Published online Oct 26, 2021. doi: 10.12998/wjcc.v9.i30.9023
Peer-review started: March 12, 2021
First decision: July 16, 2021
Revised: July 26, 2021
Accepted: September 16, 2021
Article in press: September 16, 2021
Published online: October 26, 2021
Processing time: 223 Days and 1.8 Hours
Multiple myeloma is an incurable malignant plasma cell disorder that represents the most common primary malignant bone tumor. It commonly involves bone metastasis in multiple vertebral bodies, and the Spinal Instability Neoplastic Score scoring system may not be fully applicable to multiple myeloma (MM) patients.
To evaluate the spinal stability of patients with MM spinal involvement to guide their clinical treatment.
By using the Delphi method, we collected and extracted information through a series of questionnaires and improved it via feedback. We also preliminarily established a spinal stability scoring system for multiple myeloma.
Fifteen clinicians completed a second round of questionnaires and compared their answers with those of the first round of questionnaires to identify significant comments or changes that required group discussions. As a result, no further feedback was used to improve the scoring system. After integrating the information from the expert consultation questionnaire, we established the initial scoring system for MM spine stability and used the scoring system to assess a series of representative clinical cases. The MM spinal stability scoring system was created by calculating the scores of the six separate components: location, pain, number of segments, physiological curvature, comorbidities, and neurological function. The minimum value was “0”, and the maximum value was “24”. A score of “0–10” indicated “spine stability”, a score of “11–17” indicated “potential instability”, and a score of “18–24” indicated “spine instability”. Patients with a score of “11–24” need an intervention such as surgery.
The initial establishment of the MM spine stability scoring system provides a vital theoretical basis for the evaluation of spine stability in individuals with MM.
Core Tip: Multiple myeloma (MM) is an incurable malignant plasma cell disorder that represents the most common primary malignant bone tumor. According to the 2010 Spine Oncology Study Group, spinal instability is defined as the loss of spinal integrity due to tumor growth, which is associated with motor-related pain and symptoms, progressive deformities, and/or impairments in neurological function under physiological loads. Many studies have validated this scoring system and applied it in clinical practice for diseases including primary spinal tumors, metastatic spinal tumors, and MM. However, MM is different from other primary and metastatic malignant tumors of the spine. Osteolytic destruction is the most common type of bone destruction in most MM patients; it commonly involves bone metastasis in multiple vertebral bodies, and is often accompanied by peripheral soft tissue masses and nerve compression symptoms. To some extent, Spinal Instability Neoplastic Score is not applicable to MM patients. Based on the disease characteristics of multiple myeloma, a simple and practical new method for evaluating spinal stability in individuals with multiple myeloma is proposed, and can be used for the clinical evaluation and intervention of multiple myeloma patients.
- Citation: Yao XC, Shi XJ, Xu ZY, Tan J, Wei YZ, Qi L, Zhou ZH, Du XR. Preliminary establishment of a spinal stability scoring system for multiple myeloma. World J Clin Cases 2021; 9(30): 9023-9037
- URL: https://www.wjgnet.com/2307-8960/full/v9/i30/9023.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i30.9023
Multiple myeloma (MM) is an incurable malignant plasma cell disorder that represents the most common primary malignant bone tumor. Older patients, with a median age of 59 years, are more likely to develop MM, but the exact incidence rate of the disease is unknown[1-4]. As the aging process in China accelerates, it is predicted that MM, with a rapid growth in incidence, will become one of the more significant diseases that affect people”s health in the country. In the treatment of MM, spinal stability problems due to the lesion are increasing[5-8]. Currently, there is no method of evaluating the spinal stability of individuals with multiple myeloma. According to the 2010 Spine Oncology Study Group (SOSG), spinal instability is defined as the loss of spinal integrity due to tumor growth, which is associated with motor-related pain and symptoms, progressive deformities, and/or impairments in neurological function under physiological loads[9]. Many studies have validated this scoring system and applied it in clinical practice for diseases including primary spinal tumors, metastatic spinal tumors, and MM. People found that Spinal Instability Neoplastic Score (SINS) demonstrated near-perfect inter- and intraobserver reliability in determining three clinically relevant categories of stability. Therefore, SINS has become the most widely used scoring system for evaluating tumor-related spinal instability in the world.
However, MM is different from other primary and metastatic malignant tumors of the spine. Osteolytic destruction is the most common type of bone destruction in most MM patients; it commonly involves bone metastasis in multiple vertebral bodies, and is often accompanied by peripheral soft tissue masses and nerve compression symptoms. To some extent, SINS is not applicable to MM patients.
Based on the disease characteristics of multiple myeloma, a simple and practical new method for evaluating spinal stability in individuals with multiple myeloma is proposed, and can be used for the clinical evaluation and intervention of multiple myeloma patients.
The current literature on multiple myeloma and spinal stability was systematically reviewed before the study began to determine the best clinical and imaging evidence of spinal stability and to establish a framework for MM spine stability assessments[9-12].
The Delphi method is a method of communication among groups of experts from all over the world that enables a team to systematically deal with complex problems or tasks (how to define spinal instability with MM in the study). By using this method, information was collected and extracted through a series of questionnaires and improved via feedback. This process included the following 5 steps.
The initial group meeting included a seminar hosted by the designated “chairperson” who determined the criteria for evaluating spine stability. From the field of spine surgery and multiple myeloma, a total of 15 orthopedic and hematologists were asked to list factors associated with spinal instability in the context of the tumor. The first round of evaluations was then organized, and different scores were assigned based on the importance of the indicators to form a framework for the spinal stability scoring system of multiple myeloma.
The second round of surveys was conducted via questionnaires, and a questionnaire was formulated to determine the relative importance of each factor. A five-item Likert scale was adopted as the evaluation index for the spinal stability scoring system for spinal cord tumors in multiple myeloma patients, and the degree of importance was divided into five grades: “very important”, “important”, “moderate”, “less important”, and “not important”. The indicators were evaluated in combination with the experience of the experts. The five grades of “very important”, “important”, “moderate”, “less important”, and “not important” were assigned point values of “5”, “4”, “3”, “2”, and “1”, respectively, to facilitate statistical processing. The indicators added by experts were recorded in the “supplementary indicators” column, and the evaluations, comments, and suggestions for each indicator were recorded in the “remarks” column.
After the second round of questionnaires, additional feedback from expert members was collected to improve the scoring system until the expert opinions tended to be consistent.
A multiple myeloma spine stability scoring system was established.
A surgeon applied the multiple myeloma spine stability scoring system to a series of representative cases to assess the feasibility and trialability of the new system.
A total of 72 cases were reviewed and scored using the SINS and MM spinal stability scoring system by the authors. Cases with insufficient history or inadequate imaging were excluded. Images provided included select slices from either computed tomography (CT) scans or magnetic resonance imaging (MRI) combined with X-rays.
Patients’ clinical data were analyzed by the chi-square test. All data were analyzed by SPSS 23.0 statistical software. The measurement data are expressed as the mean ± SD, and P < 0.05 was considered as significantly different.
Subsequently, fifteen clinicians completed a second round of questionnaires (Table 1) and compared their answers with those of the first round of questionnaires to identify significant comments or changes that required group discussions. As a result, no further feedback was used to improve the scoring system. Expert opinions tended to be consistent (Table 2). After integrating the information from the expert consultation questionnaire, we established the initial scoring system for MM spine stability and used the scoring system to assess a series of representative clinical cases. The scoring system consisted of the following six components.
| Content | n (%) | |
| Gender | ||
| Males | 11 (73) | |
| Females | 4 (27) | |
| Age (yr) | ||
| 31-40 | 6 (40) | |
| 41-50 | 3 (20) | |
| ≥ 50 | 6 (40) | |
| Engaged in medical care time (yr) | ||
| ≤ 10 | 3 (20) | |
| 11-20 | 5 (33) | |
| > 20 | 7 (47) | |
| Educational background | ||
| Bachelor‘s degree | 4 (27) | |
| Master’s degree | 4 (27) | |
| doctorate | 7 (46) | |
| Professional titles | ||
| Attending | 5 (33) | |
| Associate chief of doctor | 4 (27) | |
| Chief of doctor | 6 (40) | |
| First-level indices | Second-level indices | mean ± SD | CV% |
| Location | Junctional | 4.87 ± 0.34 | 0.07 |
| Mobile | 4.47 ± 0.50 | 0.11 | |
| Semirigid | 3.53 ± 0.62 | 0.17 | |
| Rigid | 3.07 ± 0.44 | 0.14 | |
| Lesion-free | 2.47 ± 0.81 | 0.33 | |
| Level of pain | Recalcitrant pain in the corresponding zone (not relieved after chemotherapy) VAS > 7 | 4.80 ± 0.40 | 0.08 |
| Moderate pain in the corresponding zone (not relieved after chemotherapy) VAS 4-7 | 4.47 ± 0.49 | 0.11 | |
| Mild pain in the corresponding zone (VAS = 3 after chemotherapy) | 3.67 ± 0.48 | 0.13 | |
| Mild pain during activity (VAS ≤ 2 after chemotherapy) no rest pain | 3.20 ± 0.40 | 0.12 | |
| No pain during activity after chemotherapy | 2.67 ± 0.94 | 0.35 | |
| Number of segments | > 3 | 4.93 ± 0.25 | 0.05 |
| 3 | 4.87 ± 0.56 | 0.11 | |
| 2 | 4.67 ± 0.79 | 0.17 | |
| 1 | 3.80 ± 0.99 | 0.26 | |
| No change in morphology | 2.73 ± 0.10 | 0.36 | |
| physiological curvature | |||
| Lateral radiograph | Physiological curvature of the lesion is abnormal | 4.67 ± 0.47 | 0.10 |
| Physiological curvature of the lesion is normal | 3.00 ± 0.52 | 0.17 | |
| Front radiograph | Scoliosis/rotation | 4.80 ± 0.40 | 0.08 |
| No scoliosis/rotation | 3.00 ± 0.52 | 0.17 | |
| Comorbidities | Spondylolisthesis ( 1 degree) | 4.87 ± 0.34 | 0.07 |
| Shift/dislocation (0-1degree) | 4.53 ± 0.62 | 0.14 | |
| Herniated disk | 3.93 ± 0.44 | 0.11 | |
| Bone spurs | 3.13 ± 0.50 | 0.16 | |
| Bony fusion | 2.80 ± 0.54 | 0.19 | |
| Neurological function | Frankel A | 5.00 ± 0.00 | 0.00 |
| Frankel B | 4.87 ± 0.34 | 0.07 | |
| Frankel C | 4.73 ± 0.44 | 0.09 | |
| Frankel D | 4.07 ± 0.25 | 0.06 | |
| Frankel E | 2.87 ± 0.34 | 0.12 |
Location: This section refers to the SINS evaluation method. Different parts of the spine have different effects on stability after lesions (mainly vertebral compression fractures). Multiple myeloma is a diffuse lesion in which vertebral bodies and appendages can all be involved and the three-column structure of the spine is affected. This behavior is different from the behavior of metastatic and primary tumors of the spine; therefore, it is chosen as the first-grade index. Junctional involvement, such as occipitocervical (C1-C2), cervicothoracic (C7-T2), thoracolumbar (T11-L1), and lumbosacral (L5-S1) involvement, scored a “4”. Mobile spines, such as those with cervical vertebrae (C3–7) and lumbar vertebrae (L2–4) involvement, scored a “3”. Semirigid spines (T3-T10) scored a “2”. Rigid spines (S2-S5) scored a “1”. Cases without spinal involvement scored a “0” (Table 3).
| Location | Score |
| Junctional | 4 |
| Occipitocervical region (C1-C2) | |
| Cervicothoracic region (C7-T2) | |
| Thoracolumbar region (T11-L1) | |
| Lumbosacral region (L5-S1) | |
| Mobile | 3 |
| Cervical vertebra (C3-C7) | |
| Lumbar vertebra (L2-L4) | |
| Semirigid (T3-T10) | 2 |
| Rigid (S2-S5) | 1 |
| Lesion-free | 0 |
Pain: Back pain is the most common symptom of multiple myeloma. The causes of pain include tumor pain and mechanical pain caused by spinal stability changes. The pain caused by tumors can be quickly relieved after chemotherapy, while mechanical pain is difficult to relieve. Thus, we regarded pain as a primary index and further classified it with a specific score. Intractable pain [not alleviated by bed rest/chemoth
| Pain | Score |
| Intractable pain (not alleviated by bed rest/chemotherapy, VAS > 7) | 4 |
| Moderate pain (not alleviated by bed rest/chemotherapy, VAS 4-7) | 3 |
| Mild pain (After bed rest/chemotherapy, VAS = 3) | 2 |
| Slight pain after activity (VAS ≤ 2) no pain when resting | 1 |
| No pain during physical activity after chemotherapy | 0 |
The lesion sites and the number of involved segments are important factors affecting the instability of the spine. Pathological compression fractures of two or more spinal segments often occur in patients with multiple myeloma. This behavior is significantly different from the behavior of spinal metastases or primary tumors. We further divided the index and assigned scores to the different types of fractures: compression fractures involving more than three segments scored a “4”; those involving three segments scored a “3”; those involving two segments scored a “2”; those involving a single segment scored a “1”; and an uncompressed fracture morphology/vertebral morphology that presented no change scored a “0” (Table 5). Lateral radiography of the spine or MRI is the best way to observe the characteristics of this pathological issue.
| Number of segments | Score |
| > 3 | 4 |
| 3 | 3 |
| 2 | 2 |
| 1 | 1 |
| No change in morphology | 0 |
Changes in the physiological curvature of the spine in the sagittal or coronal plane due to compression fractures of the spine are an important basis for spinal stability, which can be assessed by imaging. Although lateral radiographs of overextension and flexion of the spine are often used in the diagnosis of degenerative spinal instability, overextension and flexion of the spine may induce or cause compression fractures or aggravate the original fracture in patients with multiple myeloma, which is not recommended. Although the stability of the spine can also be evaluated by comparing images taken in the supine or erect positions, the supine position is safer for patients with multiple myeloma who are suspected of having spinal instability. In view of this clinical condition, the indicator was further divided: 1. according to the lateral X-ray, abnormal physical curvature of the lesion site scored a “2” and normal physical curvature of the lesion site scored a “0” and 2. According to the anteroposterior X-ray, spines with scoliosis/rotation scored a “2” and those without scoliosis/rotation scored a “0” (Table 6). The lateral radiograph of the spine is simple and practical and can be compared and followed up at different times. It should be the first choice for evaluation.
| Physiological curvature | Score |
| Lateral radiograph | |
| Physiological curvature of the lesion is abnormal | 2 |
| Physiological curvature of the lesion is normal | 0 |
| Front radiograph | |
| Scoliosis/rotation | 2 |
| No scoliosis/rotation | 0 |
MM tends to occur more frequently in elderly people than primary spine tumors. These patients may have degenerative changes, such as disc herniation, epiphysis, spondylolisthesis, and bony fusion, which may increase the instability of the spine before they are diagnosed with MM. According to the characteristics of the spine, we divided this index into four scores: spines with slippage (> 1 degree) scored a “4”; those with displacement/dislocation (0–1 degrees) scored a “3”; those with disc herniation scored a “2”; those with a traction spur scored a “1”; and those with bone fusion and normal spines scored a “0” (Table 7).
| Comorbidities | Score |
| Spondylolisthesis (> 1 degree) | 4 |
| Shift/dislocation (0-1 degree) | 3 |
| Herniated disk | 2 |
| Bone spurs | 1 |
| Bony fusion | 0 |
Spinal instability can lead to changes in neurological function, and it is often found in individuals with both multiple myeloma and intraspinal tumor infiltration, which causes compression of the spinal cord and nerve roots, resulting in severe complications such as paraplegia and incontinence. For the purpose of identification, this scoring system first excludes MM patients with tumor lesions in the spinal canal. The Frankel scoring system is commonly used in clinical practice and is easy to understand. This indicator was based on Frankel”s assessment of neurological function: Frankel A (complete loss of sensory and motor function below the injury plane) scored a “4”; Frankel B (no motor function with some sensory function below the injury plane)) scored a “3”; Frankel C (some useless motor function below the injury plane) scored a “2”; Frankel D (useful motor function below the injury plane, but not fully normal) scored a “1”; and Frankel E (normal sensorimotor and sphincter function) scored a “0” (Table 8).
| Neurological function (according to the Frankel classification) | Score |
| Frankel A | 4 |
| Frankel B | 3 |
| Frankel C | 2 |
| Frankel D | 1 |
| Frankel E | 0 |
The MM spinal stability scoring system was created by calculating the scores of the six separate components. The minimum value was “0”, and the maximum value was “24”. A score of “0–10” indicated “spine stability”, a score of “11–17” indicated “potential instability”, and a score of “18–24” indicated “spine instability”. Patients with a score of “11–24” need an intervention such as surgery.
The following three cases illustrate the clinical application of the MM spinal stability score.
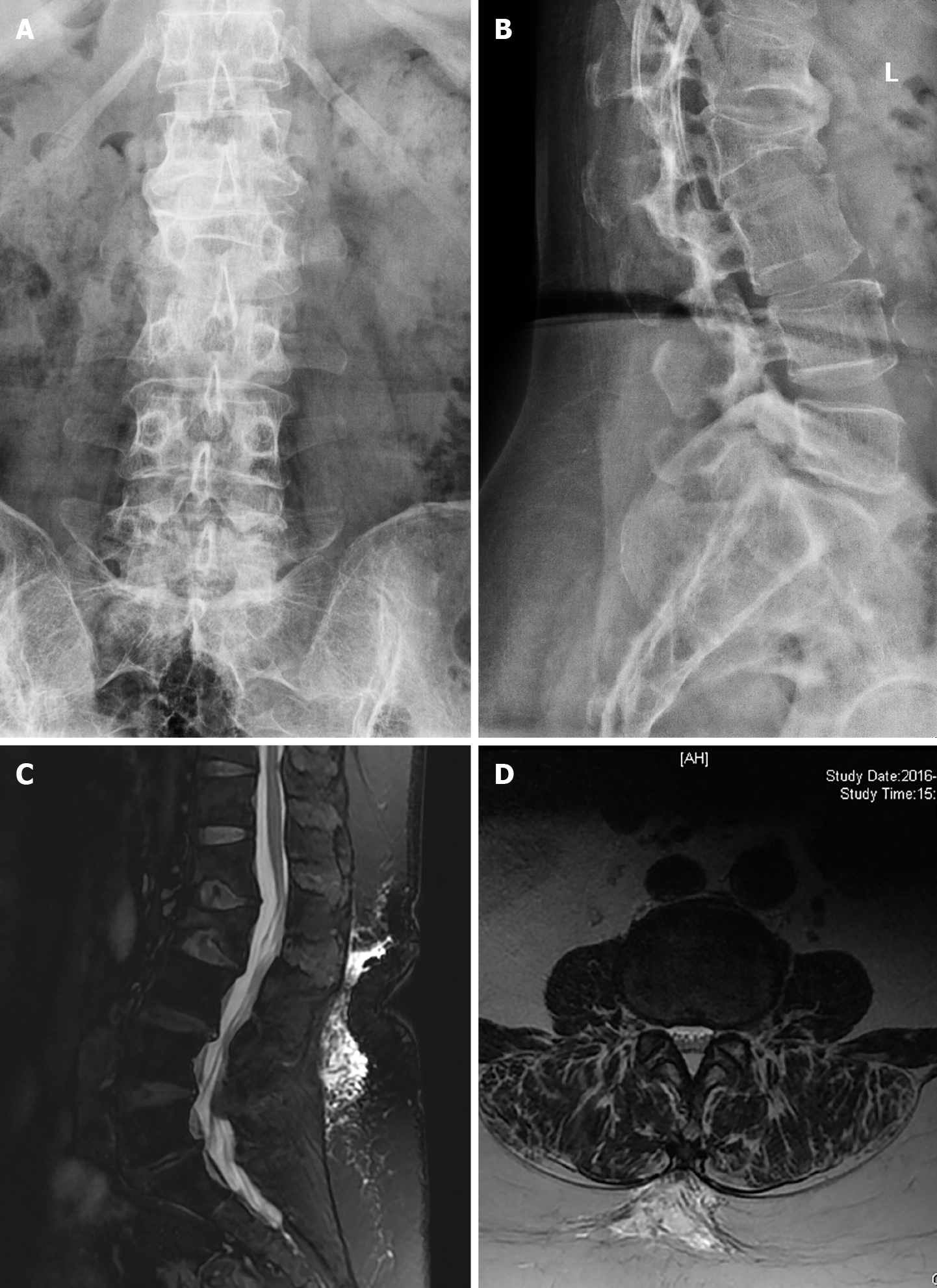
Case 1: A 52-year-old male with MM had a vertebral compression fracture at T11 and L1–2 and the following scores: VAS = 3; number of segments = 3; physiological curvature: positive and lateral according to X-ray and MRI; complications: none; and Frankel score of neurological function: D. The MM spine stability score of this patient was as follows: 3 points for location + 2 points for pain + 3 points for the segments + 0 points for the physiological curvature + 0 points for complications + 1 point for neurological function = 9 points. The score indicated “spinal stability” (Figure 1).
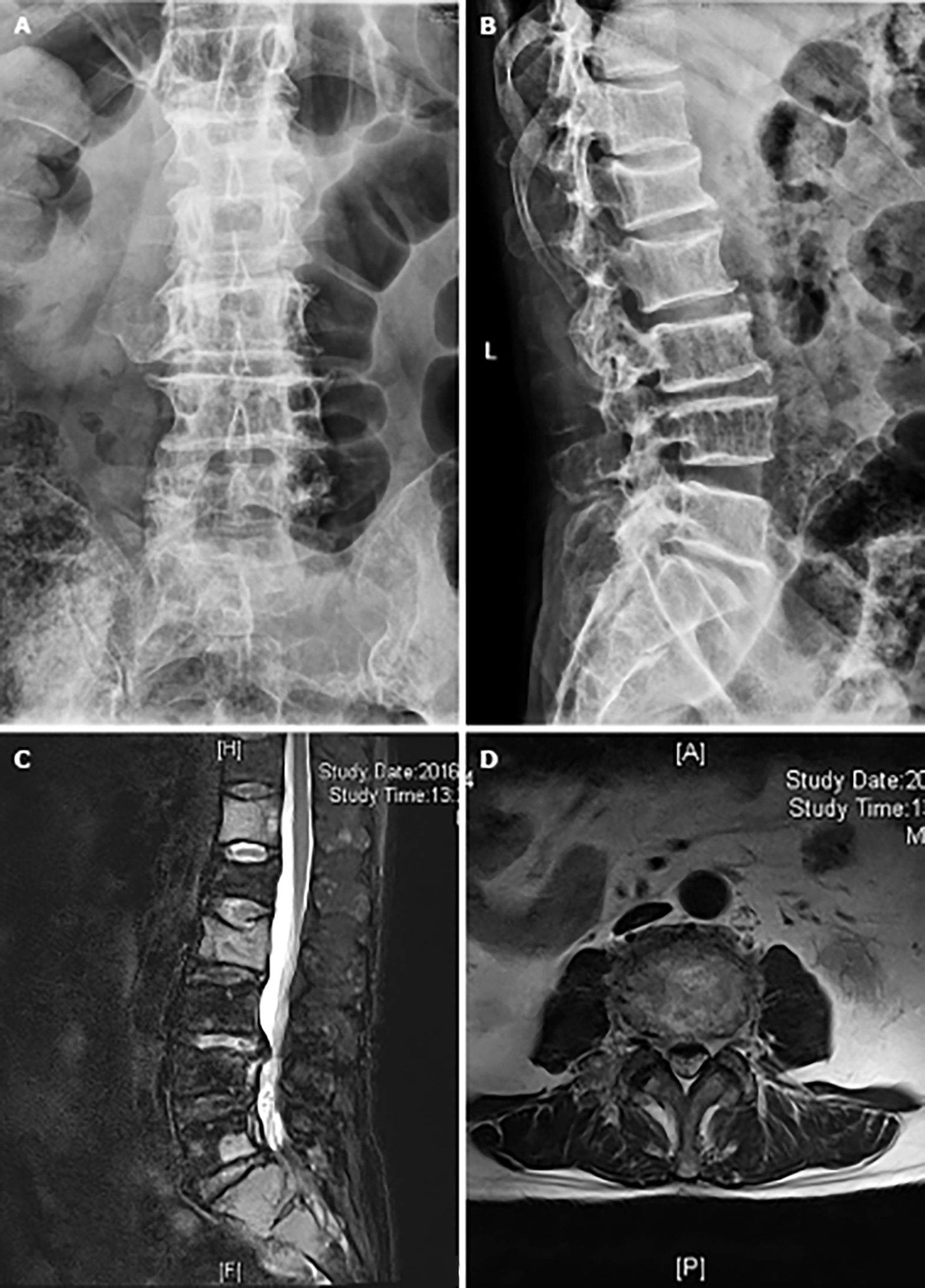
Case 2: A 58-year-old male with MM had lumbar disc herniation. The spinal stability score was as follows: 4 points for location + 3 points for pain + 4 points for the segments + 0 points for the physiological curvature + 2 points for complications + 0 points for neurological function = 13 points. The score indicated “potential instability” (Figure 2).
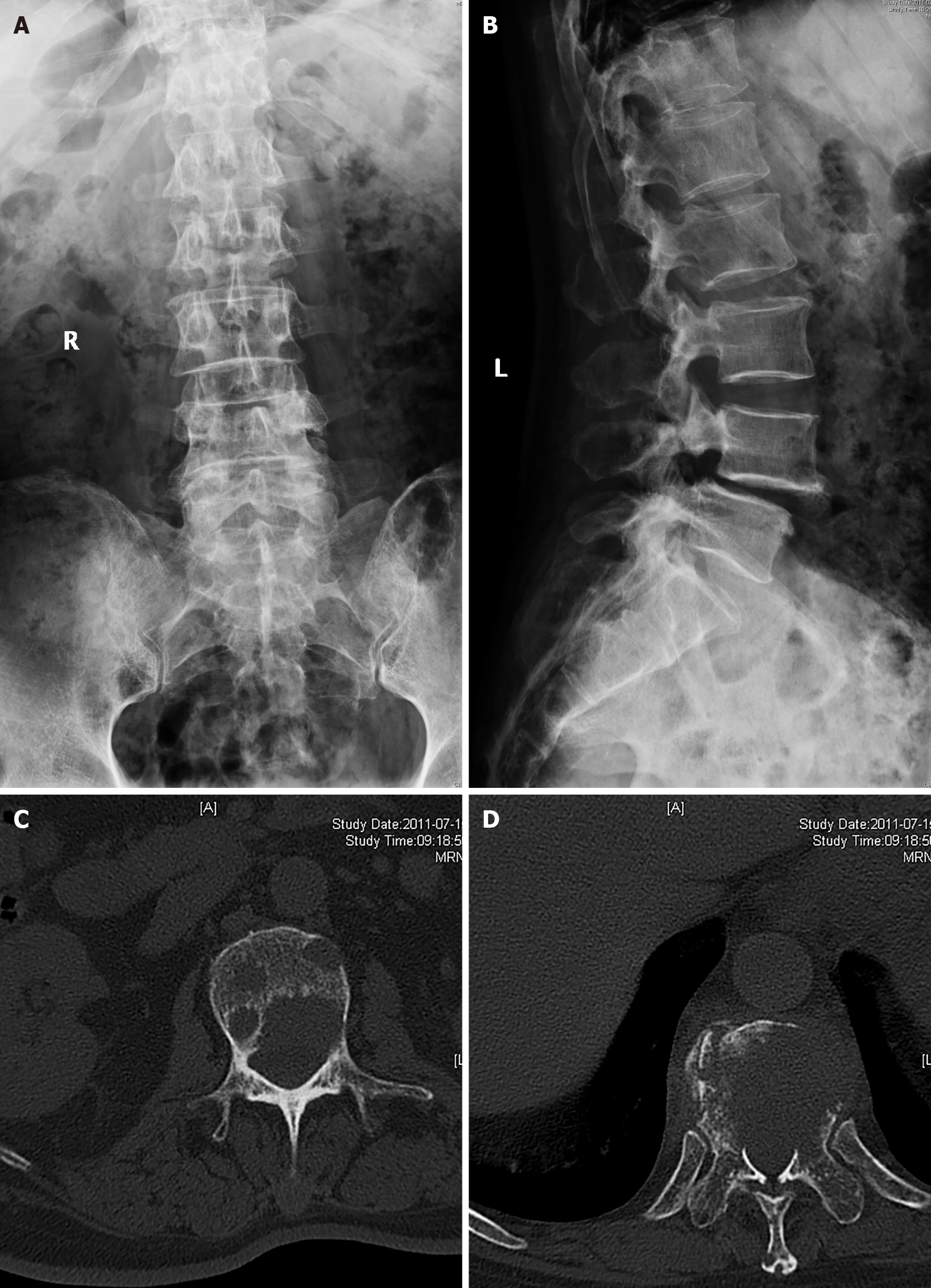
Case 3: A 58-year-old male with MM had spondylolisthesis and lumbar spondylolysis (2 degrees). The spinal stability score was as follows: 4 points for location + 4 points for pain + 2 points for the segments + 2 points for the physiological curvature + 4 points for complications + 2 points for neurological function = 18 points. The score indicated “spinal instability” (Figure 3).
A comparison of the MM scoring system results with those of the SINS scoring system showed that the results of the MM scoring system were inconsistent with those of the SINS (McNemar-Bowker 38.105; P = 0.000) (Table 9). The main difference was in the evaluation of potential instability of the spine.
| SINS | McNemar-Bowker | P value | |||||
| MM | Stable | Potentially unstable | Unstable | Total | 38.105 | 0.000 | |
| Stable | 5 | 37 | 3 | 45 | |||
| Potentially unstable | 1 | 21 | 3 | 25 | |||
| Unstable | 0 | 1 | 1 | 2 | |||
| Total | 6 | 59 | 7 | 72 | |||
MM is characterized by the accumulation of clonal plasma cells in bone marrow (BM), the secretion of monoclonal immunoglobulins, and the presence of osteolytic bone lesions, which involve multifactorial problems. How to protect the spine and improve the quality of life of patients with routine chemotherapy in the hematology department is an important issue. It is necessary to evaluate the stability of the spine to develop interventions and determine prescriptions. At present, methods for evaluating the stability of the spine in individuals with primary tumors and metastatic cancer already exist, but no methods have been reported for the evaluation of spinal stability in individuals with multiple myeloma. Based on the clinical features of multiple myeloma, this study established a method for assessing the stability of an MM spine. It should be emphasized that the evaluation of spinal stability is one of the assessments in the course of diagnosis and treatment of MM patients. It may be the most difficult assessment for physicians who are not spinal surgeons. Therefore, constructing a simple and easy-to-learn scoring system is our main research goal.
The spine requires stability to ensure its degree of movement without pain and to prevent neurological dysfunction and abnormal angulation[13]. Spinal stability depends on the integrity of the static structure and function of its components (bones, ligaments, intervertebral discs, facet joints, etc.), the dynamic structures of the muscles, the structure of the nervous system, and the functional integrity. Spinal instability caused by tumors is mainly due to the destruction of the bone structure, and other structures are for the most part normal; this condition is quite distinct from those of spinal degenerative instability (with mainly affects ligaments and intervertebral discs and causes changes in facet joints) and traumatic spinal instability (which leads to bone, ligament, and muscle damage or fractures). Similarly, it is not the same as spinal instability caused by neuromuscular disease. Since multiple myeloma is predominantly characterized by osteolytic lesions, osteogenesis and mixed bone changes do not occur. Therefore, it is not appropriate to evaluate the stability of the spine in individuals with multiple myeloma by using methods for assessing the spinal stability of individuals with primary tumors and spinal metastases.
SOSG defines spinal instability as a loss of functional integrity of the spine. Potential instability of the spine is an intermediate state between stability and instability, which is also a significant factor affecting the clinical decision-making process of treatment for individuals with a spinal disease and tumors. There is no consensus on the definition of potential instability[9], but the importance of the underlying spinal instability with multiple myeloma is noticeable. Surgical intervention can be performed for spinal nerve compression caused by multiple myeloma spinal lesions[5-8,14-16]. For MM patients without neurological deficits, it is of great clinical significance to evaluate the stability of the spine, detect spinal instability, determine whether it is accompanied by spinal cord and neurological dysfunction, and prevent spinal instability caused by pathological fractures and the deterioration of neurological symptoms.
The purpose of the MM spine stability assessment is to guide clinical decision-making and it should be characterized by effectiveness, repeatability, reliability, and maneuverability. Most importantly, it should promote multidisciplinary cooperation and communication between spine surgeons and hematologists. Currently, the SINS score is an internationally accepted method for assessing tumor-related spinal stability. The scoring system was established on the basis of six aspects, including tumor location, degree of pain, type of bone destruction, imaging changes in the spinal line, degree of vertebral collapse, and posterior lateral involvement as determined by the SOSG in 2010. Bilsky et al[17] analyzed the reliability and effectiveness of the SINS scoring system, which is considered to have good prediction accuracy. The specificity and sensitivity of the SINS scoring system in predicting spinal instability were 79.5% and 95.7%, respectively. Fisher et al[18] have shown that the SINS scoring system is highly reliable; of 629 patients with spinal instability or potential instability, 621 had SINS scores > 7, and most of them were potentially unstable. Campos et al[19] also obtained similar results for the study of the repeatability and reliability of the SINS scoring system.
Despite the recognition of the specificity and sensitivity of the SINS scoring system, there is still a lack of relevant large-scale prospective studies. Moreover, the scoring system only evaluates the stability of local lesions without considering the general status of the patient. In previous literature, some scholars used the SINS scoring system to evaluate the spinal stability of patients with multiple myeloma, but the sensitivity of multiple myeloma to chemotherapy and radiotherapy and its clinical features were not considered[20-22]. Therefore, the SINS scoring system still has some limitations when used in the MM population. Our group reviewed the clinical data of 72 patients with MM spinal involvement and evaluated them with the SINS scoring system and MM spinal stability scoring system, and found that the two scoring systems differed greatly in assessing “potential instability”. Subsequently, for a number of patients, the SINS scoring system showed “stability”, while the MM scoring results showed “stability” and “potential instability”. MM tends to occur in the elderly population, and some patients have spinal degeneration, ankylosing spondylitis, and other diseases. In contrast to other primary/secondary malignant tumors of the spine, the number of tumor infiltrating segments by MM was large, and almost all cases involved osteolytic destruction. MM directly destroys the bone, causing the rigidity of the spine to decrease. In addition, multiple segments are involved in the course of MM, so MM is more likely to cause spinal instability or increase tumor-related instability on the basis of the original degenerative instability of the spine. These factors are closely related to the evaluation of MM spine stability; however, the SINS scoring system does not take these factors into consideration. Therefore, the actual stability and potential risk of instability of patients with MM spinal involvement are higher than the results obtained by the SINS scoring system.
The lesion location of the tumor affects the stability of the spine. The risk of instability is the largest in the transitional sites of the spine, with the highest score weighting in these areas; the next largest risk of instability is in the active areas, while the weightings of the semiactive region composed of T3-T10 and the fixed region composed of S2-S5 were low[23,24].
Although pain is not the only symptom of spinal instability that is caused by tumors, it plays an important role in assessing the instability of the spine. Pain caused by spinal instability can be aggravated by exercise and relieved by bed rest, which is related to the destruction of the spinal structure. As the disease progresses, most patients with MM may feel pain in the chest and lower back, which is caused by local tumor infiltration and spinal instability. Pain associated with tumor invasion can be effectively controlled by chemotherapy, while pain caused by instability cannot be relieved after chemotherapy. Therefore, we rated the pain according to the location and severity of the pain. We evaluated postchemotherapy pain caused by spinal instability, which was different from the pain assessed in the SINS scoring system.
Many studies have indicated that skeletal system-related destruction includes osteolytic lesions and bone pain in patients with MM. Moreover, osteolytic lesions are important factors causing structural instability, and the risk of vertebral collapse caused by osteolytic lesions is higher than that caused by osteoblastic lesions[25].
Unlike spinal metastatic and primary tumors, which may occur with osteogenesis or osteolytic lesions, this indicator showed no significant differences in the MM spinal stability assessment, which is different from the results of the SINS scoring system.
In general, changes in physiological curvature or abnormalities often lead to instability of the spine[26]. Malformations may occur gradually, and may be the cumulative effect of multiple lesions. Since vertebral compression fractures caused by multiple myeloma are mostly accompanied by multiple fractures, kyphosis, and spinal degeneration due to advanced age, the scoring system includes the patient”s spinal curvature as an indicator. In addition, degenerative changes in the spine (spondylolisthesis/displacement greater than 1 degree, disc herniation less than 1 degree, bone spurs, bony fusion, or no lesion) were also assessed separately as first-level indicators; this method of assessment was different from that of the SINS scoring system.
More than one segment of the spine was involved in MM. Moreover, a greater number of segments involved in the vertebral compression fracture corresponded to a greater probability of spinal instability, so we considered the number of affected segments as a primary indicator. It should be noted that spinal compression fractures may not be continuous in many situations, and the doctor may evaluate the stability of the corresponding site based on the fracture, which was not mentioned in the previous SINS scoring system.
Sudden neurological dysfunction may occur in patients with MM during treatment, including compression of the spinal cord caused by direct tumor infiltration of the spinal canal and neurological changes due to vertebral instability, which can be distinguished by imaging examinations. In contrast to the SINS scoring system, this scoring system excluded neurological dysfunction caused by intraspinal lesions and assessed neurological changes due to spinal instability based on the Frankel score.
This scoring system was based on the above indicators and was used to guide the clinical treatment of individuals with MM. The most important clinical contributions of the system are its ability to evaluate patients with MM, provide specific interventions according to the scores, and minimize the serious consequences of spinal instability in order to improve the patients’ quality of life. Notably, the spine stability score is a part of the assessment of the stability of a patient’s spine. BMI, daily activity, bone quality, and history of previous spinal surgery may also affect the stability of the spine. Special considerations are needed in an overall evaluation of a patient. In guiding treatment, the timing of interventions may change as the disease becomes less invasive. Stability is a part of the assessment when making a surgical treatment decision. The general health, prognosis, neurological function, and decisions of patients must also be taken into consideration.
Multiple myeloma with special characteristics is different from primary bone tumors and bone metastases. The initial establishment of the MM spine stability scoring system provides a vital theoretical basis for the evaluation of spine stability in individuals with MM. After further verification and reliability testing of the MM scoring system, we believe that the establishment of the MM spinal stability scoring system is reasonable and that the system has value in clinical applications and guiding clinical decisions.
In the evaluation of patients with spinal tumors, spinal stability assessment is very important, and it often guides our decisions in the selection of surgical or conservative treatment. At present, the most commonly used clinical spinal tumor stability evaluation system is the spinal instability neoplastic score (SINS) system.
Although multiple myeloma (MM) can also be evaluated by the SINS scoring system, we found that patients with MM have their own characteristics; almost all of them have osteolytic destruction, and most cases involve multiple segments of the spine. To evaluate the spinal stability of patients with MM more accurately in the clinic, we referred to the SINS scoring system to establish a scoring system that could evaluate the spinal stability of MM.
The objective of the study was to evaluate the clinical applicability of the MM stability score by comparing it with the SINS system. The MM spinal stability score system will be used to evaluate clinical MM patients. Through the evaluation of spinal stability, corresponding intervention measures should be given in time to improve the quality of life of the patients and improve their prognosis.
The current literature on multiple myeloma and spinal stability was systematically reviewed before the study began to determine the best clinical and imaging evidence of spinal stability and to establish a framework for MM spine stability assessments. The spine stability scoring system of multiple myeloma was established by the Delphi method. The MM scoring system and SINS scoring system were used to analyze the same group of data, and the consistency of the two scoring systems was tested.
After integrating the information from the expert consultation questionnaire, we established the initial scoring system for MM spine stability and used the scoring system to assess a series of representative clinical cases. The scoring system consisted of the following six components: "Location", "Pain", "Number of segments", "Physiological curvature", "Comorbidities", and "Neurological function". The MM spinal stability scoring system was created by calculating the scores of the six separate components. The minimum value was “0”, and the maximum value was “24”. A score of “0–10” indicated “spine stability”, a score of “11–17” indicated “potential instability”, and a score of “18–24” indicated “spine instability”. Patients with a score of “11–24” need an intervention such as surgery. We selected some typical cases to be evaluated with the MM spinal scoring system and SINS system, and the results were compared. We found that most of the "potentially unstable" patients in the MM score were rated as "stable" in the SINS score.
The authors established the initial scoring system for MM spine stability. The authors believe that the MM spinal stability scoring system is more suitable for MM patients than the SINS scoring system.
In the future, the authors will further optimize the MM spine stability scoring system. The authors prepared clinical trials for prospective studies to analyze the advantages and disadvantages of the MM spinal stability scoring system.
| 1. | Lu J, Lu J, Chen W, Huo Y, Huang X, Hou J; Chinese Medical Doctor Association Hematology Branch. Clinical features and treatment outcome in newly diagnosed Chinese patients with multiple myeloma: results of a multicenter analysis. Blood Cancer J. 2014;4:e239. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 79] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Siegel R, Ward E, Brawley O, Jemal A. Cancer statistics, 2011: the impact of eliminating socioeconomic and racial disparities on premature cancer deaths. CA Cancer J Clin. 2011;61:212-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3032] [Cited by in RCA: 3131] [Article Influence: 208.7] [Reference Citation Analysis (0)] |
| 3. | Ailawadhi S, Aldoss IT, Yang D, Razavi P, Cozen W, Sher T, Chanan-Khan A. Outcome disparities in multiple myeloma: a SEER-based comparative analysis of ethnic subgroups. Br J Haematol. 2012;158:91-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 97] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 4. | Jain RV, Mills PK, Parikh-Patel A. Cancer incidence in the south Asian population of California, 1988-2000. J Carcinog. 2005;4:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Surgeon’s Committee of the Chinese Myeloma Working Group of the International Myeloma Foundation. Consensus on Surgical Management of Myeloma Bone Disease. Orthop Surg. 2016;8:263-269. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Terpos E, Morgan G, Dimopoulos MA, Drake MT, Lentzsch S, Raje N, Sezer O, García-Sanz R, Shimizu K, Turesson I, Reiman T, Jurczyszyn A, Merlini G, Spencer A, Leleu X, Cavo M, Munshi N, Rajkumar SV, Durie BG, Roodman GD. International Myeloma Working Group recommendations for the treatment of multiple myeloma-related bone disease. J Clin Oncol. 2013;31:2347-2357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 247] [Cited by in RCA: 246] [Article Influence: 18.9] [Reference Citation Analysis (0)] |
| 7. | Guzik G. Oncological and functional results of the surgical treatment of vertebral metastases in patients with multiple myeloma". BMC Surg. 2017;17:92. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Zadnik PL, Goodwin CR, Karami KJ, Mehta AI, Amin AG, Groves ML, Wolinsky JP, Witham TF, Bydon A, Gokaslan ZL, Sciubba DM. Outcomes following surgical intervention for impending and gross instability caused by multiple myeloma in the spinal column. J Neurosurg Spine. 2015;22:301-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 9. | Fisher CG, DiPaola CP, Ryken TC, Bilsky MH, Shaffrey CI, Berven SH, Harrop JS, Fehlings MG, Boriani S, Chou D, Schmidt MH, Polly DW, Biagini R, Burch S, Dekutoski MB, Ganju A, Gerszten PC, Gokaslan ZL, Groff MW, Liebsch NJ, Mendel E, Okuno SH, Patel S, Rhines LD, Rose PS, Sciubba DM, Sundaresan N, Tomita K, Varga PP, Vialle LR, Vrionis FD, Yamada Y, Fourney DR. A novel classification system for spinal instability in neoplastic disease: an evidence-based approach and expert consensus from the Spine Oncology Study Group. Spine (Phila Pa 1976). 2010;35:E1221-E1229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1058] [Cited by in RCA: 816] [Article Influence: 51.0] [Reference Citation Analysis (0)] |
| 10. | Muto M, Giurazza F, Guarnieri G, Izzo R, Diano A. Neuroimaging of Spinal Instability. Magn Reson Imaging Clin N Am. 2016;24:485-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Gopinath P. Lumbar segmental instability: Points to ponder. J Orthop. 2015;12:165-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 12. | Xu C, Yin M, Sun Z, Yan Y, Mo W, Yan W. An Independent Interobserver Reliability and Intraobserver Reproducibility Evaluation of Spinal Instability Neoplastic Score and Kostuik Classification Systems for Spinal Tumor. World Neurosurg. 2020;137:e564-e569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | White AA, Southwick WO, Panjabi MM. Clinical instability in the lower cervical spine a review of past and current concepts. Spine. 1976;1:15-27. [DOI] [Full Text] |
| 14. | Denaro V, Denaro L, Albo E, Papapietro N, Piccioli A, Di Martino A. Surgical management of spinal fractures and neurological involvement in patients with myeloma. Injury. 2016;47 Suppl 4:S49-S53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Zeifang F, Zahlten-Hinguranage A, Goldschmidt H, Cremer F, Bernd L, Sabo D. Long-term survival after surgical intervention for bone disease in multiple myeloma. Ann Oncol. 2005;16:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 16. | Dürr HR, Wegener B, Krödel A, Müller PE, Jansson V, Refior HJ. Multiple myeloma: surgery of the spine: retrospective analysis of 27 patients. Spine (Phila Pa 1976). 2002;27:320-4; discussion 325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 41] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Bilsky M, Fischer CG, Gokasalan ZL, Fehlings MG, Boriani S, Polly D, Schmidt MH, Dekutoski M, Yamada Y, Fourney D. The Spinal Instability Neoplastic Score (SINS): An Analysis if Reliability and Validity from the Spine Oncology Study Group. Int J Radiat Oncol Biol Phys. 2010;78:S263-S263. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Fisher CG, Versteeg AL, Schouten R, Boriani S, Varga PP, Rhines LD, Heran MK, Kawahara N, Fourney D, Reynolds JJ, Fehlings MG, Gokaslan ZL. Reliability of the spinal instability neoplastic scale among radiologists: an assessment of instability secondary to spinal metastases. AJR Am J Roentgenol. 2014;203:869-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 19. | Campos M, Urrutia J, Zamora T, Román J, Canessa V, Borghero Y, Palma A, Molina M. The Spine Instability Neoplastic Score: an independent reliability and reproducibility analysis. Spine J. 2014;14:1466-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 20. | Taneichi H, Kaneda K, Takeda N, Abumi K, Satoh S. Risk factors and probability of vertebral body collapse in metastases of the thoracic and lumbar spine. Spine (Phila Pa 1976). 1997;22:239-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 185] [Cited by in RCA: 159] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 21. | Kostuik JP, Errico TJ, Gleason TF, Errico CC. Spinal stabilization of vertebral column tumors. Spine (Phila Pa 1976). 1988;13:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 110] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 22. | Cybulski GR. Methods of surgical stabilization for metastatic disease of the spine. Neurosurgery. 1989;25:240-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Mazel C, Hoffmann E, Antonietti P, Grunenwald D, Henry M, Williams J. Posterior cervicothoracic instrumentation in spine tumors. Spine (Phila Pa 1976). 2004;29:1246-1253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 65] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 24. | An HS, Vaccaro A, Cotler JM, Lin S. Spinal disorders at the cervicothoracic junction. Spine (Phila Pa 1976). 1994;19:2557-2564. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 130] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 25. | Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;256-264. [PubMed] |
| 26. | Tomita K, Kawahara N, Kobayashi T, Yoshida A, Murakami H, Akamaru T. Surgical strategy for spinal metastases. Spine (Phila Pa 1976). 2001;26:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 973] [Cited by in RCA: 978] [Article Influence: 39.1] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work noncommercially, and license their derivative works on different terms, provided the original work is properly cited and the use is noncommercial. See: http://creativecommons.org/Licenses/bync/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report”s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ahmed S S-Editor: Ma YJ L-Editor: A P-Editor: Guo X