Published online Aug 16, 2021. doi: 10.12998/wjcc.v9.i23.6781
Peer-review started: January 16, 2021
First decision: May 5, 2021
Revised: May 11, 2021
Accepted: July 5, 2021
Article in press: July 5, 2021
Published online: August 16, 2021
Processing time: 201 Days and 11.9 Hours
Foreign bodies stuck in the throat and esophagus can be discharged through the digestive tract. Esophageal-lodged foreign bodies can cause secondary injury or detrimental response, with hepatic abscess being one such, albeit rare, outcome. Review and discussion of the few case reports on such instances will help to improve the overall understanding of such conditions and aid in differential diagnosis to improve patient outcome.
A 51-year-old female patient with pre-existing diabetes visited our hospital following a 15-d experience of chills and fever. Both plain and enhanced magnetic resonance imaging and color Doppler ultrasound examination of the liver and gallbladder revealed a space-occupying lesion in the caudate lobe of the liver (7.8 cm × 6.0 cm × 5.0 cm). Initially, a malignant tumor was suspected, but differential diagnosis was unable to exclude the possibility of hepatic abscess. Conservative anti-infection therapy produced a less than ideal outcome. Additional examination by hepatobiliary imaging with computed tomography suggested a foreign body present in the upper abdomen and hepatic abscess, and subsequent endoscopy revealed a sinus tract in the anterior wall of the duodenal bulb. Therefore, surgery was performed to remove the object (fishbone) and drain the abscess. After a 2-wk uneventful recovery, the patient was discharged. The final diagnosis was foreign body-induced hepatic abscess of the caudate lobe.
Differential diagnosis is important for hepatic masses, and systematic examination and physician awareness can aid in diagnosing and curing such rare conditions.
Core Tip: Most foreign bodies that become lodged in the throat and esophagus can be discharged uneventfully through the digestive tract, but rare patients will suffer gastrointestinal perforation. We report here the case of an elderly woman whose hepatic abscess caused by transverse of an esophageal foreign body was misdiagnosed as cystadenocarcinoma. The magnetic resonance imaging diagnosis of malignant tumor was not supported by computed tomography and endoscopy findings. Ultimately, surgery and 2-wk anti-infective drug course resolved this case of foreign body-induced hepatic abscess of the caudate lobe. This case emphasizes the importance of differential diagnosis for hepatic masses.
- Citation: Pan W, Lin LJ, Meng ZW, Cai XR, Chen YL. Hepatic abscess caused by esophageal foreign body misdiagnosed as cystadenocarcinoma by magnetic resonance imaging: A case report. World J Clin Cases 2021; 9(23): 6781-6788
- URL: https://www.wjgnet.com/2307-8960/full/v9/i23/6781.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i23.6781
Fujian is located on the southeast coast of China, where cases of esophageal foreign body, caused by fishbone, are frequently encountered in clinical practice. Most foreign bodies that become lodged in the throat or esophagus can be naturally and safely discharged through the digestive tract, with less than 1% of patients suffering from gastrointestinal perforation[1]. However, very rarely, esophageal foreign bodies lead to hepatic abscess.
The process of such hepatic abscess formation occurs mainly from gastrointestinal peristalsis allowing the foreign body to penetrate the esophageal wall and reach the liver[2]. Reportedly, more than 40% of these cases are caused by fishbone[2] and, because the left liver is adjacent to the gastroduodenum, most of the foreign body-induced hepatic abscess cases involve the left liver[3,4].
A 51-year-old female patient with diabetes visited the Hepatobiliary Surgery Department of our hospital to address a persistence of chills and fever that had lasted for over 2 wk.
The patient reported that her symptoms had started 15 d prior to presentation, with her highest recorded body temperature during that time reaching 38.8 °C. She had visited another local hospital and had been given anti-infection treatment, which had not resolved the symptoms. The repeat fever prompted her to visit our hospital.
The patient had been diagnosed with diabetes 1 year prior but was not monitoring her glucose levels. She also had a history of appendectomy and no known drug allergies. She denied any history of hypertension or coronary heart disease. She recalled no experience of physical discomfort. She has not had physical examinations for an extended period of time.
The patient denied any relevant family history.
Evaluation of the vital signs showed blood pressure of 115/71 mmHg, heart rate of 90 beats per min, temperature of 36.7 °C, and respiratory rate of 18 breaths per min. The height was 160 cm and weight was 65 kg (being classified by body mass index as ‘slightly overweight’).
Physical examination showed a slight tenderness under the xiphoid process and upper abdomen. No palpable lymphadenopathy or mass was found. There were no remarkable findings with respect to other clinical signs (e.g., McBurney's point tenderness, rebound tenderness and muscle tension, and abnormalities of the cardio-pulmonary system).
After being admitted, the patient underwent laboratory examinations including routine blood test, stool analysis with fecal occult blood test, liver and kidney function tests, electrolyte panel, blood coagulation factor tests, and tumor markers tests. Endoscopy and the preoperative examinations eliminated the possibility of syphilis, hepatitis B, hepatitis C, and human immunodeficiency virus infection. Routine blood test showed elevated leukocytes (24.67 × 109/L; normal range: 4.00-10.00 × 109/L) and neutrophils (91.24%; normal range: 50%-70%). The biochemical tests showed decreased albumin (28.2 g/L; normal range: 35.0-54.0 g/L) and increased alanine aminotransferase (84 IU/L; normal range: 0-40 IU/L), aspartate aminotransferase (67 IU/L; normal range: 0-46 IU/L), and D-dimer (14.68 mg/mL; normal range: 0-0.50 mg/mL). The tumor markers carcinoembryonic antigen (CEA) (0.8 ng/mL; normal range: 0-5.0 ng/mL) and CA199 (5.45 U/mL; normal range: 0-40 U/mL) were within the normal range. There was no remarkable finding obtained from any of the other hematologic tests.
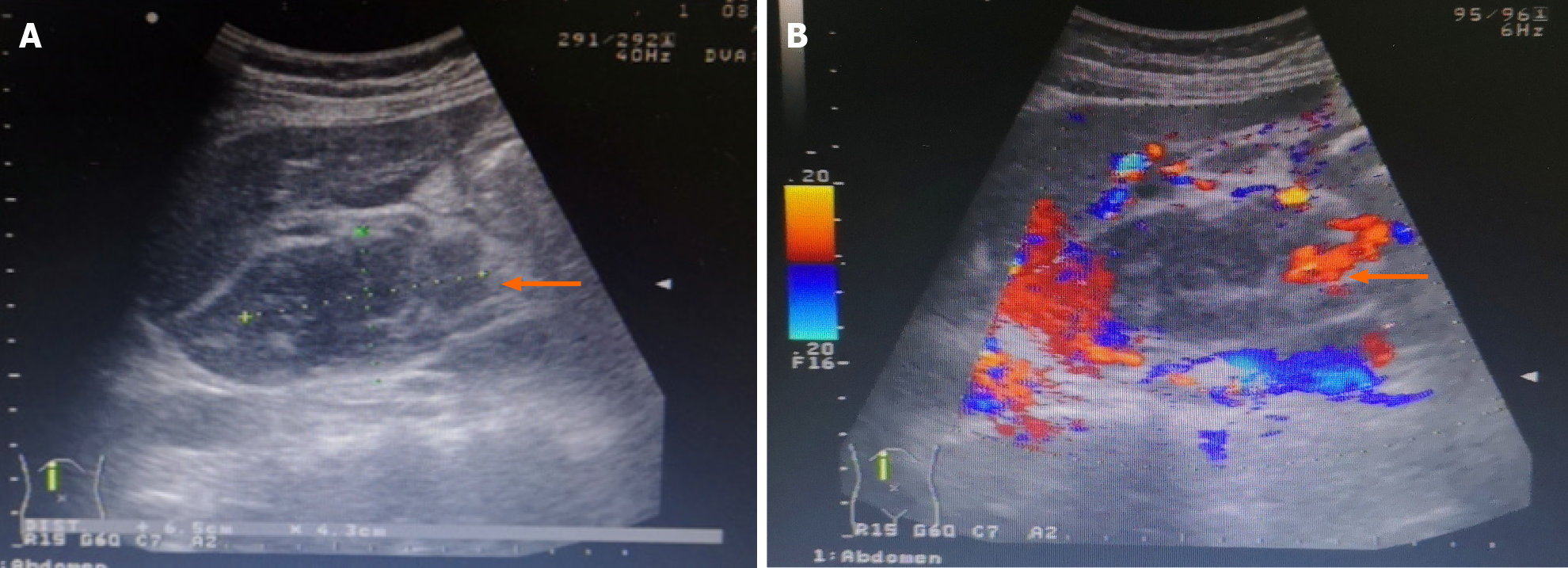
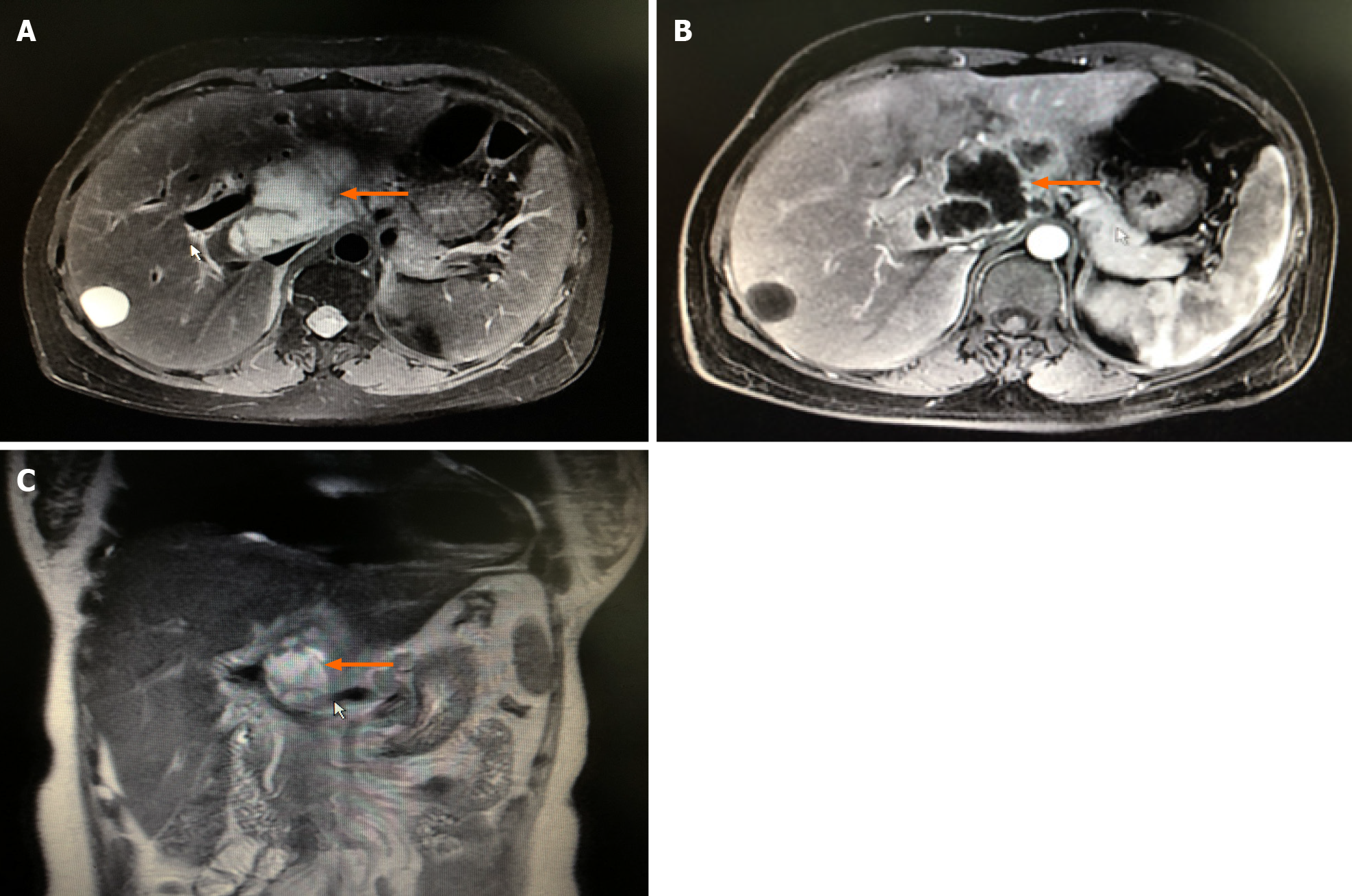
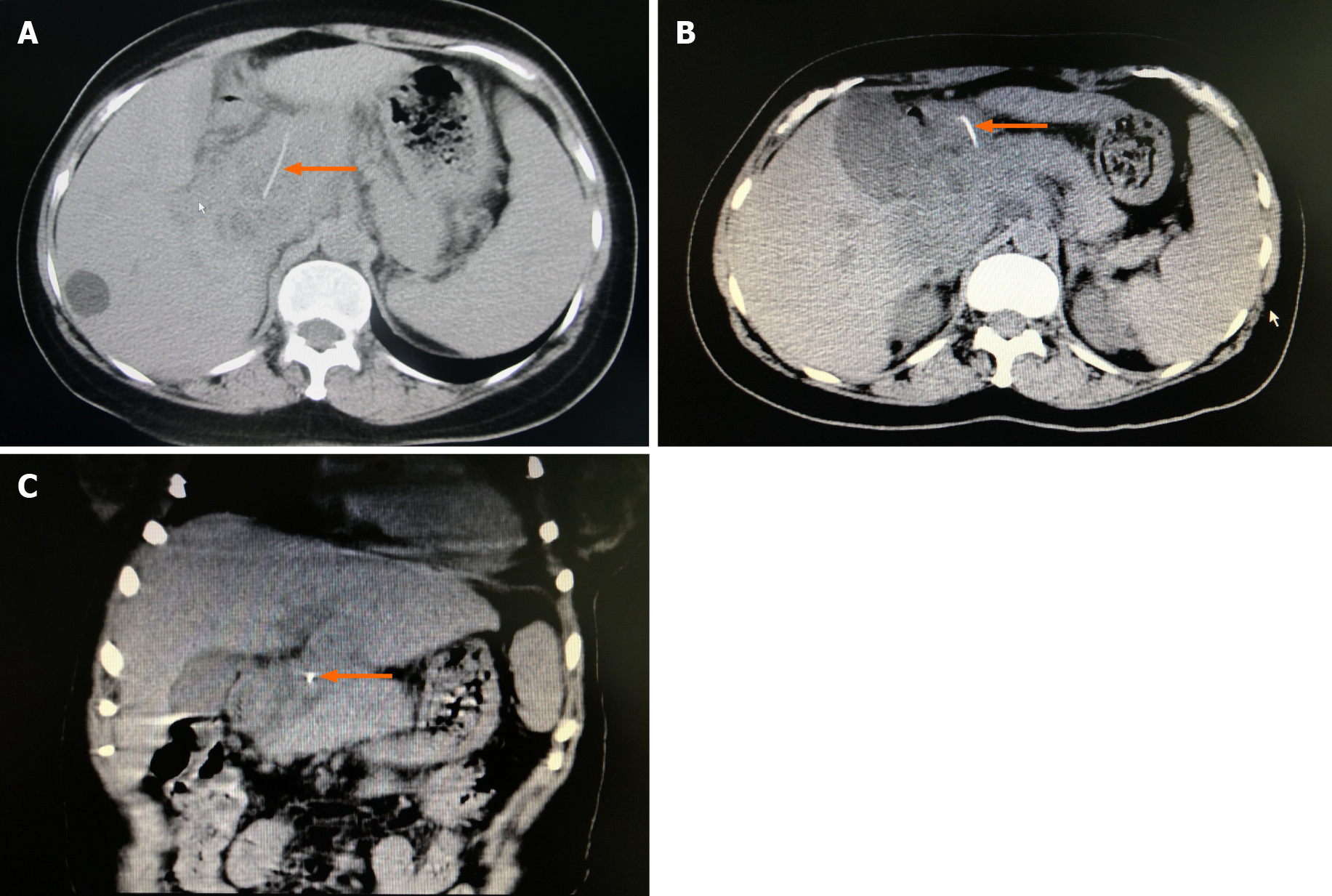
Plain computed tomography (CT) scanning of the liver and gallbladder, performed in another hospital, had displayed a low-density mass in the patient’s hepatic porta, and the possibility of malignant tumor cannot be ruled out. We augmented the imaging examination by performing color Doppler ultrasound of the liver and gallbladder, and found a hypoechogenic mass in the caudate lobe of the liver (6.5 cm × 4.3 cm in size) which was suspected as a malignant tumor (Figure 1). Plain plus enhanced magnetic resonance imaging of the liver and gallbladder also showed a space-occupying lesion on the caudate lobe of the liver (7.6 cm × 4.4 cm × 5.0 cm), which was suspected as cystadenocarcinoma (Figure 2) and was considered in differential diagnosis (from hepatic abscess) along with the patient’s clinical manifestations. A new plain CT scan of the liver, gallbladder, and spleen suggested a foreign body (fishbone) in the upper abdomen, which had perforated the gastric wall and reached the hepatic hila, and consequent abscess formation in the caudate lobe and superior head of the pancreas (7.8 cm × 6.0 cm × 5.0 cm) (Figure 3).
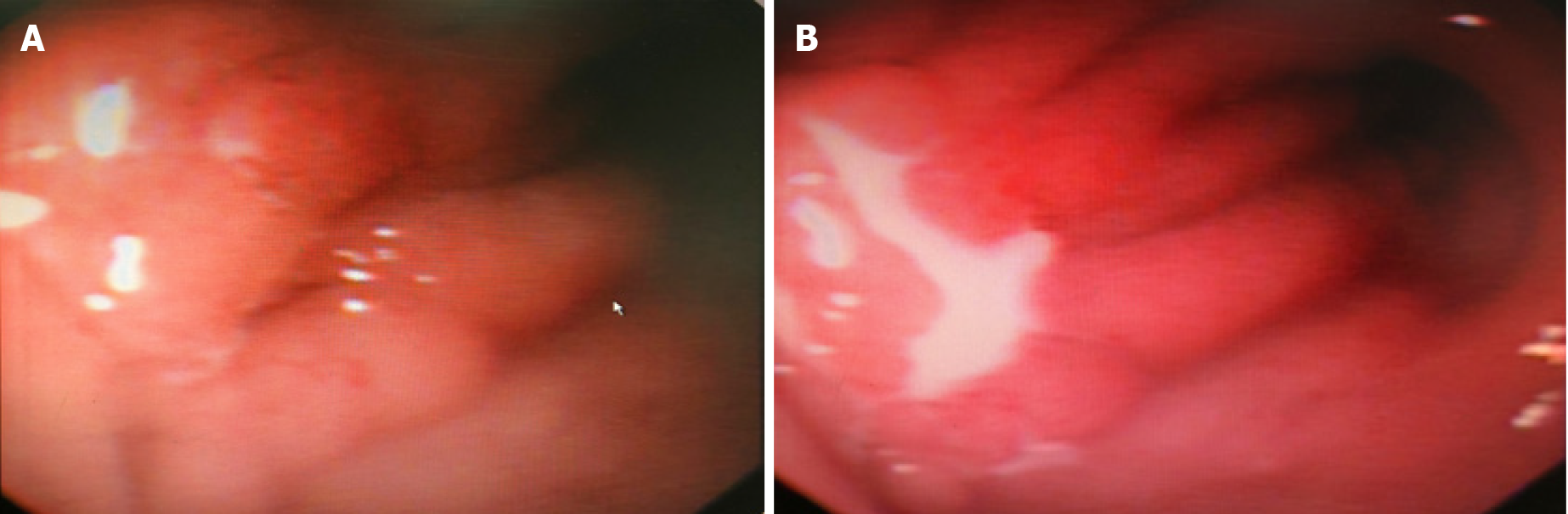
Gastroscopy was ordered and revealed chronic gastritis and a sinus tract located in the anterior wall of the duodenal bulb (Figure 4).
Highly-suspected hepatic abscess caused by esophageal foreign body (fishbone).
After admission, anti-infective treatment was administered (latamoxef sodium 2.0 g bid). The patient’s fever subsided, and she reported experiencing no discomfort. Routine blood test showed appreciable decreases in (but still slightly elevated levels of) leukocytes (12.10 × 109/L) and neutrophils (82.20%). Biochemical examinations found that the albumin level had decreased even further below the normal range (at 26.7 g/L) but restoration to normal levels of alanine aminotransferase (22 IU/L) and aspartate aminotransferase (24 IU/L). There were no other remarkable findings.
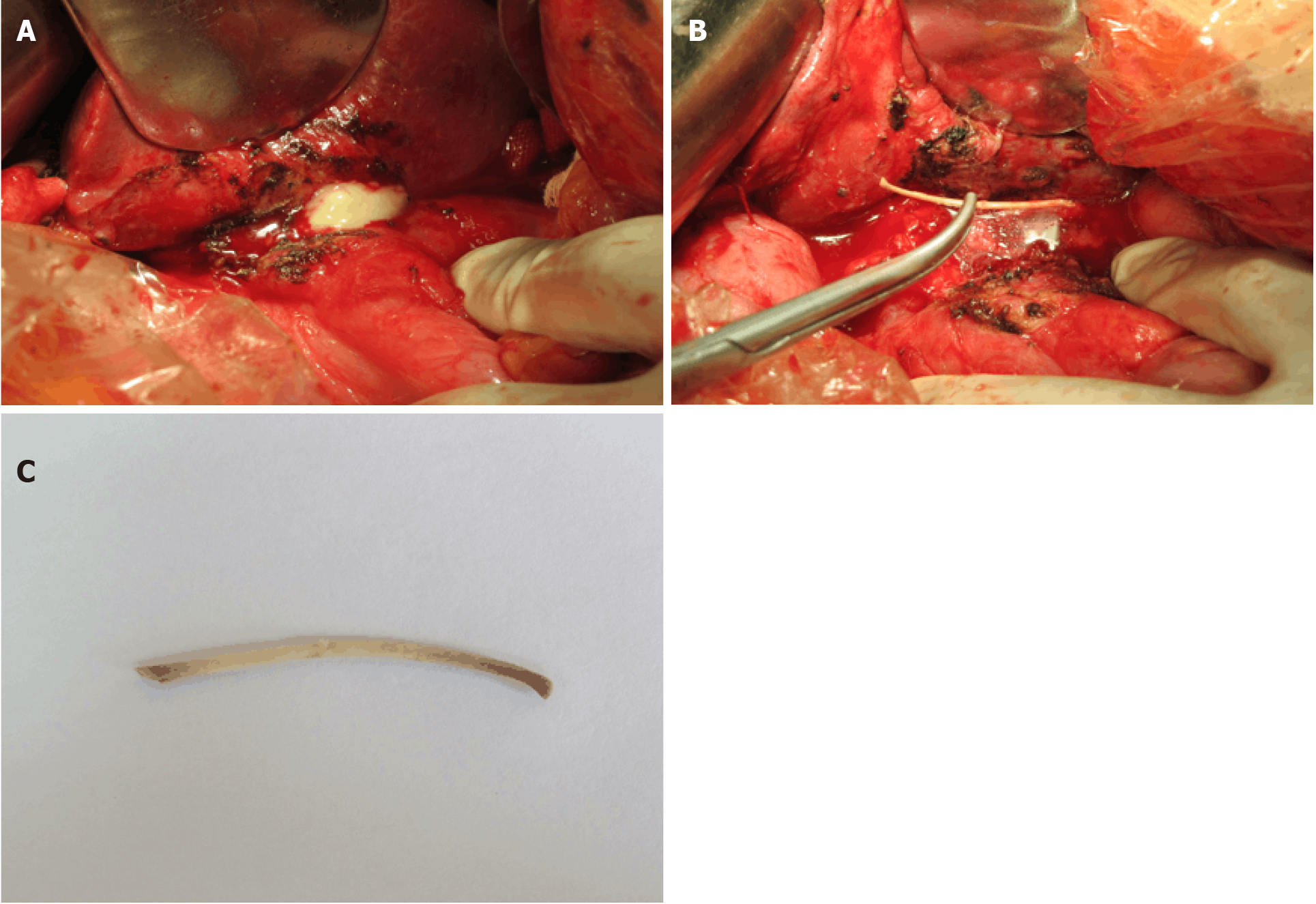
The antibiotic treatment was deemed effective. However, the underlying cause of foreign body perforating the gastric wall and reaching the hepatic hila to form an abscess in the caudate lobe and superior head of the pancreas still needed to be addressed, and served as a surgical indication. The patient underwent exploratory laparotomy plus debridement and drainage of the abdominal abscess, removal of duodenal perforator, jejunostomy, and lysis of the intestinal adhesion. Intraoperatively, a giant multicavity and thick-walled abscess was found, involving the posterosuperior gastric antrum, anterior caudate lobe of the liver, and superior head of the pancreas; the abscess size was 9 cm × 8 cm × 8 cm. The abscess was also found to have expanded into the posterior hepatoduodenal ligament, clinging to the portal vein. Opening of the purulent cavity revealed yellowish-white pus content. The tissue was congestive and edematous. Upon aspiration of the pus and debridement of the necrotic tissue, a single, slender, bony foreign body was exposed (4 cm in length; 0.3 cm diameter) (Figure 5). It was physically perforating the duodenum and reaching into the abdominal cavity; the removal was carried out carefully, with respect to the possibilities of intestinal adhesion and angulation in the abdominal cavity.
The duration of surgery was 180 min and intraoperative blood loss was 50 mL. Postoperative anti-infective treatment was administered (latamoxef sodium 2.0 g bid) for 1 wk. At 2 wk postoperatively, the patient had recovered and was discharged without event.
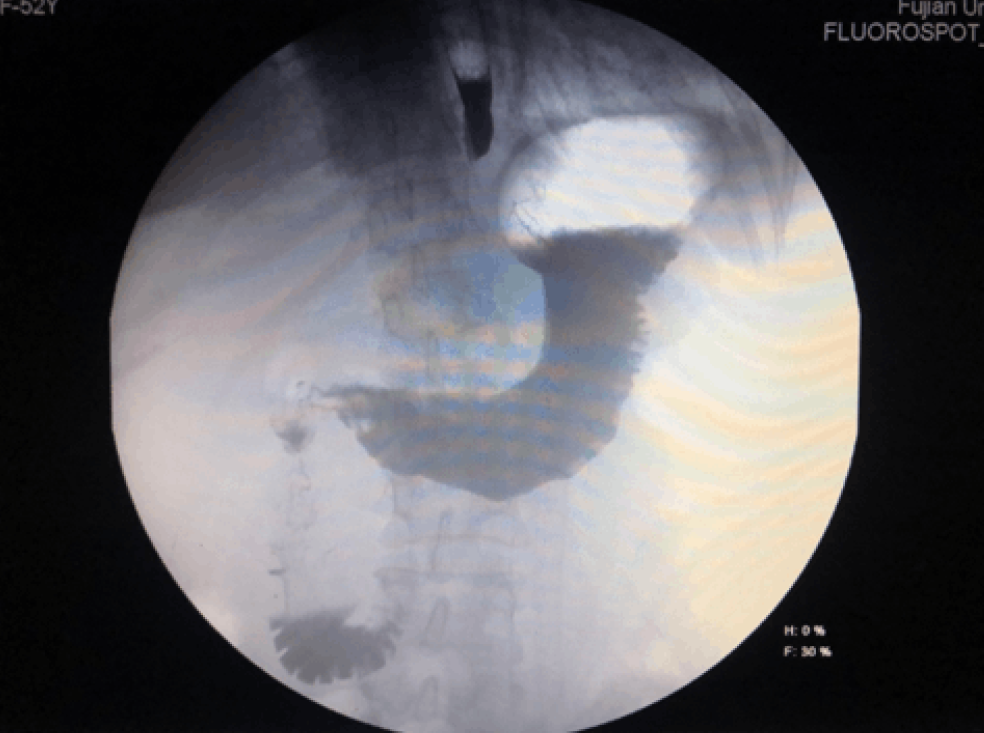
At 2 wk after the surgery, the patient was submitted to a follow-up digital gastroenterography, for which no contrast extravasation was observed in the gastroduodenum (Figure 6). At the 6 mo follow-up, the patient did not develop any complications such as intestinal obstruction. Results of liver function, kidney function, and complete blood count tests were all within the normal range.
Hepatic abscess is a severe infectious disease, which is caused by pyogenic lesion due to infection of the liver. The complex biliary system and arteriovenous system in the liver, unfortunately, provide a space suitable for bacterial parasitism and infection, thereby greatly increasing the probability of infection in patients. Hepatic abscess is characterized by rapid bacterial infection, obvious clinical symptoms, and many complications, which endanger the life safety of patients at all times. Due to the protective function of the greater omentum, however, more than 50% of patients with hepatic abscess caused by foreign body perforation present symptoms after more than 2 wk, delaying clinic visit, diagnosis, and treatment; as such, the mortality is also higher than that of patients with common hepatic abscess, which has been reported as 17.6%[5].
In our case, the patient had no history of hepatitis and both CEA and CA199 were negative[6]. However, according to CT and magnetic resonance imaging results from previous hospitals, hepatobiliary cystadenocarcinoma could not be excluded. The main point of differentiation between the two is that the wall of liver abscess is thicker and uniform, while cystadenocarcinoma is characterized by mural solid nodules[7]. Cystic adenocarcinoma complicated with infection may also lead to fever, leukocyte elevation, and other signs of infection, with more atypical clinical symptoms and laboratory test results. The course of hepatic abscess in the abdominal cavity caused by inadvertent swallowing of a fishbone and its perforating the gastric wall was long, and the progression of the disease was slow. Antibiotics were applied repeatedly for anti-infection treatment, resulting only in slight improvements in the patient’s symptoms. As the patient was not cured, the hepatic abscess formed gradually. Therefore, early diagnosis and treatment are critical, with preoperative imaging diagnosis being particularly important.
The main symptoms of hepatic abscess caused by foreign bodies include epigastric pain, fever, poor appetite, vomiting, etc., which are similar to those of common hepatic abscess, lacking an obvious specificity that would otherwise support more timely management. Most patients have no memory of foreign-body swallowing, but we should pay attention to whether the patient has a history of pica when performing inquiry into medical history[8]. Most foreign bodies are small and difficult to distinguish on imaging[9], underlying the overall low preoperative diagnostic rate and delay in treatment initiation. Many studies have suggested that the reported incidence of hepatic abscess caused by foreign bodies is lower than the actual situation[10]. However, if the foreign body can be found, the correct diagnosis can be made by combining clinical examination findings with medical history.
The linear calcification of foreign bodies detected on CT is an important imaging basis for the diagnosis of hepatic abscess caused by foreign bodies[11]. CT can display the location, size, shape, edge, and relationship with surrounding organs and blood vessels, as well as secondary changes of foreign bodies in an all-round, comprehensive, and intuitive way, which is of great significance in the discovery of foreign bodies and the diagnosis of complications. Our case indicates that CT may be superior to magnetic resonance imaging in the diagnosis of hepatic abscess caused by foreign bodies. Moreover, digestive endoscopy is helpful to identify the location of a foreign body perforating the digestive tract, assisting in definitive diagnosis and initiation of accurate treatment[4]. In the treatment of hepatic abscess caused by foreign bodies, removal of the foreign body and successful drainage of the abscess are paramount. The ongoing development of laparoscopy and the da Vinci robot platform has led to an increased rate of such surgeries by minimally invasive routes. For patients with cystadenocarcinoma that cannot be ruled out preoperatively, radical resection is recommended, and the recurrence rate after simple fenestration and local incision is 90%[12].
The diagnosis of hepatic abscess caused by esophageal foreign bodies remains a challenge. The incidence of esophageal foreign bodies is relatively high, while hepatic abscess caused by esophageal foreign bodies is not uncommon. Despite having been investigated in previous case studies, this condition is still regularly misdiagnosed as tumor. Misdiagnosis can result in improper or delayed treatment, causing severe complications. Differential diagnosis based on imaging and histological methods, combined with specialized examinations for this condition, is therefore of utmost importance. Surgical treatment at the early stage can reduce the possibility of developing severe complications.
| 1. | Maiss J, Raithel M, Nägel A. [Foreign bodies in the upper gastrointestinal tract]. HNO. 2012;60:792, 794-797. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Leggieri N, Marques-Vidal P, Cerwenka H, Denys A, Dorta G, Moutardier V, Raoult D. Migrated foreign body liver abscess: illustrative case report, systematic review, and proposed diagnostic algorithm. Medicine (Baltimore). 2010;89:85-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 59] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | de la Vega M, Rivero JC, Ruíz L, Suárez S. A fish bone in the liver. Lancet. 2001;358:982. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Chong LW, Sun CK, Wu CC. Successful treatment of liver abscess secondary to foreign body penetration of the alimentary tract: a case report and literature review. World J Gastroenterol. 2014;20:3703-3711. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 35] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Fujiwara Y, Shiba H, Nakabayashi Y, Otsuka M, Yanaga K. Hepatic abscess in the Spiegel lobe caused by foreign body penetration: report of a case report. Surg Case Rep. 2017;3:24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Zhang FB, Zhang AM, Zhang ZB, Huang X, Wang XT, Dong JH. Preoperative differential diagnosis between intrahepatic biliary cystadenoma and cystadenocarcinoma: a single-center experience. World J Gastroenterol. 2014;20:12595-12601. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Mavilia MG, Pakala T, Molina M, Wu GY. Differentiating Cystic Liver Lesions: A Review of Imaging Modalities, Diagnosis and Management. J Clin Transl Hepatol. 2018;6:208-216. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 51] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 8. | Perkins M, Lovell J, Gruenewald S. Life-threatening pica: liver abscess from perforating foreign body. Australas Radiol. 1999;43:349-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Goh BK, Chow PK, Quah HM, Ong HS, Eu KW, Ooi LL, Wong WK. Perforation of the gastrointestinal tract secondary to ingestion of foreign bodies. World J Surg. 2006;30:372-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 222] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 10. | Gundara JS, Harrison R. An unusual zoonosis: liver abscess secondary to asymptomatic colonic foreign body. HPB Surg. 2010;2010:794271. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Akazawa Y, Watanabe S, Nobukiyo S, Iwatake H, Seki Y, Umehara T, Tsutsumi K, Koizuka I. The management of possible fishbone ingestion. Auris Nasus Larynx. 2004;31:413-416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 41] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Lee CW, Tsai HI, Lin YS, Wu TH, Yu MC, Chen MF. Intrahepatic biliary mucinous cystic neoplasms: clinicoradiological characteristics and surgical results. BMC Gastroenterol. 2015;15:67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Shimizu Y S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Ma YJ