Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9211
Peer-review started: May 14, 2021
First decision: July 6, 2021
Revised: July 17, 2021
Accepted: August 30, 2021
Article in press: August 30, 2021
Published online: October 26, 2021
Processing time: 159 Days and 17.7 Hours
Indwelling inferior vena cava (IVC) filters might cause various complications, including filter penetration, filter fracture, filter migration, and thrombosis of the IVC. Penetration and migration complications are common, while a caudal migrated double-basket filter with associated infected iliac pseudoaneurysm has seldom been reported.
We report a 64-year-old female admitted for sudden onset of severe right abdominal pain after IVC filter placement for 3 mo. The patient had a history of failed endovascular IVC filter retrieval. Computed tomography showed that the retrieval hook of the filter penetrated the right common iliac artery and vein, leading to right iliac artery pseudoaneurysm accompanied by right ureteral obstruction with ipsilateral hydronephrosis, and bilateral iliac veins were occluded. Emergency open repair was performed to remove the IVC filter, the right iliac pseudoaneurysm, and the compromised segments of the iliac veins and IVC with right common iliac artery reconstruction. Staphylococcus aureus was isolated from the tissue culture. The patient was discharged on postoperative day 12 with anticoagulation therapy and antibiotic therapy after discharge. Six-month follow-up computed tomography revealed that the right common iliac artery was patent, and only mild hydronephrosis was detected.
An indwelling IVC filter, even ‘embedded’ within organized thrombus, could still cause life-threatening complications. Open procedures remain the last resort for IVC filters with severe complications.
Core Tip: Few cases are reported about symptomatic penetration caused by double-basket indwelling inferior vena cava (IVC) filter. Herein, we report an unusual case of infected iliac pseudoaneurysm caused by penetration of an indwelling caudal migrated double-basket IVC filter. After open repair and antibiotic therapy, the patient had a good result at 6-mo follow up. This case demonstrated that an indwelling IVC filter in iliocaval confluence, even ‘embedded’ within organized thrombus, could still cause life-threatening complications, and a more aggressive strategy might be necessary for this situation. Open procedures remain the effective treatment for indwelling IVC filters with severe complications.
- Citation: Weng CX, Wang SM, Wang TH, Zhao JC, Yuan D. Successful management of infected right iliac pseudoaneurysm caused by penetration of migrated inferior vena cava filter: A case report. World J Clin Cases 2021; 9(30): 9211-9217
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9211.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9211
Caval interruption via inferior vena cava (IVC) filter for the prevention of fatal pulmonary embolization was acceptable in selected patients with venous thromboembolism concomitant with contraindication to anticoagulation or failed anticoagulation therapy. According to the Society of Interventional Radiology, routine removal of retrievable IVC filter was recommended once the risk of pulmonary embolization was mitigated because indwelling IVC filters might cause various complications, including filter penetration, filter fracture, filter migration, and thrombosis of the IVC. Pene
A 64-year-old female with IVC filter placement 3 mo ago was presented to our institution with severe right abdominal pain for 1 d.
The patient was admitted to a local hospital for deep venous thrombosis of the left lower extremity 3 mo ago. A double-basket retrievable IVC filter (Visee WXF-32, Shandong Visee Medical Devices Company Limited, China) was placed in infrarenal IVC through the right femoral vein, and anticoagulation therapy was applied. Endovascular retrieval of the IVC filter through the femoral vein approach with standard technique failed 10 d later in the local hospital. Imaging follow-up ceased due to the COVID-19 pandemic.
The patient presented to our institution 3 mo later with severe right abdominal pain for 1 d. The patient had no fever or chills. She denied melena, but her urine was reddish.
The patient had history of scoliosis and poorly controlled diabetes mellitus.
The patient was addicted to smoking and alcohol.
After admission, the patient had a heart rate of 97 bpm, a respiratory rate of 23 breaths per minute, and a blood pressure of 126/73 mmHg. Physical examination revealed diffused abdominal tenderness and rebound tenderness. The right lower limb was slightly swollen, and the pulse in the right femoral artery was weak.
Laboratory tests showed no hepatic or kidney dysfunction, with hemoglobin of 101 g/L, leukocyte count of 14.74 × 109/L, and neutrophilic granulocyte percentage of 91.0%. During the surgery, partial pseudoaneurysm was extracted for tissue culture. Staphylococcus aureus was isolated from the tissue culture, which was sensitive to moxifloxacin.
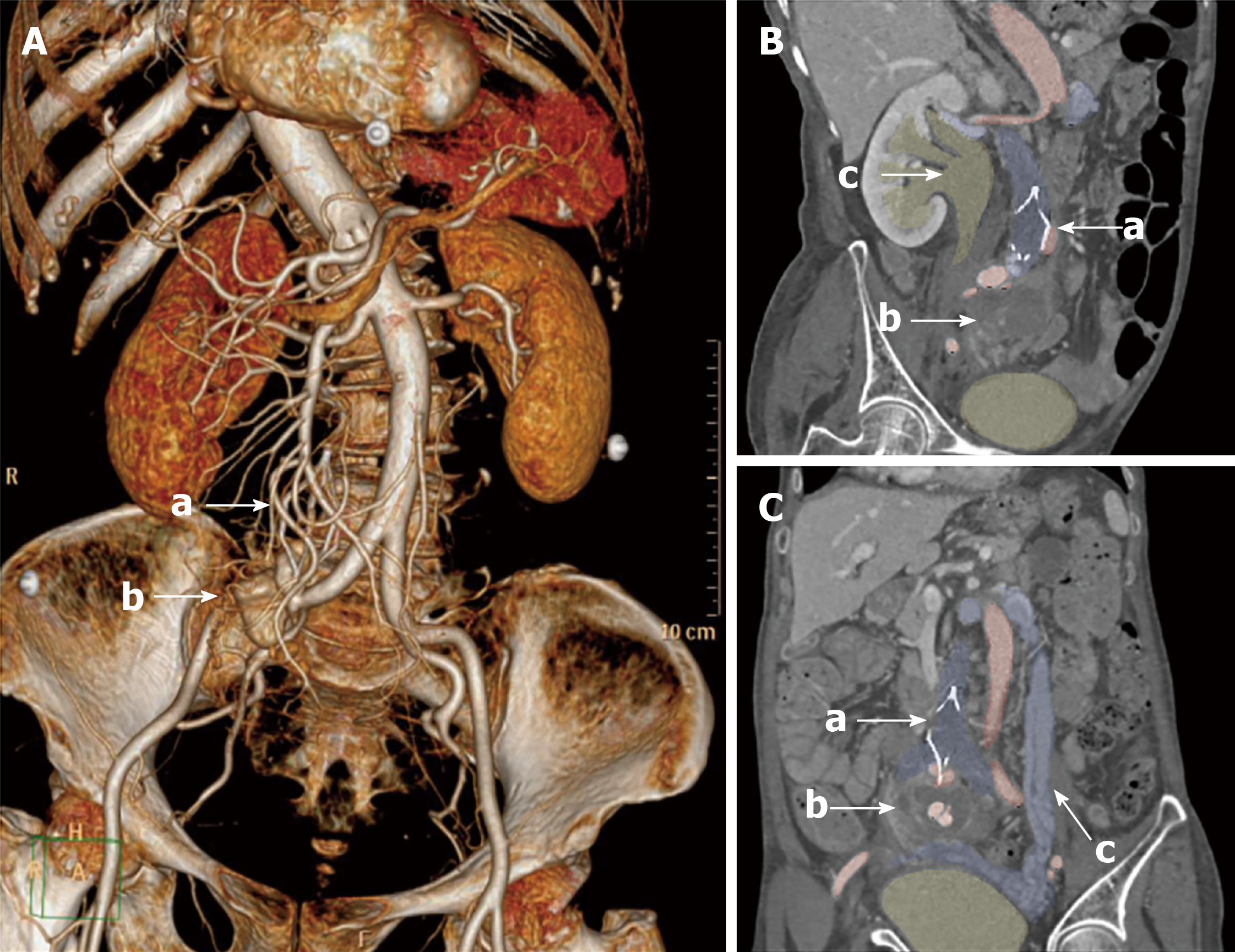
Computed tomography angiography showed that the retrieval hook of the filter penetrated the right common iliac artery (CIA), leading to a 52 mm × 48 mm × 55 mm right iliac artery pseudoaneurysm, accompanied by right ureteral obstruction with ipsilateral hydronephrosis (Figure 1A and B). Bilateral iliac veins and lower part of the IVC were completely occluded, with substantial pelvic varicosities (Figure 1C).
The final diagnosis of the presented case was Staphylococcus aureus infected right iliac pseudoaneurysm and hydronephrosis caused by penetration of the migrated IVC filter.
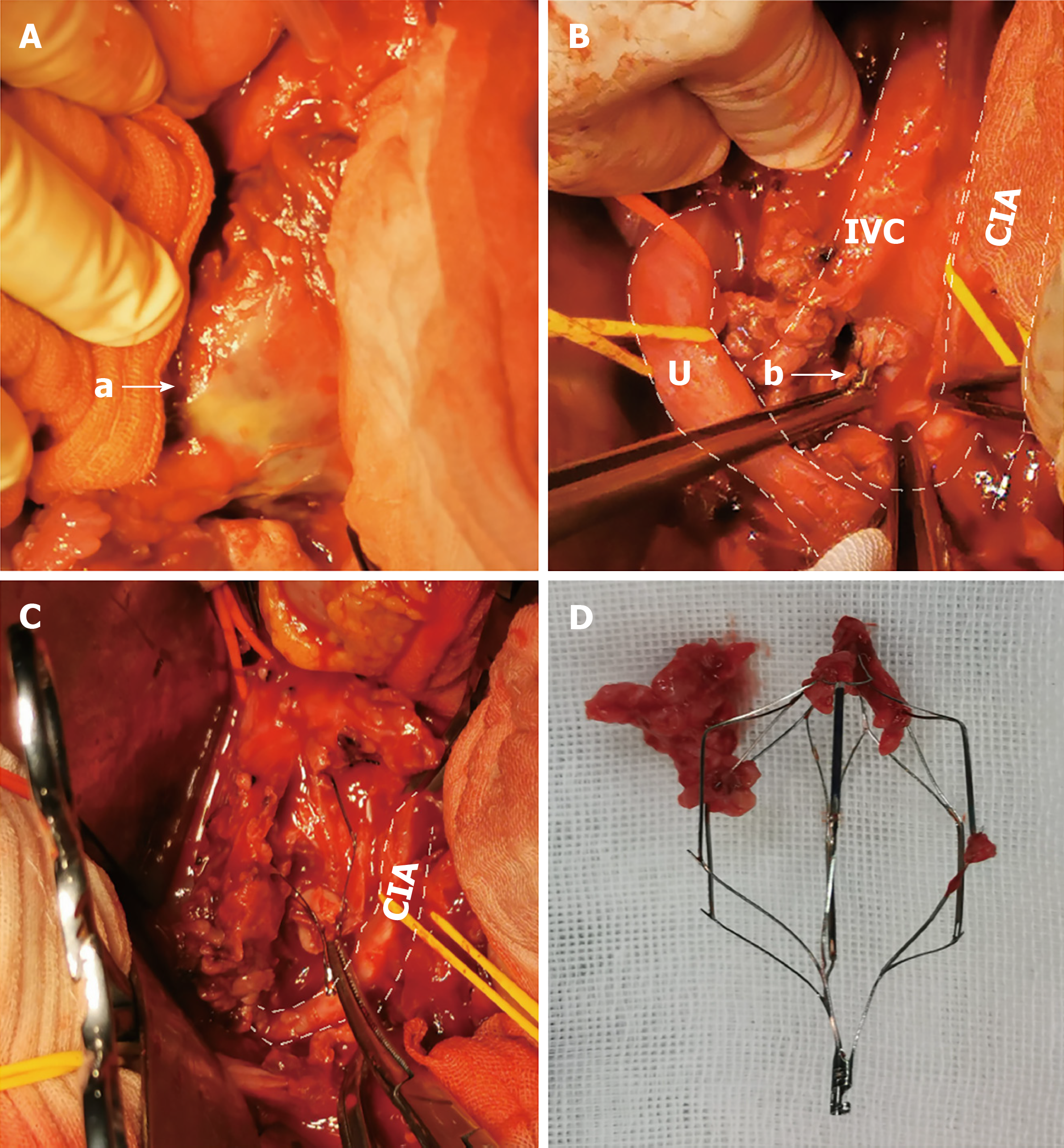
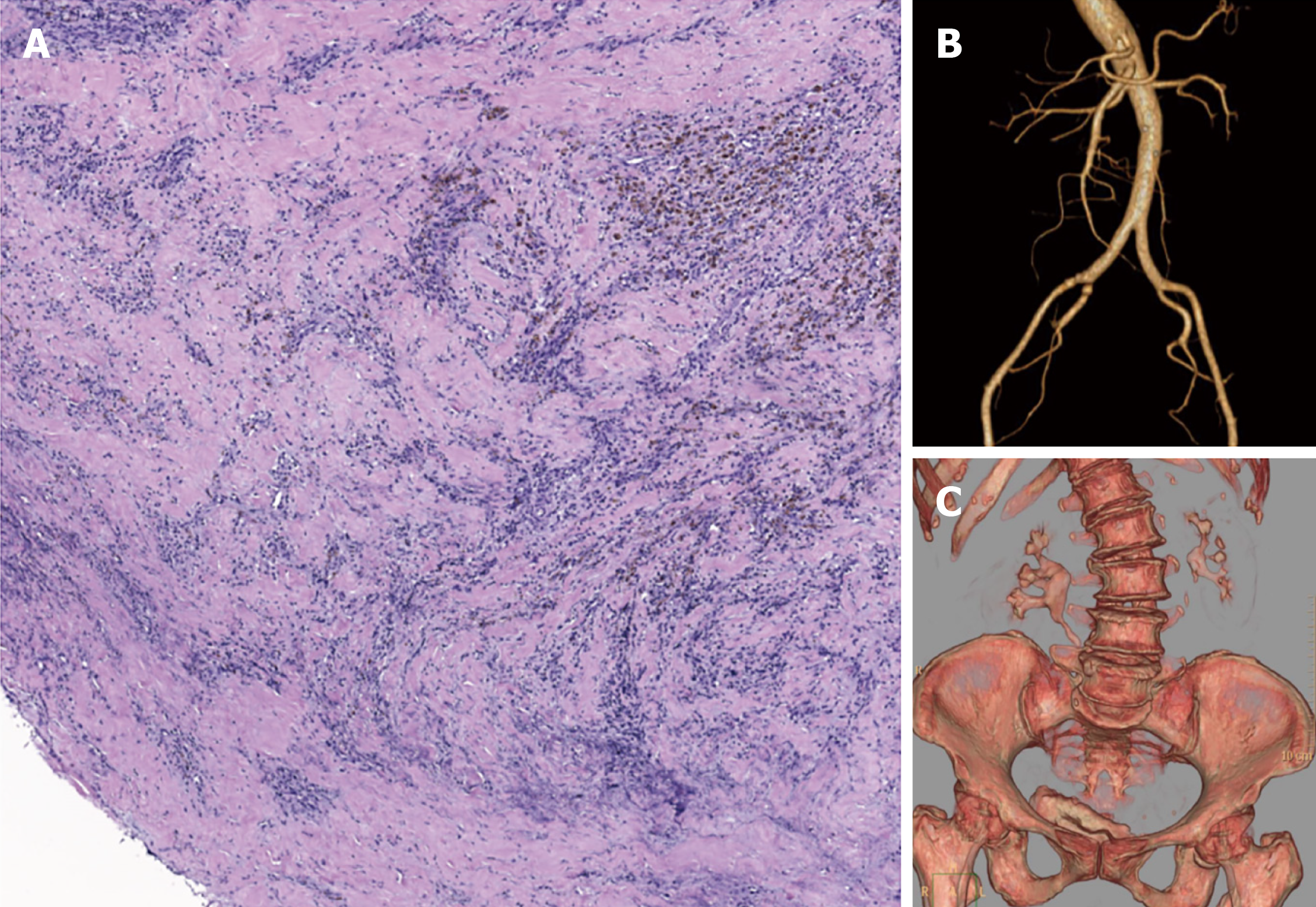
Considering right iliac artery pseudoaneurysm caused by the IVC filter and occlusion of bilateral iliac vein, an emergency open repair was conducted immediately. A midline transperitoneal approach was performed under general anesthesia. A pseudoaneurysm with abscess was found in the pelvic cavity, without intestinal perforation (Figure 2A). The right CIA, internal iliac artery, and external iliac artery were controlled after heparinization. Subsequently, the pseudoaneurysm associated with the surrounding infected tissues were debrided. The crevasse was located at the distal part of the right CIA, and right ureteral obstruction was found (Figure 2B). The IVC and bilateral common iliac veins were completely obstructed by the organized thrombus (Figure 2C). Then, the IVC filter was completely removed (Figure 2D). After that, the right CIA was revascularized through a directed in situ anastomosis, and then right ureterolysis was performed. The right dorsal pedal arterial pulses were palpable without any sign of limb ischemia, and the swollenness of the right lower limbs did not aggravate after surgery. Postoperative pathology indicated a large amount of inflammatory cell infiltration and necrosis in the wall of the pseudoaneurysm and the organized thrombus in the IVC (Figure 3A). Antibiotic therapy with ceftriaxone was initiated before operation considering the signs of peritonitis. Moxifloxacin was used after the results of culture and sensitivity test were available.
The patient recovered uneventfully postoperatively. The bilateral dorsal pedal arterial pulses were palpable, and the swollenness of the right lower limbs was alleviated. The bacterial culture of peritoneal drain was negative on postoperative day 7. Computed tomography urography and single-photon emission computed tomography renal radionuclide imaging revealed that the right urinary tract was incompletely obstructed, while the bilateral renal function was normal. The patient was discharged on postoperative day 12. She received anticoagulation therapy with 20 mg rivaroxaban quaque die and a total of 6 wk antibiotic therapy with 0.4 g moxifloxacin quaque die after discharge.
Six-month follow-up showed the patient recovered well without abdominal pains or claudication, and the edema in the right lower limb improved. Laboratory tests showed no signs of infection with normal levels of procalcitonin. Computed tomography angiography revealed that the right external iliac artery and internal iliac artery were patent, and only mild hydronephrosis was detected (Figures 3B and C).
Current evidence suggested a high prevalence of IVC penetration in the long-term follow-up of IVC filter, reaching approximately 15%-70%[4]. However, IVC penet
To the knowledge of the authors, five cases with caudal migration of the IVC filter have been reported previously[5,6] and only one with double-basket filter, which was thought to be associated with venous thrombectomy using Fogarty embolectomy catheter without fluoroscopy monitoring. A caudal migrated double-basket filter with associated infected iliac pseudoaneurysm has seldom been reported previously. Considering the surgical history of previously failed endovascular retrieval and that no risk factors of filter migration was detected[5,6], the reason for the caudal migration in our case might be iatrogenic, which could result in an abnormal filter position.
Infected pseudoaneurysm was another relatively rare but intractable complication of IVC filter[7]. In our case, Staphylococcus aureus, which is a Gram-positive coccus, was isolated from resected pseudoaneurysm, and massive inflammatory cell infiltration was found in the tissues of the pseudoaneurysm and thrombus in IVC. The findings of tissue culture and pathology examination suggested that the IVC filter might be a potential source of infection. Besides, because the patient had right ureteral obstruction with ipsilateral hydronephrosis caused by pseudoaneurysm, this infection might originate from the urinary tract.
We hypothesize that the caudal migration resulted in abutting of the retrieval hook in the wall of CIV that induced a persistent inflammatory response, and then vascular damage was presented. The filter-associated chronic iliocaval thrombosis somehow ‘fixed’ the IVC filter in the abnormal position with the retrieval hook against the pulsating right iliac artery resulting in the pseudoaneurysm formation. The right iliac pseudoaneurysm, which occurred with the compression of the right urinary tract, caused ipsilateral hydronephrosis. In addition, the concurrent infection made it more intractable.
According to current guidelines, indwelling retrievable IVC filters should be routinely removed in patients with mitigated pulmonary embolization risk[8,9]. However, the general IVC filter retrieval rates remained low. Thus, the decision for filter placement should be cautiously considered.
For filters unable to be retrieved via standard techniques, advanced endovascular techniques were recommended, with high success and low procedure-associated complication rates[9]. In addition, open retrieval was suggested in certain scenarios, including cardiac or pulmonary migration, pseudoaneurysm, and persistent symptoms after failed endovascular retrievals[8,10]. As the migrated IVC filter caused infected pseudoaneurysm with ureteral obstruction and chronic iliocaval thrombosis, an emergency open procedure was appropriate in our case. Debridement of the compromised segment of vessels and hematoma in combination with in situ revascularization was applied to the infected pseudoaneurysm, and the compression symptoms were relieved, which was difficult to achieve via endovascular approaches.
Antibiotic therapy is another important part of infected aneurysm treatment. As for the duration, the optimal length of antibiotic therapy for infected pseudoaneurysm was controversial and should be individualized, but antibiotic therapy for at least 6 wk to 6 mo postoperatively may be considered according to current consensus[11,12]. In our case, the choice of moxifloxacin was based on the results of culture and sensitivity tests of the resected pseudoaneurysm, which was an effective and relatively safe option for the treatment of patients with intra-abdominal infections. The infected tissue was debrided with no prosthetic material used, and the bacterial culture of peritoneal drain turned negative on postoperative day 7 and day 9. After a 6-wk antibiotic therapy, the patient had no fever, and the laboratory tests indicated normal levels of procalcitonin and leukocyte count, thus, the antibiotic therapy ceased.
The current study indicated that asymptomatic patients with failed endovascular IVC filter retrieval do not require open surgical filter removal the majority of the time, even in the presence of significant filter penetration[13], and the filter-associated thrombus was the major cause of filter retrieval failure[14]. But there is no reliable way to evaluate whether a filter in the iliocaval confluence, even within chronic thrombosis, would result in symptomatic filter penetration. Thus, the decision to leave the filter “permanent” should not be applied lightly, as permanent filters are not permanently harmless for patients.
This case demonstrated that an indwelling IVC filter in iliocaval confluence, even ‘embedded’ within organized thrombus, could still cause life-threatening complications, and an improper filter retrieval procedure might be the trigger of all problems. Patients with indwelling IVC filters should undergo regular follow-up, and a more aggressive strategy might be necessary for those patients with filters in an abnormal position to reduce the risk of long-term filter-associated complications. Open procedures remain the effective treatment for indwelling IVC filter with severe complications.
| 1. | Caplin DM, Nikolic B, Kalva SP, Ganguli S, Saad WE, Zuckerman DA; Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for the performance of inferior vena cava filter placement for the prevention of pulmonary embolism. J Vasc Interv Radiol. 2011;22:1499-1506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 62] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Marron RM, Rali P, Hountras P, Bull TM. Inferior Vena Cava Filters: Past, Present, and Future. Chest. 2020;158:2579-2589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 3. | Jia Z, Wu A, Tam M, Spain J, McKinney JM, Wang W. Caval Penetration by Inferior Vena Cava Filters: A Systematic Literature Review of Clinical Significance and Management. Circulation. 2015;132:944-952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 133] [Article Influence: 12.1] [Reference Citation Analysis (0)] |
| 4. | Ayad MT, Gillespie DL. Long-term complications of inferior vena cava filters. J Vasc Surg Venous Lymphat Disord. 2019;7:139-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 5. | Chen L, Zhang J, Yang Z. Inferior Vena Cava Filter Migration to the Left Internal Iliac Vein. Ann Vasc Surg. 2020;65:289.e13-289.e16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Bélénotti P, Sarlon-Bartoli G, Bartoli MA, Benyamine A, Thevenin B, Muller C, Serratrice J, Magnan PE, Weiller PJ. Vena cava filter migration: An unappreciated complication. about four cases and review of the literature. Ann Vasc Surg. 2011;25:1141.e9-1141.e14. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 7. | Assifi MM, Bagameri G, Dimuzio PJ, Eisenberg JA. Management of infected caval filter with simultaneous aortic pseudoaneurysm and retroperitoneal perforation: a case report and literature review. Vascular. 2012;20:225-228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Expert Panel on Interventional Radiology. Minocha J, Smith AM, Kapoor BS, Fidelman N, Cain TR, Caplin DM, Eldrup-Jorgensen J, Farsad K, Gupta A, Lee MH, McBride JJ, Moores LK, Rochon PJ, Lorenz JM. ACR Appropriateness Criteria® Radiologic Management of Venous Thromboembolism-Inferior Vena Cava Filters. J Am Coll Radiol. 2019;16:S214-S226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 9. | Kaufman JA, Barnes GD, Chaer RA, Cuschieri J, Eberhardt RT, Johnson MS, Kuo WT, Murin S, Patel S, Rajasekhar A, Weinberg I, Gillespie DL. Society of Interventional Radiology Clinical Practice Guideline for Inferior Vena Cava Filters in the Treatment of Patients with Venous Thromboembolic Disease: Developed in collaboration with the American College of Cardiology, American College of Chest Physicians, American College of Surgeons Committee on Trauma, American Heart Association, Society for Vascular Surgery, and Society for Vascular Medicine. J Vasc Interv Radiol. 2020;31:1529-1544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 137] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 10. | Charlton-Ouw KM, Afaq S, Leake SS, Sandhu HK, Sola CN, Saqib NU, Azizzadeh A, Safi HJ. Indications and Outcomes of Open Inferior Vena Cava Filter Removal. Ann Vasc Surg. 2018;46:205.e5-205.e11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Chakfé N, Diener H, Lejay A, Assadian O, Berard X, Caillon J, Fourneau I, Glaudemans AWJM, Koncar I, Lindholt J, Melissano G, Saleem BR, Senneville E, Slart RHJA, Szeberin Z, Venermo M, Vermassen F, Wyss TR; Esvs Guidelines Committee; de Borst GJ, Bastos Gonçalves F, Kakkos SK, Kolh P, Tulamo R, Vega de Ceniga M, Document Reviewers, von Allmen RS, van den Berg JC, Debus ES, Koelemay MJW, Linares-Palomino JP, Moneta GL, Ricco JB, Wanhainen A. Editor's Choice - European Society for Vascular Surgery (ESVS) 2020 Clinical Practice Guidelines on the Management of Vascular Graft and Endograft Infections. Eur J Vasc Endovasc Surg. 2020;59:339-384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 461] [Cited by in RCA: 368] [Article Influence: 61.3] [Reference Citation Analysis (0)] |
| 12. | Wilson WR, Bower TC, Creager MA, Amin-Hanjani S, O’Gara PT, Lockhart PB, Darouiche RO, Ramlawi B, Derdeyn CP, Bolger AF, Levison ME, Taubert KA, Baltimore RS, Baddour LM. Vascular Graft Infections, Mycotic Aneurysms, and Endovascular Infections: A Scientific Statement from the American Heart Association. 2016. [RCA] [DOI] [Full Text] [Cited by in Crossref: 200] [Cited by in RCA: 371] [Article Influence: 37.1] [Reference Citation Analysis (0)] |
| 13. | Pratt WB, Sandhu HK, Leake SS, Jamshidy I, Sola CN, Afifi RO, Safi HJ, Charlton-Ouw KM. Asymptomatic patients with unsuccessful percutaneous inferior vena cava filter retrieval rarely develop complications despite strut penetrations through the caval wall. J Vasc Surg Venous Lymphat Disord. 2020;8:54-61. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (1)] |
| 14. | Jia Z, Fuller TA, McKinney JM, Paz-Fumagalli R, Frey GT, Sella DM, Van Ha T, Wang W. Utility of Retrievable Inferior Vena Cava Filters: A Systematic Literature Review and Analysis of the Reasons for Nonretrieval of Filters with Temporary Indications. Cardiovasc Intervent Radiol. 2018;41:675-682. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Ho CM, Marickar F S-Editor: Wang LL L-Editor: Filipodia P-Editor: Yu HG