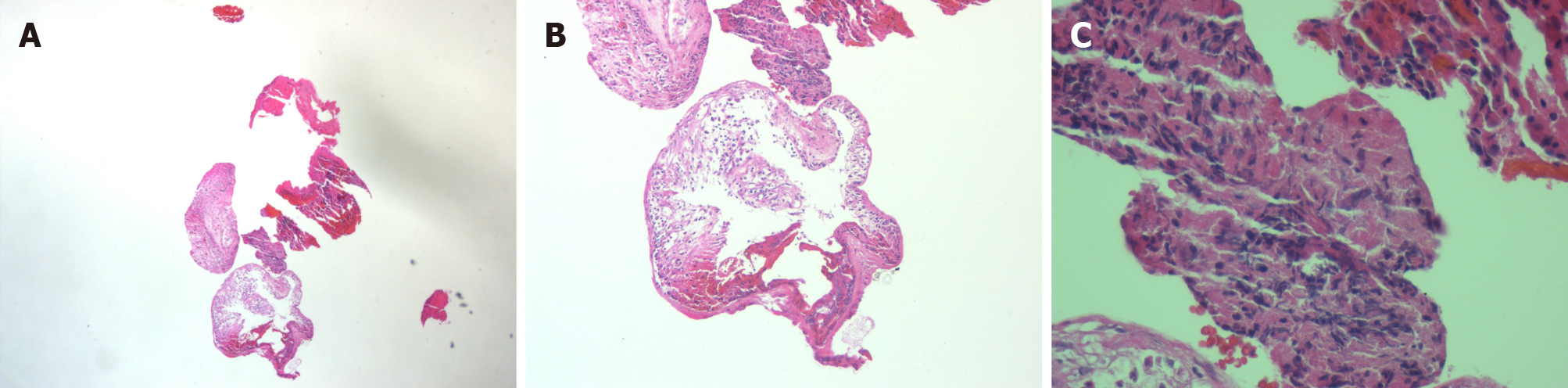
After careful preparation, surgeons successfully implanted a perfusion system into the corneoscleral tunnel. Once the anterior chamber was stable, surgeons were able to remove the lens. The occupying lesion was found to occupy 75% of the vitreous cavity. It was also found that the surface of the retinal tissues was necrotic and exhibited edema. Following dissection, a large amount of white viscous semi-solid tissue was found in the occupying lesion. The peripheral retina was also necrotic and denatured. The entire white viscous tissue was completely removed, and the necrotic retina was cleaned up. Only a small portion of the normal retinal tissue remained on the nasal side, accounting for approximately 20% of the vitreous cavity. The vitreous cavity was then filled with silicone oil. Necrotic tissues were extracted, and the white viscous tissue was sent for pathological examination and microbial culture (Figure 7).
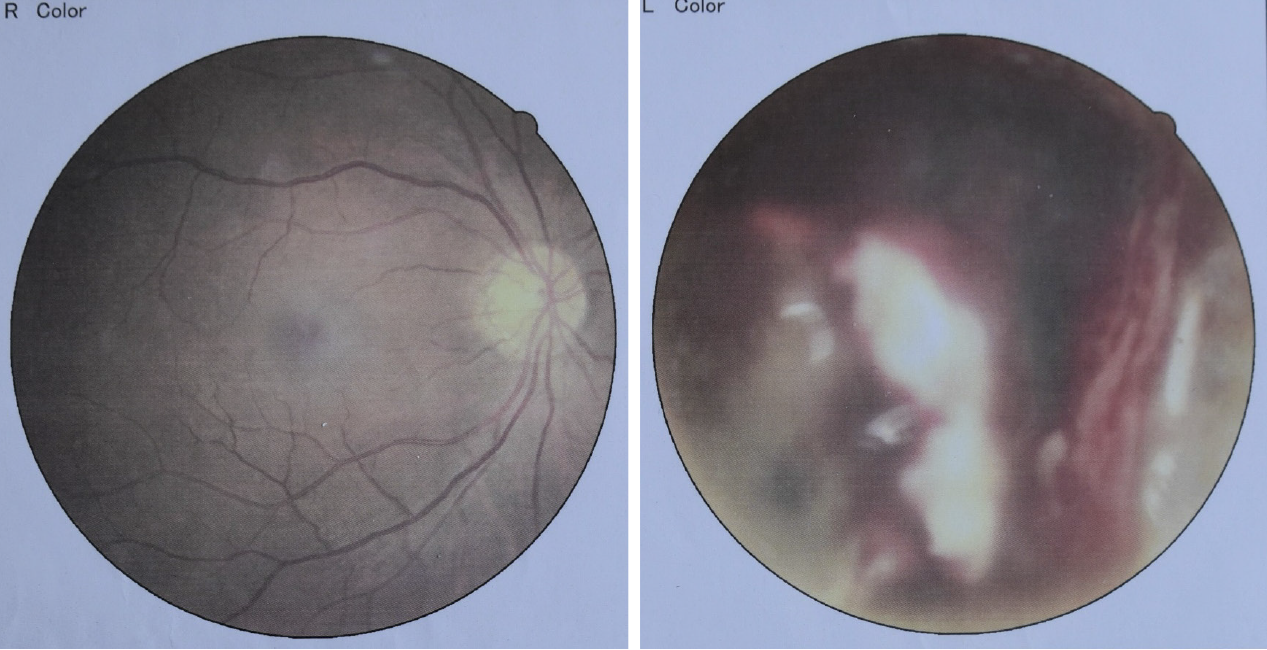
Three days after surgery, the cornea became bright, and the vitreous cavity turned clear. The scleral tissue, a small portion of the retina, and a small amount of the white viscous tissue became visible (Figures 8 and 9). We then administered an intravenous infusion of cefuroxime to prevent infection. Five days after surgery, pathological analysis was carried out (Figure 10); this revealed necrotic and inflammatory cell infiltration within the tissues of the left eye. Six days after surgery, microbiological culture revealed mucoid P. aeruginosa, which was sensitive to a variety of antibiotics (Tables 2 and 3). However, the conditions in the patient’s left eye suddenly deteriorated; the anterior chamber showed wide coverage of white turbidity. We were not able to visualize the iris clearly and there was moderate edema in the left eyelid, conjunctival congestion, edema, and headache. MRI revealed thickening of the eye ring and abnormal hillock signals in the rear of the eyeball. After analysis, it was believed that the lesion in the patient’s eye was infected with P. aeruginosa. Considering the patient’s past medical history and the results of CT examination, the patient was diagnosed with bronchiectasis and infection. Analysis of blood from the lungs subsequently revealed that the P. aeruginosa had disseminated into the choroidal blood vessels[5]. Due to the reduced blood flow, the bacteria had reproduced in the choroid and formed a mucinous abscess. The abscess was removed during surgery. This, combined with the application of silicone oil, and the systemic administration of antibiotics led to the local control of infection. However, the bacterial infection grew and disseminated towards the outside of the eye. This induced inflammation in the eye and the sur
| Antibacterial drug | MIC (mg/L) | Sensitivity | Antibacterial drug | MIC (mg/L) | Sensitivity |
| Cefepime | 26 | S | Amikacin | 20 | S |
| Ciprofloxacin | 22 | S | Gentamicin | 18 | S |
| Imipenem | 30 | S | Meropenem | 26 | S |
| Polymyxin | 19 | S | Piperacillin | 24 | S |
| Piperacillin/Taz | 32 | S | Ceftazidime | 20 | S |
| Aztreonam | 24 | S | Cefoperazone/Sul | 32 | S |
| Ofloxacin | 18 | S |
| Antibacterial drug | Method | Outcome | Sensitivity | Antibacterial drug | Method | Outcome | Sensitivity |
| Aztreonam | KB (mm) | 30 | S | Piperacillin/Taz | KB (mm) | 32 | S |
| Ampicillin | KB (mm) | 6 | R | Cefepime | MIC (mg/L) | ≤ 1 | S |
| Levofloxacin | MIC (mg/L) | 1 | S | Amikacin | MIC (mg/L) | ≤ 2 | S |
| Gentamicin | MIC (mg/L) | ≤ 1 | S | Imipenem | MIC (mg/L) | 2 | S |
| Compound trimethoprim | KB (mm) | 6 | R | Tobramycin | MIC (mg/L) | 2 | S |
The patient was admitted to the hospital with an occupying lesion in the left eye. In the context of unsupported imaging evidence, we considered other measures to analyze and diagnose the nature of the occupying lesion. However, as the patient’s condition was complicated by a severe cataract, the nature of the occupying lesion could not be diagnosed by observation through the fundus and observing its ap
It is evident that there is an urgent need to identify the exact nature of any occupying lesion. If there is an insufficient body of evidence, diagnostic surgical treatment can be conducted, if surgical indications are satisfied. Moreover, when this type of surgical treatment is conducted, doctors must consider the possibility of re-infection, as seen in the present case. The present case indicates that ophthalmologists must be open-minded when diagnosing and treating their patients. While seeking solutions to ophthalmological problems, ophthalmologists should also consider systemic problems rather than solely focusing on problems associated with the eyes. Furthermore, the impact of systemic problems can extend into local areas. Consequently, it is important that physicians consider their options from both a local and systemic point of view. The successful treatment of the current case highlights the importance of analyzing difficult ophthalmic cases by combining multidisciplinary therapy diagnosis, different treatment options, and the relative benefits for the patient. These considerations will allow us to generate a feasible treatment plan that is safe and effective.
| 1. | Pichi F, Nucci P, Srivastava SK. Choroidal Macrovessel. Ophthalmology. 2016;123:531. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 2. | Yan L, He G, Zhou X, Zheng Y, Zhu Y, Yang J, Zhang M, Zhou Y. Contrast-enhanced ultrasound in the diagnosis of orbital space-occupying lesions. Clin Radiol. 2017;72:798.e1-798.e6. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 3. | Hallinan JT, Pillay P, Koh LH, Goh KY, Yu WY. Eye Globe Abnormalities on MR and CT in Adults: An Anatomical Approach. Korean J Radiol. 2016;17:664-673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 4. | Beckmann S, Simanowski JH. Update in Contrast-Enhanced Ultrasound. Visc Med. 2020;36:476-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Wagner S, Sommer R, Hinsberger S, Lu C, Hartmann RW, Empting M, Titz A. Novel Strategies for the Treatment of Pseudomonas aeruginosa Infections. J Med Chem. 2016;59:5929-5969. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 202] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 6. | Azam MW, Khan AU. Updates on the pathogenicity status of Pseudomonas aeruginosa. Drug Discov Today. 2019;24:350-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 248] [Article Influence: 35.4] [Reference Citation Analysis (0)] |
| 7. | Cennamo G, Montorio D, Carosielli M, Romano MR, Cennamo G. Multimodal imaging in choroidal metastasis. Ophthalmic Res. 2021;64:411-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Bianchi JI, Nirwan RS, Fulda Graue E, Ross-Hirsch A, Lopez-Rubio S, DiLoreto DA Jr, Singh AD. Spontaneous Resolution of a Choroidal Mass: A Case Series. Ocul Oncol Pathol. 2020;6:305-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Ophthalmology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Apiratwarakul K, Sergi C S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Yuan YY