Published online Oct 16, 2021. doi: 10.12998/wjcc.v9.i29.8894
Peer-review started: June 8, 2021
First decision: June 25, 2021
Revised: July 7, 2021
Accepted: July 28, 2021
Article in press: July 28, 2021
Published online: October 16, 2021
Processing time: 129 Days and 6.6 Hours
Ovarian pregnancy after assisted reproductive technology treatment has rarely been reported; ovarian pregnancy following intrauterine insemination (IUI) is even rarer, and only nine cases have previously been reported.
We report a case of ovarian pregnancy rupture after ovulation induction and IUI. The patient presented with bilateral lower abdominal pain and was referred to the emergency department. Ultrasound examination revealed ovarian pregnancy and intraperitoneal bleeding. Laparoscopy revealed an ovarian pregnancy with hemo
Close attention should be paid to any history of pelvic inflammatory disease before commencing IUI treatment,and patients with such a history should be closely followed up after IUI. Early measurement of serum β-human chorionic gonadotropin levels and ultrasonic examination are essential for timely diagnosis of ovarian pregnancy after ovulation induction and IUI to avoid more serious complications.
Core Tip: Ovarian pregnancy following intrauterine insemination (IUI) is a rare complication with few case reports; ovarian enlargement due to ovulation induction increases the risk of ovarian rupture, causing severe bleeding. Close attention should be paid to patients with a history of pelvic inflammatory disease before commencing IUI treatment,and such patients should be closely followed up after IUI. Early mea
- Citation: Wu B, Li K, Chen XF, Zhang J, Wang J, Xiang Y, Zhou HG. Ovarian pregnancy rupture following ovulation induction and intrauterine insemination: A case report. World J Clin Cases 2021; 9(29): 8894-8900
- URL: https://www.wjgnet.com/2307-8960/full/v9/i29/8894.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i29.8894
Ovarian pregnancy, a rare form of ectopic pregnancy (EP), constitutes approximately 0.5% to 3.0% of EPs, with a reported incidence ranging from 1 in 7000 to 1 in 40000 pregnancies[1,2].
The use of assisted reproductive technology (ART) is associated with a 0.15% to 1.00% incidence of EP[3]; nevertheless, ovarian pregnancy remains an extremely rare complication despite the increased incidence of EPs following assisted conception[1]. Herein, we present a case of ovarian pregnancy rupture following ovulation induction and intrauterine insemination (IUI), along with the relevant literature review. Further, we evaluate the current literature to understand ways to prevent and manage ovarian pregnancy following IUI.
The patient, a 28-year-old primigravida with a history of 43 d of amenorrhea, presented with bilateral lower abdominal pain and was referred to the emergency department. She reported having undergone IUI 30 d before presentation, owing to primary infertility for 3 years.
The patient had previously undergone ovulation induction and IUI twice. In the second IUI cycle, she underwent ovulation induction with letrozole 5 mg daily during days 5-9 of her menstrual cycle. Transvaginal ultrasound revealed one developed follicle in the right ovary, which was followed by the administration of 10000 IU of human chorionic gonadotrophin (HCG) and IUI on the subsequent day. The initial serum β-HCG concentration was 130 mIU/mL 19 d after IUI, with a slower increase to 697.3 mIU/mL 26 d after IUI.
The patient had no history of sexually transmitted diseases, endometriosis, or previous gynecologic surgery. Nevertheless, the patient was positive for Ureaplasma urealyticum 3 mo before IUI but had no symptoms of urogenital tract infection. Hysterosalpingography revealed a normal uterus and bilateral patent fallopian tubes.
The patient has a history of hyperthyroidism for 12 years. Through drug treatment, normal thyroid function was observed during IUI treatment.No family history.
The patient’s body temperature was 36.3ºC, heart rate was 78 bpm, respiratory rate was 20 breaths per minute, and blood pressure was 96/63 mmHg. Gynecologic examination in the emergency department revealed tenderness in bilateral adnexa uteri, with stable vital signs. About 5 mL of non-coagulated blood was obtained by puncturing the vaginal vault.
The serum β-HCG level of the patient had elevated to 2817 mIU/mL 30 d after IUI.
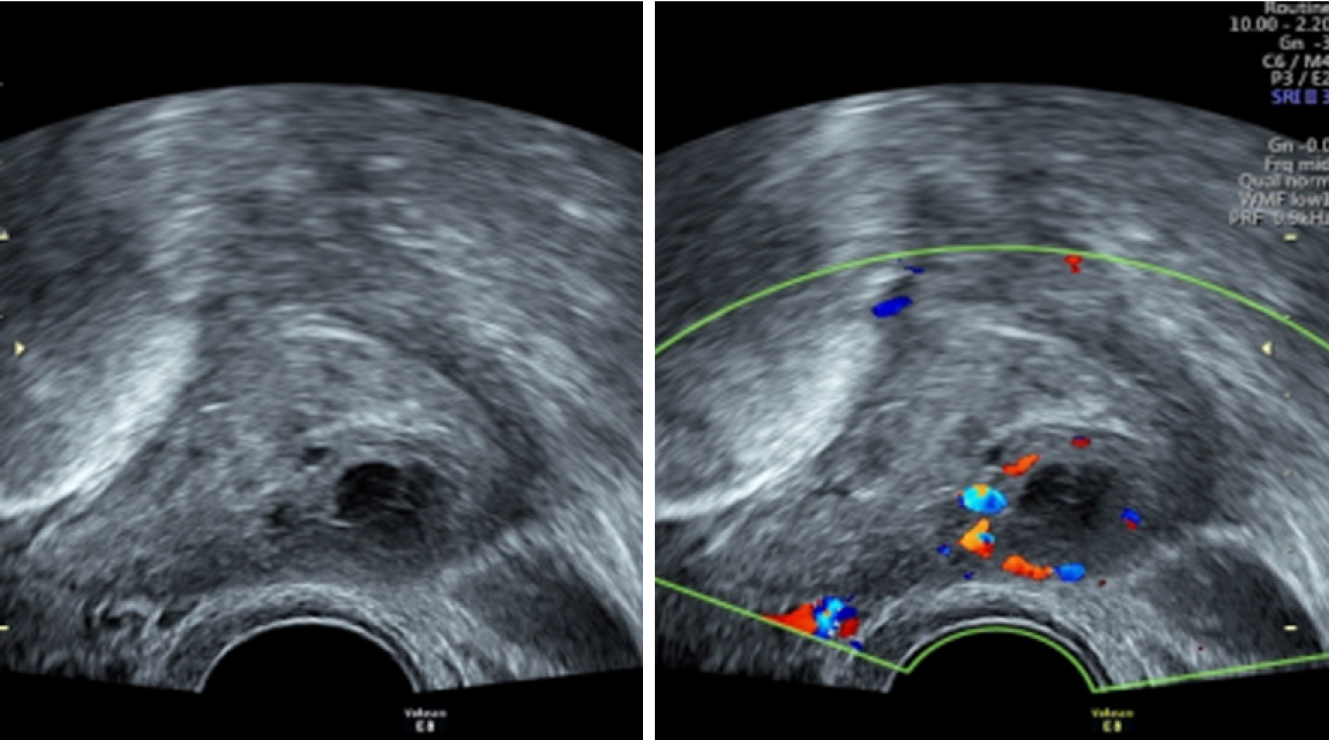
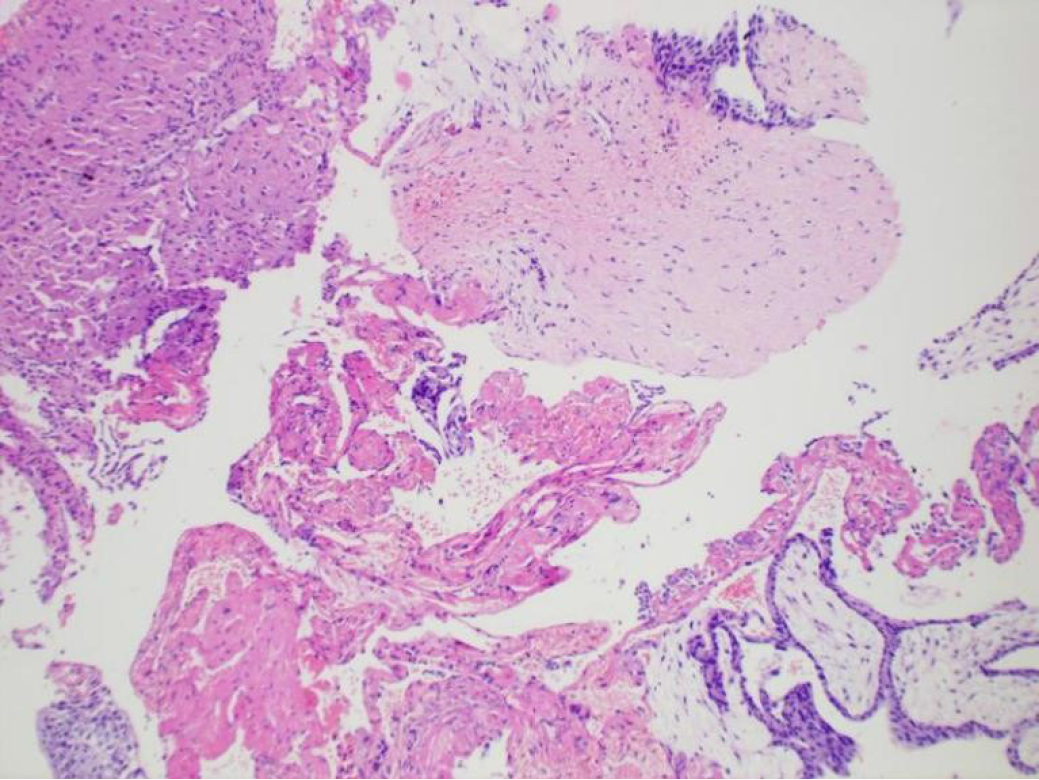
Emergency transvaginal ultrasound examination revealed a uterus that was normal in size but without an intrauterine gestational sac, a 43 mm × 19 mm moderate echogenic mass located very close to the right ovary, and a 39 mm × 18 mm fluid dark area behind the uterus (Figure 1). A preliminary diagnosis of suspected ovarian pregnancy rupture (or rupture of corpus luteum) and hematoperitoneum was established. An emergency laparoscopy was planned. Intraoperative examination revealed a hemorrhagic mass surrounded by a blood clot on the surface of the right ovary. The mass was resected and subjected to pathologic examination. Histological examination revealed chorionic villi attached to the ovarian tissue (Figure 2).
The final diagnosis of the present case was ovarian pregnancy rupture after IUI.
Emergency laparoscopic surgery revealed intraperitoneal hemorrhage amounting to 600 mL, with an approximately 1.5 cm × 1.0 cm × 1.0 cm hemorrhagic mass surrounded by a blood clot on the surface of the right ovary. Suspected chorionic villi were observed inside the mass, with a small rupture with evidence of active bleeding; the mass was resected and subjected to pathologic examination. Nevertheless, the right fallopian tube, contralateral ovary, and ovarian tube appeared normal. Notably, intraoperative examination revealed that the omentum was attached to the right pelvic peritoneum; meanwhile, the sigmoid colon was attached to the left pelvic wall. Pelvic adhesions were then treated.
The patient had a good postoperative recovery and was discharged on postoperative day 4. Follow-up examination revealed that her β-HCG level decreased gradually after the operation, reaching 2.05 mIU/mL on postoperative day 16. About 3 mo later, the patient spontaneously conceived an intrauterine pregnancy, which was still ongoing at the time of writing this study.
Although IUI is a widely used method of ART, it still carries a risk of EP. Ovarian pregnancy is an extremely rare complication after IUI; it may cause pelvic bleeding or ovariectomy, and even circulatory collapse, which could be life threatening[4].
Spiegelberg[5] reported that for an EP to be classified as ovarian pregnancy, the fallopian tube and its fimbriae should be intact and separate from the ovary, the normal position of the ovary should be occupied by the gestational sac, the ovary and the uterus must be connected by the utero-ovarian ligament, and the ovarian tissue must be present in the wall of the gestational sac. All these criteria were fulfilled by the present case.
A literature search yielded only nine cases of ovarian pregnancy following IUI (Table 1)[6-14]. The median patient age in these cases was 29.4 years. All 10 women (including the current patient) were primigravidae, and the ovarian pregnancies of three of these women were diagnosed preoperatively based on the presence of viable fetal heart motion. A common feature observed in these cases was ovarian enlar
| Ref. | Age in yr | Obstetric index | Risk factors | Ovulationinduction regime | No. of dominant follicles | Gestationalage at diagnosis in wk | Rupture hemorrhage | Pregnancy at another site | Preoperative diagnosis | Treatment |
| El-Lakany et al[6] | 30 | G1 | Ovulationinduction | HMG | 2 | 8 | 800 mL | None | No | Laparoscopicoophorectomy |
| Bontis et al[7] | 31 | G1 | Endometriosis, prior laparoscopy and ovulationinduction | HMG | 2 | 4 | No data | None | No | Laparotomy andpartial ovariectomy |
| Einenkel et al[8] | 26 | G1 | Prior laparoscopy and ovulationinduction | Triptorelin + FSH | No data | 7 | 80 mL | None | Yes | Laparoscopiccystectomy |
| Plotti et al[9] | 34 | G1 | Ovulationstimulation | No data | No data | 8 | 350 mL | Bilateral ovarian | Yes | Laparotomyand bilateralovariectomy |
| Kaur et al[10] | 34 | G1 | Ovulationinduction | Letrozole + HMG | No data | 6 | No data | None | Yes | Laparoscopicresection |
| Shiau et al[11] | 24 | G1 | Ovulationinduction | Clomiphene + HMG | 5 | 6 | 1450 mL | None | No | Laparotomyand wedgeresection |
| Goyal et al[12] | 22 | G1 | Ovulationinduction | No data | No data | No data | No data | None | No | Laparotomyand excisionof sac |
| Gundabattula et al[13] | 32 | G1 | Ovulationinduction | Tamoxifen + HMG | 2 | 9 | 2000 mL | Intrauterine gestation | No | Laparoscopicresection |
| Eom et al[14] | 33 | G1 | Ovulationinduction | Clomiphene + HMG | 4 | 6 | 800 mL | Right tubal pregnancy | No | Laparoscopicresection and salpingectomy |
| Present case | 28 | G1 | Ovulationinduction and pelvic adhesion | Letrozole | 1 | 6 | 600 mL | None | No | Laparoscopicresection |
The pathophysiologic mechanisms underlying abnormal embryo implantation are unclear. Some theories suggest that ovarian EP could be caused by an obstruction in the release of the ovum from the ruptured follicle after intrafollicular fertilization or by embryo migration, which is related to certain conditions that damage the fallopian tube, altering tubal motility[15,16].
The risk factors for ovarian pregnancy include intrauterine device usage, pelvic inflammatory disease (PID), previous gynecologic surgery, endometriosis, sexually transmitted infections, use of ART, previous ectopic pregnancy, and salpingitis[4]. Fernandez et al[17] reported that ovulation induction carries an increased risk of ovarian pregnancy; during ovulation induction, the increased level of estrogen and progesterone would inhibit the peristalsis frequency of the fallopian tube and affect its normal movement.
Several authors have reported that ART procedures increase the chance of an EP[18-20]. The ovarian pregnancy following the IUI procedure in the present case could be attributed to the higher volume of sperm suspension and a higher pressure with which it is injected into the uterus, causing backward migration of the egg to the surface of the ovary following fertilization on the ovarian surface scars from ovulation.
According to a review focused on unusual EPs[21], ovarian pregnancy is associated with PID; this condition is thought to be responsible for ovarian inflammation, which causes thickening of the tunica albuginea, reducing the follicular fluid pressure. This is speculated to cause ovulation disorder, wherein the ovum is detained in the broken follicles and fertilized just in the ovary. This pathologic process may account for the primary implantation in the ovary. Therefore, the pelvic adhesions detected during laparoscopic surgery in this case may also have been responsible for the ovarian pregnancy. The diagnosis of PID may have been missed during gynecological examination before IUI treatment. Attention should be paid to the screening and timely treatment of PID to prevent pelvic adhesion before starting ART treatment.
Thus, close clinical follow-up, monitoring, and routine ultrasound examination are recommended after ovulation induction. In the present case, IUI after ovulation induction and pelvic adhesions may have been the causes of ovarian EP.
Early diagnosis is important to avoid more serious complications and emergency invasive surgery. It could help to understand the risk factors for EP. Transvaginal ultrasound is a valuable diagnostic method to detect early ovarian pregnancy. However, specific ultrasound features that aid a preoperative diagnosis may not always be visible. Thus, serial quantitative β-HCG levels correlated with ultrasound findings are recommended to distinguish an early intrauterine pregnancy from EP[4]. Further, early diagnosis through ultrasound examination could be difficult in women who have previously undergone ovarian induction. In fact, patients who have already undergone ovarian induction typically have enlarged ovaries and accumulated fluid in the pelvic cavity. Therefore, pelvic ultrasound should be performed more carefully in such patients. Although the ultrasound features of ovarian pregnancy were obvious in the current case, they were insufficient to establish a definite diagnosis.
Although surgery is the preferred treatment for early ovarian pregnancy, less aggressive treatment that ensures preservation of the ovarian tissue is warranted, as these patients are expected to conceive again. Laparoscopy approach should be the preferred treatment method for such patients[6,8,10,13,14].
Five of the previous nine patients were treated laparoscopically, and laparotomy was performed in the other four cases. As our patient had abdominal pain with hemoperitoneum, emergent laparoscopic resection surgery was performed; the hemoperitoneum was caused by a small mass in the right ovary, which was surrounded by a hematoma and showed minimal bleeding. The final histological examination revealed chorionic villi, confirming the diagnosis of ovarian pregnancy. Just 3 mo after surgery, the patient conceived a spontaneous intrauterine pregnancy.
In conclusion, the present case reiterates that close attention should be paid to a history of PID before IUI treatment,and patients with such a history should be closely followed up after IUI. Early measurement of serum β-HCG levels and ultrasonic examination could facilitate a timely diagnosis of ovarian pregnancy. Laparoscopic surgery could provide an exact diagnosis and enable prompt surgical intervention in these rare cases, along with preserving the ovarian tissue.
| 1. | Raziel A, Schachter M, Mordechai E, Friedler S, Panski M, Ron-El R. Ovarian pregnancy-a 12-year experience of 19 cases in one institution. Eur J Obstet Gynecol Reprod Biol. 2004;114:92-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 63] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 2. | Joseph RJ, Irvine LM. Ovarian ectopic pregnancy: aetiology, diagnosis, and challenges in surgical management. J Obstet Gynaecol. 2012;32:472-474. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 26] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 3. | Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, Wright VC. A comparison of heterotopic and intrauterine-only pregnancy outcomes after assisted reproductive technologies in the United States from 1999 to 2002. Fertil Steril. 2007;87:303-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 4. | Jwa SC, Seto S, Takamura M, Kuwahara A, Kajihara T, Ishihara O. Ovarian stimulation increases the risk of ectopic pregnancy for fresh embryo transfers: an analysis of 68,851 clinical pregnancies from the Japanese Assisted Reproductive Technology registry. Fertil Steril. 2020;114:1198-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 18] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 5. | Spiegelberg O. Casuistry in ovarian pregnancy. Arch Gynecol Surv. 1978;13:73-79. [RCA] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 140] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 6. | El-Lakany N, Hock Y, Boyd N. Obstetric case reports: Primary ovarian pregnancy following intra-uterine insemination. J Obstet Gynaecol. 1995;15:182-183. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Bontis J, Grimbizis G, Tarlatzis BC, Miliaras D, Bili H. Intrafollicular ovarian pregnancy after ovulation induction/intrauterine insemination: pathophysiological aspects and diagnostic problems. Hum Reprod. 1997;12:376-378. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 33] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Einenkel J, Baier D, Horn LC, Alexander H. Laparoscopic therapy of an intact primary ovarian pregnancy with ovarian hyperstimulation syndrome: case report. Hum Reprod. 2000;15:2037-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 9. | Plotti F, Di Giovanni A, Oliva C, Battaglia F, Plotti G. Bilateral ovarian pregnancy after intrauterine insemination and controlled ovarian stimulation. Fertil Steril. 2008;90:2015.e3-2015.e5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Kaur H, Shashikala T, Bharath M, Shetty N, Rao KA. Ovarian ectopic pregnancy following assisted reproductive techniques: A rare entity. Int J Infert Fetal Med. 2011;2:37-39. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Shiau CS, Huang YH, Chang MY, Hsieh TT, Lo LM, Ching CC, Hsieh CL. Ovarian pregnancy following intrauterine insemination. Taiwan J Obstet Gynecol. 2012;51:458-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Goyal LD, Tondon R, Goel P, Sehgal A. Ovarian ectopic pregnancy: A 10 years' experience and review of literature. Iran J Reprod Med. 2014;12:825-830. [PubMed] |
| 13. | Gundabattula SR, Resapu P, Surampudi K, Surapaneni T, De Padua M. Ovarian apoplexy resulting from ruptured heterotopic pregnancy following intrauterine insemination. J Obstet Gynaecol Res. 2017;43:1222-1226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Eom JM, Choi JS, Bae J, Lee WM, Lee E, Lee J, Keum JH. Coexisting ovarian and tubal pregnancies on opposite sides after intrauterine insemination: a case report. BMC Pregnancy Childbirth. 2018;18:259. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Melcer Y, Maymon R, Vaknin Z, Pansky M, Mendlovic S, Barel O, Smorgick N. Primary Ovarian Ectopic Pregnancy: Still a Medical Challenge. J Reprod Med. 2016;61:58-62. [PubMed] |
| 16. | Mathur SK, Parmar P, Gupta P, Kumar M, Gilotra M, Bhatia Y. Ruptured primary ovarian ectopic pregnancy: case report and review of the literature. J Gynecol Surg. 2015;31:354-356. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Fernandez H, Coste J, Job-Spira N. Controlled ovarian hyperstimulation as a risk factor for ectopic pregnancy. Obstet Gynecol. 1991;78:656-659. [PubMed] |
| 18. | Marcus SF, Brinsden PR. Analysis of the incidence and risk factors associated with ectopic pregnancy following in-vitro fertilization and embryo transfer. Hum Reprod. 1995;10:199-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 123] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 19. | Strandell A, Thorburn J, Hamberger L. Risk factors for ectopic pregnancy in assisted reproduction. Fertil Steril. 1999;71:282-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 123] [Cited by in RCA: 110] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 20. | Clayton HB, Schieve LA, Peterson HB, Jamieson DJ, Reynolds MA, Wright VC. Ectopic pregnancy risk with assisted reproductive technology procedures. Obstet Gynecol. 2006;107:595-604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 163] [Cited by in RCA: 160] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 21. | Shan N, Dong D, Deng W, Fu Y. Unusual ectopic pregnancies: a retrospective analysis of 65 cases. J Obstet Gynaecol Res. 2014;40:147-154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 25] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Salimi M S-Editor: Wang LL L-Editor: Filipodia P-Editor: Yuan YY