Published online Sep 26, 2021. doi: 10.12998/wjcc.v9.i27.8214
Peer-review started: May 8, 2021
First decision: June 6, 2021
Revised: June 17, 2021
Accepted: July 5, 2021
Article in press: July 5, 2021
Published online: September 26, 2021
Processing time: 130 Days and 20.4 Hours
Walled-off necrosis (WON), as a local complication of acute necrotizing pancreatitis, is difficult to differentiate from pancreatic pseudocysts (PPC). Imaging modalities such as computed tomography show a lower accuracy than endoscopic ultrasound (EUS) in confirming the diagnosis. EUS-guided cystogastrostomy following direct endoscopic necrosectomy has achieved excellent results and has been regarded as a preferred alternative to traditional surgery. However, high-risk bleeding is one of the greatest concerns.
Two patients with symptomatic pancreatic fluid collections (PFCs) were admitted to our hospital for EUS-guided lumen-apposing metal stent therapy. The female patient suffered from intermittent abdominal pain and underwent two perioperative CT examinations. The male patient had recurrent pancreatitis and showed a growing PFC. The initial diagnosis was a PPC according to contrast-enhanced CT. However, the evidence of solid contents on EUS prompted revision of the diagnosis to WON. An endoscope was inserted into the cavity, and some necrotic debris and multiple hidden vascular structures were observed. Owing to conservative treatment by irrigation with sterile water instead of direct necrosectomy, we successfully avoided damaging hidden vessels and reduced the risk of intraoperative bleeding.
The application of EUS is helpful for the identification of PFCs. Careful intervention should be conducted for WON with multiple vessels to prevent bleeding.
Core Tip: Walled-off necrosis (WON) is difficult to differentiate from pancreatic pseudocysts in clinical practice. Imaging modalities such as computed tomography show a lower accuracy than endoscopic ultrasound (EUS) in confirming the diagnosis. With the worldwide application of electrocautery lumen-apposing metal stents, direct endoscopic necrosectomy has emerged as the most effective approach for treating WON. However, bleeding might be induced by direct damage. Here, we present two cases of WON in which the diagnosis was revised by intraoperative EUS and high-risk bleeding was successfully prevented.
- Citation: Xu N, Zhai YQ, Li LS, Chai NL. Multiple hidden vessels in walled-off necrosis with high-risk bleeding: Report of two cases. World J Clin Cases 2021; 9(27): 8214-8219
- URL: https://www.wjgnet.com/2307-8960/full/v9/i27/8214.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i27.8214
Walled-off necrosis (WON) and pancreatic pseudocysts (PPCs) are local complications of acute pancreatitis according to the updated Atlanta classification[1]. WON is defined as a partially liquefied collection containing solid luminal content, which could be used to differentiate it from PPCs on imaging, with an accuracy of 79.5%-83.6%[2]. Unfortunately, WON is frequently misdiagnosed as PPCs by radiologists. Bleeding is the most common complication of endoscopic drainage. The existence of a vessel within an area of WON, which might increase the risk of hemorrhage, has rarely been reported in the literature. The presence of multiple vessels multiplies the risk of vascular rupture. Herein, we present the cases of two patients who underwent direct endoscopic necrosectomy (DEN) with a novel lumen-apposing metal stent (LAMS) whose diagnoses were revised by intraoperative endoscopic ultrasound (EUS). In these cases, careful intervention prevented traumatic bleeding from multiple vessels.
Case 1: A 34-year-old woman with intermittent abdominal pain over 1 year was initially diagnosed with PPCs according to contrast-enhanced CT and admitted to our hospital on November 17, 2020.
Case 2: A 32-year-old man with recurrent pancreatitis was diagnosed with a growing pancreatic fluid collection (PFC) by CT and admitted to our hospital for further treatment on January 6, 2021.
Case 1: Contrast-enhanced abdominal CT showed a heterogeneous fluid collection in the peripancreatic area, with an approximate diameter of 11 cm, on October 22, 2019.
Case 2: The patient was initially diagnosed with a PPC at another hospital 4 mo prior and transferred to our hospital for EUS-guided LAMS therapy.
Case 1: The patient had a history of acute pancreatitis approximately 1 year prior.
Case 2: Five years prior, the patient suffered from pancreatitis for the first time.
Cases 1 and 2: The personal and family histories were unremarkable.
Case 1: The patient was suffering from intermittent abdominal pain on admission to our hospital. Upon physical examination, her temperature was 36.6 ℃, her respiratory rate was 22 breaths per minute, her blood pressure was 124/78 mmHg, and her pulse rate was 135 bpm. The other tests did not show obvious abnormal manifestations.
Case 2: The patient had mild abdominal pain. All vital signs were normal.
Case 1: No pancreatitis-related abnormalities were found by blood biochemical examination.
Case 2: A significant increase in the carbohydrate antigen 19-9 level was found by blood biochemical examination, as well as a slight increase in the carbohydrate antigen 125 level.
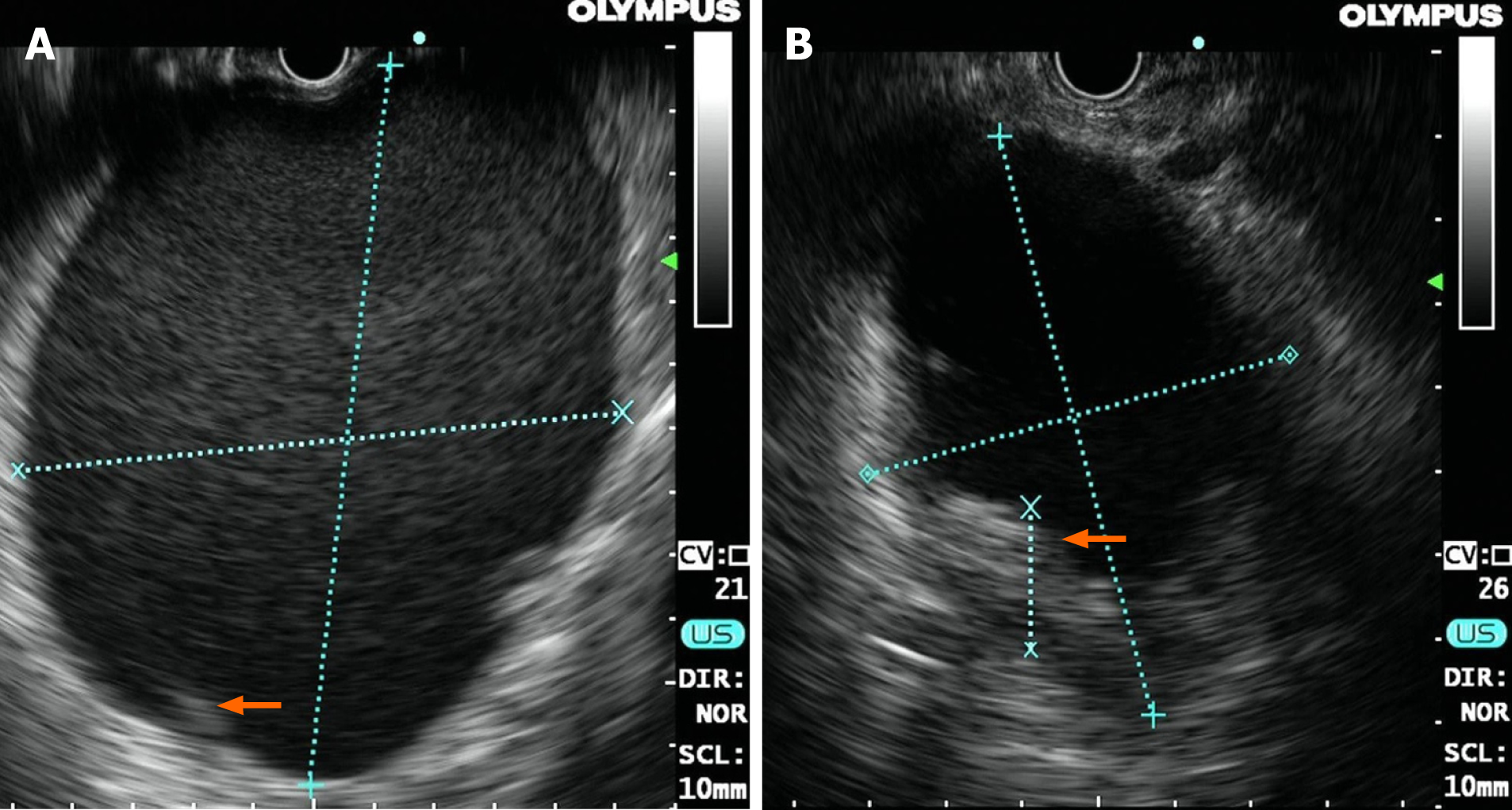
Case 1: Contrast-enhanced abdominal CT at our hospital still showed a heterogeneous fluid collection, with negligible changes in the dimensions of the lesion (Figure 1A). Linear EUS (GF-UCT260, Olympus, Japan), as a routine procedure to localize the blood vessels surrounding a cyst and detect the morphological features of a lesion, was first performed. Surprisingly, we found some high-density shadows during the procedure (Figure 2A), which confirmed the incorrect diagnosis determined on CT. Simultaneously, no signs of blood vessels in or around the cyst were observed.
Case 2: The patient was diagnosed with a PPC, with an approximate diameter of 5 cm, 3 mo prior by abdominal CT and magnetic resonance cholangiopancreatography (Figure 1B and C). On December 18, 2020, contrast-enhanced CT showed that the dimensions of the lesion had increased to 7.12 cm × 3.99 cm. Linear EUS showed signs of high-density shadows inside of the cyst (Figure 2B). No signs of vessels were found.
Based on the two patient’s medical histories and EUS examination findings, we arranged for them to undergo EUS-guided cystogastrostomy followed by the placement of an electrocautery LAMS (16 mm × 26 mm, Micro-Tech Co., Ltd., Nanjing, China). Under direct visualization, a large amount of necrotic debris and the presence of multiple hidden vessels (Figure 3) were observed. Based on the endoscopy findings, the diagnosis of these two patients was revised to WON with the presence of multiple hidden vessels.
After multiple hidden vessels were detected by direct visualization under endoscopy, irrigation with sterile water alone was performed. Subsequent monitoring for postoperative infection showed that the temperature of both patients remained in the normal range. Using rat-tooth forceps, two consecutive DEN sessions were performed prudentially.
No active bleeding was found in these two patients during hospitalization. Within 1 mo, the metal stent was carefully extracted without complications. Two months after DEN, these two patients reported no abdominal pain. The last follow-up contrast-enhanced CT of the abdomen indicated disappearance of the PPCs and no signs of recurrence.
PPCs and WON are both local complications of acute pancreatitis with similar morphological features on imaging modalities[3]. Abdominal CT is recommended as the first-line imaging modality on admission in the absence of contraindications[4]. However, in some situations, a definite diagnosis of WON or PPCs is difficult for radiologists to achieve due to their similarities[5]. Reviewing the CT scans retrospectively, we detected some subtle radiological signs of nonliquid contents and some cord-like shadows (Figure 4), which should be recognized by radiologists as well as endoscopists.
Although more invasive, EUS has been highlighted for assessing solid debris in WON[6]. The application of EUS to evaluate the morphological features of WON, including size and contents, has significant therapeutic implications[7]. With evidence of solid contents on EUS, the misdiagnosis of PPCs could be revised. Furthermore, localizing the blood vessels surrounding a cyst is of great importance to confirm the optimal puncture site for EUS-guided drainage. Color Doppler can also be used to avoid vascular structures if needed[8].
The management of WON is challenging, and its treatment strategy has shifted from surgery to endoscopy. Recently, a novel LAMS has further promoted the popularity of this approach. Owing to the formation of a drainage channel between the gastrointestinal tract and the PFC, DEN, which has been proven to be a more effective and less invasive approach, is commonly used in the treatment of symptomatic WON[9]. EUS-guided transluminal drainage with an LAMS has a significantly higher rate of clinical success than that with a traditional double pigtail plastic stent[10].
However, gastrointestinal bleeding, as the most common complication of LAMS therapy, could be induced by direct damage or pseudoaneurysm formation[11]. A case of large crossing blood vessels within an area of WON has already been reported[12]. A retrospective study of EUS-mediated drainage with an LAMS showed an increased incidence of pseudoaneurysm bleeding[13]. Thus, if the presence of multiple hidden vessels is identified, conservative treatment by irrigation with sterile water instead of direct necrosectomy should be performed, and if an LAMS is present in vivo, monitoring for delayed bleeding should be considered.
This is the first report of multiple vessels crossing within an area of WON in two cases. Due to intraoperative EUS before cystogastrostomy and simple irrigation, we successfully avoided damaging hidden vessels and thus reduced the risk of intraoperative bleeding.
| 1. | Yasuda I, Takahashi K. Endoscopic management of walled-off pancreatic necrosis. Dig Endosc. 2021;33:335-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 60] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 2. | Takahashi N, Papachristou GI, Schmit GD, Chahal P, LeRoy AJ, Sarr MG, Vege SS, Mandrekar JN, Baron TH. CT findings of walled-off pancreatic necrosis (WOPN): differentiation from pseudocyst and prediction of outcome after endoscopic therapy. Eur Radiol. 2008;18:2522-2529. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 54] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Stamatakos M, Stefanaki C, Kontzoglou K, Stergiopoulos S, Giannopoulos G, Safioleas M. Walled-off pancreatic necrosis. World J Gastroenterol. 2010;16:1707-1712. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 54] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Arvanitakis M, Dumonceau JM, Albert J, Badaoui A, Bali MA, Barthet M, Besselink M, Deviere J, Oliveira Ferreira A, Gyökeres T, Hritz I, Hucl T, Milashka M, Papanikolaou IS, Poley JW, Seewald S, Vanbiervliet G, van Lienden K, van Santvoort H, Voermans R, Delhaye M, van Hooft J. Endoscopic management of acute necrotizing pancreatitis: European Society of Gastrointestinal Endoscopy (ESGE) evidence-based multidisciplinary guidelines. Endoscopy. 2018;50:524-546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 335] [Article Influence: 41.9] [Reference Citation Analysis (0)] |
| 5. | Abou Karam A, Bagherpour A, Calleros J, Laks S. Imaging of endoscopic cystogastrostomy in pancreatic walled-off necrosis: what the radiologist needs to know. Abdom Radiol (NY). 2018;43:3043-3053. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Rana SS, Chaudhary V, Sharma R, Sharma V, Chhabra P, Bhasin DK. Comparison of abdominal ultrasound, endoscopic ultrasound and magnetic resonance imaging in detection of necrotic debris in walled-off pancreatic necrosis. Gastroenterol Rep (Oxf). 2016;4:50-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Rana SS, Bhasin DK, Sharma RK, Kathiresan J, Gupta R. Do the morphological features of walled off pancreatic necrosis on endoscopic ultrasound determine the outcome of endoscopic transmural drainage? Endosc Ultrasound. 2014;3:118-122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 43] [Cited by in RCA: 75] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 8. | Mitrovic M, Dugalic V, Kovac J, Tadic B, Milosevic S, Lukic B, Lekic N, Cvetic V. Successful Embolization of Posterior Inferior Pancreaticoduodenal Artery Pseudoaneurysm on the Grounds of Chronic Pancreatitis-Case Report and Literature Review. Medicina (Kaunas). 2020;56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 9. | Rerknimitr R. Endoscopic Transmural Necrosectomy: Timing, Indications, and Methods. Clin Endosc. 2020;53:49-53. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Bang JY, Varadarajulu S. Endoscopic ultrasound-guided management of pancreatic pseudocysts and walled-off necrosis. Clin Endosc. 2014;47:429-431. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 25] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Rana SS. An overview of walled-off pancreatic necrosis for clinicians. Expert Rev Gastroenterol Hepatol. 2019;13:331-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 50] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 12. | Alhasan F, Hoilat GJ, Malas W, Mahmood SK, Zivny J, Alsayid M. Endoscopic Management of Giant Walled-Off Pancreatic Necrosis With a High Risk of Bleeding. ACG Case Rep J. 2019;6:e00199. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Brimhall B, Han S, Tatman PD, Clark TJ, Wani S, Brauer B, Edmundowicz S, Wagh MS, Attwell A, Hammad H, Shah RJ. Increased Incidence of Pseudoaneurysm Bleeding With Lumen-Apposing Metal Stents Compared to Double-Pigtail Plastic Stents in Patients With Peripancreatic Fluid Collections. Clin Gastroenterol Hepatol. 2018;16:1521-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 114] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nishikawa K S-Editor: Wang LL L-Editor: Wang TQ P-Editor: Zhang YL