Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7245
Peer-review started: April 20, 2021
First decision: May 24, 2021
Revised: June 3, 2021
Accepted: July 2, 2021
Article in press: July 2, 2021
Published online: August 26, 2021
Processing time: 125 Days and 22.7 Hours
Bronchogenic cysts (BCs) are benign congenital foregut malformations that are mostly present in the mediastinum and pulmonary parenchyma but rarely seen in the retroperitoneum.
We report the case of 17-year-old girl who complained of epigastric pain. A cystic lesion was found in the left suprarenal region on spectral computed tomography. The ovoid, well-defined, and homogeneous cystic lesion revealed slightly enhancement on conventional imaging but no enhancement on 40 KeV virtual mono-energetic images. The iodine density value of the lesion was 0.001 mg/mL and the Z-effective value was 7.25, which were close to those of fluid material in in vitro experiments. Magnetic resonance imaging revealed a cystic mass of intermediate signal intensity on T1-weighted imaging and high signal intensity on T2-weighted imaging. A laparoscopic surgery was carried out. Intraoperatively, a cystic lesion with a smooth surface was found in the left retroperitoneum. And the cystic wall was completely resected after intracystic fluid was suctioned. The histopathological examination findings of the lesion were compatible with BC. The patient recovered uneventfully without sighs of recurrence during a 10-mo follow-up period.
Radiological examinations play a significant role in the diagnosis of suprarenal BCs and spectral images offer additional spectral parameters. Accurate preoperative diagnoses of retroperitoneal BCs based on thorough imaging examinations are beneficial to the operation of laparoscopic resection.
Core Tip: Bronchogenic cysts (BCs) are benign congenital foregut malformations that are mostly present in the mediastinum and intrapulmonary but rarely seen in the retroperitoneum. We report a case of BC in the left suprarenal region which was diagnosed based on spectral computed tomography imaging and magnetic resonance imaging. After a laparoscopic surgery, the patient recovered uneventfully without sighs of recurrence during a 10-mo follow-up period.
- Citation: Wu LD, Wen K, Cheng ZR, Alwalid O, Han P. Retroperitoneal bronchogenic cyst in suprarenal region treated by laparoscopic resection: A case report. World J Clin Cases 2021; 9(24): 7245-7250
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7245.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7245
Bronchogenic cysts (BCs) are congenital foregut-derived aberrations of the respiratory tract in the process of embryonic development[1]. They are usually located in the mediastinum and pulmonary parenchyma, and rarely occurred in the retroperitoneum. In most cases, retroperitoneal bronchogenic cysts (RBCs) occur near the left adrenal gland or pancreas[2].
In dual energy computed tomography (CT), material decomposition and quantification depend on photoelectric effect and Compton effect in different elemental compositions generated by X-ray[3]. Dual layer detector spectral CT (also known as spectral CT) is a new detector-based dual energy CT for clinical use, in which the top and bottom layers of detector absorb low- and high-energy photons, respectively. Owing to the technology of novel dual layer detector, both conventional images and energy images reach perfect temporal and spatial registration. Spectral images are comprised of virtual mono-energetic images (VMI), iodine density map, Z-effective (Z-eff) map, and so on[4]. Spectral imaging has widely used in the study of abdominal diseases. It was reported that the optimal energy level of VMI could decrease pseudo-enhancement effect of renal cysts in in vivo and in vitro experiments based on spectral imaging[5,6]. Other spectral parameters such as iodine density value and Z-effective value were also used to differentiate cystic lesions from solid lesions[7,8]. Currently, there is no report about imaging manifestations of suprarenl BCs based on spectral CT imaging. Herein, we report the first case of suprarenl BC found on the spectral CT and review cases of RBCs in English-language publications.
A 17-year-old girl was referred to Union Hospital (Huazhong University of Science and Technology, Wuhan, Hubei Province, China) with epigastric pain.
The patient had epigastric pain for a week without back pain or other symptoms.
The patient had no previous history of hypertension or endocrine-related disease.
The patient was in good health in the past and had no family history.
Routine and specialized physical examination of the patient showed no obvious abnormalities.
Except erythrocyte count was slightly decreased, other laboratory results of the patient were within the normal limits.
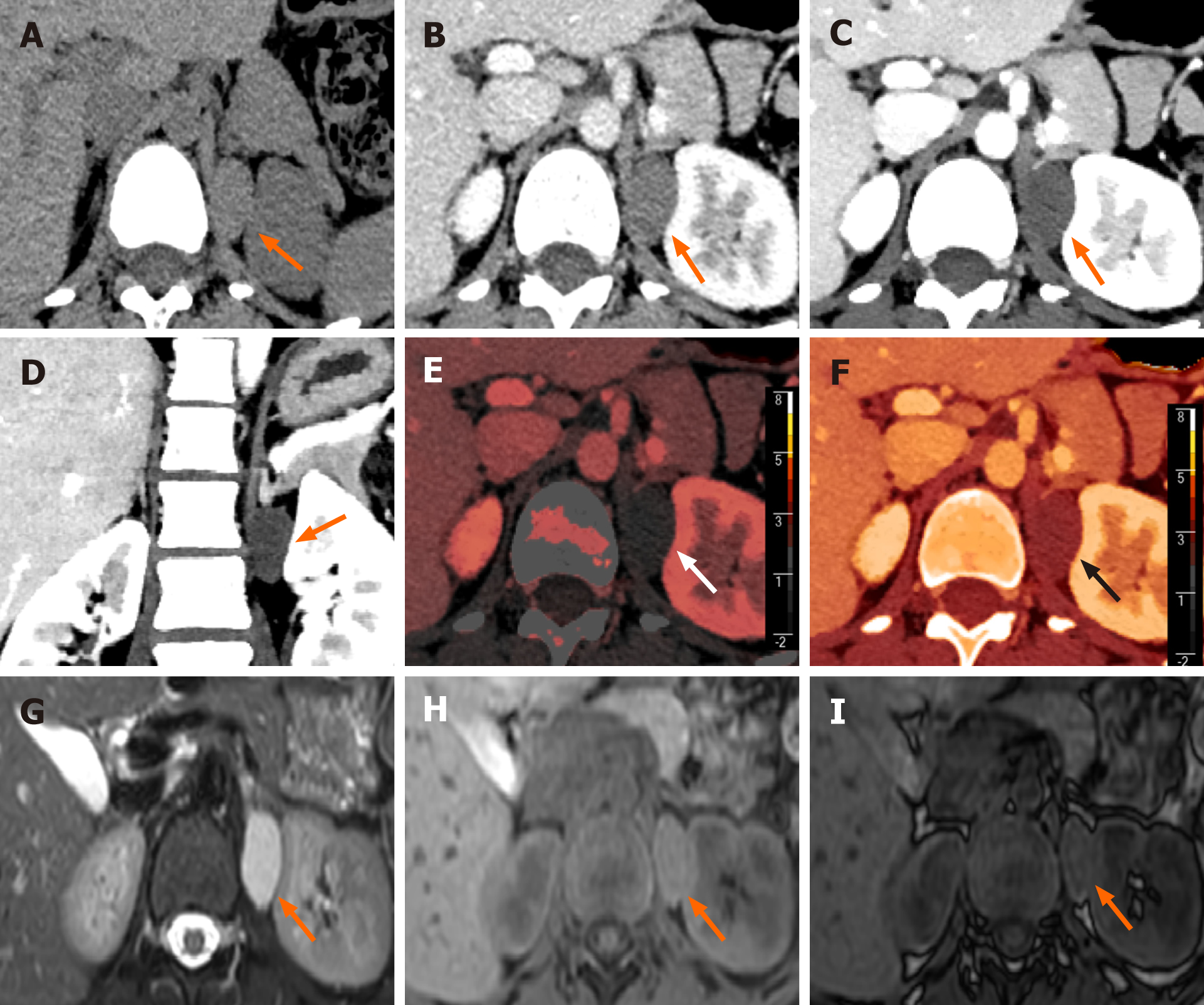
Spectral images showed a 29 mm × 17 mm × 28 mm ovoid, well-defined, and homogeneous cystic lesion in the left adrenal area. The lesion was slightly enhanced on conventional images while no enhancement on VMI40KeV. In coronary plane of VMI40KeV, the lesion margin was clear with significant contrast. The iodine density value of the lesion was 0.001 mg/mL and the Z-eff value was 7.25. Magnetic resonance imaging revealed a cystic mass with intermediate signal intensity on T1-weighted imaging (T1WI) and high signal intensity on T2-weighted imaging (T2WI). Chemical shift imaging revealed no fat component within the lesion (Figure 1).
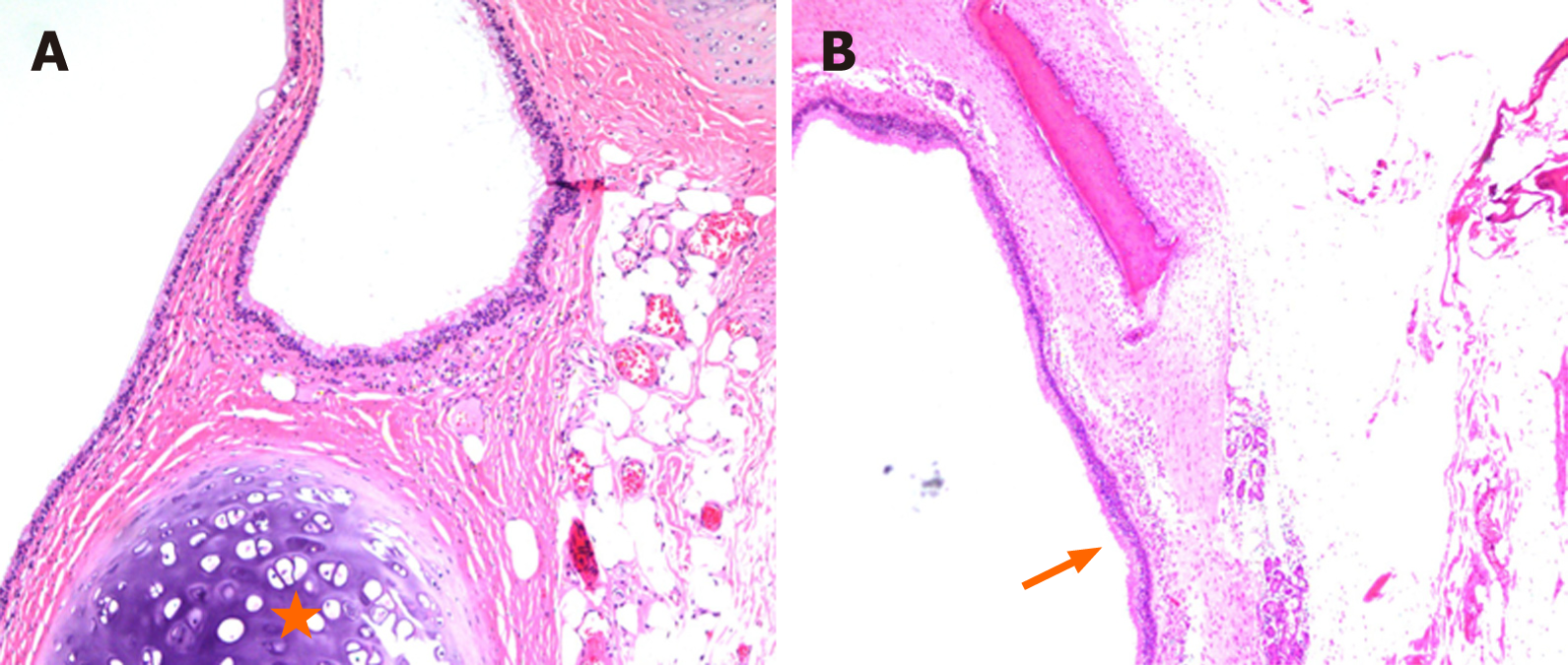
The histopathological characteristics of the lesion are compatible with BC. On gross examination, the cystic lesion was about 30 mm in size. Upon sectioning, the lesion contained gray yellowish fluid. The cystic wall with a smooth inner surface measured about 1-2 mm in thickness. The cyst contained pseudostratified ciliated columnar epithelium and mature hyaline cartilage (Figure 2).
To confirm the diagnosis, a retroperitoneal laparoscopic resection was carried out. During the surgery, a 2.0 cm skin incision was made in the mid-axillary line 1.5 cm above the iliac crest and a laparoscope was placed through a 10 mm trocar in this site. Two additional trocars (5 mm and 10 mm) were placed in the anterior and posterior axillary line below the inferior margin of the twelfth rib, respectively. The patient was placed in the left lateral position with the kidney rest elevated. The angle between the long axis of the patient’s upper trunk and long axis of the table was 20º-30º. And surgeons were in the dorsal side of the patient close to buttocks. Meticulous dissection and fine operation technique were applied to avoid the injury to the peritoneum and vessels. Intraoperatively, a cystic lesion with a smooth surface was found in the left retroperitoneum. The cystic wall was completely resected after intracystic fluid was suctioned.
The patient recovered uneventfully without sighs of recurrence during a 10-mo follow-up period.
BCs are benign malformation as a result of the abnormal budding of the foregut at the 3rd-7th weeks of the embryogenesis. When the connection between bronchial buds and tracheobronchial tree completely separates, the buds may migrate to unusual locations such as neck, intraspinal, pericardiac, and subdiaphragm[9,10]. A search on PubMed database revealed 64 publications of RBCs published worldwide in the English literature. After screening the full texts and pathological results, 48 publications reporting on 50 cases of RBCs were eventually yielded.
RBCs tend to be found on the left side of the abdomen. About half of them were located in the suprarenal area. According to Rud et al[2], the left pericardioperitoneal canal shuts later and is larger than the right one, which provides an explanation for the predominantly left side location of RBCs. The mean age of these patients was 39.1 ± 15.2 years. The mean size of cysts was 5.9 ± 3.2 cm. Slightly over half of patients had been identified incidentally without related symptoms. Of symptomatic patients, the majority complained of nonspecific epigastric pain and a small number complained of thoracic pain and back pain. To relieve clinical manifestations and reduce the risk of complications and malignant change, surgical excision is recommended. And laparoscopic resection has been widely used to lessen economic burden as well as postoperative pain of patients[11]. More than half of patients with RBCs underwent laparoscopic resection and the majority were free of complications during the postoperative course.
BCs has ciliated, pseudo-stratified, columnar epithelium with parenchyma containing any one as follows: Seromucous glands, smooth muscle, or cartilage[12]. Ultrasonography generally shows a cystic hypo/isoechoic lesion. On conventional images, RBCs are round or fusiform, well-circumscribed, and hypodense lesions with slight enhancement or without enhancement. RBCs usually manifest low or intermediate signal intensity on T1WI and high signal intensity on T2WI. In our case, increased attenuation on CT and increased signal intensity on T1WI suggested proteinaceous fluid. Some cases in the literature also reported this imaging appearance[13,14]. Fat components were rarely seen in BCs. Most RBCs manifested as no signal loss on the opposed-phase imaging or no signal decrease on T1WI with fat suppression, which was similar to the appearance of our case[15].
We report the first case of RBC found on spectral CT. VMI are reconstructed by both high-energy and low-energy data sets of spectral imaging, which overcome pseudo-enhancement of cystic lesion caused by beam-hardening artifacts[5,6,16]. Also the image noise of whole spectrum is stable and relatively low. Therefore, the image quality of low-energy VMI is significantly improved. In our case, the lesion had slight enhancement on conventional images, while pseudo-enhancement of cystic lesion was eliminated and lesion conspicuity and margin delineation were more pronounced on VMI40KeV. On iodine density map, iodine remain or uptake in specific blood vessels, organs, or lesions could be quantified using region of interest method[4]. The extremely low iodine density of the lesion indicated a lack of cellular components, which excluded solid tumors with iodine uptake[7]. Z-eff values depend on Compton effect and photoelectric effect of the material in the process of spectral decomposition[4]. The Z-eff value of the lesion was 7.25, equal to that of fluid material reported on a phantom research of spectral imaging[8], which suggested that it was full of fluid contents.
The retroperitoneal laparoscopic resection was applied in our case. During the operation, the cystic wall was completely resected after intracystic fluid was suctioned. With thorough preoperative imaging and laboratory examinations, benign cystic lesions would be diagnosed confidently in the suprarenal region. Comparing to the laparoscopic surgery performed on other adrenal lesions, the surgery of RBCs has a clearer surgical field as well as shorter operative time.
BCs are benign congenital foregut malformations caused by abnormal migration of bronchial buds. We report the first case of suprarenal BCs found on spectral CT. Radiological examinations play a significant role in diagnosis of suprarenal BCs and spectral images offer additional spectral parameters. Accurate preoperative diagnosis of RBCs based on thorough imaging examinations is beneficial to the operation of laparoscopic resection.
| 1. | Sumiyoshi K, Shimizu S, Enjoji M, Iwashita A, Kawakami K. Bronchogenic cyst in the abdomen. Virchows Arch A Pathol Anat Histopathol. 1985;408:93-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 72] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 2. | Rud O, May M, Brookman-Amissah S, Moersler J, Greiner A, Gilfrich C. Retroperitoneal bronchogenic cyst treated by laparoscopic surgery. Chirurg. 2010;81:243-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and Multi-Energy CT: Principles, Technical Approaches, and Clinical Applications. Radiology. 2015;276:637-653. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 790] [Cited by in RCA: 1152] [Article Influence: 104.7] [Reference Citation Analysis (0)] |
| 4. | Rassouli N, Etesami M, Dhanantwari A, Rajiah P. Detector-based spectral CT with a novel dual-layer technology: principles and applications. Insights Imaging. 2017;8:589-598. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 96] [Cited by in RCA: 205] [Article Influence: 22.8] [Reference Citation Analysis (0)] |
| 5. | Jung DC, Oh YT, Kim MD, Park M. Usefulness of the virtual monochromatic image in dual-energy spectral CT for decreasing renal cyst pseudoenhancement: a phantom study. AJR Am J Roentgenol. 2012;199:1316-1319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 6. | Mileto A, Nelson RC, Samei E, Jaffe TA, Paulson EK, Barina A, Choudhury KR, Wilson JM, Marin D. Impact of dual-energy multi-detector row CT with virtual monochromatic imaging on renal cyst pseudoenhancement: in vitro and in vivo study. Radiology. 2014;272:767-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 89] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Kim H, Park CM, Kang CK, Yoon J, Chae KJ, Goo JM. Effect of CT Acquisition Parameters on Iodine Density Measurement at Dual-Layer Spectral CT. AJR Am J Roentgenol. 2018;211:748-754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Garcia LI, Azorin JF, Almansa JF. A new method to measure electron density and effective atomic number using dual-energy CT images. Phys Med Biol. 2016;61:265-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 9. | Chung SK, Lee KW, Kang HI, Yamashita C, Kudo M, Yoshida Y. Design and synthesis of potential inhibitors of the ergosterol biosynthesis as antifungal agents. Bioorg Med Chem. 2000;8:2475-2486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 238] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 10. | Wen Y, Chen W, Chen J, He X. Retroperitoneal bronchogenic cyst resembling an adrenal tumor: two case reports and literature review. J Int Med Res. 2020;48:300060520925673. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 11. | Dietrich A, de Santibañes M, Rodriguez Santos F, Santino J, Cristiano A, Sanchez Clariá R. Resection of a Retroperitoneal Bronchogenic Cyst: Laparoscopic Approach. CRSLS. 2014;18. [DOI] [Full Text] |
| 12. | Liang MK, Marks JL. Congenital bronchogenic cyst in the gastric mucosa. J Clin Pathol. 2005;58:1344. [PubMed] |
| 13. | Chu PY, Hwang TI, Teng TH, Lee CC. A retroperitoneal bronchogenic cyst successfully treated by laparoscopic surgery. Ann Saudi Med. 2007;27:199-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 14. | Terasaka T, Otsuka F, Ogura-Ochi K, Miyoshi T, Inagaki K, Kobayashi Y, Nasu Y, Makino H. Retroperitoneal bronchogenic cyst: a rare incidentaloma discovered in a juvenile hypertensive patient. Hypertens Res. 2014;37:595-597. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Brient C, Muller C, Cassagneau P, Taieb D, Sebag F, Henry JF. A retroperitoneal bronchogenic cyst. J Visc Surg. 2012;149:e361-e363. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Sellerer T, Noël PB, Patino M, Parakh A, Ehn S, Zeiter S, Holz JA, Hammel J, Fingerle AA, Pfeiffer F, Maintz D, Rummeny EJ, Muenzel D, Sahani DV. Dual-energy CT: a phantom comparison of different platforms for abdominal imaging. Eur Radiol. 2018;28:2745-2755. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 116] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cimen SG S-Editor: Wu YXJ L-Editor: Wang TQ P-Editor: Zhang YL