Published online Aug 26, 2021. doi: 10.12998/wjcc.v9.i24.7212
Peer-review started: March 6, 2021
First decision: May 24, 2021
Revised: June 2, 2021
Accepted: July 16, 2021
Article in press: July 16, 2021
Published online: August 26, 2021
Processing time: 170 Days and 7.6 Hours
Neurogenic tumors account for about ten percent of all tumors of childhood, and benign tumor originating from Schwann cells is rare in peripheral nerves. Schwannoma of the tongue is quite rare in children.
We present the case of an 8-year-old male with schwannoma in the anterolateral tongue. The mass was slow-growing for one year with no pain and discomfort. He underwent transoral mass excision under general anesthesia. Gross examination revealed a smooth surfaced, 17 mm × 14 mm × 7 mm sized, encapsulated nodule with a clear resection margin. Schwannoma of the tongue was confirmed by the pathological exam. He reported no motor or sensory change, such as dysgeusia or paresthesia, or phonation difficulty during postoperative 12 mo follow-up.
Schwannoma of the tongue is a rare benign neoplasm in childhood. If a painless firm mass is encountered in the tongue of a child, solid tumors like schwannoma should be considered in the differential diagnosis.
Core Tip: Schwannoma of the tongue is a rare benign neoplasm in childhood. If a painless firm mass is encountered in the tongue of a child, solid tumors like schwannoma should be considered in the differential diagnosis. Based on the suspicion of schwannoma, meticulous surgical excision is necessary in terms of functional preservation and preventing recurrence.
- Citation: Yun CB, Kim YM, Choi JS, Kim JW. Pediatric schwannoma of the tongue: A case report and review of literature. World J Clin Cases 2021; 9(24): 7212-7217
- URL: https://www.wjgnet.com/2307-8960/full/v9/i24/7212.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i24.7212
Neurogenic tumors account for 10% of all tumors of childhood[1]. Of these, schwannoma (neurilemmoma), which is a slow growing, benign tumor originating from Schwann cells, is rare in peripheral nerves[2]. About 25% of schwannomas are identified in the head and neck area, and only 1% have intraoral origins, which include tongue, palate, buccal mucosa, lip, and gingiva[3] Although several reports have been issued on this topic of intraoral schwannoma in young patients, no review has been published on pediatric schwannoma of the tongue. Herein, we present a case of pediatric schwannoma of the tongue and review available literature over the last 56 years (from 1964 to 2020). In the English literature over the past 56 years, a total of 17 pediatric cases of schwannoma of the tongue have been reported. Based on a review of these reports, we explored common clinical symptoms, clinical courses, and the differential diagnosis of this disease.
An 8-year-old boy presented at our otorhinolaryngology outpatient clinic with complaints of a slow growing painless mass in his tongue. He had an anterolateral tongue with slow-growing for one year.
He denied all symptoms including pain, dysgeusia, dysphagia, dysphonia, bleeding, and impaired tongue mobility.
The patient had a free previous medical history.
He denied any family history.
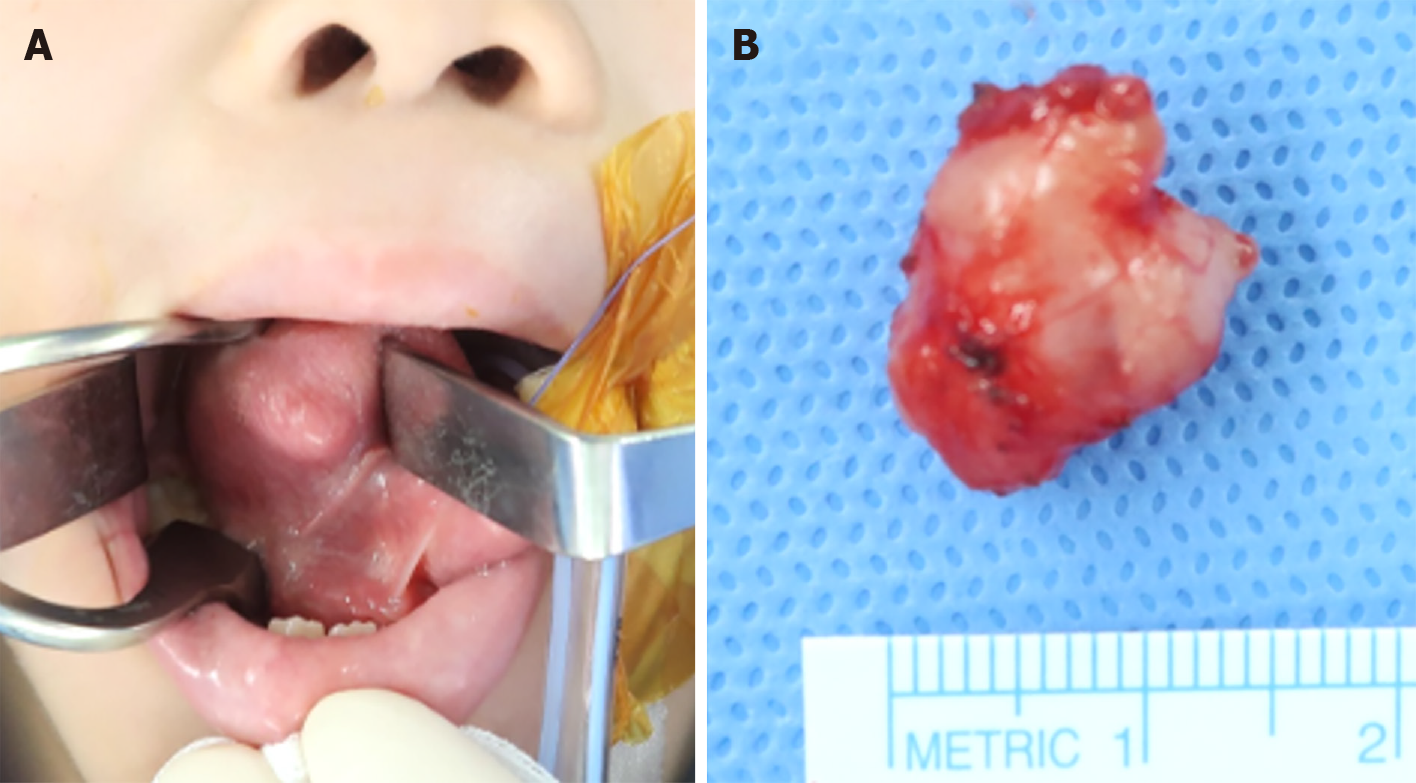
A 15 mm sized submucosal firm, hard, non-tender mass was identified in the right anterolateral side of the tongue (Figure 1A). Overlying mucosa was intact, and cervical lymph nodes were not palpable.
Initial laboratory testing showed no abnormality.
No radiological investigations were performed because the mass was easily visible and palpable.
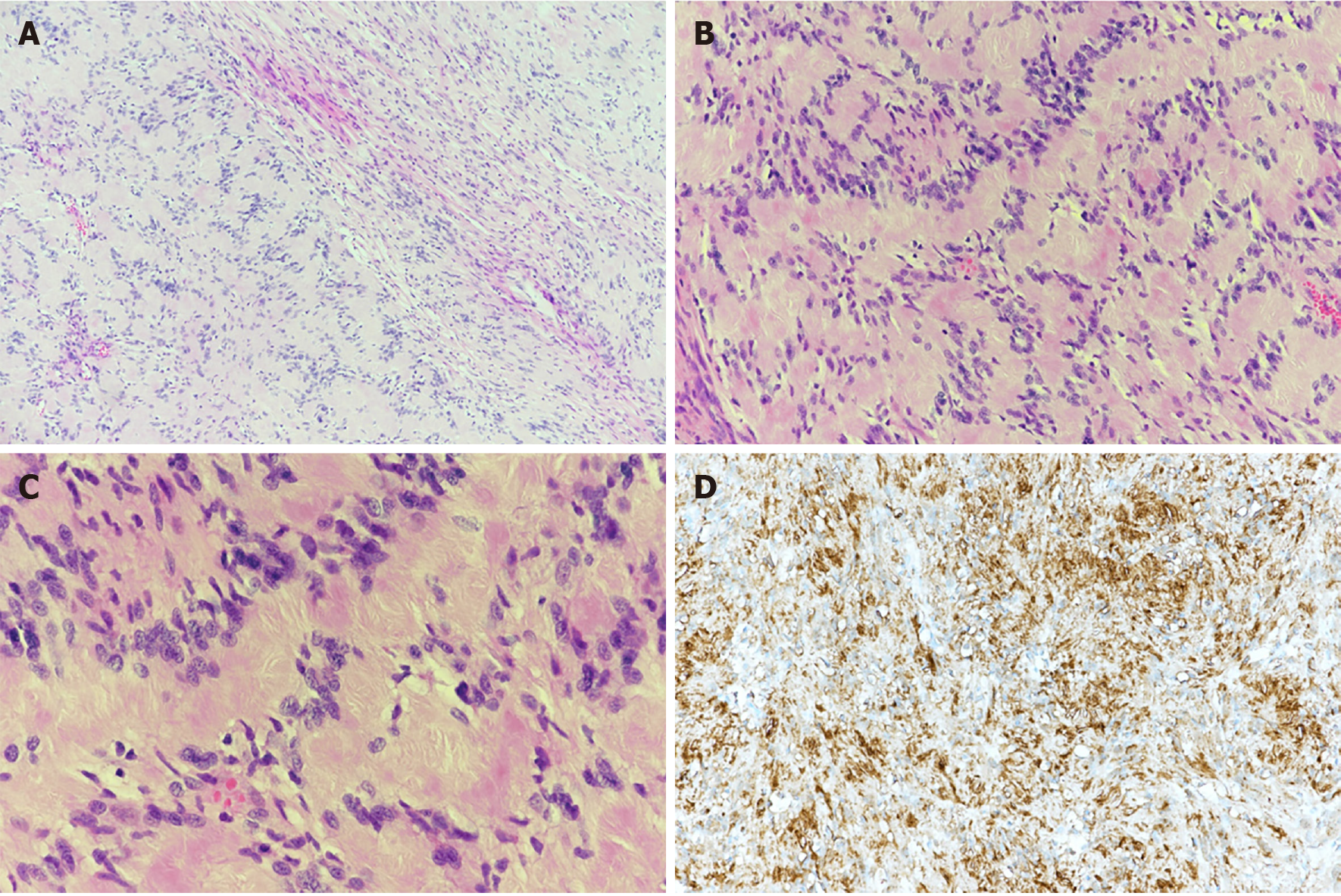
Microscopically the tumor was composed of Schwann cells arranged in a cellular palisading pattern (Antoni type A) with Verocay bodies and a second (Antoni type B) looser, disorganized arrangement (Figure 2A). Antoni A areas composed of Verocay bodies which consists of a stacked arrangement of two rows of elongated palisading nuclei that alternates with acellular zones (Figure 2B and C). Diagnosis was confirmed by immunohistochemical staining; tumor tissue was strongly positive for S-100 (Figure 2D).
He underwent transoral mass excision under general anesthesia. Gross examination revealed a smooth surfaced, 17 mm × 14 mm × 7 mm sized, encapsulated nodule with a clear resection margin (Figure 1B).
The patient was discharged from the hospital without complications at postoperative two days, and reported no motor or sensory change, such as dysgeusia or paresthesia, or phonation difficulty for postoperative 12 mo.
Schwannomas are benign neoplasms arising from any nerve, including autonomic, peripheral, or cranial nerves, but not from optic or olfactory nerves[4]. About 25% of all schwannomas are located in the head and neck, and the parapharyngeal space is the most common site[2,3]. Schwannomas in the oral cavity are uncommon (1%), and usually affect the tongue followed by buccal or vestibular mucosa, soft palate, floor of mouth, gingiva, or lip[5,6]. Tongue schwannomas may occur at any age, but peak incidence is usually seen between 20 and 50 years of age[3]. Reports indicate any part of the tongue may be involved (e.g., ventral, base, or tip)[7-10]. The majority of cases (around two-thirds) involve the anterior, mobile portion, and in the other third, the posterior portion of the tongue base. Among the 21 pediatric cases reviewed, proportions of anterior and posterior locations were almost equal.
During our literature review from 1964 to 2020, we identified 20 cases of pediatric schwannoma of the tongue (Table 1). The 21 cases (including our case) showed no gender predilection [11 males (52.4%) and 10 females (47.6%)]. Age at onset ranged from 7 to 15 years (mean 12 years). The location of tumor was divided into half anterior and posterior. Eleven cases occurred anteriorly and 7 posteriorly; those of other three cases were not mentioned. Schwannoma diameters ranged from 5 to 30 mm and all were resected using a transoral approach. Most patients had no complaints after surgery, though four had symptoms such as snoring, oral bleeding, or a mastication or swallowing difficulty.
| Ref. | Age (yr) | Sex | Location of tumor | Size (greatest dimension, mm) | Presenting symptoms | Surgical approach |
| López-Jornet and Bermejo-Fenoll[17], 2005 | 8 | F | Posterior | 30 | Painless mass | Transoral |
| Uj[18], 1967 | 13 | F | N/A | N/A | Painless mass | Transoral |
| Barbosa and Hansen[19], 1984 | 12 | M | N/A | 5 | Painless mass | Transoral |
| Akimoto et al[20], 1987 | 14 | M | Anterior | 10 | Painless mass | Transoral |
| Siar et al[21], 1988 | 13 | F | N/A | 44 | Painless mass | Transoral |
| Bassichis and McClay[9], 2004 | 9 | M | Posterior | 23 | Snoring, difficulty breathing | Transoral |
| Cinar et al[10], 2004 | 7 | M | Anterior | 10 | Painless mass | Transoral |
| Hsu et al[22], 2006 | 9 | M | Anterior | 12 | Painless mass | Transoral |
| 12 | F | Anterior | 16 | Painless mass | Transoral | |
| 15 | F | Anterior | 12 | Painless mass | Transoral | |
| Enoz et al[23], 2006 | 7 | M | Anterior | 25 | Painless mass | Transoral |
| Pereira et al[24], 2008 | 12 | M | Posterior | 15 | Painless mass | Transoral |
| Karaca et al[25], 2010 | 13 | F | Anterior | 20 | Painless mass | Transoral |
| Naidu and Sinha[12], 2010 | 12 | M | Anterior | N/A | Oral bleeding | Transoral |
| Lukšić et al[26], 2011 | 10 | M | Posterior | 18 | Painless mass | Transoral |
| Husain et al[27], 2011 | 10 | F | Posterior | 50 | Disturbance in mastication | Transoral |
| Manna et al[28], 2012 | 15 | M | Posterior | 12 | Disturbance in swallowing | Transoral |
| Bouguila et al[29], 2013 | 15 | F | Posterior | 28 | Oral bleeding | Transoral |
| Bhola et al[30], 2014 | 14 | F | Anterior | 15 | Painful nodule | Transoral |
| Moreno-García et al[13], 2014 | 13 | F | Anterior | 20 | Painless mass | Transoral |
Tongue schwannoma can arise from the hypoglossal, lingual, or glossopharyngeal nerves, but it is difficult to determine its origin preoperatively[11]. It has been previously reported most patients are asymptomatic, and that in some the tumor is ulcerative and causes oral bleeding[12]. Typically, if a patient has nerve-related symptoms before or after operation, the origin of the schwannoma can be inferred. However, if a patient is asymptomatic perioperatively, e.g., because the tumor has been growing slowly over several years, the tumor’s origin cannot be inferred, and surgical procedure requires meticulous enucleation to minimize nerve injuries. Our patient had a lesion of duration one year, but did not have paresthesia, pain, loss of taste sensation, motor or sensory loss, or phonation difficulties, and postoperatively, did not complain of any complication. Accordingly, we could not determine its neural origin.
Schwannomas are usually solitary, but if a patient has multifocal lesions, (1) Multiple localized neurilemmomas; (2) Neurofibroma in von Recklinghausen’s disease; and (3) Schwannomatosis (a non-hereditary disease characterized by multiple subcutaneous and intradermal schwannomas along with variety of intracranial tumors) should be considered[3,13]. The main components of the differential diagnosis in pediatric tongue solid tumor are other benign neoplasms such as hamartoma, choristoma, rhabdomyoma, neurofibroma, lipoblastoma, myoblastoma, and neurilemmoma[14]. In a pediatric tongue lesion series, Sato et al[15] reported a high percentage (80%) of vascular and lymphatic lesions and a relatively low percentage of solid tumors (8%)[15]. Unlike adult patients, salivary gland tumor of the tongue is rare in childhood. Therefore, when a pediatric patient is encountered with solid, firm mass in the tongue, we consider solid tumors of neuromuscular origin after excluding lymphovascular lesions. Magnetic resonance imaging can be useful during initial workups in terms of differential diagnosis and determining lesion extents[13]. Characteristically, Schwannoma has a homogeneous well-circumscribed border and does not infiltrate surrounding tissues[4].
Due to the low incidence and nonspecific clinical presentation, the diagnosis of schwannoma is confirmed by histopathologic and immunohistochemical evaluations. Microscopically, the encapsulated tumor typically has a biphasic appearance. Antoni A areas contain Schwann cells densely packed in a palisading pattern with Verocay bodies, whereas Antoni type B areas are looser and disorganized. Diagnosis is confirmed by immunohistochemical staining for S-100, SOX10, Leu-7 antigen, vimentin, and glial fibrillary acidic protein[13,16]. In this case, the diagnosis was performed by only S-100 which is a typical marker of Schwann cell.
The treatment of choice for tongue schwannoma is complete surgical excision, which if achieved prevents recurrence[13]. Thus, incomplete excision must be avoided to ensure the preservations of normal speech and swallowing function, especially in children. Malignant transformation is rare[16], and the transoral approach is appropriate for aesthetic restoration[11].
Schwannoma of the tongue is a rare benign neoplasm in childhood. If a painless firm mass is encountered in the tongue of a child, solid tumors like schwannoma should be considered in the differential diagnosis. Complete meticulous surgical excision is important in terms of functional preservation and preventing recurrence.
| 1. | de Campora E, Radici M, de Campora L. Neurogenic tumors of the head and neck in children. Int J Pediatr Otorhinolaryngol. 1999;49 Suppl 1:S231-S233. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 2. | Cohen M, Wang MB. Schwannoma of the tongue: two case reports and review of the literature. Eur Arch Otorhinolaryngol. 2009;266:1823-1829. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 56] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Bansal R, Trivedi P, Patel S. Schwannoma of the tongue. Oral Oncol Extra. 2005;41:15-17. |
| 4. | Lollar KW, Pollak N, Liess BD, Miick R, Zitsch RP, 3rd. Schwannoma of the hard palate. Am J Otolaryngol. 2010;31:139-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 27] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 5. | Hatziotia JC, Asprides H. Neurilemoma (schwannoma) or the oral cavity. Oral Surg Oral Med Oral Pathol. 1967;24:510-526. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 77] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Wright BA, Jackson D. Neural tumors of the oral cavity. A review of the spectrum of benign and malignant oral tumors of the oral cavity and jaws. Oral Surg Oral Med Oral Pathol. 1980;49:509-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 110] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 7. | Pfeifle R, Baur DA, Paulino A, Helman J. Schwannoma of the tongue: report of 2 cases. J Oral Maxillofac Surg. 2001;59:802-804. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 74] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Mevio E, Gorini E, Lenzi A, Migliorini L. Schwannoma of the tongue: one case report. Rev Laryngol Otol Rhinol (Bord). 2002;123:259-261. [PubMed] |
| 9. | Bassichis BA, McClay JE. Pedunculated neurilemmoma of the tongue base. Otolaryngol Head Neck Surg. 2004;130:639-641. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Cinar F, Cinar S, Harman G. Schwannoma of the tip of the tongue in a child. Plast Reconstr Surg. 2004;114:1657-1658. [PubMed] |
| 11. | Ying YL, Zimmer LA, Myers EN. Base of tongue schwannoma: a case report. Laryngoscope. 2006;116:1284-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Naidu GS, Sinha SM. Schwannoma of the tongue: an unusual presentation in a child. Indian J Dent Res. 2010;21:457-459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 13. | Moreno-García C, Pons-García MA, González-García R, Monje-Gil F. Schwannoma of tongue. J Maxillofac Oral Surg. 2014;13:217-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Horn C, Thaker HM, Tampakopoulou DA, De Serres LM, Keller JL, Haddad J Jr. Tongue lesions in the pediatric population. Otolaryngol Head Neck Surg. 2001;124:164-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 15. | Sato M, Tanaka N, Sato T, Amagasa T. Oral and maxillofacial tumours in children: a review. Br J Oral Maxillofac Surg. 1997;35:92-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 94] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 16. | Kavčič J, Božič M. Schwannoma of the tongue. BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 17. | López-Jornet P, Bermejo-Fenoll A. Neurilemmoma of the tongue. Oral Oncol. 2005;41:154-157. |
| 18. | Uj J. Neurinoma of the tongue. Report of a case. Oral Surg Oral Med Oral Pathol. 1967;23:787-788. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Barbosa J, Hansen LS. Solitary multilobular schwannoma of the oral cavity. J Oral Med. 1984;39:232-235. [PubMed] |
| 20. | Akimoto Y, Yamamoto H, Nishimura H, Komiya M, Kaneko K. Neurilemmoma in the oral cavity. J Nihon Univ Sch Dent. 1987;29:203-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Siar CH, Ng KH, Chia TY, Kulkarni MG. Atypical neurilemmomas of the tongue--report of two cases. Singapore Med J. 1988;29:83-85. [PubMed] |
| 22. | Hsu YC, Hwang CF, Hsu RF, Kuo FY, Chien CY. Schwannoma (neurilemmoma) of the tongue. Acta Otolaryngol. 2006;126:861-865. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 24] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Enoz M, Suoglu Y, Ilhan R. Lingual schwannoma. J Cancer Res Ther. 2006;2:76-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 24. | Pereira LJ, Pereira PP, dos Santos Jde P, Reis Filho VF, Dominguete PR, Pereira AA. Lingual schwannoma involving the posterior lateral border of the tongue in a young individual: case report. J Clin Pediatr Dent. 2008;33:59-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 25. | Karaca CT, Habesoglu TE, Naiboglu B, Habesoglu M, Oysu C, Egeli E, Tosun I. Schwannoma of the tongue in a child. Am J Otolaryngol. 2010;31:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Lukšić I, Müller D, Virag M, Manojlović S, Ostović KT. Schwannoma of the tongue in a child. J Craniomaxillofac Surg. 2011;39:441-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 17] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 27. | Husain S, Yunus MR, Ramli R, Athar PP. Schwannoma of the tongue in a ten-year old child. J Pak Med Assoc. 2011;61:500-501. [PubMed] |
| 28. | Manna F, Barbi E, Murru F, Bussani R. Lingual schwannoma in pediatric patients. J Craniofac Surg. 2012;23:e454-e456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Bouguila J, Khalef I, BenAli M, Sriha B, Soyah N, Boughammoura L. [Tongue base schwannoma in a child]. Rev Stomatol Chir Maxillofac Chir Orale. 2013;114:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 30. | Bhola N, Jadhav A, Borle R, Khemka G, Bhutekar U, Kumar S. Schwannoma of the tongue in a paediatric patient: a case report and 20-year review. Case Rep Dent. 2014;2014:780762. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aziret M, Jin ZD, Mangla C S-Editor: Fan JR L-Editor: A P-Editor: Li X