Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8249
Peer-review started: May 12, 2021
First decision: June 15, 2021
Revised: June 29, 2021
Accepted: August 2, 2021
Article in press: August 2, 2021
Published online: September 26, 2021
Processing time: 126 Days and 17.4 Hours
Granulomatous lobular mastitis (GLM) is a type of benign chronic inflammatory disease that poses therapeutic challenges to healthcare providers. The diagnosis of GLM relies on tissue biopsy, and incorrect treatment may lead to delayed diagnosis, considerable aesthetic damage, and even mastectomy.
We report the case of a 37-year-old Chinese woman who was lactating and had GLM in both breasts. At the time of treatment, the right breast had a mass of approximately 15 cm × 11 cm, which was hard and had poor mobility. Multiple skin ulcerations and pus spills were also observed on the surface of the breast. The left breast had a mass of about 13 cm × 9 cm, which was hard and had poor mobility.
Herein, we report a case of bilateral GLM in a lactating woman that was successfully treated with traditional Chinese medicine (TCM), without the requirement for surgery or other treatments. Therefore, TCM may have advantages in the nonsurgical treatment of GLM.
Core Tip: The treatment of granulomatous lobular mastitis (GLM) with traditional Chinese medicine (TCM) combined with external treatment has a significant positive effect coupled with a low recurrence rate. Thus, TCM is considered an appropriate treatment modality for the majority of patients with GLM and can also protect the appearance of the breast.
- Citation: Li ZY, Sun XM, Li JW, Liu XF, Sun ZY, Chen HH, Dong YL, Sun XH. Treatment of bilateral granulomatous lobular mastitis during lactation with traditional Chinese medicine: A case report. World J Clin Cases 2021; 9(27): 8249-8259
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8249.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8249
Granulomatous lobular mastitis (GLM) is a non-caseous necrosis that is limited to the breast lobules. Granulomas are the main pathological characteristics of benign chronic inflammatory disease[1]. Kessler and Wollochm[2] reported GLM for the first time in 1972, and the incidence rate has increased year by year[3]. Associated clinical findings have included erythema, edema, draining sinus, pain, and ulceration[4]. The pathogenesis of GLM is currently unclear, and both modern medical research and traditional Chinese medicine (TCM) have formed a phenomenon of "a hundred schools of thought contend" about the etiology, pathogenesis, and clinical therapy associated with GLM.
At present, there is no gold standard for the management and treatment of GLM, but current treatment methods include conservative treatment based on TCM. It should be noted that in China, TCM may have advantages in the nonsurgical treatment of GLM[5], as well as steroids, surgical interventions, or immunosuppressive therapies (such as methotrexate). Simple incision, drainage, and antibiotic treatment have also been used in the treatment of GLM, but the effect remains controversial. Given that the pathogenesis of GLM is unclear, and the treatment methods are not unified, side effects of drug therapy are common and mastectomies are often performed unnecessarily. Furthermore, recurrence after mastectomy has still been reported despite these extensive interventions[6], making GLM a difficult disease to treat in the field of Western medicine. However, the treatment of GLM with TCM combined with external treatment has a significant positive effect coupled with a low recurrence rate. Thus, TCM is considered an appropriate treatment modality for the majority of patients with GLM and can also protect the appearance of the breast.
Herein, we report a case of bilateral GLM in a lactating woman that was successfully treated with TCM without the requirement for surgery or other treat
The patient started to complain of symptoms about 20 d postpartum with her second child. The right breast mass was found during lactation and was accompanied by local skin redness and swelling. Three needle punctures were performed in the outpatient department of a local hospital, all of which showed pus, and did not significantly relieve swelling. Therefore, the patient was subsequently admitted to the local hospital on January 5, 2019 for treatment.
The patient was a 37-year-old Chinese woman who initially presented with a firm mass on her right breast, which had enlarged and become painful over a 5-mo period, and a left breast mass, which had persisted for more than 1 mo. The patient showed no erythema, fever, or other discomforts since the onset of the disease.
The patient had a free previous medical history.
The patient had no history of smoking and drinking and had a history of two cesarean sections without complications.
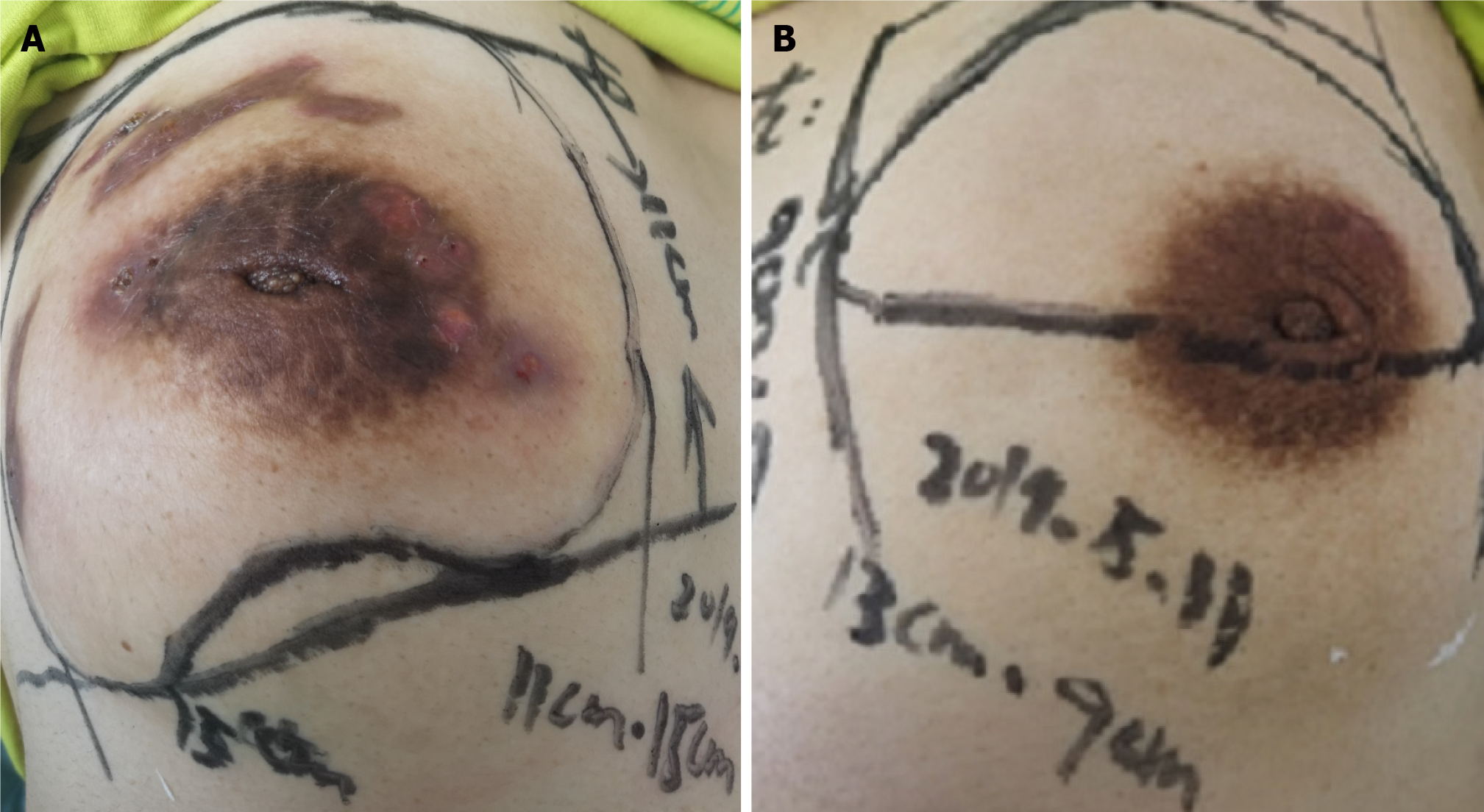
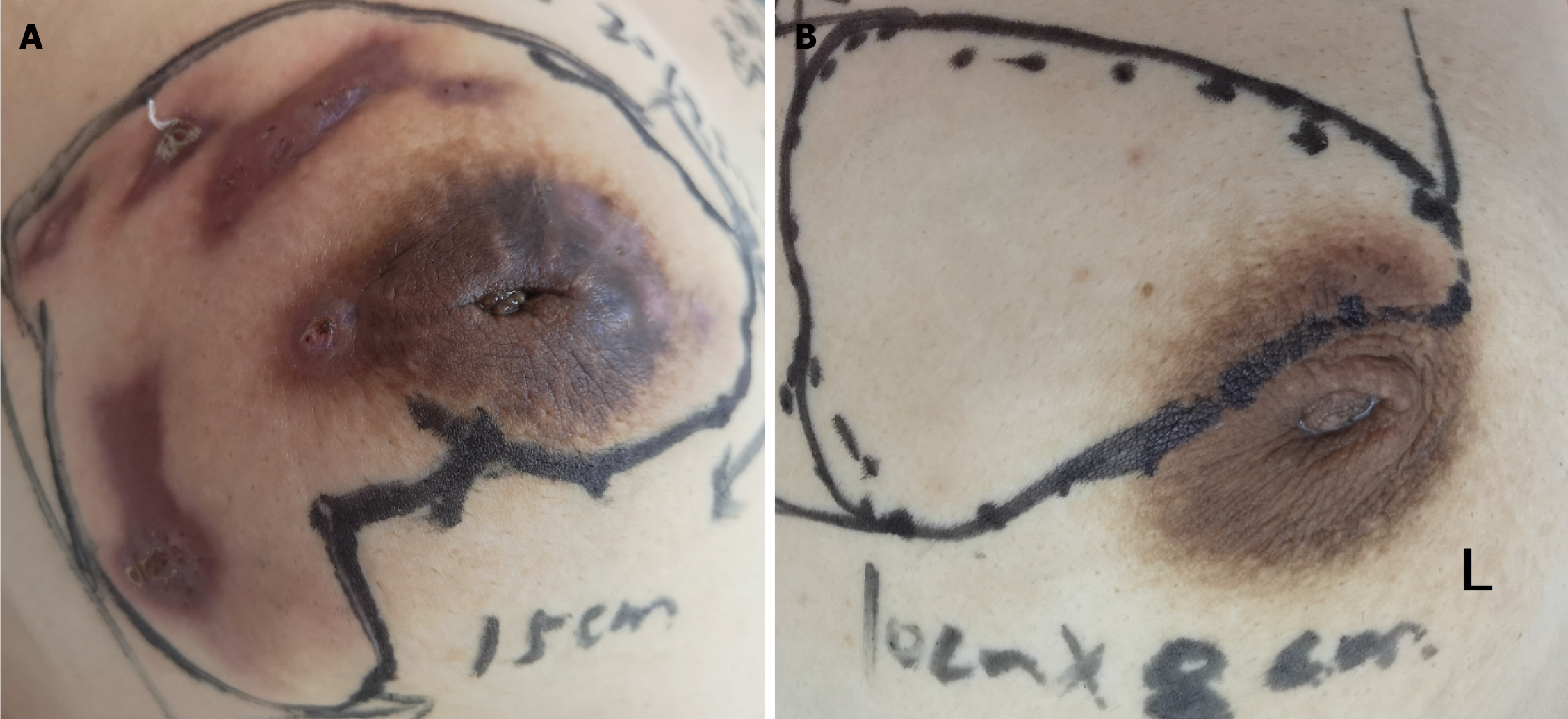
The right breast had a mass that was approximately 15 cm × 11 cm, and the left breast had a mass of 13 cm × 9 cm in size (Table 1). The masses were both homogeneous and hard with poor mobility. Multiple skin ulcerations were present on the right breast surface, and pus was observed. Both nipples were sunken (Figure 1), and the right armpit had swollen lymph nodes. No erythema nodules were found in the lower limbs.
| Geographical parameters of the masses | |
| The right breast | 15 cm × 11 cm |
| The left breast | 13 cm × 9 cm |
Laboratory serum antibody tests were positive for M. tuberculosis [immunoglobulin (Ig) G], and anti-tuberculosis drugs were subsequently administered. However, anti-tuberculosis treatment (oral isoniazid, rifampicin, and ethambutol, once a day) was not effective for 3.5 mo. Furthermore, routine blood and biochemical examinations were normal.
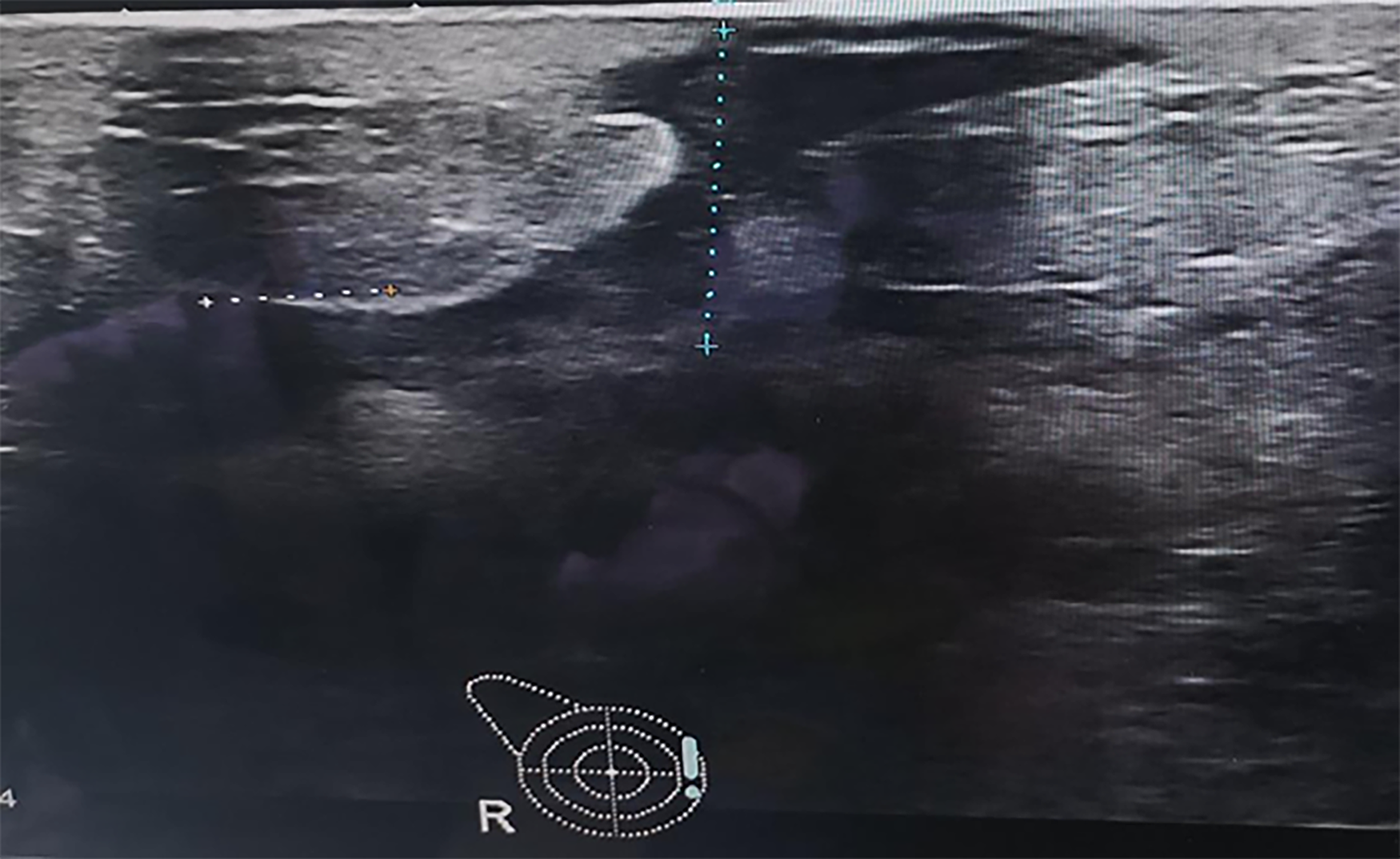
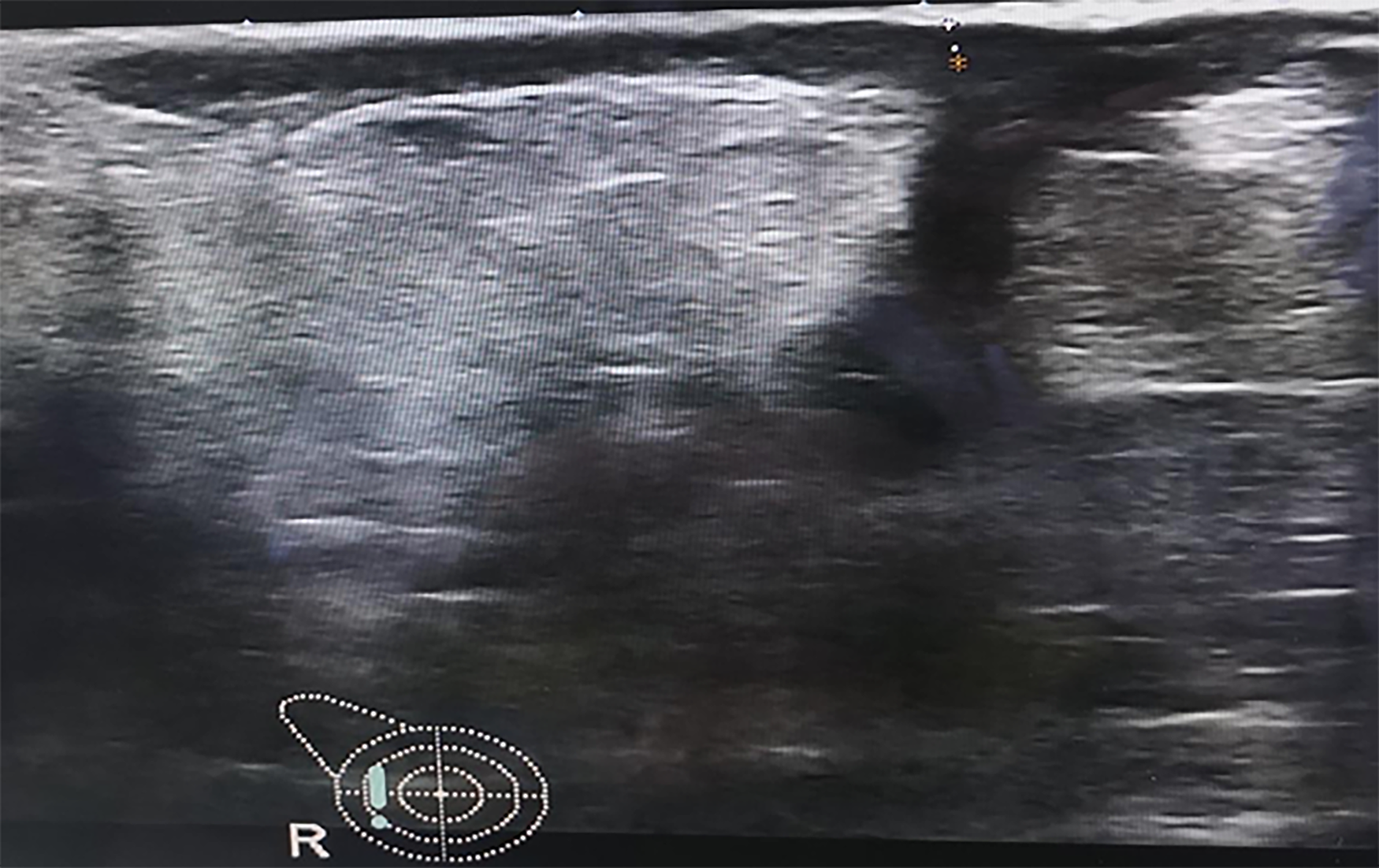
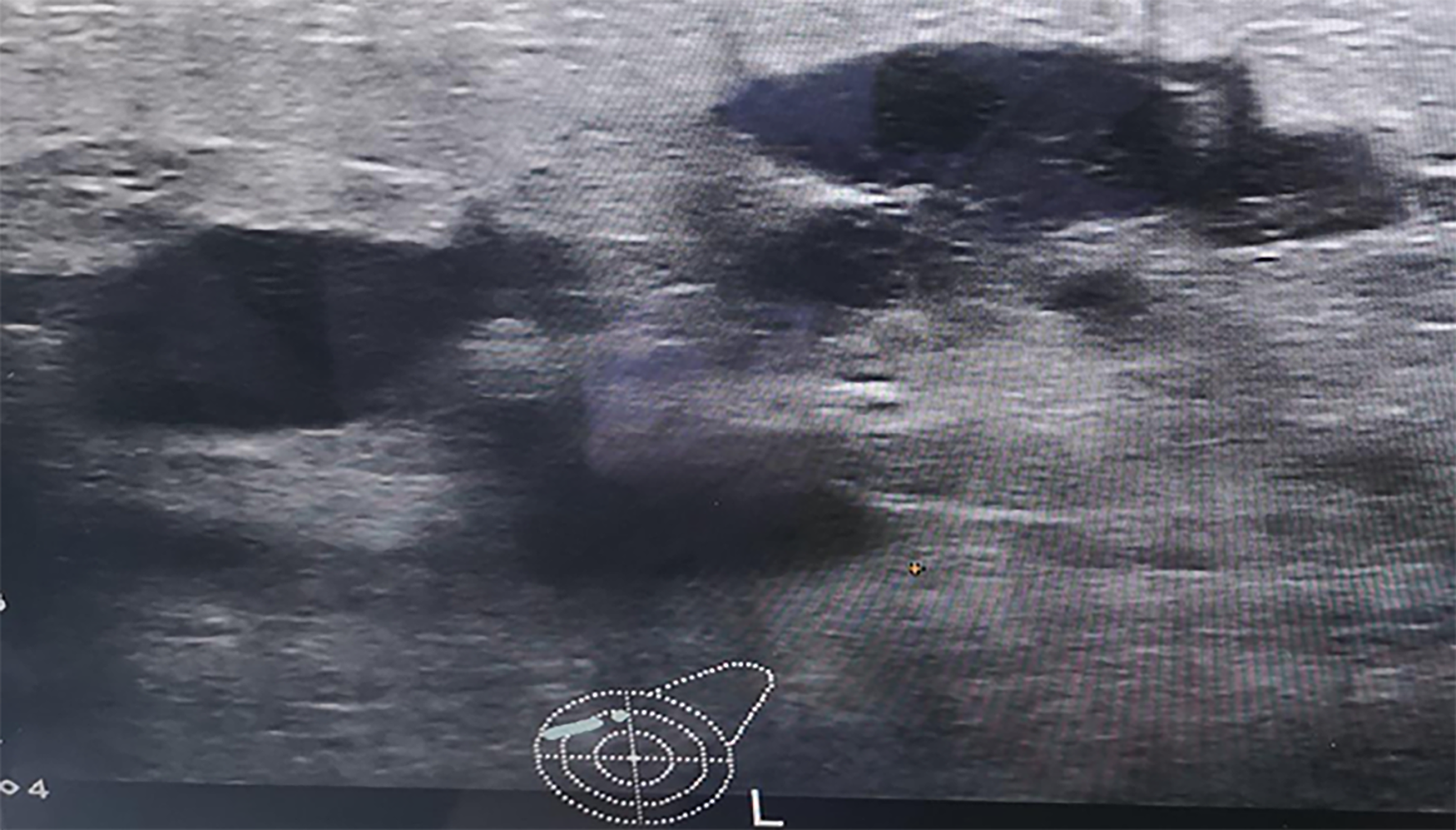
Ultrasound showed the lactating breasts (self-reported stop for 20 d). The right breast was shown to comprise masses and nodules, suggesting suppurative inflammation, and the right axillary lymph nodes were slightly larger.
A plain computed tomography scan of the lungs (January 5, 2019) showed multiple nodules in bilateral lungs. In addition, fatty liver and low-density nodules in the right breast area were noted.
On May 11, 2019, color Doppler ultrasound showed that multiple ducts in the body and fat layers of the double mammary glands expanded to form an irregular liquid dark area, and the bilateral axillary lymph nodes were slightly larger. Ultrasonography showed ill-defined, hypoechoic, heterogeneous lesions, with specific signs, including the ‘funnel sign,’ ‘tunnel sign,’ and ‘quicksand sign’, which were accom
On January 8, 2019, a core biopsy of the breast (right breast puncture) showed granulomatous inflammation, which suggested GLM was considered (pathology report number: 201900613). The immune results on May 27, 2019 were as follows: CD3+CD8+: 31.77 (20.74-29.42); CD3+: 78.39↑ (64.19–75.77); CD4/CD8: 1.25 (normal range). Six tests of female sex hormones were normal. A core biopsy of the left breast also showed granulomatous inflammation, which suggested GLM (pathology report number: 201928549).
The final diagnosis of the presented case was bilateral GLM.
Total mastectomy and breast reconstructive surgery were offered to the patient by the local hospital, but she rejected this proposal because of her circumstances and financial situation.
The patient attended our outpatient clinic to seek further treatment. At that time, her symptoms comprised dull pain in both breasts and broken skin on the right breast surface. She is usually impatient and likes spicy food. She denied taking health care products and had a regular menstrual cycle. She had no history of smoking and drinking and had a history of two cesarean sections without complications.
The Western medicine diagnosis was GLM, while the TCM diagnosis was mastitis (liver depression, spleen deficiency, Qi depression, and phlegm coagulation). The treatment principle was soothing the liver and strengthening the spleen, in addition to regulating the flow of Qi to eliminate phlegm. The patient was prescribed with the following: Bupleurum (12 g), yujin (12 g), xiangfu (9 g), paeony (9 g), angelica (12 g), hedyotis (30 g), hawthorn (18 g), danshen (30 g), venison (18 g), tea root (30 g), anemone (9 g), polygonum cuspidatum (15 g), yinchen (9 g), prunella (18 g), viola (12 g), saponatum (12 g), platycodon (9 g), gancao (6 g), astragalus (30 g), magnolia (9 g), pinellia ternary (9 g), chenpi (9 g), scutellaria (12 g), and yuanzhi (20 g). The aforementioned components were decocted in water and prescribed as one dose per day, 14 doses in total. In addition, the patient was instructed to apply Daqing cream (self-made in hospital) for external use. The cream was applied to the right and left breast lumps using gauze, and this was repeated every day. The patient was instructed to avoid fried and spicy food during the treatment, eat more fresh fruit and vegetables, maintain a low level of stress, and frequently clean the sunken nipples.
On May 30, 2019, after 14 d of continuous administration Chinese medicine, the mass was reduced to 10 cm × 6 cm in the right breast and 10 cm × 8 cm in the left breast, and the texture was softer than before treatment (Figure 5). On May 11, 2019, the prescription was amended to additionally include dangshen (12 g), atractylodes (12 g), macrocephala (12 g), and Poria cocos (12 g), for a total of 28 doses. Topical drugs continued to be used.
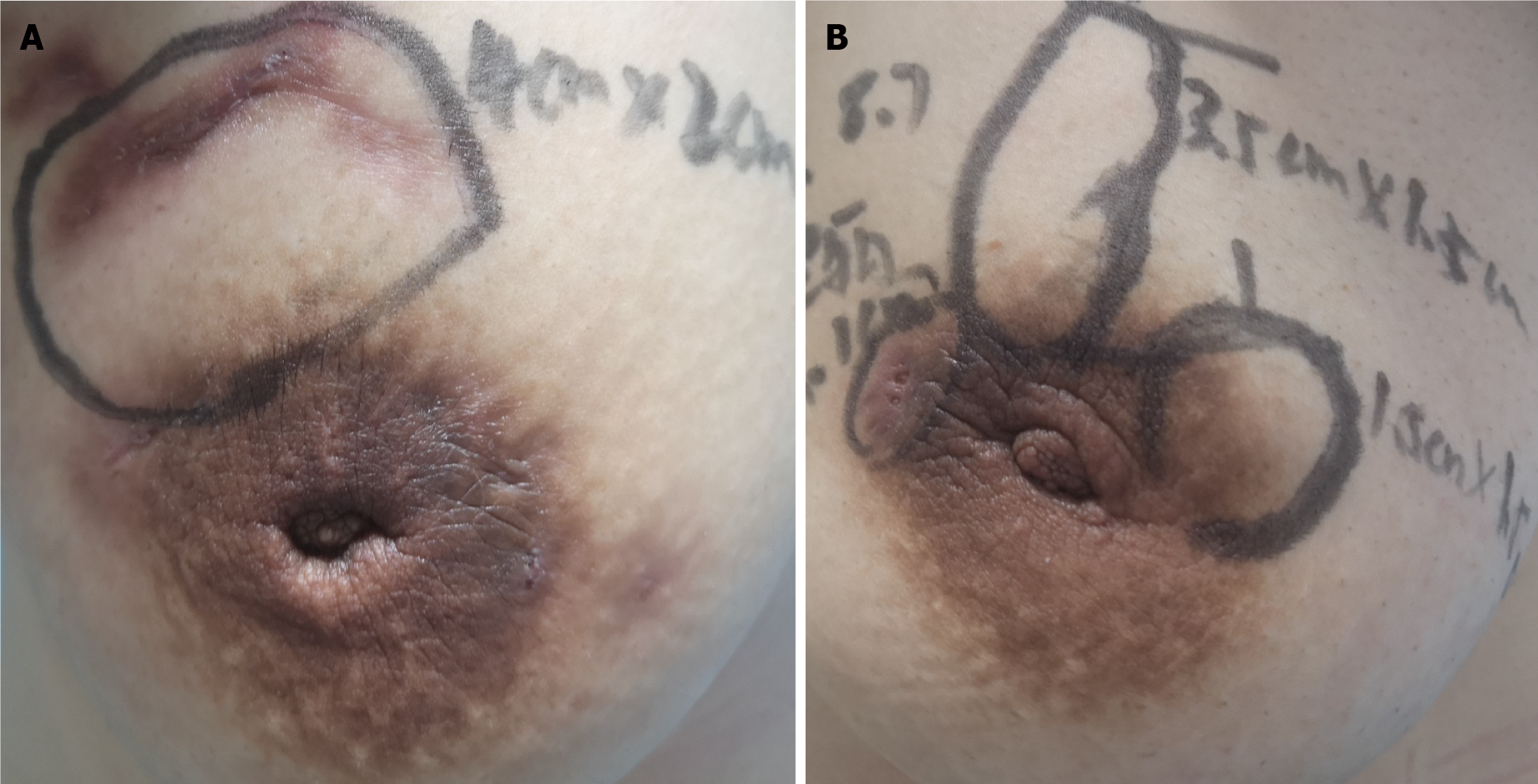
On August 7, 2019, after 2 mo of administration, the local mass was significantly reduced (approximately 4 cm × 2 cm in the right breast and 1.5 cm × 1.5 cm in the left breast). Some purulent exudation was apparent (Figure 6). The prescriptions are as follows: Dangshen (12 g), baizhu (12 g), fuling (12 g), liquorice (6 g), platycodon (9 g), scutellaria (12 g), gardenia (9 g), bupleurum (12 g), yujin (12 g), xiangfu (9 g), angelica (12 g), shengdi (9 g), baishao (12 g), chuanxiong (9 g), prunella vulgaris (20 g), zedoary (12 g), huzhang (18 g), angelica (9 g), chenpi (12 g), hawthorn (18 g), danshen (30 g), pangolin (3 g), yinchen (9 g), and lotus leaves (20 g). Topical drugs continued to be used.
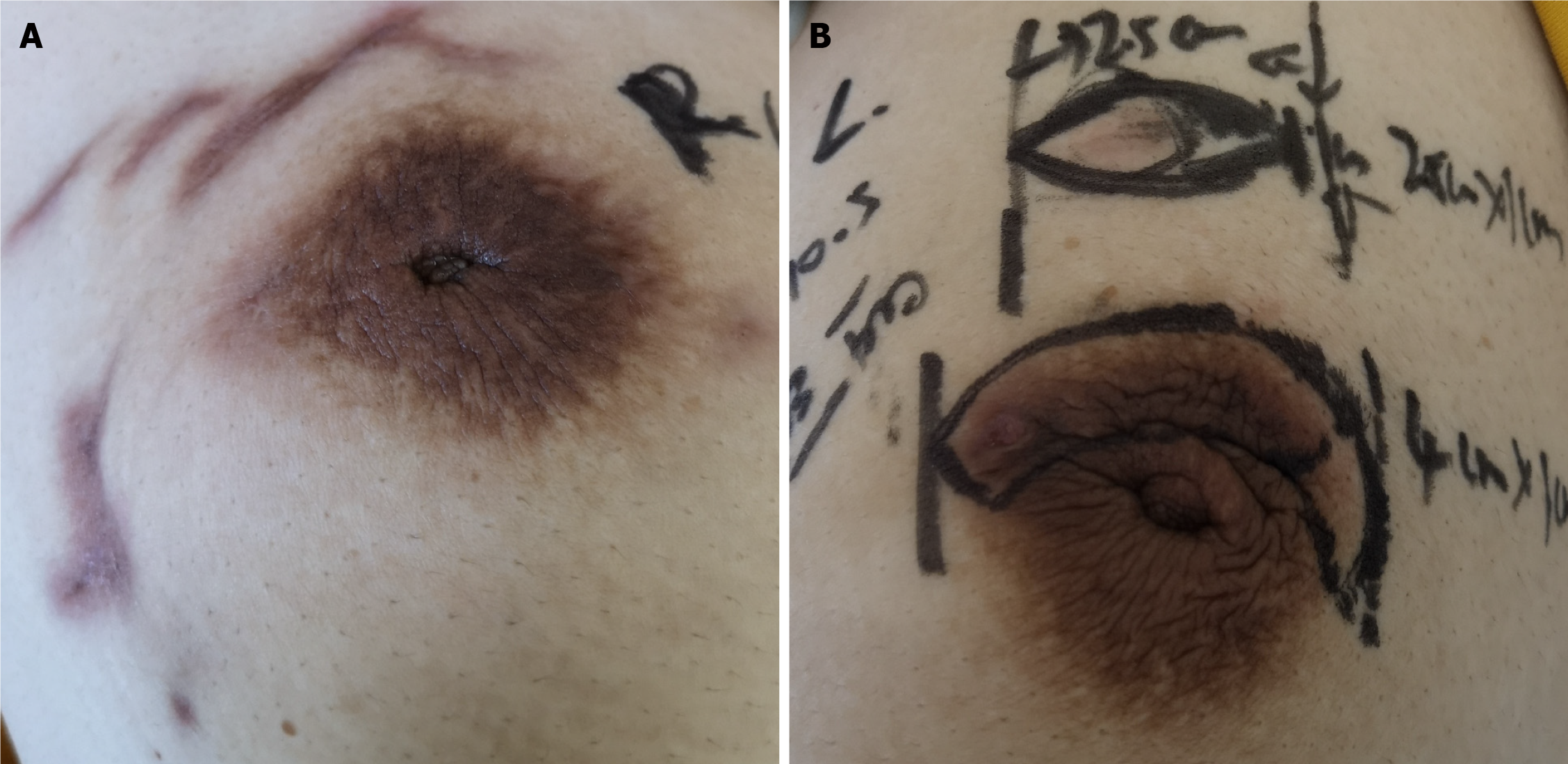
On October 5, 2019, the right breast was not palpable, the left breast local mass was reduced to 2.5 cm × 1.0 cm, and the breach was healed (Figure 7). The prescription was as follows: Dangshen (12 g), baizhu (12 g), poria (12 g), liquorice (6 g), platycodon (9 g), astragalus (30 g), bupleurum (12 g), yujin (9 g), xiangfu (9 g), angelica (9 g), white peony (9 g), chenpi (9 g), jiangbanxia (9 g), zaojiaoci (9 g), hopu (12 g), shengdi (9 g), chuanxiong (9 g), luhancao (9 g), staghorn cream (6 g), anemone (9 g), ate buttercup root (9 g), stir-fried malt (20 g), danshen (20 g).
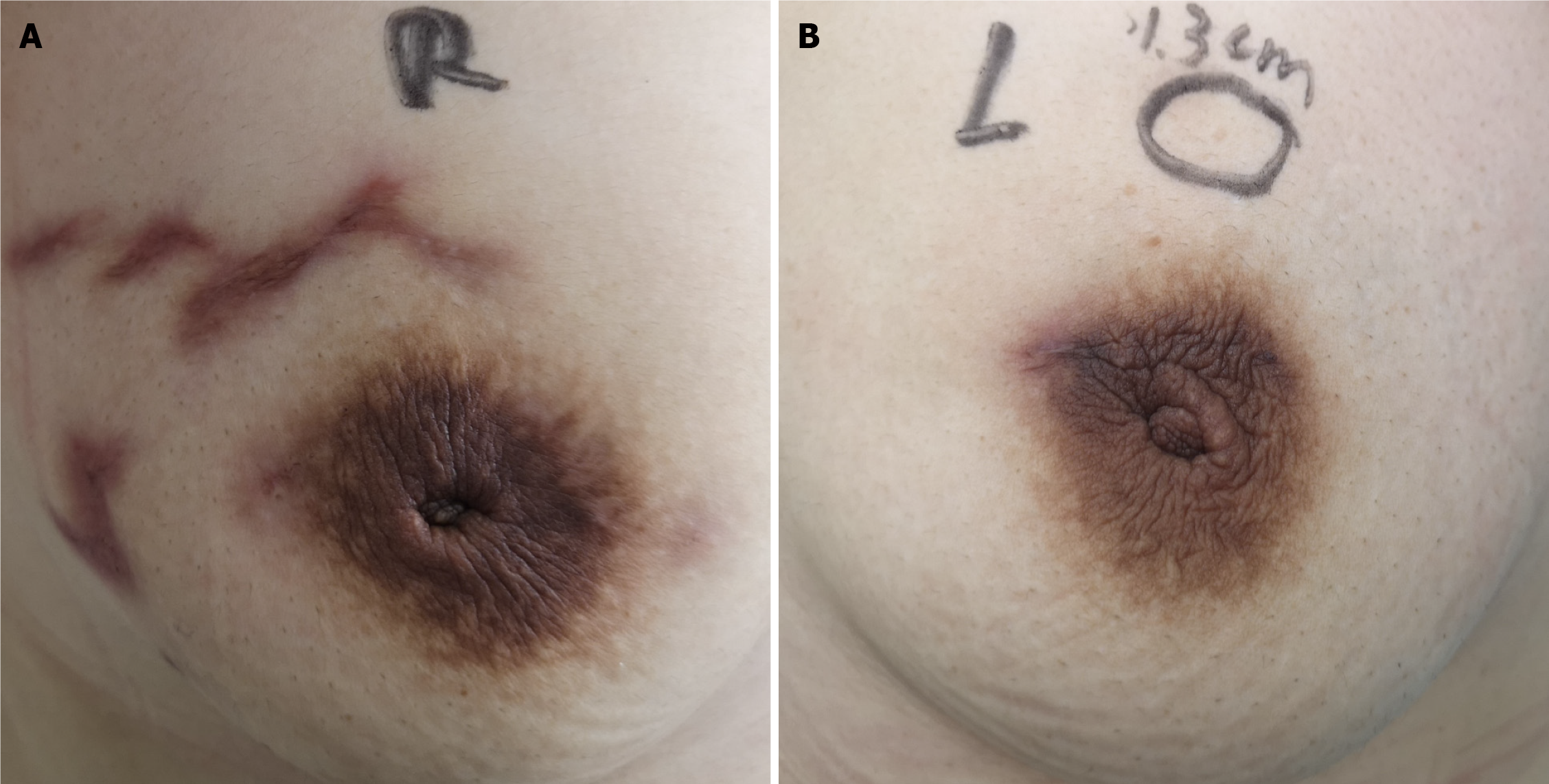
On November 23, 2019, the local mass in the left breast was reduced to 1.3 cm and the breach was completely healed (Figure 8). The patient insisted on taking the Chinese medicine again to consolidate the curative effect; thus, the whole prescription was as follows: On October 5, the saponifia and eaten buttercup root were removed, adding Angelica dahurica (9 g) and Fritillaria thunbergii (9 g). By January 2020, no mass was palpable in the breasts (Figure 9). B-ultrasonic examination showed that the thickness of the breasts was normal, the mammary ducts were normal, the breasts were hyperplastic, and there were no enlarged lymph nodes in the axilla.
The patient stopped taking medicine 1 mo after the treatment was initiated, and she was subsequently followed on April 12, 2020. The patient had no discomfort in the bilateral mammary glands, and no abnormality was found in the ultrasound reexamination.
GLM is a chronic inflammatory disease characterized by non-caseous necrosis and granuloma formation in breast lobules. While it has been reported that the disease most commonly occurs in the non-lactation period, there are an increasing number of cases of GLM in the lactation period in clinical practice; however, whether GLM belongs to non-lactation granulomatous mastitis remains to be discussed. The current case of GLM was first found on the 20th day of lactation, considering granulomatous mastitis associated with galactosis. Brown and Tang[7] proposed that GLM may be an immune phenomenon induced by the local stimulation of milk, and therefore applied the name of "post-lactation granulomatous mastitis".
In the current case, the levels of inflammatory cells such as leukocytes were not high, and no bacteria were found in the pus culture; thus, the anti-inflammatory treatment was ineffective. Besides, the patient used anti-tuberculosis treatment for more than 3 mo for the treatment of right mammary granulomatous mastitis. However, the right breast mass and damage were not reduced as a result of the treatment, and the left granulomatous mastitis was also complicated; thus, the anti-tuberculosis treatment was discontinued. The results of the needle puncture ruled out tuberculous mastitis, and the anti-tuberculosis drug treatment was ineffective, which was inconsistent with some clinical reports that anti-tuberculosis drugs were effective in treating GLM[8]. Thus, large sample case observations are necessary in the future to further understand this finding. Some scholars[9] speculated that GLM is an underestimated diagnosis of breast tuberculosis; nevertheless, the possibility of breast tuberculosis should be completely excluded before diagnosis. Although anti-tuberculosis drugs are effective for some patients, evidence for the efficacy of these drugs is lacking. The increase in CD3+ and CD3+CD8+ T lymphocytes suggests that the disease may be related to immunity. A number of domestic studies have confirmed that non-lactational mastitis patients exhibit different degrees of immune dysfunction. Chen et al[10] reported that the percentages of CD3 and CD4/CD8 cells in each subgroup of T cells were increased, as were the levels of IgG, IgA, and C4, while complement C3 was decreased[10]. Xia et al[11] believed that about 50% of the patients showed abnormalities in various subsets of T lymphocytes, which were mainly decreased[11].
At present, the side effects of antibiotic treatment, including those of hormones, are considerable, and there remains a high recurrence rate. Surgery often causes great damage to the patients' body and has a high cost and serious impact on aesthetics, and the patients' acceptance rate is low. However, TCM is often effective in the treatment of GLM, and many Chinese herbal medicines have shown enhanced therapeutic effects.
According to its clinical symptoms and signs, modern medical experts classify GLM as “mastitis” and “galactorrhea”. The protracted period is the most complicated and refractory to the disease, and is characterized by the coexistence of rigidity, abscesses, ulcers, and sinus tract. The rigidity does not need to become pus or a small amount of pus, which will not heal for a long time and form sinus tract[12]. GLM occurs in the breast; the nipple belongs to the circulation of the liver channel, and the breast belongs to the circulation of the stomach channel. The liver likes to be organized but dislikes depression, while the female is more depressed, which makes the liver stagnant and Qi stagnant, and the depression turns into fire for a long time. If the liver Qi is not sparse, it is easy to take advantage of the spleen soil, causing the spleen to lose its healthy function, phlegm, and blood stasis, subsequently blocking the milk collaterals and agglomerating, such that the disease is often lingering and hard to heal.
In the current case, the breasts were stiff at the initial diagnosis, which led to the delay in diagnosing granulomatous mastitis. The syndrome was liver depression, spleen deficiency, Qi stagnation, and phlegm coagulation. Treatment methods were selected on the basis of their ability to soothe the liver and spleen and regulate the flow of Qi to eliminate phlegm and promote the dissipation of the mass. This prescription is based on the TCM theory that “the breast belongs to the stomach, and the nipple belongs to the liver". From the theory of TCM, the disease is more common in the peripheral quadrant of the breast, often involving the nipple areola, which is related to the meridian circulation. Furthermore, the lung is the organ responsible for storing phlegm, and the spleen is the source of phlegm; both are closely related to the generation of phlegm evil. The disease is closely related to phlegm and fire. Due to the disunity of TCM syndrome differentiation, GLM is considered closely related to the four meridians of the spleen, stomach, liver, and lungs, and is mainly caused by pathological factors, such as phlegm and fire. The main aim of GLM treatment is to soothe the liver, relieve depression, and disperse the phlegm.
Chinese herbs are usually prescribed as formulas guided by TCM theory, often combining multiple herbs in a prescription[13]. Therefore, it is rational to use herbal components in the same principle. Regarding GLM, the prescription is given to soothe and soften the liver and regulate the Qi with the four flavors of bupleurum, xiangfu, yujin, and paeony. Furthermore, the three herbs dangshen, baizhu, and fuling in the sijunzi decoction are taken to invigorate the spleen and remove dampness from the stomach, which can obstruct the phlegm, hinder the body's movement and transformation, and agglomerate into lumps. GLM is mainly manifested by lumps. Prunella vulgaris and Fritillaria thunbergia can directly reach the breast lesions. Moreover, women often suffer from anxiety and sleep problems due to long-term pain during illness. To this end, a small amount of polygala is used to calm the nerves and heart, and licorice is used to mix the various drugs. Together with the external application of daqinggao, this combination can reduce heat and swelling, and subsequently close the ulceration and remove the mass.
Commonly, if the local skin is red and swollen and heat is obvious on imaging, dandelion (30 g), Polygonum cuspidatum (12 g), anemone (9 g), Hedyotis diffusa willd (30 g), and melon wilt (15 g) can be added to enhance the effect of heat-clearing and detumescence.
If the mass is hard and cannot be dissipated, or in the event that the hard and purulent nature is not obvious, trigonometry (12 g), zedoary turmeric (9 g), cinnamon (3 g), antler cream (6 g), gleditsia (9 g), and pangolin (6 g) can be used to activate blood circulation, remove stasis, eliminate phlegm, and soften the indurated mass.
In the event that the wound surface heals slowly and the secretion is thin after ulceration or incision and drainage, Astragalus (30 g), angelica (12 g), and Salvia miltiorrhiza (20 g) can be added to strengthen the body resistance.
Chinese herbs have a long history of clinical use, and thousands of years of clinical experience provides clues for pharmacological studies. In modern pharmacology research on the main components of Chinese herbal compounds, Song et al[14] found that bupleurum extract can improve depression; its mechanism may be related to the antagonism of the 5-HT3R signaling pathway and the maintenance of intracellular calcium concentration at a steady level, which is closely related to the effect of bupleurum in relieving liver depression. Saikosaponin SS, an effective component of Bupleurum chinense, has anti-inflammatory and anti-exudation effects and can inhibit the release of inflammatory mediators and the growth of granulomas, as well as the ability to increase capillary permeability caused by histamine and 5-hydroxytryptamine[15]. At the same time, it can also significantly inhibit other inflammatory reactions, such as leukocyte migration and connective tissue proliferation. The anti-inflammatory effect of Bupleurum chinense is mainly related to stimulation of the adrenal gland, which subsequently promotes the synthesis of the adrenal cortex and the secretion of glucocorticoids[16].
The Compendium of Materia Medica describes Xiangfu as the general manager of Qi disease and the head of the gynecology department[17]. It is a commonly used medicine for relieving liver depression and Qi in blood. Modern pharmacological research indicates that Xiangfu has similar functions to antidepressants and lowers blood glucose and lipids, and has anti-inflammatory, anti-bacterial, and antitumor properties.
The main chemical components of curcumin are volatile oil and curcumin, which function to promote blood circulation, pain relief, Qi, and blood cooling, as well as to relieve depression and heat. Curcumin is commonly used in clinical compatibility with other drugs to treat cancer, protect the liver, reduce blood lipid levels, and inhibit bacteria for its anti-inflammatory properties[18].
Paeonia alba is a commonly used medicine for tonifying the blood and regulating menstruation. Modern research indicates that it has positive effects on depression, protects the liver, and has analgesic, anti-inflammatory, and antitumor properties[19].
Sijunzi decoction is an important Chinese medicine for nourishing Qi and blood, which consists of ginseng, Atractylodes macrocephala, Poria cocos, and baked licorice. Since ginseng is considered too valuable, it is often replaced by dangshen in clinical practice. Its main chemical components are saponins, flavonoids, and polysaccharides, and its pharmacological effects include regulating gastrointestinal function, improving body immunity, and anti-tumor, anti-fatigue, and anti-aging effects[20].
In conclusion, TCM has unique advantages in promoting wound healing, reducing granulation, and enhancing human immunity. Additionally, patient cooperation, emotional management, and diet regulation also play significant roles in disease healing. In the future, we hope to be able to refine the classification of patients according to their differences, explore the characteristics and trends of patients prone to bilateral breast disease, predict the disease, and treat the disease at the initial stage.
At present, there is no agreed treatment guideline for the diagnosis and treatment of GLM, and there is no high-level data evidence to support the selection of different treatment methods; thus, more in-depth research is required to provide a more robust clinical plan. Further research, especially randomized control studies with a larger sample size, should be conducted to explore optimal treatments for patients with different risk profiles.
| 1. | Lin Y, Zhu HY, Situ HL, Guan RD, Song X. Clinical practice of treating granulomatous mastitis with characteristic therapy of traditional Chinese medicine. Proceedings of the 12th National Academic Conference of traditional Chinese medicine and integrated Chinese and Western Medicine on breast diseases; 2011 Oct 28; Beijing, China. Beijing: CNKI, 2011: 184-188. |
| 2. | Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol. 1972;58:642-646. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 393] [Cited by in RCA: 465] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 3. | Zhu LP, Jia WX, Ni D, Li YT, Wu T, Zhao Q. Clinical manifestations, X-ray and MRI diagnosis of granulomatous mastitis. J Clin Radiol. 2011;30:193-196. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Davis J, Cocco D, Matz S, Hsu CH, Brown MJ, Lee J, Bouton ME, Caruso DM, Komenaka IK. Re-evaluating if observation continues to be the best management of idiopathic granulomatous mastitis. Surgery. 2019;166:1176-1180. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Zhang C, Lei S, Kong C, Tan Y, Dai X, He J, Xiao Q, Huang S. Clinical study on surgical treatment of granulomatous lobular mastitis. Gland Surg. 2019;8:712-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 6. | Brennan ME, Morgan M, Heilat GB, Kanesalingam K. Granulomatous lobular mastitis: Clinical update and case study. Aust J Gen Pract. 2020;49:44-47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Brown KL, Tang PH. Postlactational tumoral granulomatous mastitis: a localized immune phenomenon. Am J Surg. 1979;138:326-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 59] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Rao NY, Wang L, Su FX, Jin L, Zeng YJ, Jia WJ, Li SR, Wu JN, Liu JQ, Song EW. Anti-tuberculosis treatment for idiopathic granulomatous mastitis mimicking breast cancer:a retrospective review of 36 cases. J Cancer Res Ther Oncol. 2014;2:1-6. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 9. | Sriram K, Moffatt D, Stapledon R. Tuberculosis infection of the breast mistaken for granulomatous mastitis: a case report. Cases J. 2008;1:273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Chen FF, Feng JM, Gao QQ, Qu WC, Wu XQ, Wan H. Non breast-feeding mastitis patient peripheral immune function test and its clinical significance. Waike Lilun Yu Shijian. 2015;20:252-254. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 11. | Xia YR, Chen HF, Ye MN, Chen LY, Bao YJ. Variations of T lymphocytes, immunoglobulin, and complements levels in peripheral blood of non-lacta. Zhonghua Ruxianbing Zazhi. 2012;5:504-514. [DOI] [Full Text] |
| 12. | Hu XM, Wang R, Liu S. Liu Sheng's experience in the treatment of acne mastitis. Liaoning Zhongyi Zazhi. 2016;43:716-717. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Hu B, Du Q, Shen K, Xu L. Principles and scientific basis of traditional Chinese medicine in cancer treatment. J Bioanal Biomed. 2012;6:2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 14. | Song CH, Ge QF, Zhang HY. Effect of Shuyu Capsule on Ca2+ of hippocampal neurons activated by 5-HT3R. Shandong Zhongyiyao Daxue Xuebao. 2014;38:263-265. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 15. | Li RG. Analysis of effective components and pharmacological actions of Bupleurum chinense. Shanxi Zhongyi. 2013;34:750-751. [DOI] [Full Text] |
| 16. | Shu WJ, Yao XL, Chen ZY, Zou R, Tang JM. Pharmacological research and clinical application of Bupleurum chinense. Guangxi Kexueyuan Xuebao. 2017;33:268-273. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Pan SB, Kong N, Li J, Wang X, Zhao J, Zhang YQ. Research progress on chemical constituents and pharmacological action of Cyperus japonicus. Zhongguo Xiandai Zhongyao. 2019;21:1429-1434. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 18. | Yuan XX, Yang MM, Zhao GQ. Research progress of chemical constituents and pharmacological action of Yujin. Chengde Yixueyuan Xuebao. 2016;33:487-489. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Ye XW, Xia LT, Ren HM, Deng YL, Yang M, Zhang JL, Chen X, Liu HP, Zhang Q. Research progress on processing history evolution, chemical constituents and pharmacological action of Paeoniae Radix Alba. Zhongcao Yao. 2020;51:1951-1969. [DOI] [Full Text] |
| 20. | Xiong S, Ding XC. Research progress of chemical composition and pharmacological action of Sijunzi Decoction. Shandong Yixueyuan Xuebao. 2017;39:371-374. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Li SC S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Wang LYT