Published online Jan 16, 2021. doi: 10.12998/wjcc.v9.i2.357
Peer-review started: September 16, 2020
First decision: November 14, 2020
Revised: November 14, 2020
Accepted: December 11, 2020
Article in press: December 11, 2020
Published online: January 16, 2021
Processing time: 113 Days and 18.7 Hours
Limb length discrepancy (LLD) after total knee arthroplasty (TKA) has been considered as one of the reasons for the unsatisfactory outcome. However, there is no consensus about the extent of LLD that can be considered as clinically relevant.
To evaluate the incidence of radiographic LLD and its impact on functional outcome following TKA.
All randomized-controlled trial and observational studies on LLD in TKA, published till 22nd June 2020, were systematically searched and reviewed. The primary outcome was “limb lengthening or LLD after TKA”. The secondary outcomes included “assessment of LLD in varus/valgus deformity” and “impact of LLD on the functional outcome”.
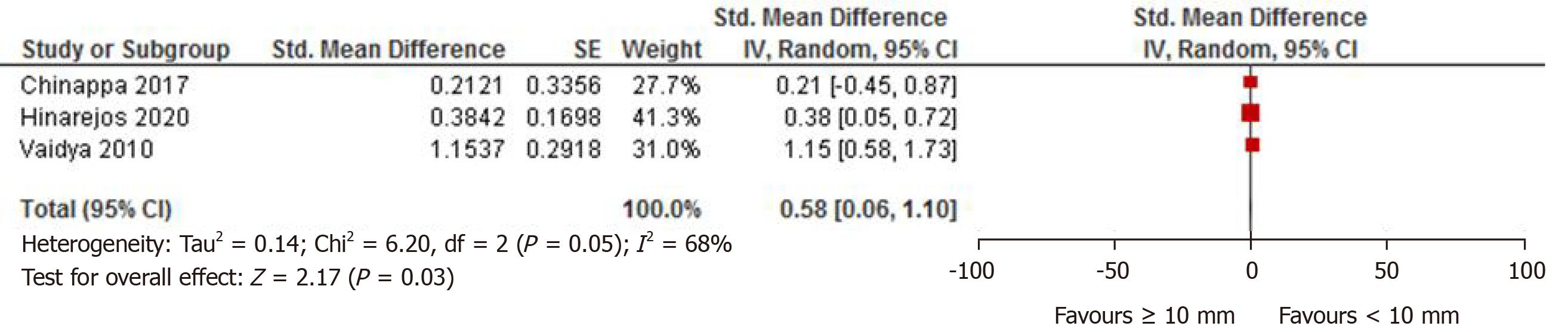
Of 45 retrieved studies, qualitative and quantitative assessment of data was performed from eight studies and six studies, respectively. Five studies (n = 1551) reported the average limb lengthening of 5.98 mm. The LLD after TKA was ranging from 0.4 ± 10 mm to 15.3 ± 2.88 mm. The incidence of postoperative radiographic LLD was reported in 44% to 83.3% of patients. There was no difference in the preoperative and postoperative LLD (MD -1.23; 95%CI: -3.72, 1.27; P = 0.34). Pooled data of two studies (n = 219) revealed significant limb lengthening in valgus deformity than varus (MD -2.69; 95%CI: -5.11, 0.27; P = 0.03). The pooled data of three studies (n = 611) showed significantly worse functional outcome in patients with LLD of ≥ 10 mm compared to < 10 mm (standard MD 0.58; 95%CI: 0.06, 1.10; P = 0.03).
Limb lengthening after TKA is common, and it is significantly more in valgus than varus deformity. Significant LLD (≥ 10 mm) is associated with suboptimal functional outcome.
Core Tip: Limb length inequality following total knee arthroplasty (TKA) is an important cause of patient dissatisfaction. This meta-analysis evaluated the limb length discrepancy (LLD) and its impact on the functional outcome following TKA. Five studies (n = 1551) reported the average limb lengthening of 5.98 mm. The LLD after TKA was ranging from 0.4 ± 10 mm to 15.3 ± 2.88 mm. There was no difference in the preoperative and postoperative LLD (MD -1.23; 95%CI: -3.72, 1.27; P = 0.34). Pooled data of two studies (n = 219) revealed significant limb lengthening in valgus deformity than varus (MD -2.69; 95%CI: -5.11, 0.27; P = 0.03). The pooled data of three studies (n = 611) showed significantly worse functional outcome in patients with LLD of ≥ 10 mm compared to < 10 mm (standard MD 0.58; 95%CI: 0.06, 1.10; P = 0.03). Most of the patient's limb gets lengthened after TKA; however, it affects the functional outcome when the LLD is more than equal to 10 mm.
- Citation: Tripathy SK, Pradhan SS, Varghese P, Purudappa PP, Velagada S, Goyal T, Panda BB, Vanyambadi J. Limb length discrepancy after total knee arthroplasty: A systematic review and meta-analysis. World J Clin Cases 2021; 9(2): 357-371
- URL: https://www.wjgnet.com/2307-8960/full/v9/i2/357.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i2.357
Despite the advancement in technology and a better understanding of total knee arthroplasty (TKA), nearly 15%-20% of patients remain dissatisfied after surgery[1,2]. Many studies have reported that there is a discrepancy in the patient-reported outcome, and physicians reported outcome after TKA. The clinical and functional outcomes, as reported by the physicians, are higher than the patients reported outcome[1-3]. Although many factors may contribute to this disparity, limb length discrepancy (LLD) is one of the crucial issues, and it has not been adequately studied[4]. Unlike total hip arthroplasty, where the limb length can be adjusted with implant modifications and surgical techniques, it is least modifiable in TKA. The principle of TKA involves minimal bone resection and ligament balancing with equal flexion-extension gap, and hence limb length alteration is unavoidable[5]. The change in limb length is not commonly measured after TKA; nevertheless, LLD has been shown to increase the incidences of back pain, radiculopathy, gait disorders, and general dissatisfaction[6-10].
The patient may perceive the gait modification after unilateral TKA as an unacceptable outcome. It has been proven that mechanical load and isometric torque is more on the longer limb, and it has a negative impact on the nearby joints. There may be precipitations of low back pain, hip pain because of arthritic changes and also compensatory pelvis and spinal curvature changes[6-10]. There are limited studies in literature till date evaluating LLD after TKA[11-18]. While few studies reported LLD as a common occurrence after TKA[11-14], others reported that radiographic LLD is uncommon[15-17]. Recently, few researchers have reported radiographic LLD of ≥ 10 mm as a clinically relevant change[16,17]. Contrary to it, the perceived LLD has been given more weightage in a few studies[15,16]. Therefore, this systematic review and meta-analysis were conducted to evaluate the incidence of radiographic LLD and its impact on functional outcome following TKA.
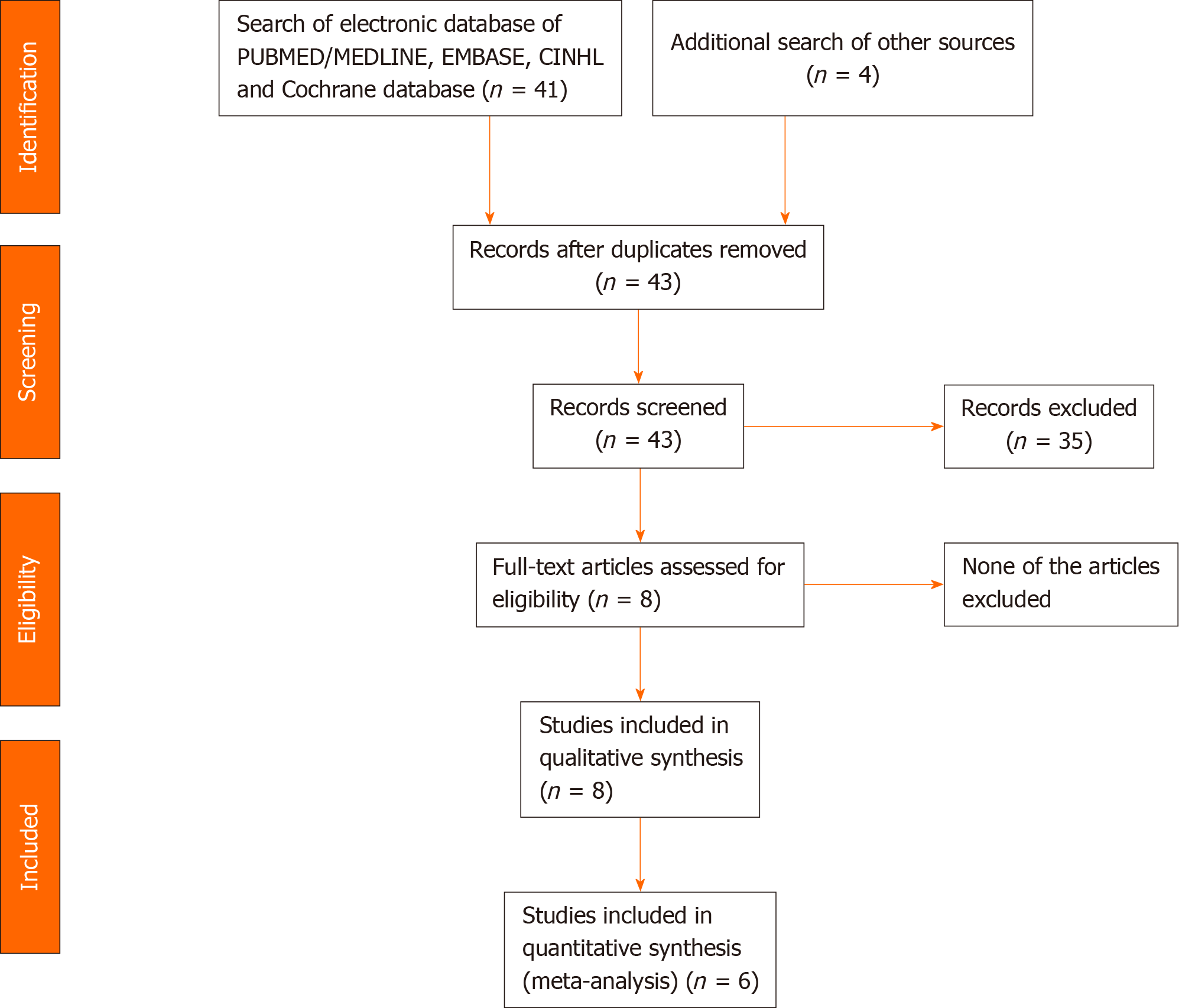
This systematic review was performed with a predefined protocol using the (Patients, Intervention, Comparison and Outcome) PICO format. The review was conducted and presented according to Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) statement standards (Figure 1). This systematic review was registered in PROSPERO (Regd. No. CRD42020193434).
All randomized-controlled trials and observational studies that evaluated the limb length alteration or LLD after TKA surgeries were included for review.
Patients operated with unilateral or bilateral TKA with measurement of lower limb length in the preoperative period and postoperative period were included. The patients operated with revision knee arthroplasty, associated extra-articular deformity, previous knee surgery or lower limb bony procedures were excluded.
All patients should have undergone TKA (either conventional Jig based surgery or navigation or robotic-assisted) with any surgical approach using either cruciate-retaining or posterior stabilized implant. The principle of TKA should be either gap balancing or measured resection technique.
The primary outcome measure was assessment of limb lengthening/LLD after TKA. The secondary outcome measures included assessment of LLD in varus/valgus deformities and unilateral/bilateral TKA. The other measures were assessment of perceived LLD and the impact of LLD on functional outcome.
Definitions of outcome measures: Limb lengthening refers to increase in limb length compared to its preoperative state measured either by clinical method or radiographic method. LLD is the difference in the length of the affected limb (operated with TKA) compared to the contralateral limb (either operated with TKA or a non-operated limb). If the operated knee was lengthened, a plus sign (+) was assigned, and if it was shortened, a minus (-) sign was allotted before the parameter. Perceived LLD indicates the perception of an individual about the limb length variation.
A literature search was performed by two authors (SKT, BBP) to identify all studies related to limb length variation/discrepancy following TKA. The electronic databases of PubMed/Medline, Embase, CINAHL and the Cochrane Central Register of Controlled Trials were searched using the keywords “limb length”, “limb-lengthening”, “LLD”, “TKA” and “total knee replacement”. The last search was performed on 22nd June 2020. The search was restricted to the English language. The title and abstract of retrieved articles were assessed for possible inclusion in the review. The bibliographic lists of the relevant articles and reviews were also searched for further potentially eligible. We resolved any discrepancies in study selection by a discussion between the authors. A third independent author (PV) was consulted in the event of disagreement (Figure 1).
Data extraction was done using a data extraction form, and two authors (SSP, PV) independently extracted data from eligible studies (author, year of publication, study design, intervention, follow up, outcome). Any disagreement was resolved through the discussion with a third author (SKT).
The methodological quality and risk of bias of the included articles were assessed independently by two authors (SKT, BBP) using the Newcastle–Ottawa scale (NOS)[19] (Table 1). The NOS uses a star system with a maximum of nine stars to evaluate a study in three domains (8 items): The selection of the study groups, the comparability of the groups, and the ascertainment of the outcome of interest. Each item was allocated one star for low risk and no star for high risk. Studies that received a score of nine stars were considered as low risk of bias, seven or eight stars as moderate risk, and six or less as high risk of bias. Disagreements were resolved by discussion between the two reviewers. If no agreement could be reached, the opinion of a third author (TG) was sought.
| Ref. | Selection | Comparability | Outcome | |||||||
| Representativeness of exposed cohort | Selection of nonexposed cohort | Ascertainment of exposure | Demonstration that outcome of interest was not present at start of study | Adjust for the most important risk factors | Adjust for other risk factors | Assessment of outcome | Follow-up length | Loss to follow-up rate | Total quality score | |
| Postoperative limb length | Preoperative limb length | TKA | Limb lengthening/LLD | Age, sex, BMI | Varus/valgus deformity, KL grade etc. | Limb length change | Any postoperative period | < 20% | ||
| Vaidya et al[11], 2010 | + | + | + | + | - | - | + | + | + | 7 (moderate risk) |
| Lang et al[12], 2012 | + | + | + | + | + | + | + | + | + | 9 (low risk) |
| Chang et al[13], 2013 | + | + | + | + | + | + | + | + | + | 9 (low risk) |
| Tipton et al[14], 2015 | + | + | + | + | + | + | + | + | + | 9 (low risk) |
| Kim et al[4], 2015 | + | + | + | - | + | + | - | + | + | 7 (moderate risk) |
| Goldstein et al[15], 2016 | + | + | + | + | + | + | - | + | + | 8 (moderate risk) |
| Chinnappa et al[16], 2017 | + | + | + | + | + | + | + | + | + | 9 (low risk) |
| Hinarejos et al[17], 2020 | + | + | + | + | + | + | + | + | + | 9 (low risk) |
Data were analyzed using Review Manager (RevMan) V.5.1[20]. Data were pooled and expressed as mean difference (MD) with 95%CI in case of continuous data. The odds ratio (OR) with 95%CI was calculated in categorical data. All the analyses were performed by Generic Inverse Variance method using random-effects weighting, where the log RRs (relative risk) for cohort studies or log ORs for case-control studies were weighted by the inverse of the variance to obtain a pooled RR estimate[21]. A P < 0.05 was considered statistically significant. Inter-study heterogeneity was assessed by Cochrane's Q (χ2 P < 0.10) and quantified by I2. I2 greater than 25% was considered as low heterogeneity, 50% as moderate, and > 75% as high heterogeneity. In order to address the high degree of heterogeneity, a random MD was calculated[22,23].
Searches of electronic database identified 45 studies, of which eight studies were eligible for review (Figure 1). Fours studies were retrospective cohorts, and four were prospective studies. Six studies followed the PICO format and recruited osteoarthritis (OA) knee patients with predefined inclusion and exclusion criteria. They evaluated the limb lengthening/LLD or collected the data after the intervention (TKA). One study collected the data in a reverse way. They divided the patients into two LLD groups (> 15 mm vs ≤ 15 mm) and compared the parameters between them. Another study was totally focussed on perceived LLD (Table 2). The assessment of bias using the NOS scale revealed moderate bias in three studies and low bias in the other five studies (Table 1).
| Ref. | Inclusion/exclusion criteria | No of knees (UL, BL) | Study design | Age in years ± SD (range) | Sex (M:F) | BMI (Kg/m2) | Intervention (TKA) | Follow up |
| Vaidya et al[11], 2010 (level IV) | BL OA knee with varus deformity, operated for unilateral or bilateral TKA with minimum 6 mo follow up (n = 54 pts) | 30 UL | Cohort retrospective | 64 (48-80) | 7:23 | - | Mid-vastus approach; PFC sigma RP-F Highflex (56), PFC Sigma RP (26), IB II Zimmer (2); Patella replaced | Minimum 6 mo |
| 30 BL (six pts underwent stage wise TKA, included in both groups) | Cohort retrospective | 65.8 (54-83) | 6:24 | - | Minimum 6 mo | |||
| Lang et al[12], 2012 (level III) | BL OA knee (both varus and valgus) without significant extraarticular deformity (n = 102 pts) | 102 (54 UL, 47 BL) | Cohort retrospective | 70.3 ± 9.9 | 35:67 | 30.0 ± 6.4 | Medial parapatellar approach, principles of flexion/extension gap balancing85 CR and 17 PS | 6 wk |
| Chang et al[13], 2013 (level III) | Inclusion: TKA for primary OA knee with one year follow up. Exclusion: Pts with previous surgery on the ipsilateral limb, spine surgery, neurological disorders, cancer, death due to diseases unrelated to TKA, periprosthetic infection, or another condition capable of affecting the result of this study, such as depression, dementia, or problems of the contralateral knee were excluded (n = 466 pts) | 761 knees (171 UL, 295 BL, 466 patients) | Cohort Retrospective study (prospectively collected data) | 67.9 ± 5.9 (49–84) | 26:440 | 27.1 ± 3.4 | Medial parapatellar approach, patella replaced | 1 yr |
| Tipton et al[14], 2015 (level III) | Inclusion: Primary TKA with availability of both preoperative and postoperative standing full-length radiographs for measurement. Exclusion: Patients with gross bony deformities or poor quality radiographs were excluded (n = 137) | 137 UL | Cross sectional Prospective study | 68 ± 10 | 40:82 | 30 ± 5.0 | Medial parapatellar approach, minimal bone resection with thinnest poly-insert | Postoperative setting |
| Kim et al[4], 20151 (level IV) | Inclusion: Primary computer-assisted TKA in OA knee with varus deformity. Exclusion: Varus > 20°, hip pathology, osteotomy in the affected limb, severe bony defects, severe osteoporosis, flexion contracture > 30°, BMI > 30 kg/m2, and spine deformity with pelvic tilt | 148 (≤ 15 mm LLD in 81 knees, 55 pts; > 15 mm LLD in 67 knees, 52 pts) | Cohort retrospective | ≤ 15 mm: 69.1 ± 6.7; > 15 mm: 70.1 ± 8.4 | 15:133 | ≤ 15 mm: 26.3 ± 3.2; > 15 mm: 27.1 ± 3.6 | Mid-vastus approach, Orthopilot navigation system. PS implant. No patella resurfacing | Minimum 2 yr |
| Goldstein et al[15], 2016 (level III) | Inclusion: Primary TKA for unilateral osteoarthritis between 18-90 yr of age. Exclusion: Pts with allergy or intolerance to the study materials, previous surgeries on the ipsilateral or contralateral joints or limbs likely to affect the outcome, substance abuse or dependence within the past 6 mo (n = 71) | 71 UL | Cross sectional prospective study | 65 ± 8.4 (47-89) | 27:44 | 35.1 ± 9.9 (20.2-74.8) | Medial parapatellar or midvastus approach | 1 yr |
| Chinnappa et al[16], 2017 (level II) | Inclusion: Primary unilateral TKA without extraarticular deformity (n = 91). Exclusion: Patients with known leg length inequality due to other causes (radiographic leg lengthening post THA > 5 mm and longstanding leg length inequality > 5 yr requiring orthotics) were excluded. | 91 UL | Cohort. Prospective study | 70.2 ± 8.9 (50-89) | 34:57 | 29.4 ± 5.0 (17.5–48.6) | Medial parapatellar approach, aim to restore neutral HKA axis. PS implant. Bone resection using Jig or computer navigation | Radiographic measurement on second postoperative day, functional outcome at 6 mo |
| Hinarejos et al[17], 2020 (level II) | Inclusion: Unilateral primary TKA. Exclusion: Pts with previous fractures of the lower limbs, patients with surgeries or diseases affecting any of the hips or ankles, preoperative or postoperative flexion contracture > 5°, poor quality radiographs, patients without postoperative KSS evaluation (n = 460) | 460 UL | Cohort. Prospective study | 71 ± 8.4 | 128:332 | 31.3 ± 4.9 | Medial parapatellar approach; intramedullary guide for femur and extramedullary jig for tibia, minimal bone resection with thinnest insert. CR in 30.4%, PS in 69.6%. Patella replaced | At 6 mo, radiographic evaluation; at 1 yr, functional evaluation |
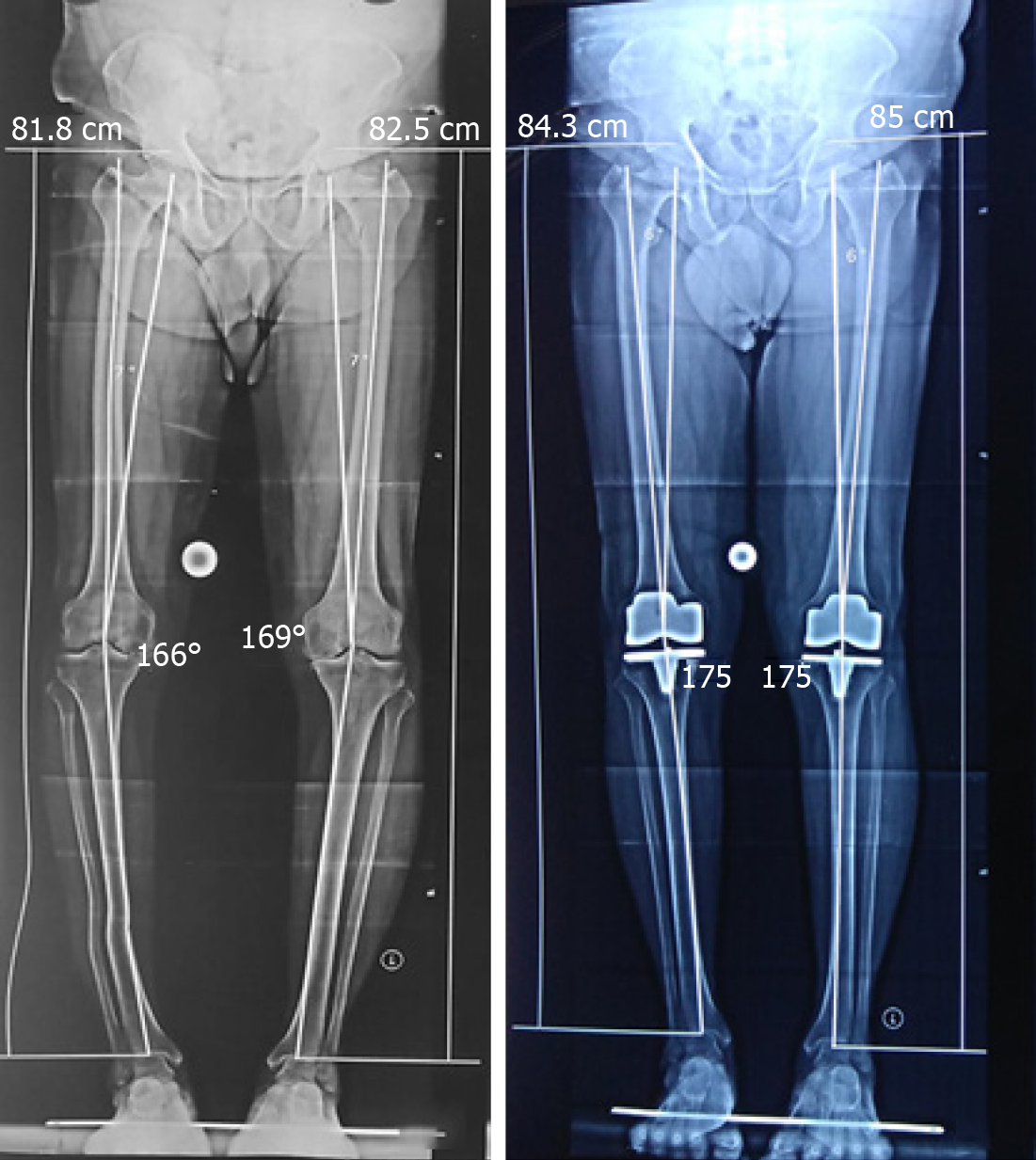
Five studies (n = 1551 knees) provided numeric data about the extent of limb length increase in the postoperative period of TKA[12-14,16,17]. Overall, the limb was lengthened after TKA, and the average value of lengthening was 5.98 mm. There was a clinically relevant lengthening of ≥ 10 mm in 8.26% to 83.33% of patients after TKA (Figure 2).
Five studies mentioned about LLD after TKA[11-13,16,17]. The LLD after TKA was ranging from 0.4 ± 10 mm to 15.3 ± 2.88 mm. The incidence of radiographic LLD after TKA was reported in 44% to 83.3% of patients. One study considered ≥ 10 mm as a relevant radiographic LLD and reported only 11% incidence of postoperative radiographic LLD taking 10 mm as the cut-off point[16]. One study considered > 15 mm as clinically relevant and observed 45% of patients with significant postoperative LLD[4] (Tables 3 and 4).
| Ref. | Deformity (degree) | Pre-op LLD (mm) | Postop LLD (mm) | % of patients with limb lengthening/LLD | Limb lengthening (mm) | % of patients with perceived postop LLD | Factor affecting radiographic LLD/remarks | ||
| Preop | Postop | Change in alignment | |||||||
| Vaidya et al[11], 2010 | - | - | - | 15.3 ± 2.88 | 83.3 (≥ 10 mm in all) | 8 (26.7) | LLD is more common after unilateral TKA than bilateral. LLD of ≥ 2 cm is perceived by patient after unilateral TKA. LLD affects the functional outcome after UL TKA in BL OA knee with varus deformity | ||
| - | - | - | 5 ± 2.01 | 46.66 (≥ 10 mm in all) | 0 | ||||
| Lang et al[12], 2012 | 2.5 | 1 | 1.5 | - | 2 (95%CI: 0.5-3.5) | 83.3% | 6.3 ± 6.85 (range -11-24) | - | Limb lengthening is frequent after TKA and is almost similar to that of nonoperative limb. Limb lengthening had no relationship with age (P = 0.864), sex (P = 0.514), BMI (P = 0.548), or constraint type (P = 0.849), contralateral OA knee severity. LLD in bilateral TKA is minimal but it is significantly different in unilateral TKA |
| Chang et al[13], 2013 | 11.9 ± 5.5º (37o to -9º) | 1.5 ± 2.7 (11o to -6o) | 10.4 | 6 ± 5 | 5 ± 4 | 43.9% limb lengthening by ≥ 10 mm, 3.4% limb shortening of ≥ 10 mm | 9 ± 1.1 | - | Greater LL increase was correlated with a greater preoperative HKA angle and smaller BMI. Preoperative flexion contracture, postoperative flexion contracture and postoperative HKA have no correlation to LL. Limb length, height, and weight increased, BMI remained unchanged, and LLD decreased 1 year after TKA. The bilateral group had a greater height increase and lower rate of LLD |
| Tipton et al[14], 2015 | 4.16 | 2.76 | 1.40 | - | - | 59.1% | 4.28 ± 1.11, 59% reported increase in limb length by 4.38 mm | There was no correlation BMI with limb length. Limb lengthening after TKA does not frequently occur to a statistically significant extent, regardless of preoperative joint state | |
| Goldstein et al[15], 2016 | - | - | - | - | - | - | - | 10% | Perceived LLD is common in patients undergoing TKA and it decreases after surgery. About 10% of patients perceive a LLD after surgery and it usually resolves with time. Age, BMI, Preoperative and postoperative mechanical axis and preoperative perceived LLD has no correlation with postoperative perceived LLD |
| Chinnappa et al[16], 2017 | -3.1 | 0.8 | 3.9 | -3.0 ± 8.0 | 0.4 ± 10 | 77% (≥ 10 mm in 11%) | 3.5 ± 8.4 (77% lengthened: Mean 6.7 ± 4.9 mm; 23% shortened: Mean -7.4 ± 8.5) | 14% | Radiographic LLD is uncommon after TKA. It has no correlation with age, sex, BMI, polyethylene insert thickness, pre-operative FFD, post-operative FFD, contralateral knee OA, or arthroplasty, severity of pre-operative angular deformity or degree of angular correction. Post-operative radiographic LLD is associated with increased preoperative LLD (P < 0.001). Perceived post-operative LLD was associated with female gender (P = 0.02), decreased satisfaction (18% vs 84%, P < 0.001) and poorer functional score |
| Hinarejos | 5.5 ± 7.7 | 3.7 ± 3.8 | 1.8 | -1.1 ± 6.4 | 0.8 ± 6.1 | 60% (≥ 10 mm in 8.26%) | 1.9 ± 8.84 | Increased LLD has no correlation with age, gender, BMI, HKA angles or with preoperative knee function. However HKA angle changes correlate with LLD. Significant LLD is not frequent after TKA, but the functional results of the surgery can be suboptimal when it is present | |
| Ref. | Type of deformity | ||||||||||
| Varus | Valgus | ||||||||||
| No of knees | Preop varus | Postop varus (o) | Change in angle | Average lengthening | No of knees | Preop varus (o) | Postop varus (o) | Change in angle | Average lengthening | ||
| Lang et al[12], 2012 | 66 | 8.7 ± 4.6 | 2.1± 2.5 | -6.6 | 5.2 ± 5.8 (S) | 36 | -8.9 ± 5.9 | -1.1 ± 3.3 | -7.8 | 8.4 ± 8.2 (S) | |
| Tipton et al[14], 2015 | 87 | 9.34 ± 4.66 | 4.86 ± 3.03 | -4.99 (4.77) | 3.77 ± 11.1 (S) | 45 | -6.67 ± 5.79 | -0.468 ± 3.57 | -6.08 ± 5.72 | 5.56 ± 11.3 (S) | |
| Severity of deformity | |||||||||||
| -10 to 10 degree | < -10 (valgus) | > 10 (varus) | |||||||||
| No of knees | Limb length change | No of knees | Limb length change | No of knees | Limb length change | ||||||
| Lang et al[12], 2012 | 65 | 4.7 ± 6.4 (S) | 12 | 12 ± 8.6 (S) | 25 | 7.9 ± 5.2 (S) | |||||
| Tipton et al[14], 2015 | 93 | 1.64 ± 10.3 (NS) | 9 | 15.1 ± 10 (NS) | 35 | 8.51 ± 10.7 (NS) | |||||
| Unilateral or bilateral TKA | |||||||||||
| Unilateral TKA | Bilateral TKA | ||||||||||
| No of knees | LLD | No of knees | LLD | ||||||||
| Vaidya et al[11], 2010 | 30 | 15.3 ± 2.88 | 30 | 5 ± 2.01 (S) | |||||||
| Lang et al[12], 2012 | 54 | 3.0 (95%CI: 0.5-5.4, NS) | 47 | 0.9 (95%CI: −0.9-2.7, NS) | |||||||
| Chang et al[13], 2013 | 171 | 6 ± 4 | 295 | 5 ± 4 (S) | |||||||
| Severity of OA in contralateral nonoperative limb/ipsilateral limb in preoperative period | |||||||||||
| KL 1, 2 | LLD (mm) | No of knees in KL 3, 4 | LLD (mm) | ||||||||
| Lang et al[12], 2012 | Contralateral knee OA status (n = 26) | 2 ± 5 | Contralateral limb status (n = 28) | 3.9 ± 11.5 (NS) | |||||||
| Tipton et al[14], 2015 | Ipsilateral preop knee OA status | -2.00 ± 8.87 (only limb lengthening) | Ipsilateral preop knee OA status | 0.594 ± 1.11 (NS) | |||||||
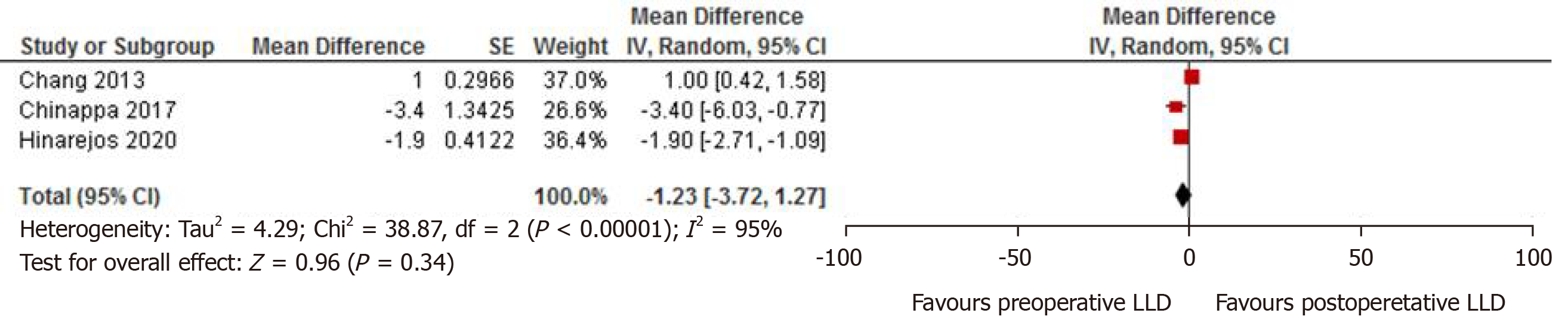
Three studies (n = 1017) mentioned the preoperative LLD[13,16,17]. The value of preoperative LLD was ranging from -3 ± 8 mm to 6 ± 5 mm. Pooled analysis of these studies revealed no significant difference in preoperative and postoperative LLD (MD -1.23; 95%CI: -3.72, 1.27; P = 0.34). There was significant heterogeneity among these studies (I2 = 95%, P < 0.00001) and hence random mean values were assessed (Figure 3).
Three studies mentioned about perceived LLD[11,15,16]. The incidence of perceived LLD in the preoperative period varies from 16% to 25%. Postoperative perceived LLD varies between 10% and 26.66%. However, the perception of postoperative LLD improved over time, and one study reported complete resolution of perception after an average duration of 8.5 wk[15].
Age/sex: Five studies assessed the impact of age on limb length variation or LLD[4,12,15,16,17]. There was no significant association between LLD and age. Three studies evaluating the association of gender on radiographic LLD did not find a significant association[15-17]. One study reported a significant association between perceived LLD and female gender[16].
Body mass index: Seven studies evaluated the association between body mass index (BMI) and LLD[4,12-17]. Six studies did not find any association between BMI and LLD/ limb length variation[4,12,14-17]. One study reported increased limb length with smaller BMI[13].
OA grade: Two studies reported the grade of OA[12,14]. One study reported the LLD of 3.9 ± 11.5 mm in patients with contralateral knee OA of Kellgren and Lawrence (KL) grade 3, 4 compared to 2 ± 5 mm in contralateral KL grade 1 and 2[12]. Another study also reported -2.00 ± 8.87 mm limb lengthening in the ipsilateral knees with preoperative KL grade 1, 2 and 0.594 ± 1.11 mm in KL grade 3 and 4[14] (Table 4).
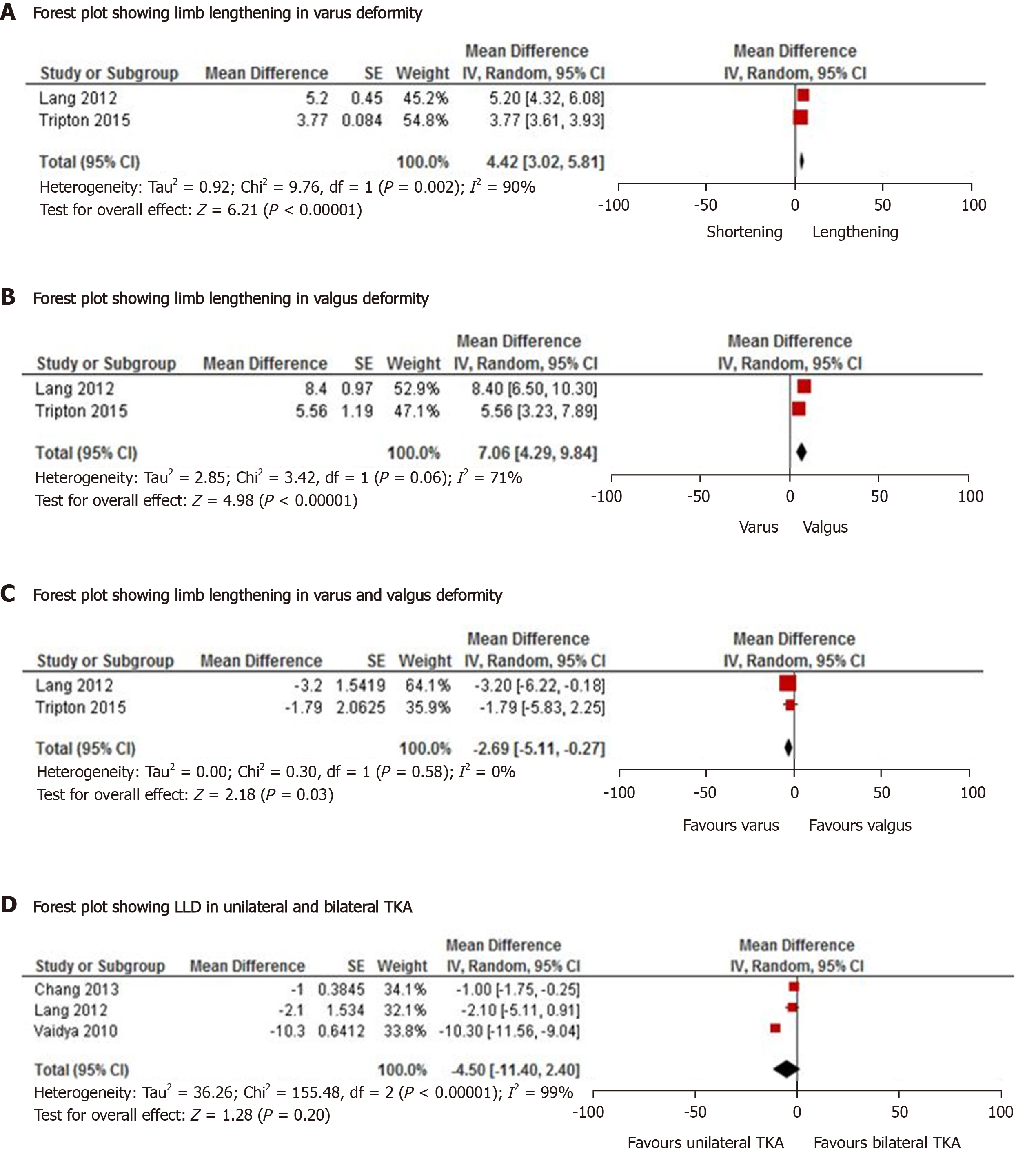
Preoperative deformity: Two studies (n = 239) evaluated the limb length alteration in varus (n = 153) and valgus (n = 101) deformity (Figure 4A and B)[12,14]. The average increase in limb-length in valgus deformity (mean 7.06; 95%CI: 4.29, 9.84) was significantly higher than varus deformity (mean 4.42 mm; 95%CI: 3.02, 5.82) (Figure 4A-C). However, there was a high degree of heterogeneity among the studies (I2 = 90%). One study reported limb length increase of 4.7 mm for every 10-degree correction of varus deformity and 6.2 mm for every 10-degree correction of the valgus deformity[12] (Table 4).
Unilateral vs bilateral: Three studies (n = 617) compared the LLD in unilateral TKA and bilateral TKA[11-13]. All these studies reported a higher LLD following unilateral TKA (n = 255) than bilateral (n = 372). The pooled data of three studies comparing unilateral TKA and bilateral TKA noted no significant difference in LLD (MD 4.5 mm, 95%CI: 11.4, 2.40; P = 0.20). However, there was a high degree of heterogeneity among the studies (I2 = 99%, P < 0.001) (Figure 4D).
Correlation of radiographic parameters with perceived LLD: One study evaluated the correlation of radiological LLD to perceived LLD[16]. Clinically relevant LLD of ≥ 10 mm was noted only in 11% of patients, whereas perceived LLD was observed in 21% of patients[16]. Another study did not find any correlation of change in mechanical axis to perceived LLD[15].
Four studies reported the effect of LLD on functional outcome[4,11,16,17] (Table 5). The study by Kim et al[4] categorized their patients into > 15 mm vs ≤ 15 mm[4]. They reported a significantly inferior outcome in patients with LLD of > 15 mm. The data of the remaining three studies (n = 611) were pooled to look for the functional outcome in patients with LLD of < 10 mm (n = 453) vs ≥ 10 mm (n = 158). The functional outcome [Knee society score (KSS) function] was significantly worse in patients with LLD of ≥ 10 mm (standard MD 0.58; 95%CI: 0.06, 1.10; P = 0.03). There was moderate heterogeneity among the studies (I2 = 68%, P = 0.05) (Figure 5).
| Ref. | Functional score | Functional outcome | LLD vs functional outcome | Perceived LLD | Remarks |
| Vaidya et al[11], 2010 | Knee society clinical rating system | Mean score in UL group was 73 ± 16.79 (95%CI: 66.73-79.27 (range 45-100) | No LLD (5): Functional score 85; LLD 10 mm (5): functional score 83; LLD 20 mm (19): Functional score 68.16; LLD 30 mm (1): Functional score 55; < 10 mm (21): 82.1429 ± 9.439; ≥ 10 mm (39): 73.9744 ± 5.261 | 26.66% (8) pts perceived LLD; no LLD: Not perceived; LLD 10 mm: Not perceived; LLD 20 mm: 7 patients; LLD 30 mm: One patient | The functional outcome after UL TKA in BL OA knee with varus deformity is inferior to BL TKA |
| Knee society clinical rating system | Mean score in BL group was 80.67 ± 21.2 (95%CI: 72.75 -88.58, range 0-100). | No LLD (16): Functional score 81.25; LLD 10 mm (13): Functional score 80; LLD 20 mm (1): Functional score 80 | No one perceived LLD | ||
| Kim et al[4], 2015 | KSS function score | LLD > 15 mm: KSS function score 88.2 ± 7.0; LLD ≤ 15 mm: KSS function score 80.1 ± 14.7 (S); no difference in ROM, HSS, KSS knee score and WOMAC | Not evaluated | Patients with LLD of > 15 mm had significantly inferior outcome than LLD < 15 mm. Preop LLD has high risk of postop LLD. Patients with unilateral TKA have higher chances of postoperative LLD | |
| Chinnappa et al[16], 2017 | WOMAC; KSS knee; KSS; function 6 mo | LLD < 10 mm: 89% pts.; LLD ≥ 10 mm: 11% pts. a: 37.1 ± 16 in ≥ 10 mm LLD vs 30.8 ± 21.2 with < 10 mm LLD (NS); b: 37 ± 20.8 in ≥ 10 mm LLD vs 29.2 ± 35.2 with < 10 mm LLD (NS); c: 29.4 ± 21.2 in ≥ 10 mm LLD vs 23.6 ± 27.7 with < 10 mm LLD (NS) | Preoperative LLD: 16% pts. Postoperative LLD: 21% pts. a: 13.1 ± 22.6 in ≥ 10 mm LLD vs 35.5 ± 18.8 with < 10 mm LLD (S); b: 16.2 ± 26.2 in ≥ 10 mm LLD vs 31.0 ± 34.1 with < 10 mm LLD (NS); c: 15.3 ± 28.9 vs 26.1 ±27.1 (NS) | Significant radiological LLD (≥ 10 mm) after TKA is uncommon (11%) and doesn’t correlate to perceived LLD. Perceived LLD is associated with decreased satisfaction and function | |
| Hinarejos et al[17], 2020 | Function KSS | Mean preop score of 51.3 ± 13.5 improved to 80.5 ± 15.1 at 12 mo (P < 0.0001) | LLD < 10 mm (422, 91.7%): Functional score 82.3 (14.6). LLD ≥ 10 mm (38, 8.3%): Functional score 76.7 (14.0) | Not evaluated | Patients with LLD of > 10 mm had significantly worse outcome |
The main finding of this review is that limb lengthening after TKA is common with an average lengthening of 5.98 mm. The limb lengthening after TKA is significantly more in the valgus knee compared to varus knee. Assessment of pooled data regarding the impact of LLD on function revealed worse functional outcome with LLD of ≥ 10 mm. Thus LLD of ≥ 10 mm may be considered as one of the causes of dissatisfaction or poor outcome after TKA.
There is a wide variation in reporting of limb length measurement after TKA. The incidence of LLD/ limb length variations in the published studies varies between 44% and 83% of patients[11-17]. This wide variation could be because of different inclusion criteria of the patients and different methods of measurement. Vaidya et al[11] measured the limb length using measuring tape[11], and other studies evaluated the radiographic limb length. The radiographic limb length measurement is more precise and seems to be a better method[12-17]. The radiographic method of limb length measurement as proposed by Lang et al[12] has been widely used and recommended for uniformity in limb length assessment[12]. Hinarejos and his associates proposed that the presence of flexion contracture can affect the limb length[17]. Ohmori et al[24] performed a simulation study and reported the importance of “flexion contracture” and “HKA angle correction” on limb length alteration following TKA[24]. Immediate postoperative evaluation (2 d to 6 wk) for radiographic LLD can affect the limb length because of flexion attitude of the limb. Hence, the timing of limb length measurement has an impact on LLD, and the ideal time should be after six weeks when most of the residual deformities are corrected, and pain is minimal[16].
There are multiple factors that affect LLD after TKA[11,18]. Age and gender were not found to be associated with radiographic LLD in many studies[12-17]. It is difficult to comment on the impact of BMI on LLD, as few studies have omitted morbid obese patients in their series[4]. Chang et al[13] reported the association between greater LLD with smaller BMI in their series of 466 patients at one-year follow-up[13]. All studies reported a greater increase in limb length following valgus deformity than varus[12,14]. The pooled analysis of two studies reporting the limb length variation following TKA observed limb lengthening of 7.06 mm in valgus deformity vs 4.42 in varus deformity (P < 0.05)[12,14]. The LLD (MD -2.69 mm; 95%CI: -5.11, -0.27) was significantly less in varus knee compared to the valgus knee. While all three studies demonstrated a smaller LLD in bilateral TKA compared to unilateral TKA, the assessment of pooled data did not show a statistically significant difference in LLD between unilateral and bilateral cases[11-13].
Recently, the perceived postoperative LLD or the awareness of LLD among patients is getting more acceptances among the researchers[15]. It has no association with radiographic LLD[16]. Studies have shown no association between mechanical HKA angles and perceived LLD[15]. Goldstein et al[15] observed 25% preoperative LLD and only 10% in the postoperative period. Of 18 patients (25%) with preoperative LLD in their series, only one had persistent LLD in the postoperative period. They concluded that most of the preoperative LLD gets settled with surgery. In patients with persistent or newly developed postoperative LLD, complete resolution was noted within three months period[15]. Chinnappa et al[16] observed an increased incidence of postoperative LLD among female patients[16].
The pooled analysis of 611 patients revealed statistically significant inferior functional outcome in patients with radiographic LLD of ≥ 10 mm[11,16.17]. Evaluation with functional KSS in these three studies maintained the homogeneity; however, the points allocated for each question were different in the study of Chinnappa et al[16] 2017. Hence standard mean difference was taken into consideration. Kim et al[4] also observed significant functional difference among patients with better ability in terms of stair climbing and KSS functional score in patients with radiographic LLD of ≤ 15 mm[4]. However, they included only preoperative varus knee with 15 mm LLD as the cut-off point. Chinnappa et al[16] reported no significant association between radiographic LLD (≥ 10 mm) with KOOS, KSS and WOMAC score; however, the perceived LLD showed significantly lower functional score in the domains of KOOS Pain, KOOS Activities of Daily Living, KOOS Quality of Life and WOMAC functional scores[16]. There is decreased satisfaction among patients with perceived LLD.
There are certain limitations to this review. First of all, all the studies were of low to moderate evidence. The high level of heterogeneity among the studies reflects the deficiencies in the currently available evidence. Second, we could perform a limited meta-analysis because of the clinical and methodological heterogeneity. There were no uniformity in limb length assessment, data evaluation and functional outcome assessment. The strength of this review is that it is the first qualitative and quantitative synthesis of evidence on leg length discrepancy in TKA. This study clearly showed that there was a significant impact of LLD on functional outcome. LLD after TKA is probably an important but under-reported modifiable cause of dissatisfaction.
In conclusion, radiological limb lengthening is common after TKA, but it may not be clinically relevant as the limb length increase is usually below 10 mm. Significant limb lengthening of ≥ 10 mm after TKA is uncommon, but it is associated with suboptimal functional outcome. There is no correlation between radiographic LLD and perceived LLD. Patients with perceived LLD are less satisfied, and they usually have a poor functional outcome. The surgeon should be aware of such a possibility and should avoid excess limb lengthening. Probably better-designed trials on LLD in TKA can explore the deficiencies, and more research on perceived LLD can further evaluate its impact on the functional outcome.
Limb length discrepancy (LLD) following total knee arthroplasty (TKA) has not been widely studied; however, a significant LLD has been considered as one of the important reasons for an unsatisfactory outcome.
There is currently no consensus about the extent of LLD that can be considered as clinically relevant following TKA. Again, few studies did not find radiographic LLD as a prognostic factor of functional outcome and stressed upon perceived LLD. Accordingly, the available studies were searched and evaluated in this systematic review and meta-analysis.
The objective of this systematic review was to evaluate the limb lengthening or LLD after TKA. The extent of LLD in varus and valgus deformities and in unilateral and bilateral TKA was also assessed. The impacts of radiographic and perceived LLD on the functional outcome were also evaluated.
All randomized controlled trial and observational studies on LLD in TKA, published till 22nd June 2020, were systematically reviewed. The primary outcome was “limb lengthening or LLD after TKA”. The secondary outcomes included “assessment of LLD in varus/valgus deformity” and “impact of LLD on the functional outcome”. Data were analyzed using Review Manager (RevMan). Data were pooled and expressed as MD with 95%CI in case of continuous data. The odds ratio with 95%CI was calculated in categorical data. Inter-study heterogeneity was assessed by Cochrane's Q (χ2 P < 0.10) and quantified by I2. The random MD was calculated to address the high degree of heterogeneity.
Of 45 studies, qualitative and quantitative assessment of data was performed from eight studies and six studies, respectively. Five studies (n = 1551) reported the average limb lengthening of 5.98 mm. The LLD after TKA was ranging from 0.4 ± 10 mm to 15.3 ± 2.88 mm. The incidence of radiographic LLD after TKA was reported in 44% to 83.3% of patients. There was no difference in preoperative and postoperative LLD (MD -1.23; 95%CI: -3.72, 1.27; P = 0.34). Pooled data of two studies (n = 219) revealed significant limb lengthening in valgus deformity than varus (MD -2.69; 95%CI: -5.11, 0.27; P = 0.03). The pooled data of three studies (n = 611) showed significantly worse functional outcome in patients with LLD ≥ 10 mm compared to < 10 mm (standard MD 0.58; 95%CI: 0.06, 1.10; P = 0.03).
Limb lengthening after TKA is common, and it is significantly more in valgus than varus deformity. Significant LLD (≥ 10 mm) is associated with suboptimal functional outcome. There is no correlation between radiological LLD and perceived LLD. Patients with perceived LLD are less satisfied, and they usually have a poor functional outcome.
The arthroplasty surgeon should be aware of the possibility of LLD following TKA, and they should take appropriate measures to avoid significant lengthening. However, more research on perceived LLD can further evaluate its impact on the functional outcome.
| 1. | Gunaratne R, Pratt DN, Banda J, Fick DP, Khan RJK, Robertson BW. Patient Dissatisfaction Following Total Knee Arthroplasty: A Systematic Review of the Literature. J Arthroplasty. 2017;32:3854-3860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 313] [Cited by in RCA: 601] [Article Influence: 66.8] [Reference Citation Analysis (0)] |
| 2. | Choi YJ, Ra HJ. Patient Satisfaction after Total Knee Arthroplasty. Knee Surg Relat Res. 2016;28:1-15. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 287] [Cited by in RCA: 299] [Article Influence: 29.9] [Reference Citation Analysis (0)] |
| 3. | Baker PN, Rushton S, Jameson SS, Reed M, Gregg P, Deehan DJ. Patient satisfaction with total knee replacement cannot be predicted from pre-operative variables alone: A cohort study from the National Joint Registry for England and Wales. Bone Joint J. 2013;95-B:1359-1365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 118] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Kim SH, Rhee SM, Lim JW, Lee HJ. The effect of leg length discrepancy on clinical outcome after TKA and identification of possible risk factors. Knee Surg Sports Traumatol Arthrosc. 2016;24:2678-2685. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 5. | Dunbar MJ, Richardson G, Robertsson O. I can't get no satisfaction after my total knee replacement: rhymes and reasons. Bone Joint J. 2013;95-B:148-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 174] [Cited by in RCA: 201] [Article Influence: 16.8] [Reference Citation Analysis (0)] |
| 6. | Plaass C, Clauss M, Ochsner PE, Ilchmann T. Influence of leg length discrepancy on clinical results after total hip arthroplasty--a prospective clinical trial. Hip Int. 2011;21:441-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 59] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 7. | Röder C, Vogel R, Burri L, Dietrich D, Staub LP. Total hip arthroplasty: leg length inequality impairs functional outcomes and patient satisfaction. BMC Musculoskelet Disord. 2012;13:95. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 66] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 8. | Edeen J, Sharkey PF, Alexander AH. Clinical significance of leg-length inequality after total hip arthroplasty. Am J Orthop (Belle Mead NJ). 1995;24:347-351. [PubMed] |
| 9. | Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87:155-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 207] [Cited by in RCA: 251] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 10. | Wylde V, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC, Blom AW. Prevalence and functional impact of patient-perceived leg length discrepancy after hip replacement. Int Orthop. 2009;33:905-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 129] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 11. | Vaidya SV, Patel MR, Panghate AN, Rathod PA. Total knee arthroplasty: Limb length discrepancy and functional outcome. Indian J Orthop. 2010;44:300-307. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Lang JE, Scott RD, Lonner JH, Bono JV, Hunter DJ, Li L. Magnitude of limb lengthening after primary total knee arthroplasty. J Arthroplasty. 2012;27:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 13. | Chang MJ, Kang YG, Chang CB, Seong SC, Kim TK. The patterns of limb length, height, weight and body mass index changes after total knee arthroplasty. J Arthroplasty. 2013;28:1856-1861. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 14. | Tipton S, Sutherland J, Schwarzkopf R. Change in Limb Length After Total Knee Arthroplasty. Geriatr Orthop Surg Rehabil. 2015;6:197-201. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Goldstein ZH, Yi PH, Batko B, Kearns S, Tetreault MW, Levine BR, Della Valle CJ, Sporer SM. Perceived Leg-Length Discrepancy After Primary Total Knee Arthroplasty: Does Knee Alignment Play a Role? Am J Orthop (Belle Mead NJ). 2016;45:E429-E433. [PubMed] |
| 16. | Chinnappa J, Chen DB, Harris IA, MacDessi SJ. Predictors and Functional Implications of Change in Leg Length After Total Knee Arthroplasty. J Arthroplasty 2017; 32: 2725-2729. e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Hinarejos P, Sánchez-Soler J, Leal-Blanquet J, Torres-Claramunt R, Monllau JC. Limb length discrepancy after total knee arthroplasty may contribute to suboptimal functional results. Eur J Orthop Surg Traumatol. 2020;30:1199-1204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 18. | Mufty S, Vandenneucker H, Bellemans J. The influence of leg length difference on clinical outcome after revision TKA. Knee. 2014;21:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Wells G, Shea B, O'Connell D, Robertson J, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analysis. Accessed 22nd June, 2020. Available from: https://www.researchgate.net/publication/261773681_The_Newcastle-Ottawa_Scale_NOS_for_Assessing_the_Quality_of_Non-Randomized_Studies_in_Meta-Analysis. |
| 20. | Review Manager (RevMan) [Computer program]. Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014. Accessed on 22nd June, 2020. Available from: https://www.scienceopen.com/document?vid=a73ee5f0-8d2f-4bea-9e24-d1e8cd7cfef8. |
| 21. | Schmidt FL, Oh IS, Hayes TL. Fixed- versus random-effects models in meta-analysis: model properties and an empirical comparison of differences in results. Br J Math Stat Psychol. 2009;62:97-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 419] [Article Influence: 24.6] [Reference Citation Analysis (0)] |
| 22. | Higgins JPT, Green S. Cochrane handbook for systematic reviews of interventions Version 5.0.0. The Cochrane Collaboration, 2008. Accessed on 22nd June 2020. Available from: www.cochrane-handbook.org. |
| 23. | Zlowodzki M, Poolman RW, Kerkhoffs GM, Tornetta P 3rd, Bhandari M; International Evidence-Based Orthopedic Surgery Working Group. How to interpret a meta-analysis and judge its value as a guide for clinical practice. Acta Orthop. 2007;78:598-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 24. | Ohmori T, Kabata T, Kajino Y, Inoue D, Taga T, Yamamoto T, Takagi T, Yoshitani J, Ueno T, Ueoka K, Tsuchiya H. Three-dimensional limb lengthening after total knee arthroplasty in a simulation study. Mod Rheumatol. 2018;28:1029-1034. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: India
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Prudhon JL S-Editor: Fan JR L-Editor: A P-Editor: Li JH