Published online Jun 26, 2021. doi: 10.12998/wjcc.v9.i18.4741
Peer-review started: October 27, 2020
First decision: January 17, 2021
Revised: April 21, 2021
Accepted: April 29, 2021
Article in press: April 29, 2021
Published online: June 26, 2021
Processing time: 223 Days and 21.6 Hours
Mesonephric adenocarcinoma (MNAC) is an extremely rare malignancy in the female genital tract. Only a few cases have been reported in the literature, and most of them occurred in the cervix, with extremely rare cases in the uterine body and ovary. MNAC has never been reported to arise in the fallopian tube.
A 45-year-old woman was referred to our institution with a history of abdominal pain. Ultrasound revealed a cystic and solid mass in left adnexal region. The patient underwent complete staging surgery when intraoperative pathological examination demonstrated that the mass was malignant. The final histological and immunohistochemical results confirmed the diagnosis of MNAC originating from the fallopian tube. Then she received four cycles of combination chemotherapy with carboplatin plus paclitaxel. The tumor recurred with hepatic metastases 4 mo after initial surgery, and second resection of the tumors in the liver plus partial hepatectomy was performed. She was supplemented with five courses of a new combination chemotherapy with gemcitabine plus carboplatin, and there was no evidence of recurrence within the 22-mo follow-up period after the second surgery.
MNAC originating from the fallopian tube is an extremely rare and high malignancy with a poor prognosis. It can be very aggressive, even at early stage. Little is known about the clinical characteristics, pathological diagnosis, prognosis, and optimal management strategy of MNAC originating from the fallopian tube. Herein we report the first case of primary MNAC deriving from the fallopian tube.
Core Tip: We present the first case of primary mesonephric adenocarcinoma (MNAC) deriving from the fallopian tube without sign of relapse or metastasis after second excision of recurrent lesions until now, which demonstrated a satisfactory response to combination chemotherapy of gemcitabine and carboplatin. MNAC originating from the fallopian tube can be very aggressive, even at early stage. Because of its sensitivity to the chemotherapy regimen, it is reasonable that combination chemotherapy of gemcitabine and carboplatin plays an important role in treatment of recurrent MNAC deriving from the fallopian tube. However, further research is needed to determine the effectiveness of this chemotherapy regimen and provide better therapeutic regimen.
- Citation: Xie C, Shen YM, Chen QH, Bian C. Primary mesonephric adenocarcinoma of the fallopian tube: A case report. World J Clin Cases 2021; 9(18): 4741-4747
- URL: https://www.wjgnet.com/2307-8960/full/v9/i18/4741.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v9.i18.4741
Mesonephric adenocarcinoma (MNAC) has only rarely been reported to occur in the uterine body; however, it has never been reported to arise in the fallopian tube. Ovarian adenocarcinomas that share immunophenotypic, morphologic, and molecular features with MNACs but lack association with mesonephric hyperplasia or remnants have been reported, therefore mesonephric-like adenocarcinomas (MLAs) are recently recommended to describe these neoplasms[1-3]. However, neither MNACs nor MLAs have been reported to arise in the fallopian tube up to now. Here we report the first case of primary fallopian tube MNAC (FT-MNAC) with distant recurrence after complete staging surgery combined with systemic chemotherapy, but there is no evidence of recurrence after the second resection of metastatic lesions followed by a new chemotherapy combination with gemcitabine plus carboplatin till now.
A 45-year-old woman presented to our institution with a 3-mo history of lower abdominal pain.
Vaginal examination revealed a palpable mass about 6 cm in diameter in the left adnexal area, and other physical examinations showed no abnormalities.
Laboratory examinations including the serum tumor markers were all within normal range.
Transvaginal ultrasound revealed a cystic and solid mass measuring 6.8 cm × 4.6 cm in diameter in left adnexal area.
A laparotomy was performed and the intraoperative frozen section revealed a diagnosis of malignancy. Therefore, the patient underwent a complete staging surgery. Intraoperative findings revealed that there was a solid and cystic mass measuring 7 cm in maximum diameter with irregular and friable surface, arising from the left fallopian tube. The capsule of the tumor mass was intact. The left ovary and the right adnexa were normal and not infiltrated by the tumor. No obvious tumor implants were observed in the pelvic and abdominal peritoneum, and other organ surfaces, including the liver, diaphragm, stomach, and omentum.
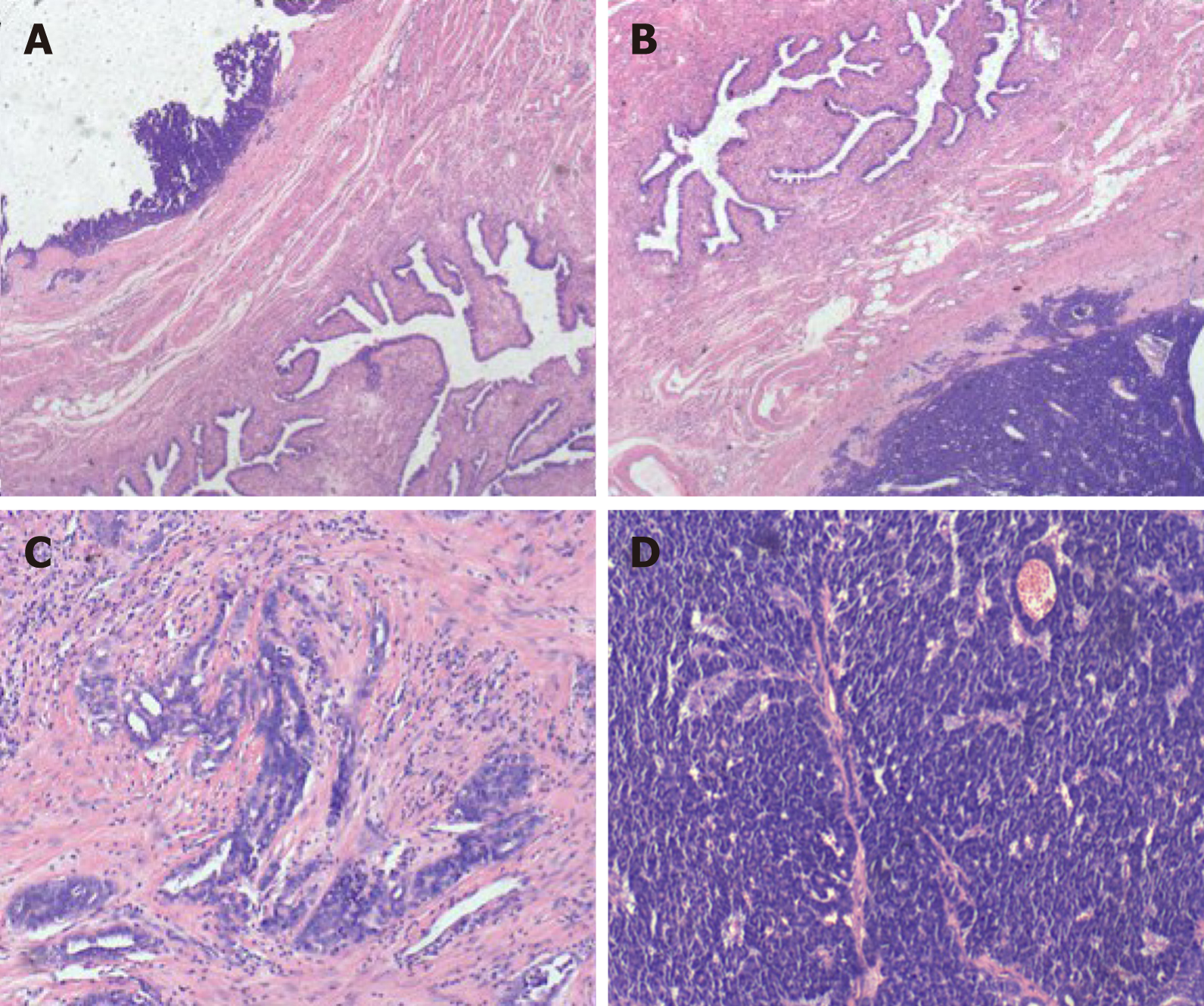
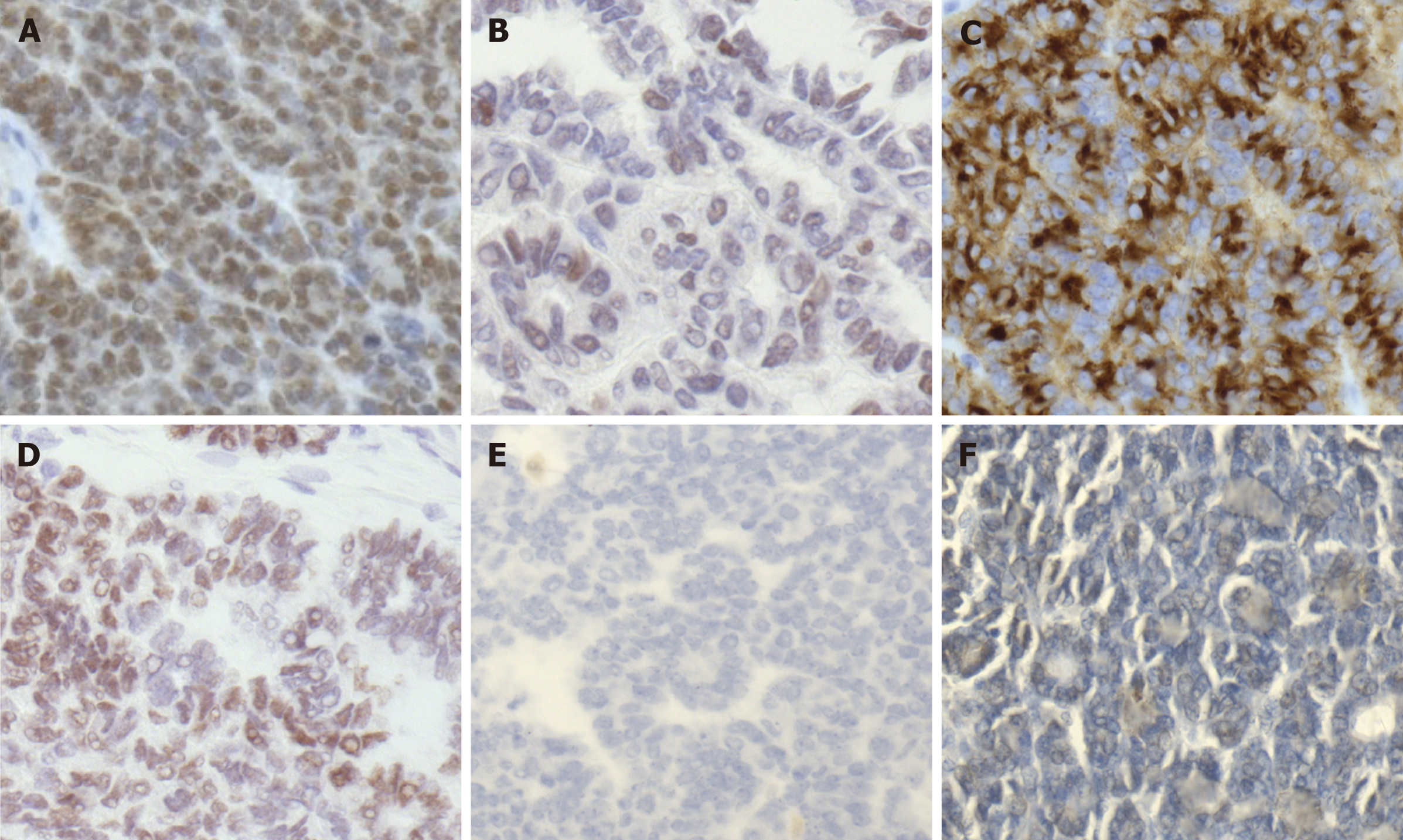
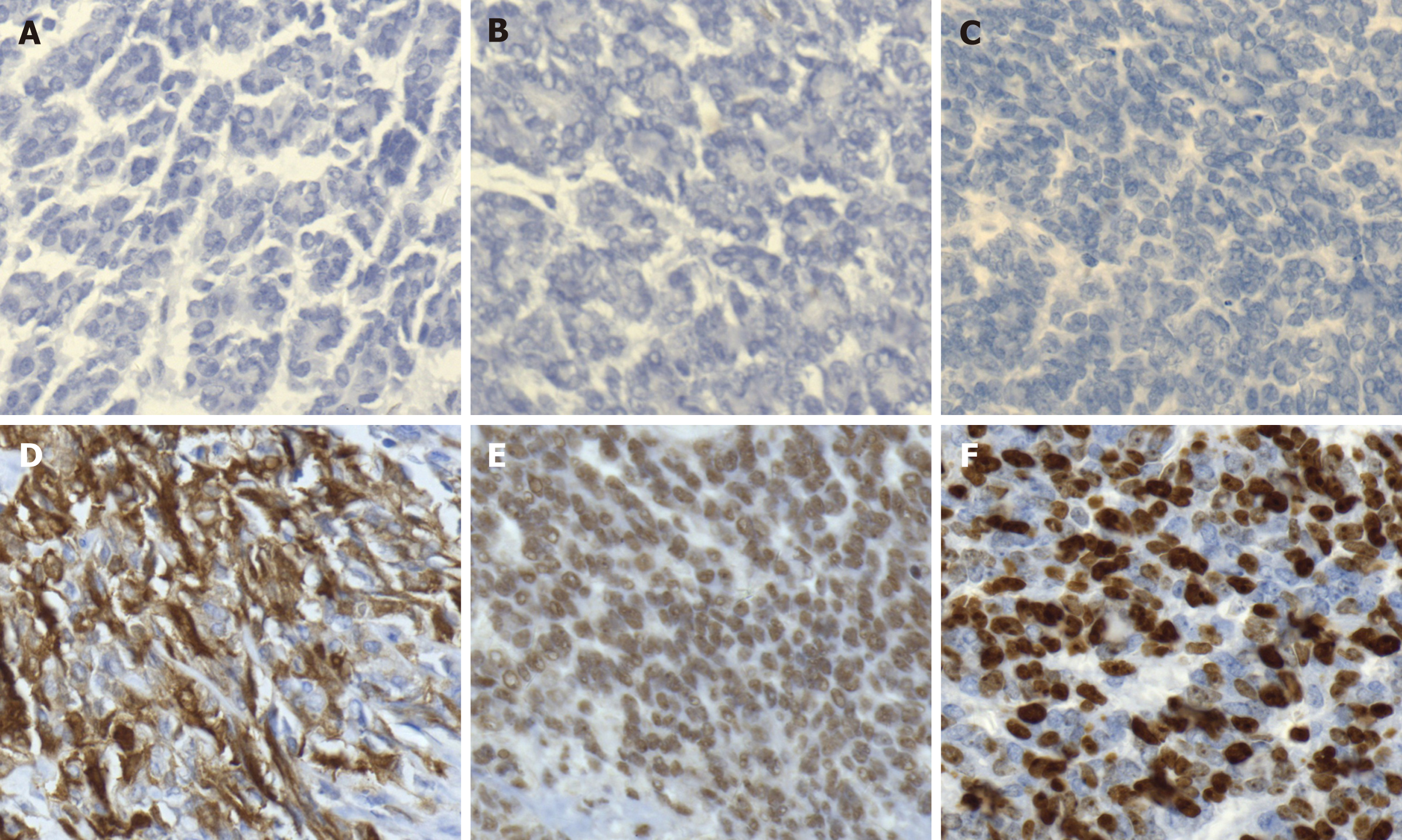
Gross examination of the excised specimen showed a mass measuring 7 cm in maximum diameter arising from the left fallopian tube wall. Histologic examination revealed that the tumor originated from the fallopian tube wall and the tumor cell involved the mucosa and serosal membrane of the fallopian tube (Figure 1A and B). Vestiges of mesonephric hyperplasia (Figure 1C) and hyperplasia into cancerous nests (Figure 1D) were histologically found. Immunohistochemical staining revealed that PAX8 expression was strong and diffuse (Figure 2A). The staining for GATA3 was weak and diffuse (Figure 2B) and CD10 revealed cytoplasmic and luminal staining (Figure 2C). The expression of thyroid transcription factor-1 was diffuse and strong (Figure 2D), but the tumors were totally negative for Calretinin (Figure 2E), Wilms' tumour-1 (Figure 2F), estrogen receptor (Figure 3A), progesterone receptor (Figure 3B), and CA125 (Figure 3C). Positive staining for P16 (Figure 3D) and P53 (Figure 3E) was detected. The positive rate of Ki-67 expression was 60%-70% (Figure 3F).
The final histological and immunohistochemical results confirmed the diagnosis of FT-MNAC. The tumor was staged as International Federation of Gynecology and Obstetrics (FIGO) stage IA.
The patient received adjuvant chemotherapy with four courses of paclitaxel (175 mg/m2) and carboplatin (300 mg/m2) after the first surgery.
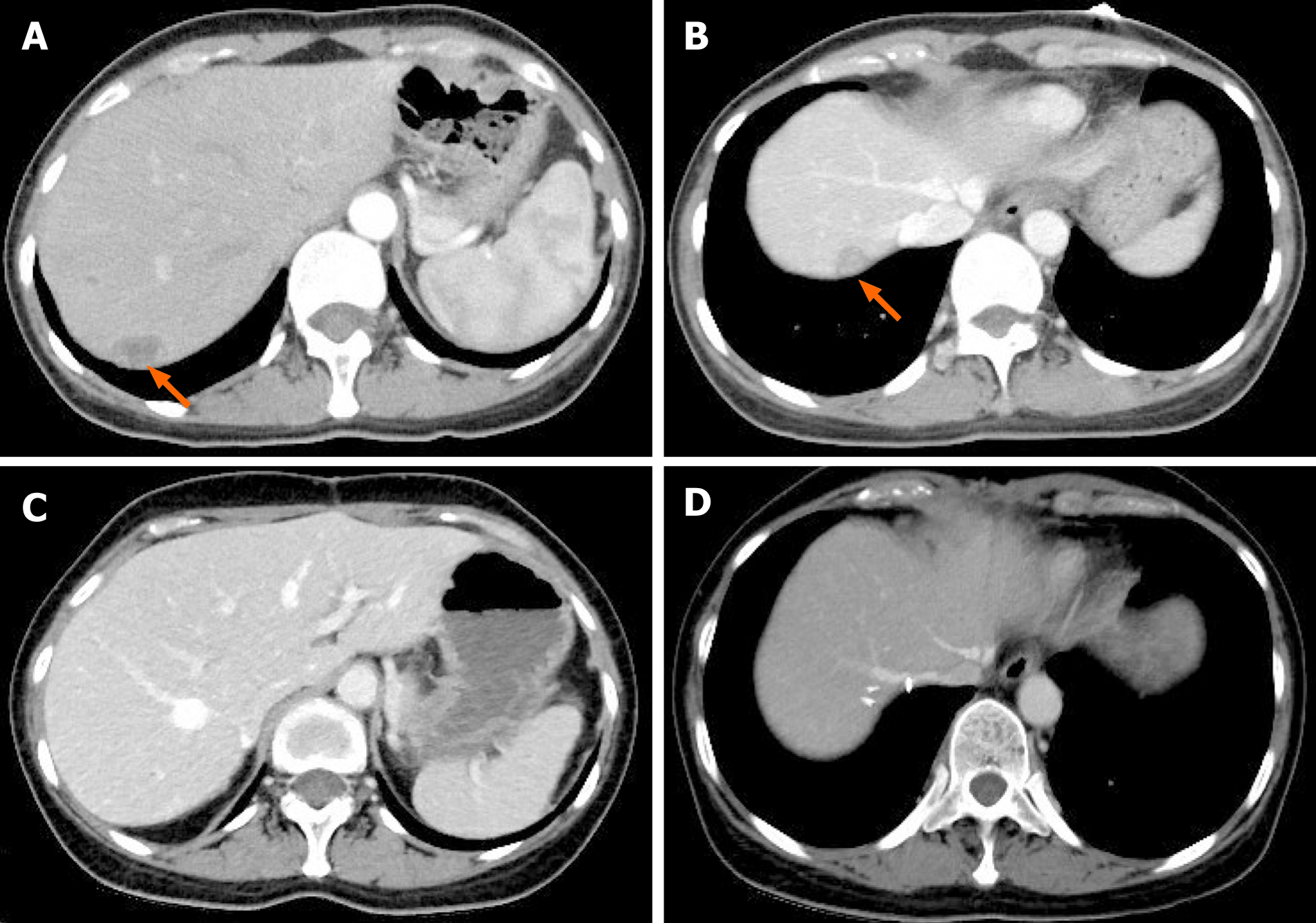
Abdominal computed tomography detected low-density nodules under the liver capsule (Figure 4A and B) 4 mo after initial surgery. Then the second resection of tumors in the liver plus partial hepatectomy (Figure 4C and D) was performed and the postoperative pathological examination indicated that the hepatic tumors were metastatic MNAC.
Five courses of a new combination chemotherapy with carboplatin (300 mg/m2) and gemcitabine (1000 mg/m2) were administered to the patient.
There was no evidence of recurrence within a 22 mo follow-up period after the second surgery.
MNAC is an extremely rare and highly malignant tumor in the female reproductive system. It is believed to be originated from remnant of the regressed mesonephric duct (also called Wolffian duct)[1,4]. Due to the lack of information on the treatment of this rare disease, there are currently no established guidelines about standard therapy of FT-MNAC. However, a radical surgery may be the initial choice for localized disease. Comprehensive staging surgery including hysterectomy, bilateral salpingo-oophorectomy, omentectomy, and para-aortic plus pelvic lymphadenectomy was performed in most of the reported MNAC patients. In this case, the woman was a perimenopausal patient who had already given birth, therefore she received complete staging surgery. Initial radical surgery is considered to be the standard treatment, but there is little evidence about the efficacy of the treatment with chemotherapy or radiotherapy after surgery. Because of its high malignancy, postoperative chemotherapy may be an important and necessary adjuvant treatment method for FT-MNAC to prevent or delay tumor recurrence like any other MNAC or fallopian tube cancer.
MNACs can be very aggressive, even at early stage. A review of the literature including 31 cases of MNAC reported that 82% of the patients had FIGO stage IB disease at initial diagnosis, but one third of the patients with FIGO stage I disease developed recurrence even after radical surgery. Distant metastases and local recurrence were frequent findings in this study, and the median time to recurrence was 2.1 years[5]. In another study, a recurrence rate of 32% was reported among patients with FIGO stage I MNAC[6]. Distant metastases at initial diagnosis were found in less than 5% of MNAC cases, but a malignant clinical course has been reported in about 40% of patients[7,8]. In our case, no distant metastasis was detected at the time of initial diagnosis. Although complete staging surgery combined with systemic chemotherapy was performed, the patient still developed tumor recurrence 4 mo after initial surgery, which indicated that FT-MNAC is very aggressive.
There are no specific recommendations about the treatment of recurrent MNAC especially FT-MNAC, due to limited number of reported cases. However, excision of locally recurrent lesions followed by systemic chemotherapy is still the optimal treatment for patients with recurrent MNAC. By the time being, there has been very little research about which che
We present the first case of primary FT-MNAC without sign of relapse or metastasis after second excision of recurrent lesions until now, which demonstrated a satisfactory response to combination chemotherapy of gemcitabine and carboplatin. FT-MNAC can be very aggressive, even at early stage. Because of its sensitivity to the chemotherapy regimen, it is reasonable that combination chemotherapy of gemcitabine and carboplatin plays an important role in the treatment of recurrent FT-MNAC. However, further research is needed to determine the effectiveness of this chemotherapy regimen and provide better therapeutic regimen.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tanabe S S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Howitt BE, Nucci MR. Mesonephric proliferations of the female genital tract. Pathology. 2018;50:141-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 2. | McCluggage WG, Vosmikova H, Laco J. Ovarian Combined Low-grade Serous and Mesonephric-like Adenocarcinoma: Further Evidence for A Mullerian Origin of Mesonephric-like Adenocarcinoma. Int J Gynecol Pathol. 2020;39:84-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 3. | McFarland M, Quick CM, McCluggage WG. Hormone receptor-negative, thyroid transcription factor 1-positive uterine and ovarian adenocarcinomas: report of a series of mesonephric-like adenocarcinomas. Histopathology. 2016;68:1013-1020. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 147] [Article Influence: 14.7] [Reference Citation Analysis (0)] |
| 4. | Pors J, Cheng A, Leo JM, Kinloch MA, Gilks B, Hoang L. A Comparison of GATA3, TTF1, CD10, and Calretinin in Identifying Mesonephric and Mesonephric-like Carcinomas of the Gynecologic Tract. Am J Surg Pathol. 2018;42:1596-1606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 118] [Article Influence: 16.9] [Reference Citation Analysis (0)] |
| 5. | Yap OW, Hendrickson MR, Teng NN, Kapp DS. Mesonephric adenocarcinoma of the cervix: a case report and review of the literature. Gynecol Oncol. 2006;103:1155-1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 6. | Dierickx A, Göker M, Braems G, Tummers P, Van den Broecke R. Mesonephric adenocarcinoma of the cervix: Case report and literature review. Gynecol Oncol Rep. 2016;17:7-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Montalvo N, Redrobán L, Galarza D. Mesonephric adenocarcinoma of the cervix: a case report with a three-year follow-up, lung metastases, and next-generation sequencing analysis. Diagn Pathol. 2019;14:71. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 8. | Na K, Kim HS. Clinicopathologic and Molecular Characteristics of Mesonephric Adenocarcinoma Arising From the Uterine Body. Am J Surg Pathol. 2019;43:12-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 100] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 9. | Montagut C, Mármol M, Rey V, Ordi J, Pahissa J, Rovirosa A, Gascón P, Mellado B. Activity of chemotherapy with carboplatin plus paclitaxel in a recurrent mesonephric adenocarcinoma of the uterine corpus. Gynecol Oncol. 2003;90:458-461. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |