Published online Oct 6, 2021. doi: 10.12998/wjcc.v9.i28.8531
Peer-review started: April 28, 2021
First decision: May 23, 2021
Revised: May 26, 2021
Accepted: August 12, 2021
Article in press: August 12, 2021
Published online: October 6, 2021
Processing time: 152 Days and 19.6 Hours
Acute renal artery thrombosis is a relatively rare disease. Early diagnosis and emergent treatment can prevent the loss of renal function and the development of hypertension.
We report a patient with acute renal artery thrombosis who presented to our hospital with acute-onset right flank pain and was treated by percutaneous mechanical thrombectomy using the Rotarex device. After 2 mo, right kidney function had recovered slightly.
Renal artery thrombosis may lead to loss of renal function and the development of hypertension. Rotarex mechanical thrombectomy may be a viable treatment option for rapid recanalization of the renal artery in patients with renal artery thrombosis.
Core Tip: Acute renal artery thrombosis is a relatively rare disease, and will lead to acute renal infarction. Several options have been reported such as systemic anticoagulation, percutaneous interventional therapy and surgical operation. It is the first time that Rotarex mechanical thrombectomy catheter was used to treat renal artery thrombosis. Our case confirmed that the Rotarex system may be a safe way to rapidly recanalize the renal artery in renal artery thrombosis patient. It may be a treatment option for renal artery thrombosis in the future.
- Citation: Li WR, Liu MY, Chen XM, Zhang ZW. Rotarex mechanical thrombectomy in renal artery thrombosis: A case report. World J Clin Cases 2021; 9(28): 8531-8536
- URL: https://www.wjgnet.com/2307-8960/full/v9/i28/8531.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i28.8531
Acute renal artery thrombosis (RAT) is a relatively rare disease, and can lead to acute renal infarction. Most of the literature on this disease is published in case reports and retrospective studies[1,2]. Because of its low incidence and atypical symptoms, and as it usually manifests as abdominal pain similar to acute pyelonephritis or renal colic, acute RAT is easily misdiagnosed[3,4]. Early diagnosis and emergent treatment can prevent the loss of renal function and the development of hypertension. A contrast-enhanced computed tomography (CT) scan is considered necessary for the diagnosis[5]. There are no available guidelines for the treatment of this rare entity, and the therapeutic options for acute renal infarction include anticoagulation, thrombolytics, and surgical thrombectomy or catheter-based treatments[6]. Here we report a patient with acute RAT who presented to our hospital with acute-onset right flank pain and was treated with percutaneous mechanical thrombectomy (PMT) using the Rotarex device. To the best of our knowledge, this is the first case report of Rotarex mechanical thrombectomy for RAT.
A 41-year-old man presented to the Emergency Department with acute onset right-sided flank pain that started 20 d prior to admission. Twenty days previously, the patient had acute right flank pain at night, and a CT scan showed no obvious abnormalities. According to his symptoms, the patient was diagnosed with urinary calculi. A few hours later, the patient's symptoms resolved spontaneously. He had similar symptoms again 10 d later, and the findings of a CT scan were similar to those of the first scan. His symptoms resolved after pethidine administration. He presented to our hospital with right-sided flank pain and vomiting. The pain was continuous, non-radiating and without any aggravating or relieving factors.
The patient had no history of fever, jaundice, constipation, diarrhea, burning micturition, hematuria, trauma, drug intake, alcohol intake, or weight loss.
He had a history of arrhythmia and was treated with radiofrequency ablation, but the specific type of arrhythmia was not clear.
No positive history of family members was reported.
Physical examination showed a body temperature of 36.2 °C, blood pressure of 169/119 mmHg, pulse rate of 88 bpm, and respiratory rate of 18 breaths/min, and oxygen saturation was 97%. Cardiac and respiratory examinations were unremarkable. The abdomen was soft and not distended, moving normally with respiration, with no tenderness, no guarding or rigidity, no organomegaly, no free fluid in the abdomen, and normal bowel sounds. The urine output was maintained.
Blood tests revealed normal hemogram, blood sugar, serum lipase, and serum amylase levels, and liver function, urine examination, lipid profile, and electrocardiogram were also normal. The serum lactate dehydrogenase level was 338 IU (< 250 IU). Renal parameters at the time of admission showed blood urea of 4.97 mmol/L (3.1-8 mmol/L) and serum creatinine of 115.9 μmol/L (59-103 μmol/L).
Because the previous two CT scans did not find the cause of abdominal pain, the possibility of mesenteric ischemia was suggested, and a contrast-enhanced CT scan of the abdomen was performed, which showed an area of non-enhancement in the right kidney and reduced flow in the right renal artery (Figure 1). He was immediately transferred to our department, and renal artery color Doppler ultrasound was performed, which confirmed stenosis of the right renal artery. In order to evaluate the current sub-renal function, renal dynamic imaging was carried out, and the glomerular filtration rate (GFR) in the left kidney was 89.5 mL/min, and was 20.9 mL/min in the right kidney.
Other laboratory tests were performed to exclude coagulation disorders, including protein C, protein S, antithrombin III, erythrocyte sedimentation rate, C-reactive protein, anti-neutrophil cytoplasmic antibody, and antinuclear antibody, and the results were all negative except for increased protein S level, which was 148.9% (55%-130%).
The final diagnosis was acute renal artery thrombosis.
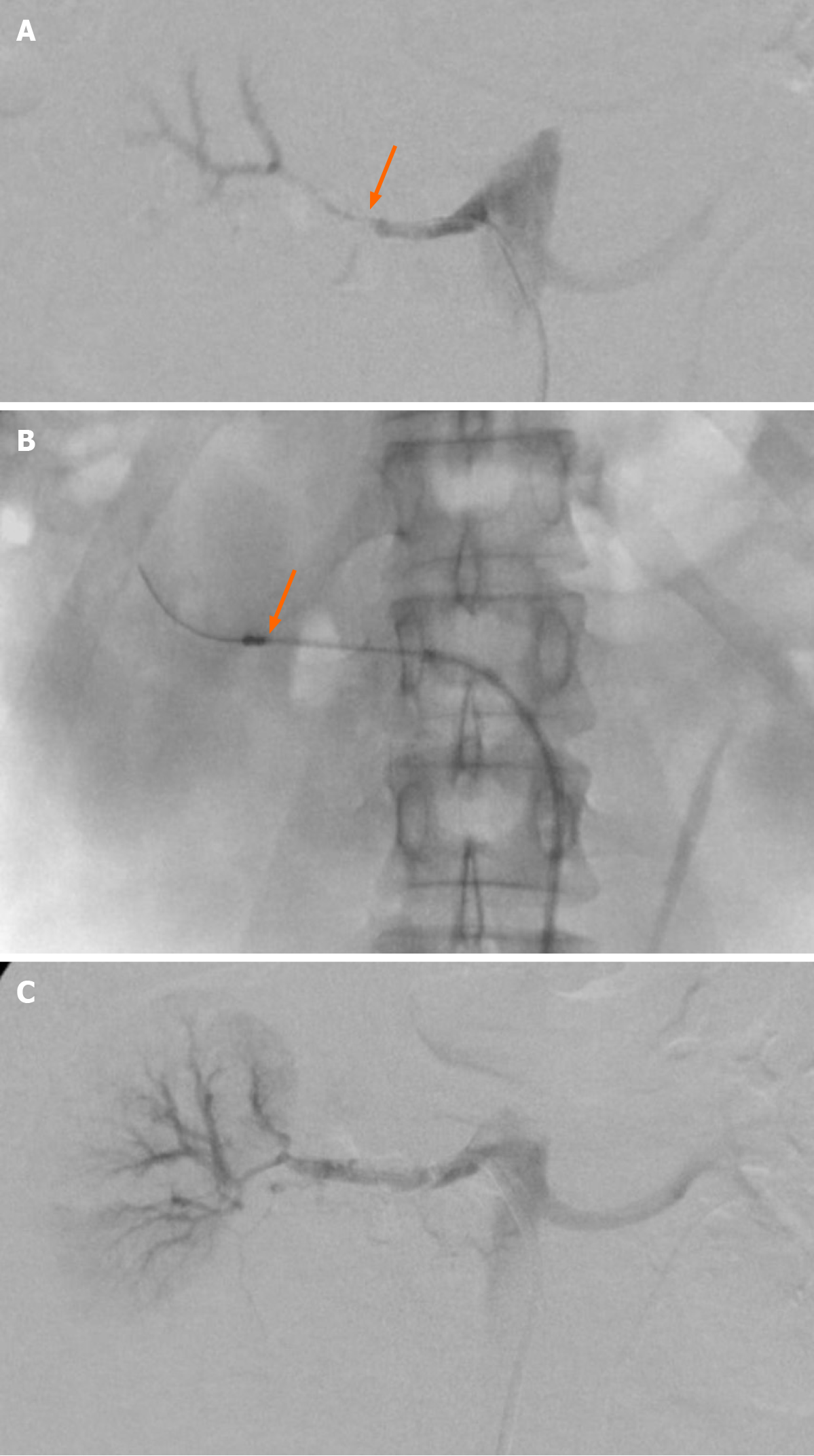
In order to avoid further RAT and prevent the loss of renal function and the development of hypertension, it was decided to use a Rotarex PMT device to restore the blood supply to the right kidney. The patient underwent arteriography via right femoral artery access. The left-sided renal angiography was normal, and the right-sided renal angiography showed thrombotic occlusion of the renal artery (Figure 2A). A 0.018-in wire was passed through the occluded segment to the distal artery as far as possible with the purpose of sufficient support. The PMT device used was the Rotarex system (Straub Medical, Wangs, Switzerland), with a 6F sheath diameter device. The Rotarex device was inserted over the wire and then activated (Figure 2B). Small careful forward and backward passages were slowly performed twice. Repeated aspiration resulted in good flow without significant stenosis (Figure 2C). The patient tolerated the procedure well. Postoperatively, the patient was started on low molecular weight heparin. His pain was relieved, blood pressure had returned to normal, but there was worsening of renal parameters on the second day. His serum creatinine reached 118.9 μmol/L (59-103 μmol/L). Three days later, his renal function improved with an increase in urine output, and his serum creatinine was 112.8 μmol/L (59-103 μmol/L). Renal artery color Doppler ultrasound confirmed complete patency of the right renal artery. He was discharged on rivaroxaban and aspirin.
After 2 mo, the patient’s serum creatinine had dropped to 95.2 μmol/L (59-103 μmol/L). Renal dynamic imaging showed that his right kidney function had recovered slightly. The GFR in the left kidney was 70.5 mL/min, and 25.0 mL/min in the right kidney.
RAT is relatively rare, often manifested by renal infarction, and may be life-threatening. The results of an autopsy study showed that the incidence rate was 14/1000 people. Renal infarction is a rare condition, with an estimated incidence in the Emergency Department of 0.004%[7]. RAT may be related to atrial fibrillation[4]. In addition, any renal artery damage caused by endovascular treatment or trauma may also lead to thrombosis, and RAT may also occur as a result of renal artery stenosis. There are also many patients with idiopathic renal artery thrombosis[8]. Our patient had a history of arrhythmia and elevated protein C levels, which may have caused RAT.
Clinical manifestations of RAT include acute onset of flank pain or lower back pain, and hematuria without signs of peritonitis[4]. The diagnosis of renal artery thrombosis is often delayed or missed due to both the rarity of the disease and its non-specific clinical presentation, and has become a diagnostic challenge in the Emergency Department. There are reports that serum LDH sensitivity can reach approximately 90%, but the specificity is poor. Therefore, a low LDH level can be used as a marker to rule out acute RAT[1,9]. An unenhanced CT scan can rule out urolithiasis, but renal artery thrombosis may be missed as in our patient. A contrast-enhanced CT scan allows a definite diagnosis of RAT and can evaluate the range of the thrombus[1,10].
Currently, there are no guidelines on the treatment of RAT. Several options have been reported such as systemic anticoagulation, percutaneous interventional therapy, and surgery[2,9]. The use of anticoagulant agents as the sole therapy has often been insufficient to alleviate symptoms and renal dysfunction resulting from renal infarcts. Endovascular treatment includes local intra-arterial thrombolysis, catheter aspiration, balloon dilatation, and stent placement[4,6,9]. The purpose of these treatments is to restore the blood supply to the ischemic kidney as soon as possible, thereby preventing the loss of renal function and the development of hypertension. In general, the period from the onset of symptoms to the onset of irreversible renal injury is 3 h[11]. However, because the diagnosis is difficult, and treatments such as anticoagulation and local intra-arterial thrombolysis take a long time, most patients cannot restore the blood supply to the kidneys during this period. However, case reports have described the recovery of kidney function after a long occlusion period of even weeks. In another case, renal artery stenting was performed 1 wk after acute renal artery occlusion, and recovery of renal function was also observed[6]. Our patient was treated 20 d after the onset of symptoms, and the creatinine level rose briefly after treatment. However, renal function of the affected side also recovered slightly after 2 mo, indicating that revascularization for subacute RAT may have the potential to reverse recalcitrant conditions. There are also reports which show unsuccessful outcome after renal artery revascularization following a prolonged period of ischemia[2,12]. In addition to the duration of ischemia, the prognosis may also depend on collaterals from the lumbar, suprarenal, and ureteral vessels, and the degree of obstruction, as subtotal obstruction results in hibernation of renal parenchyma[4,13]. PMT represents a minimally invasive option for rapid recanalization of the target artery. Manual suction thrombectomy has been used in the treatment of RAT, but the thrombus may not be removed completely and there is also the risk of damaging the renal artery[9].
The Rotarex system is one of the PMT devices, and has been widely used in thrombotic diseases of lower limb arteries and is sometimes used in superior mesenteric artery thrombosis[14,15]. This rotational thrombectomy is capable of precluding and replacing thrombolysis, and may be an effective and safe modality for restoring blood supply to the target kidney faster. Local catheter-based intra-arterial thrombolysis may require a longer treatment period. At the same time, because of the angle between the renal artery and aorta, it is difficult to maintain the catheter in the proper position during the entire process. Despite the good technical and clinical success rates in our report, long-term follow-up and more studies are needed to verify the effectiveness and safety of this treatment.
This is the first time that the Rotarex mechanical thrombectomy catheter has been used to treat RAT. Our case confirmed that the Rotarex system is a safe device for rapid recanalization of the renal artery in patients with RAT, and may be a treatment option for RAT in the future.
| 1. | Mesiano P, Rollino C, Beltrame G, Ferro M, Quattrocchio G, Fenoglio R, Pozzato M, Cecere P, Forneris G, Bazzan M, Macchia G, Roccatello D. Acute renal infarction: a single center experience. J Nephrol. 2017;30:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 2. | Silverberg D, Menes T, Rimon U, Salomon O, Halak M. Acute renal artery occlusion: Presentation, treatment, and outcome. J Vasc Surg. 2016;64:1026-1032. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 48] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Oh YK, Yang CW, Kim YL, Kang SW, Park CW, Kim YS, Lee EY, Han BG, Lee SH, Kim SH, Lee H, Lim CS. Clinical Characteristics and Outcomes of Renal Infarction. Am J Kidney Dis. 2016;67:243-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 81] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Ganju N, Sondhi S, Kandoria A. Acute renal artery embolisation: role of local catheter-based intra-arterial thrombolysis. BMJ Case Rep. 2018;2018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Wright MP, Persad RA, Cranston DW. Renal artery occlusion. BJU Int. 2001;87:9-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Gao Y, Miserlis D, Longo GM, Garg N. Renal salvage using stent graft placement after acute renal artery occlusion with prolonged ischemic time. JRSM Cardiovasc Dis. 2020;9:2048004020940520. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Hoxie HJ, Coggin CB. Renal infarction: statistical study of two hundred and five cases and detailed report of an unusual case. Arch Intern Med (Chic). 1940;65:587-594. [RCA] [DOI] [Full Text] [Cited by in Crossref: 150] [Cited by in RCA: 151] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Inaba A, Karim M. Postoperative renal artery thrombosis. Clin Exp Nephrol. 2014;18:676-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Wang J, Zhang Y, Sun YM, Zhou Y. Successful catheter aspiration and local low-dose thrombolysis in an acute renal artery embolism. Cardiovasc Revasc Med. 2013;14:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 10. | Singh S, Wang L, Yao QS, Jyotimallika J, Singh S. Spontaneous renal artery thrombosis: an unusual cause of acute abdomen. N Am J Med Sci. 2014;6:234-236. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Blum U, Billmann P, Krause T, Gabelmann A, Keller E, Moser E, Langer M. Effect of local low-dose thrombolysis on clinical outcome in acute embolic renal artery occlusion. Radiology. 1993;189:549-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 56] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Fallahzadeh MK, Yatavelli RK, Kumar A, Singh N. Acute transplant renal artery thrombosis due to distal renal artery stenosis: A case report and review of the literature. J Nephropathol. 2014;3:105-108. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | Ouriel K, Andrus CH, Ricotta JJ, DeWeese JA, Green RM. Acute renal artery occlusion: when is revascularization justified? J Vasc Surg. 1987;5:348-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Zhang Z, Chen X, Li C, Feng H, Yu H, Zhu R. Percutaneous Mechanical Thrombectomy for Acute Superior Mesenteric Artery Embolism: Preliminary Experience in Five Cases. Ann Vasc Surg. 2020;63:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Freitas B, Steiner S, Bausback Y, Branzan D, Ülrich M, Bräunlich S, Schmidt A, Scheinert D. Rotarex Mechanical Debulking in Acute and Subacute Arterial Lesions. Angiology. 2017;68:233-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ennab RM S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Liu JH