Published online Oct 6, 2021. doi: 10.12998/wjcc.v9.i28.8587
Peer-review started: May 25, 2021
First decision: June 25, 2021
Revised: July 3, 2021
Accepted: August 12, 2021
Article in press: August 12, 2021
Published online: October 6, 2021
Processing time: 125 Days and 18.2 Hours
A patient with advanced tuberculosis of the hip joint combined with Crowe type IV developmental dysplasia of the hip (DDH) and a drainage sinus is a rare condition. There are no previous reports of this condition, and it is a complex challenge for surgeons to develop a treatment scheme.
We report a 73-year-old male patient with severe hip pain and drainage sinus of the left hip for one month. Approximately 40 years ago, a drainage sinus occurred at the lateral left hip was healed at the local hospital with anti-infectious therapy. After the sinus healed, gradual pain occurred in the left hip for 40 years. Approximately one month prior, hip pain was sharply aggravated, and a drainage sinus reoccurred in the left hip. The X-ray and computed tomography examinations showed destruction of the head and neck of the left femur, as well as an acetabular deformity. The results of Mycobacterium tuberculosis antibody and Xpert were positive. Therefore, the patient was diagnosed with advanced TH combined with Crowe type IV DDH. After 22 d of treatment with anti-tuberculosis chemotherapy, the sinus healed, and the patient underwent one-stage total hip arthroplasty (THA) surgery consisting of debridement, osteotomy, and joint replacement. After surgery, the patient received anti-tuberculosis chemotherapy drugs for nine months, with no recurrent infection. After one year of follow-up, the Harris score of the patient increased from 21 pre-THA to 86.
Although drainage sinuses are a contraindication to one-stage THA, one-stage THA is still an effective and safe surgical method after the sinus heals.
Core Tip: We report a 73-year-old male patient with severe hip pain and drainage sinus of the left hip for one month. The X-ray and computed tomography examinations showed destruction of the head and neck of the left femur, as well as an acetabular deformity. The results of Mycobacterium tuberculosis antibody and Xpert were positive. Therefore, the patient was diagnosed with advanced tuberculosis hip combined with Crowe type IV Developmental dysplasia of the hip. After 22 d of treatment with anti-tuberculosis chemotherapy, the sinus healed, and the patient underwent one-stage total hip arthroplasty surgery. After surgery, the patient received anti-tuberculosis chemotherapy drugs for nine months, with no recurrent infection.
- Citation: Zhu RT, Shen LP, Chen LL, Jin G, Jiang HT. One-stage total hip arthroplasty for advanced hip tuberculosis combined with developmental dysplasia of the hip: A case report. World J Clin Cases 2021; 9(28): 8587-8594
- URL: https://www.wjgnet.com/2307-8960/full/v9/i28/8587.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i28.8587
Tuberculosis of the hip joint (TH) is a severe osteoarticular tuberculosis and always results in cartilage and bone destruction, causing pain, deformity, shortening, and instability[1]. In its early stages, symptoms and imaging changes are not typical, and the diagnosis is easily missed[2]. When severe hip bone destruction occurs, TH has reached advanced stages[1]. Total hip arthroplasty (THA) is always considered the preferred treatment option for advanced TH, which could provide a painless stable joint with normal gait and is generally divided into two-stage THA and one-stage THA[3]. Although two-stage THA achieves satisfactory clinical efficacy for treating advanced TH[4], the second-step replacement surgery must be performed several months after debridement, leading to poor joint mobility (even stiffness) and muscle atrophy, increasing the difficulty of the whole treatment procedure[5]. Therefore, surgeons prefer to choose one-stage THA that could attain satisfactory clinical efficacy and effectively shorten the treatment time[6], except for the presence of a drainage sinus, which is a contraindication to one-stage THA[7].
When the patient was admitted to our department for severe hip pain and a drainage sinus, we diagnosed advanced TH with Crowe type IV DDH of his left hip through a thorough examination. It was difficult for us to develop a suitable treatment scheme that could improve the function of the patient's TH and prevent tuberculosis. Although the patient was not qualified for one-stage THA because of sinus drainage, the first step of radical debridement and cement spacer implantation could destroy the pseudarthrosis between the ilium ala and proximal femur. If so, the stability of the left hip would be destroyed, and the patient would have to be confined to bed for at least three months, which could be fatal for the senior patient because of the severe complications resulting from bed rest.
Unfortunately, there is no previous literature or report teaching us how to develop a suitable scheme. Considering the probable serious complications of two-stage THA and improving joint function, we finally decided to carry out a one-stage THA consisting of debridement, osteotomy, and THA. In this report, we introduced our treatment plan in detail and showed the complications and recovery conditions of the patient in total.
A 73-year-old male patient was admitted to our department for a drainage sinus at the lateral skin surface of the left hip combined with severe joint pain.
The sinus occurred lateral to the left hip 40 years ago and healed with anti-infective treatment and debridement at the local hospital. One month prior, the left hip pain was exacerbated and the sinus reoccurred. After ineffective anti-infective therapy (levofloxacin and ceftazidime) at the local hospital, the patient presented to our department.
The patient was diagnosed with tuberculosis more than 40 years ago and has been cured in a local hospital.
The patient denied any other specific personal or family history of other disease.
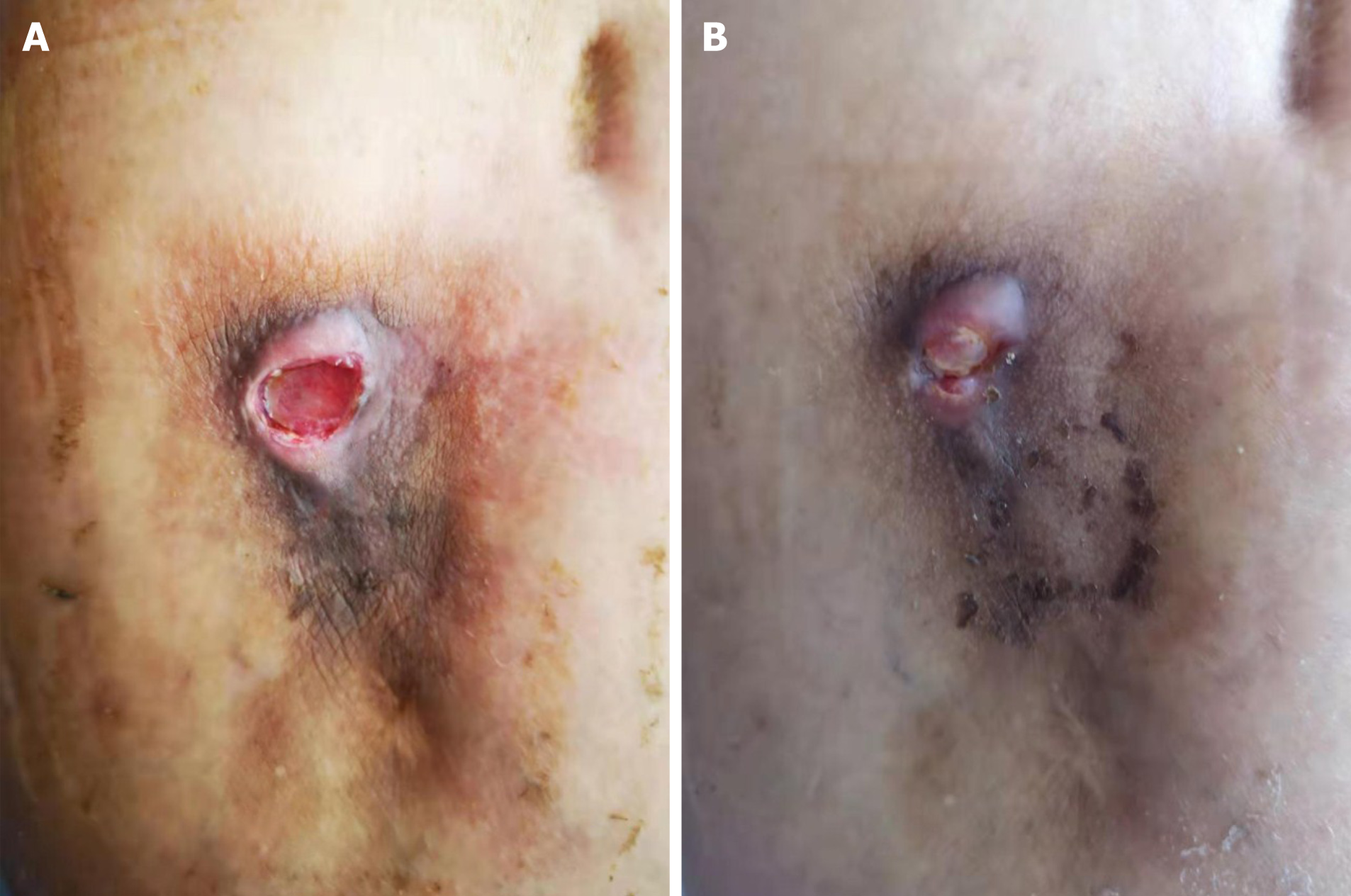
The physical examination showed plenty of fresh granulation tissue in a drainage sinus (Figure 1A). The patient had severe hip pain and was unable to move actively or passively. The left lower limb was approximately 3 cm shorter than the right lower limb. The patient could walk on the ground with the help of a crutch by himself. The Harris score of the patient's left hip was 21.
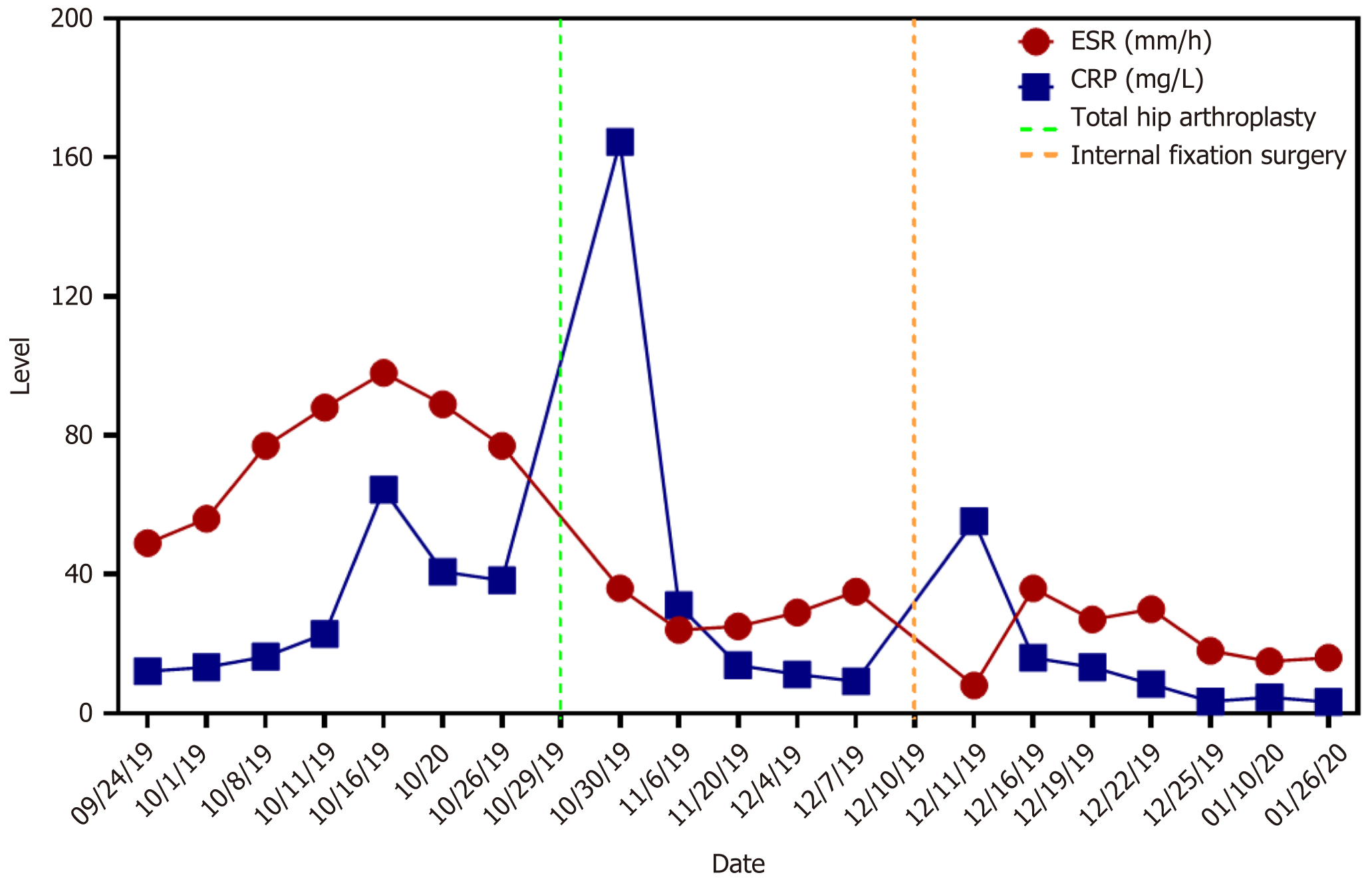
At the time of admission, the erythrocyte sedimentation rate (ESR) was 49 mm/h, and the C-reactive protein (CRP) level was 12.12 mg/L. Although a Mycobacterium tuberculosis smear was negative, we diagnosed the patient with TH according to both positive Mycobacterium tuberculosis antibody and Xpert results.
The preoperative X-ray (Figure 2A) and computed tomography (Figure 2B and C) showed heavy destruction of the left femoral head and neck, pseudarthrosis between the proximal femur and iliac ala, and a smaller and more shallow original acetabulum. The preoperative magnetic resonance (Figure 2D and E) showed a slender localized sinus and no infective foci in the pelvic cavity.
The patient was eventually diagnosed with advanced tuberculosis of the hip combined with Crowe type IV developmental dysplasia of the hip.
After undergoing anti-tuberculosis treatment (isoniazid, rifampin, pyrazinamide, and ethambutol) for 22 d, the sinus was almost healed (Figure 1B). Although a drainage sinus is a contraindication to THA, thinking of the healed sinus and difficulty of cement spacer placement in a severe hip malformation, we decided to carry out a one-stage THA on the patient.
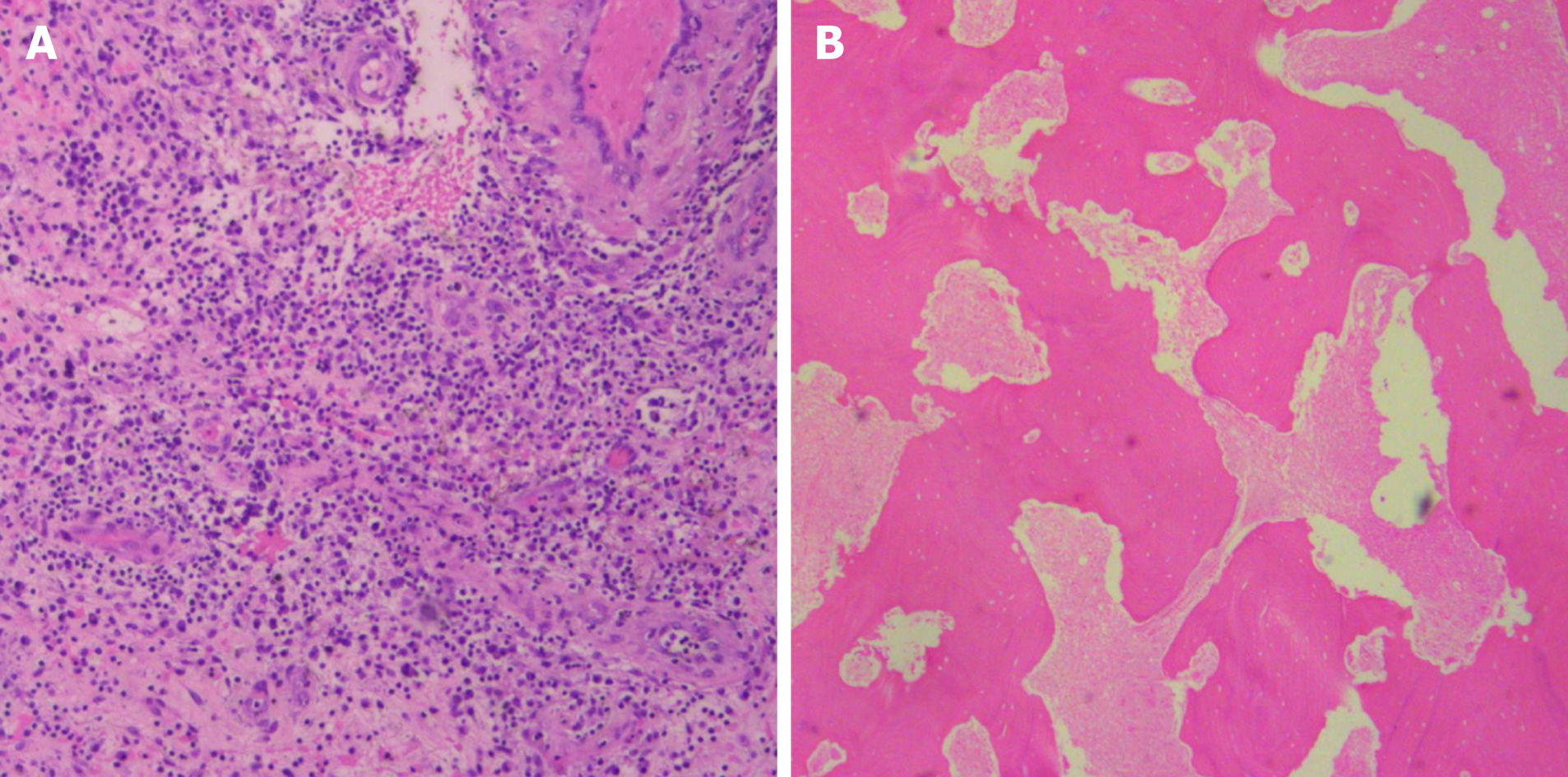
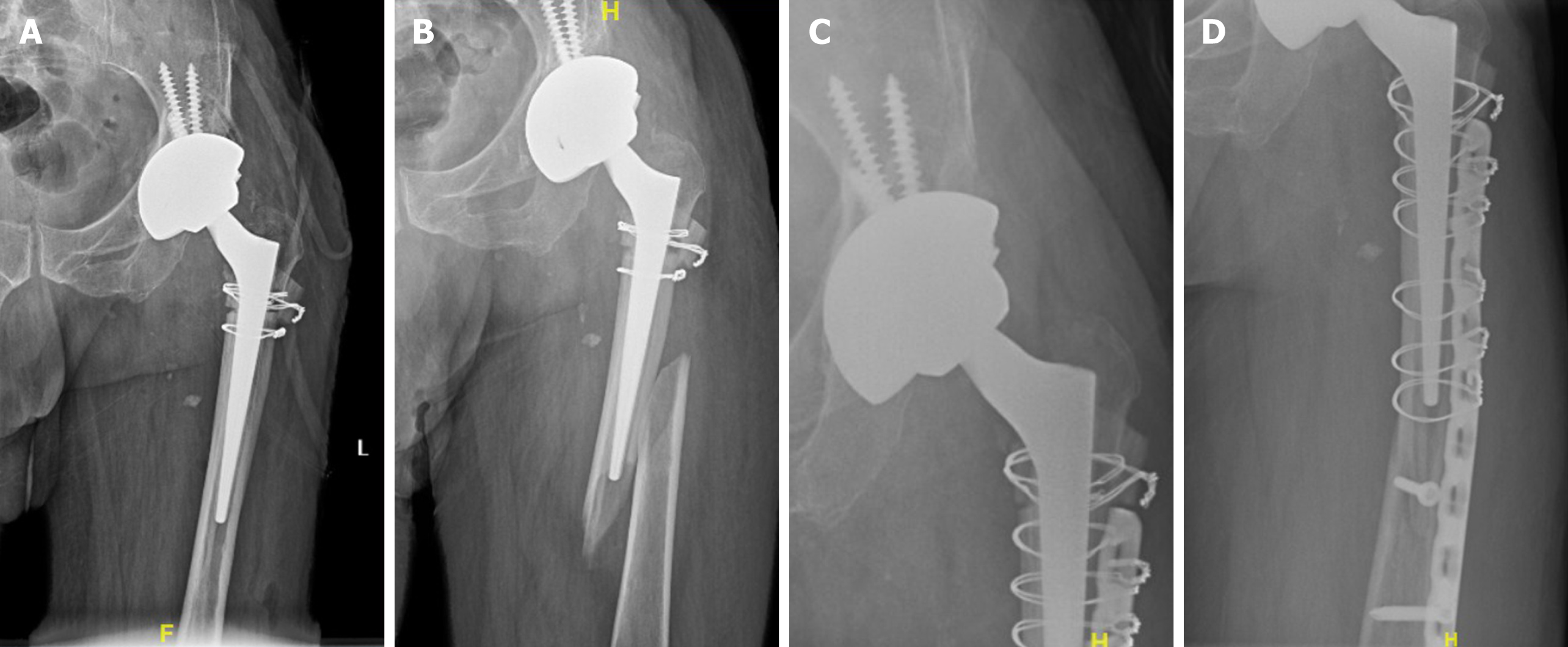
At the beginning of the operation process, the sinus was excised entirely, and sinus tissue was obtained to investigate histological changes. The intraoperative rapid pathological diagnosis showed no apparent active infection (Figure 3A). The operating field revealed complete necrosis of the gluteus maximus and gluteus medius, disappearance of the left femoral head and neck, partial structural destruction of the iliac crest, and apparent upward movement of the proximal femur. The lesion tissue was entirely excised with bone forceps, and the destroyed bone of the proximal femur, except the more significant trochanter part, was released with a wire saw. After repeatedly washing the wound with iodophor, hydrogen peroxide, and saline, we changed the operating garment and sterile towel. Then, a subtrochanteric osteotomy was carried out to protect the sciatic nerve by lessening the leg lengthening. Finally, we chose a cementless prosthesis to complete the THA surgery. The postoperative X-ray showed that the prosthesis was in a good position (Figure 4A). The lesion tissue of the left hip was sent to for pathological examination postoperatively, and the result showed evident caseous necrosis (Figure 3B).
Postoperatively, the patient received anti-tuberculosis drugs (isoniazid, rifampicin, pyrazinamide, and ethambutol) and was asked to remain in bed for six weeks after the procedure. Unfortunately, six weeks after surgery, the patient fell when he was walking to the toilet and was sent to our hospital immediately. The X-ray showed periprosthetic fractures, no loss of the prosthesis, and no destruction of the proximal femur (Figure 4B). Therefore, we carried out reduction and internal fixation of the fracture with a plate and wire. During the surgery, there was no loss of the prosthesis or reactive tuberculosis in the surgical field. Three months after internal fixation, the X-ray of the left hip showed no recurrent bone destruction or prosthesis loss (Figure 4C and D).
After internal fixation surgery, the patient continually received anti-tuberculosis chemotherapy (isoniazid, rifampicin, pyrazinamide, and ethambutol) for nine months. Three months after internal fixation surgery, the patient could walk with a crutch, and six months after surgery, he was able to walk independently.
Eighty-nine days after one-stage THA, the ESR and CRP levels returned to normal, and the tests were negative three times in a row (Figure 5). At 1-year follow-up, the Harris score of the patient was 86.
This is the first report of a patient with advanced TH with Crowe type IV DDH, especially with a drainage sinus at the affected hip. It was a challenge for us to develop a suitable clinical treatment scheme, preventing tuberculosis recurrence and preserving the function of the joint. We developed a one-stage THA plan through a literature review, including perioperative anti-tuberculosis chemotherapy, intraoperative debridement, and THA. At one-year follow-up, the patient's TH had good function, and the TH did not recur.
There are three treatment options for advanced TH: Excision arthroplasty, arthrodesis, and THA. Excision arthroplasty can offer a painless and mobile hip but finally results in hip instability and abnormal gait[8,9]. Arthrodesis offers a severely dysfunctional hip, back pain, and abnormal gait and is rarely chosen[10]. THA can provide a painless stable joint with normal gait and is generally divided into two forms: One-stage THA and two-stage THA. As a result of joint infectious disease, two-stage THA is the gold standard for treatment[4]. The first step involves radical debridement and implantation of the cement spacer. The second step is carried out after the infection is under control and involves additional debridement and implantation of the metal prosthesis. However, the second step must be performed several months after the first step, resulting in poor joint mobility (even stiffness) and muscle atrophy, increasing the difficulty of the whole treatment procedure[5].
The difference in pathogenic bacteria characteristics between pyogenic pathogens and tuberculosis bacilli creates the conditions for one-stage surgery. Bacteria covered by biofilms have strong resistance to antibiotics and host immune attacks, leading to severe surgical failure[11]. Contrary to common purulent pathogens, tuberculosis bacilli have unique biological characteristics, including slow growth, no adhesion to metal surfaces, and little biofilm formation[11-13]. Furthermore, one-stage surgery with metal implantation for active spinal tuberculosis has been successful[14]. Therefore, an increasing number of surgeons have applied one-stage THA to treat TH and have achieved satisfactory results[6].
In addition, it is not easy to carry out two-stage THA on Crowe type IV DDH[15-17]. After debridement of the affected TH, the pseudarthrosis between the proximal femur and ilium was destroyed, and implantation of an antibiotic-loaded cement spacer could not reconstruct the stability of the affected TH. This may lead to an extended stay in the bed and many complications for patients, such as deep venous thrombosis, myophagism, and pressure sores. Therefore, the one-stage THA method might be the best choice in patients with advance TH combined with Crowe type IV DDH. However, many authors believe that a drainage sinus is a contraindication to one-stage THA, because the drainage sinus is often associated with a mixed infection of other common pyogenic pathogens[4,12,18]. In our report, although a drainage sinus was lateral to the left hip, when the sinus had healed and intraoperative rapid pathological examination showed no apparent active infection, we believed that it was safe and effective to carry out one-stage THA.
Moreover, regardless of the treatment method, it is essential that standard first-line anti-tuberculosis chemotherapy, including isoniazid, rifampicin, pyrazinamide, and ethambutol, be applied for every patient between 2 wk and 6 wk preoperatively and between 9 mo and 12 mo postoperatively[19,20]. Therefore, after the level of ESR and CRP returned to normal, the patient in our report continued to receive anti-tuberculosis chemotherapy until nine months after one-stage THA.
Finally, through our treatment, the patient could walk by himself six months after internal fixation surgery, and the levels of ESR and CRP returned to normal 89 d after one-stage THA. Meanwhile, the limitation of our study is obvious. First, because of the rarity of similar cases, only one case was too few to demonstrate the effectiveness of our treatment method. Second, the follow-up data in our study were only one year, and it could not prove the long-term effectiveness.
In our opinion, to reduce complications caused by bed rest and reduce mortality, one-stage THA is more suitable for patients with advanced TH combined with Crowe type IV DDH. Moreover, although the drainage sinus was a contraindication for one-stage THA, when the sinus had healed and intraoperative rapid pathological examination showed no apparent active infection, we believed it was safe and effective to carry out one-stage THA.
| 1. | Tan SM, Chin PL. Total hip arthroplasty for surgical management of advanced tuberculous hip arthritis: Case report. World J Orthop. 2015;6:316-321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Cansü E, Erdogan F, Ulusam AO. Incision infection with Mycobacterium tuberculosis after total hip arthroplasty without any primary tuberculosis focus. J Arthroplasty. 2011;26:505.e1-505.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Zhang J, Liang L, Yang B, Li S, Yang X, Li J, Sun L, Han W. Total hip arthroplasty for tuberculosis: a case series. Ann Palliat Med. 2021;10:495-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Li L, Chou K, Deng J, Shen F, He Z, Gao S, Li Y, Lei G. Two-stage total hip arthroplasty for patients with advanced active tuberculosis of the hip. J Orthop Surg Res. 2016;11:38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Chang CH, Hu CC, Chang Y, Hsieh PH, Shih HN, Ueng SW. Two-stage revision arthroplasty for Mycobacterium Tuberculosis periprosthetic joint infection: An outcome analysis. PLoS One. 2018;13:e0203585. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 6. | Zhang YC, Zhang H. One-stage total joint arthroplasty for patients with active tuberculosis. Orthopedics. 2013;36:328-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Bhosale PB, Jaiswal R, Purohit S, Arte SM. Total Hip Arthroplasty in 52 Active Advanced Tubercular Arthritic Hips. J Arthroplasty. 2021;36:1035-1042. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Tuli SM, Mukherjee SK. Excision arthroplasty for tuberculous and pyogenic arthritis of the hip. J Bone Joint Surg Br. 1981;63-B:29-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 23] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Clegg J. The results of the pseudarthrosis after removal of an infected total hip prosthesis. J Bone Joint Surg Br. 1977;59:298-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 51] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Riggins RS, Kraus JF, Lipscomb PR. Osteoarthritis of the hip. A survey of treatment. Clin Orthop Relat Res. 1975;(106):56-59. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Stewart PS, Costerton JW. Antibiotic resistance of bacteria in biofilms. Lancet. 2001;358:135-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3133] [Cited by in RCA: 3012] [Article Influence: 120.5] [Reference Citation Analysis (5)] |
| 12. | Neogi DS, Yadav CS, Ashok Kumar, Khan SA, Rastogi S. Total hip arthroplasty in patients with active tuberculosis of the hip with advanced arthritis. Clin Orthop Relat Res. 2010;468:605-612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Ha KY, Chung YG, Ryoo SJ. Adherence and biofilm formation of Staphylococcus epidermidis and Mycobacterium tuberculosis on various spinal implants. Spine (Phila Pa 1976). 2005;30:38-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 151] [Cited by in RCA: 151] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 14. | Govender S. The outcome of allografts and anterior instrumentation in spinal tuberculosis. Clin Orthop Relat Res. 2002;(398):60-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 15. | Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;(213):20-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 355] [Cited by in RCA: 284] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 16. | Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983;(175):79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Lloyd-Roberts GC. Osteoarthritis of the hip; a study of the clinical pathology. J Bone Joint Surg Br. 1955;37-B:8-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 76] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Oztürkmen Y, Karamehmetoğlu M, Leblebici C, Gökçe A, Caniklioğlu M. Cementless total hip arthroplasty for the management of tuberculosis coxitis. Arch Orthop Trauma Surg. 2010;130:197-203. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Sultan AA, Dalton SE, Umpierrez E, Samuel LT, Rose E, Tamer P, Rabin JM, Mont MA. Total hip arthroplasty in the setting of tuberculosis infection of the hip: a systematic analysis of the current evidence. Expert Rev Med Devices. 2019;16:363-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 20. | Saraf SK, Tuli SM. Tuberculosis of hip: A current concept review. Indian J Orthop. 2015;49:1-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 30] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Yiğit Ş S-Editor: Liu M L-Editor: A P-Editor: Zhang YL