Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7279
Peer-review started: May 7, 2021
First decision: June 6, 2021
Revised: June 7, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 26, 2021
Processing time: 108 Days and 18.8 Hours
Lumbar radiculopathy is a common symptom in the clinic and is often caused by lumbar disc herniation or osteophytes compressing the nerve root; however, it is rare for nerve roots to be compressed by epidural gas. Few symptomatic epidural gas-containing pseudocyst cases have been reported. Furthermore, the reported cases were due to a mix of gas and obvious osteophytes; therefore, it was hard to rigorously conclude that gas was the factor responsible for radiculopathy. We provide evidence that because no epidural gas accumulated before radiculopathy occurred and the symptoms were relieved after removal of the gas, the epidural gas-containing pseudocyst was the root cause of radiculopathy in this case.
An 87-year-old man with a 3-wk history of right radiating pain was admitted to our hospital. Computed tomography (CT) and magnetic resonance imaging (MRI) examinations showed a vacuum phenomenon and huge lesions with low signal intensity located in the same area where the pain occurred. After carefully checking the images acquired in the last 3 mo, we found an abdominal CT examination performed 40 d prior because of abdominal pain. The CT images showed no gas-containing pseudocyst in the epidural space and notably, he had no leg pain at the time. To ensure a low-intensity intervention and complete de
This case thoroughly illustrates that an epidural gas-containing pseudocyst can result in radiculopathic pain through a comprehensive evidence chain. Percutaneous endoscopic decompression is a minimally invasive and effective treatment method.
Core Tip: The rare case reported here thoroughly illustrates that an epidural gas-containing pseudocyst can result in radiculopathic pain through a comprehensive evidence chain.
- Citation: Chen Y, Yu SD, Lu WZ, Ran JW, Yu KX. Epidural gas-containing pseudocyst leading to lumbar radiculopathy: A case report. World J Clin Cases 2021; 9(24): 7279-7284
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7279.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7279
Lumbar radiculopathy pain is commonly caused by herniated discs and progressive osteophytes due to degenerative lumbar spine disease. Nerve roots are rarely compressed by the accumulation of gas in the epidural space to lead to radiculopathic pain[1,2]. Gulati et al[3] first described free intraspinal gas collection on computed tomography (CT) images in 1980, but few studies associated with symptomatic epidural gas have been reported[4-7]. The CT images in these reports illustrated gas-containing pseudocysts located in the spinal canal that seem to compress the nerve root, and it was concluded that the accumulation of epidural gas resulted in radiculopathy. However, most of these reported symptomatic cases are based on degenerative lumbar spine disease, which is associated with osteophytes. Therefore, it was difficult to distinguish the real factor responsible for radicular pain; for example, both gas-containing pseudocysts and osteophytes existed for a long time, and osteophytes progressed over time before the symptoms finally occurred. Therefore, the existing conclusions that the accumulated epidural gas compresses the nerve to and leads to radiculopathy may not be rigorous enough.
We report one new patient who underwent CT examination 40 d before lumbar radiculopathy occurred, and the images showed no epidural gas. After radiculopathy occurred, epidural gas was found through CT, which strongly illustrated that the epidural gas resulted in lumbar radiculopathy. Endoscopic images also identified the gas-containing pseudocyst that formed and compressed the nerve root. The histological examination showed that the sampled gas-containing pseudocyst tissue was fibrous connective tissue.
An 87-year-old man with a 3-wk history of right leg radiating pain was admitted to our hospital.
Initially, right leg pain appeared after weight bearing. The pain worsened when standing, and no significant relief could even be achieved by staying in bed. The pain was located in the posterior part of his right leg, from the right hip to calf, with no numbness or hypoesthesia. He was diagnosed with lumbar disc herniation with radiculopathy in a community health service centre 10 d before admission to our hospital. He was advised to take celecoxib 0.2 g q.d., acupuncture, massage, and other physiotherapy; however, the pain was still constant, and there was no real remission. Therefore, he came to our hospital for further treatment.
The patient was diagnosed with osteoarthritis of the knee for 15 year. He underwent resection of the nucleus pulposus of the intervertebral disc 10 years ago due to lumbar disc herniation, with no symptom recurrence after surgery. He had undergone plain CT 40 d prior because of abdominal pain and no positive findings. After taking some traditional Chinese medicine, he experienced pain relief.
The patient did not drink or smoke. The patient’s family history was negative.
Lumbar muscle tension, tenderness on L5, S1 spinous process, and severe tension on the outlet of sciatic nerve of the buttock were noted. The muscle strength and tension of both lower limbs were normal. The straight-leg raising test was positive (40°) on the right, and the augmentation test was positive (30°). Both knee tendon reflex (++), left achilles tendon reflex (++), and right achilles tendon reflex (+) were positive.
The blood test showed no abnormality.
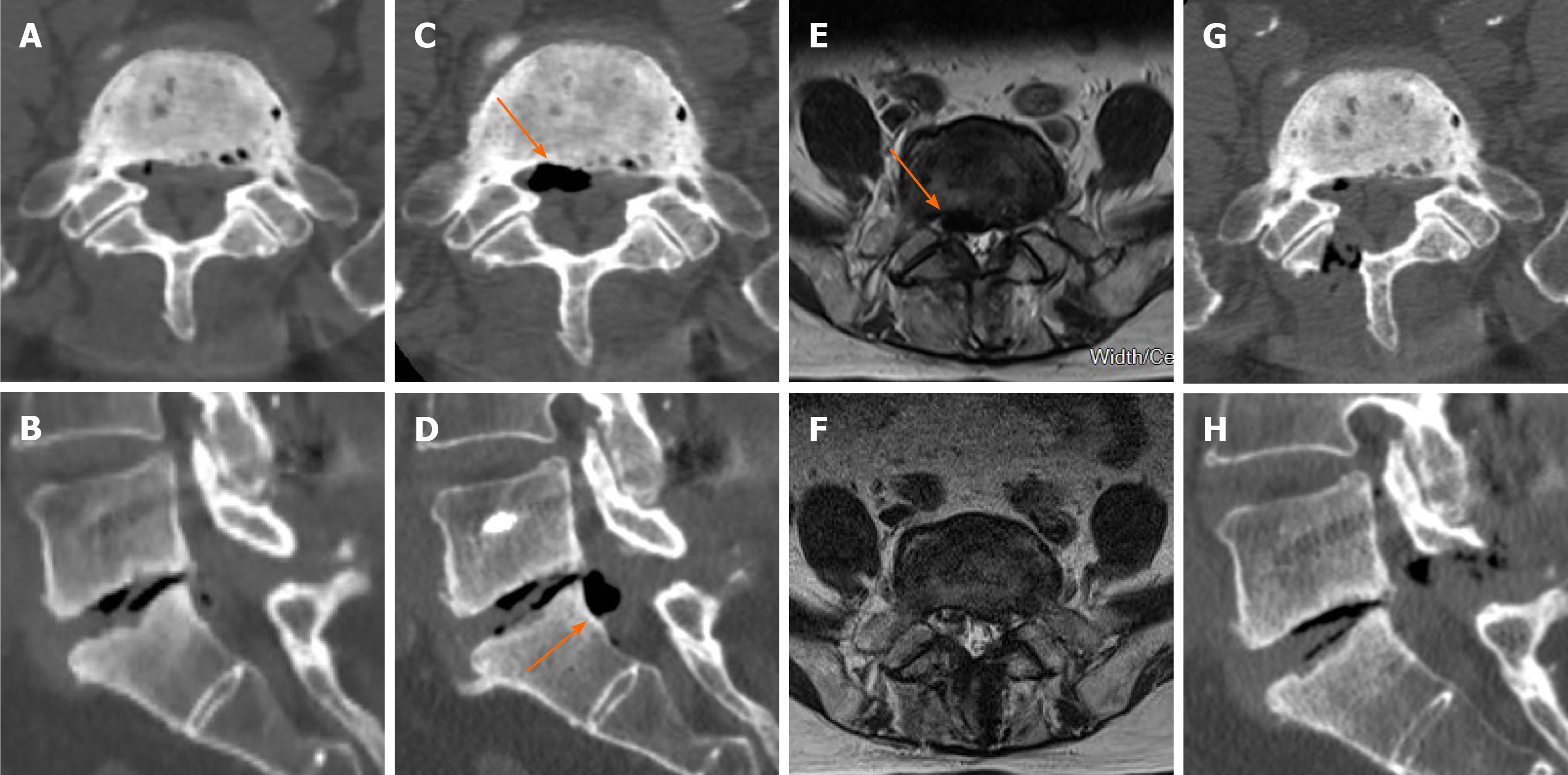
Although the patient had undergone plain CT 40 d prior because of abdominal pain, the CT image showed no gas collection in the lumbar spinal canal (Figure 1A and B). However, when the patient presented with pain this time, the CT image showed a marked L5/S1 vacuum disc phenomenon, and gas collection was located at the posterolateral position of the spinal canal adjoining the right-upper portion of the S1 posterior vertebral wall (Figure 1C-E). Magnetic resonance imaging (MRI) revealed a lesion with extremely low signal intensity on both T1WI and T2WI in the L5/S1 disc space that was consistent with the very low signal intensity in the spinal canal.
The final diagnosis of the presented case was: (1) Epidural gas-containing pseudocyst with lumbar radiculopathy; (2) Degenerative lumbar spine; and (3) Osteoarthritis of both knees.
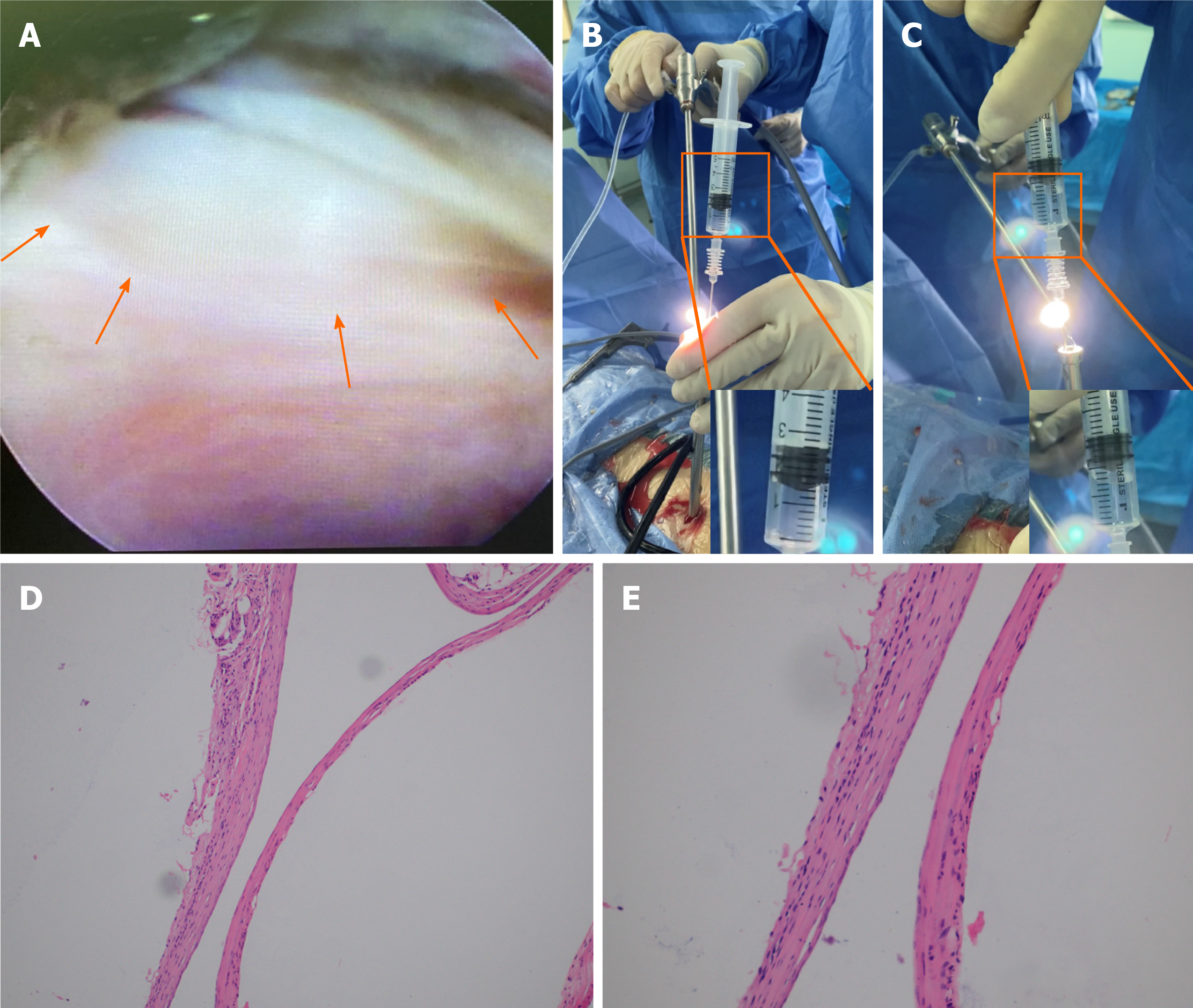
A right S1 spinal nerve block demonstrated that the pain originated from S1 spinal nerve compression. To ensure a low-intensity intervention and complete decompression of the nerve, percutaneous endoscopic lumbar nerve decompression surgery was advised. The area around the S1 nerve root was clearly exposed under endoscopy. The membranous structure of the gas-containing pseudocyst was observed on the inferior aspect of the S1 nerve root (Figure 2A). After retracting the nerve root, the gas-containing pseudocyst was exposed, a 20 G needle was used to puncture the gas-containing pseudocyst, and approximately 1 mL gas was extracted (Figure 2B and C). Basket forceps were used to cut and remove the pseudocyst. The wall of the cyst was thin and smooth. The postoperative course was uneventful. The radicular pain disappeared completely at the last follow-up.
The right leg pain was completely relieved after surgery. Postoperative examinations showed the disappearance of the gas-containing pseudocyst after percutaneous endoscopic decompression (Figure 1F-H). The histological examination showed that the sampled gas-containing pseudocyst tissue was fibrous connective tissue (Figure 2D and E). The wall of the gas-containing pseudocyst was fibrous connective tissue lined with flat cells. The radicular pain disappeared completely at the last follow-up.
Although a vacuum phenomenon in a degenerative intervertebral disc is relatively common in elderly individuals[3], epidural gas collection in the spinal canal is unusual, and there are few reports about radicular pain caused by gas compression in the lumbar spinal canal. Due to the lack of sufficient evidence, especially presymptomatic images, there is still controversy regarding what the real reason for radiculopathy is, gas or progressive osteophytes. In our case, the patient exhibited no leg pain and no obvious gas collection in the spinal canal before the symptoms occurred. When radicular pain occurred, a gas-containing pseudocyst was observed through CT and MRI examinations. After removing the gas-containing pseudocyst under endoscopy, the pain was completely relieved. This evidence chain strongly illustrates that epidural gas-containing pseudocysts result in lumbar radicular pain.
Some authors believe that epidural gas collection may arise from a valve-pump mechanism[8-10]. When a vacuum occurs in the disc, the motion of the lumbar spine may impose pressure on the intervertebral disc and extrude gas into the epidural region, and the gas is limited to the membranous structure, which may compress the nerve root and finally result in radicular pain. In this case, the specific valve-pump structure was not observed under endoscopy; however, the membranous structure of the gas-containing pseudocyst was identified, and 1 mL gas was extracted. The choice of treatment is still controversial. Some patients experience pain relief after conservative therapy; if conservative therapy fails, surgery must be performed[5,11]. Our patient’s symptoms were very serious and showed no relief after conservative treatment. Thus, surgery had to be performed. In the literature, although percutaneous aspiration under CT guidance is the most minimally invasive method, the recurrence rate is high, and the pain relief effect is poor because the membrane of the gas cyst is still intact[8,12]. Open surgery can totally remove gas cysts to achieve good clinical outcomes; however, the risk for soft tissue injury is significant[13]. In this case, we completely removed the membranous gas cyst under percutaneous endoscopy first using an interlaminar approach. The biggest advantages of this approach are minimal trauma from an 8 mm skin incision and effective pain relief from the total removal of gas cysts under direct view.
This case thoroughly illustrated that an epidural gas-containing pseudocyst can result in radiculopathic pain through a comprehensive evidence chain. Percutaneous endoscopic decompression is a minimally invasive and effective treatment method.
Dr. Yu KX appreciates the Chongqing Medicial University and Chongqing Traditional Chinese Medicine Hospital, and the guidance of Prof. Deng ZL and Prof. Lu WZ.
| 1. | Liu WC, Lee SH, Kwon AM, Park J, Park HS. Morphologic Characteristics and Clinical Significance of Computed Tomography and Magnetic Resonance Imaging Findings of Spinal Epidural Gas. World Neurosurg. 2020;141:e792-e800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Zhu B, Jiang L, Liu XG. Transforaminal Endoscopic Decompression for a Giant Epidural Gas-Containing Pseudocyst: A Case Report and Literature Review. Pain Physician. 2017;20:E445-E449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Gulati AN, Weinstein ZR. Gas in the spinal canal in association with the lumbosacral vacuum phenomenon: CT findings. Neuroradiology. 1980;20:191-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 47] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Mortensen WW, Thorne RP, Donaldson WF 3rd. Symptomatic gas-containing disc herniation. Report of four cases. Spine (Phila Pa 1976). 1991;16:190-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 34] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Kakitsubata Y, Theodorou SJ, Theodorou DJ, Yuko M, Ito Y, Yuki Y, Wada S, Maehara T. Symptomatic epidural gas cyst associated with discal vacuum phenomenon. Spine (Phila Pa 1976). 2009;34:E784-E789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Austin RM, Bankoff MS, Carter BL. Gas collections in the spinal cord on computed tomography. J Comput Assist Tomogr. 1981;5:522-524. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Tamburrelli F, Leone A, Pitta L. A rare cause of lumbar radiculopathy: spinal gas collection. J Spinal Disord. 2000;13:451-454. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Yoshida H, Shinomiya K, Nakai O, Kurosa Y, Yamaura I. Lumbar nerve root compression caused by lumbar intraspinal gas. Report of three cases. Spine (Phila Pa 1976). 1997;22:348-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 56] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 9. | Gebarski SS, Gebarski KS, Gabrielsen TO, Knake JE, Latack JT, Yang PJ. Gas as a mass: a symptomatic spinal canalicular collection. J Comput Assist Tomogr. 1984;8:145-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 20] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Cheng TM, Link MJ, Onofrio BM. Pneumatic nerve root compression: epidural gas in association with lateral disc herniation. Report of two cases. J Neurosurg. 1994;81:453-458. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Raynor RB, Saint-Louis L. Postoperative gas bubble foot drop. A case report. Spine (Phila Pa 1976). 1999;24:299-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 30] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Righini A, Lucchi S, Reganati P, Zavanone M, Bettinelli A. Percutaneous treatment of gas-containing lumbar disc herniation. Report of two cases. J Neurosurg. 1999;91:133-136. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Lee CW, Yoon KJ, Ha SS, Kang JK. Radicular compression by intraspinal epidural gas bubble occurred in distant two levels after lumbar microdiscectomy. J Korean Neurosurg Soc. 2014;56:521-526. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hamza M S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Li JH