Published online Feb 26, 2020. doi: 10.12998/wjcc.v8.i4.848
Peer-review started: December 12, 2019
First decision: December 12, 2019
Revised: December 31, 2019
Accepted: January 8, 2020
Article in press: January 8, 2020
Published online: February 26, 2020
Processing time: 75 Days and 23.5 Hours
Coronary intervention for bifurcation lesions is still challenging for interventional cardiologists. Left main (LM) bifurcation lesions have a higher risk due to the vast blood supply in this area and treatment choice is difficult. Ostial compromise of the side branch decreases patient prognosis, and its management is still an issue despite the different strategies and devices available.
A 42-year-old male patient was admitted to hospital due to chest pain and syncope. Coronary angiography showed acute LM occlusion. Following thrombus aspiration, a LM bifurcation lesion remained. Coronary angiography was repeated one week later, and at the same time, 3D optical coherence tomography (OCT) was carried out to better show the geometry of the bifurcation, which confirmed that the stenosis in the ostial left circumflex artery was caused by a long carina. After assessment of the plaque characteristics and the minimum lumen area, the cross-over strategy, kissing balloon inflation and proximal optimization technique were chosen to treat the bifurcation lesion. A “moving” carina was found twice during the intervention. Good stent apposition and expansion were confirmed by OCT after proximal optimization technique. The three-month follow-up showed good recovery and normal cardiac function.
3D-OCT can facilitate decision-making for coronary interventions in patients with critical bifurcation lesions.
Core tip: Coronary intervention for bifurcation lesions is still challenging for interventional cardiologists. Left main bifurcation lesions have a higher risk due to the vast blood supply in this area and treatment choice is difficult. Here we report the diagnosis and management of a 42-year-old male patient who had an acute left main myocardial infarction and carina shift during the follow-up coronary intervention. 3D optical coherence tomography facilitated display of the bifurcation geometry. In addition, a “moving” carina due to carina shift and tissue protrusion was also verified by 3D optical coherence tomography.
- Citation: Du BB, Tong YL, Wang XT, Liu GH, Liu K, Yang P, He YQ. Rescue treatment and follow-up intervention of a left main acute myocardial infarction with typical carina shift under 3D optical coherence tomography: A case report. World J Clin Cases 2020; 8(4): 848-853
- URL: https://www.wjgnet.com/2307-8960/full/v8/i4/848.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i4.848
Coronary intervention for bifurcation lesions is still challenging due to the different therapeutic options and possible unsatisfactory outcomes[1]. Carina shift is a common clinical condition that interventional cardiologists may encounter during intervention for coronary bifurcation lesions[2]. Distinguishing between a carina shift and plaque shift can sometimes be difficult, which may lead to different strategies and treatments[2,3].
Optical coherence tomography (OCT) has been widely used to determine coronary plaque properties and thrombus component analysis[4]. In addition, during intervention for bifurcation lesions, OCT can provide accurate assessment pre-intervention, facilitate decision-making during intervention, and assure apposition and good expansion post-intervention[5]. 3D-OCT can visualize more precisely the geometric configuration through computer reconstruction processing of the two-dimensional images.
Here, we report the case of a patient with side branch ostial compromise due to a typical carina shift during a left main (LM) bifurcation lesion intervention that was verified by 3D-OCT and the strategy chosen to treat this bifurcation lesion.
A 42-year-old man was admitted to China-Japan Union Hospital of Jilin University (Changchun, Jilin Province, China) on an emergency basis due to persistent chest pain and transient syncope.
The patient’s chest pain started 24 min previously while he was working, and shortly after that he developed syncope and fell down. The patient then regained consciousness after falling down. His colleague called the chest pain center and the patient was transferred to the cardiac catheterization laboratory upon arrival at the emergency room by ambulance.
His past medical history consisted mainly of a 20-pack-per-year smoking history. The patient had no history of hypertension or diabetes.
His father had an acute myocardial infarction in his 50s.
Physical examination showed tachycardia (heart rate: 112 bpm) and hypotension (blood pressure: 80/50 mmHg).
Laboratory assessments showed significantly elevated cardiac biomarkers (troponin I 11.0 ng/mL, myoglobin 1200 mg/L, and creatine kinase-MB 234.0 U/L).
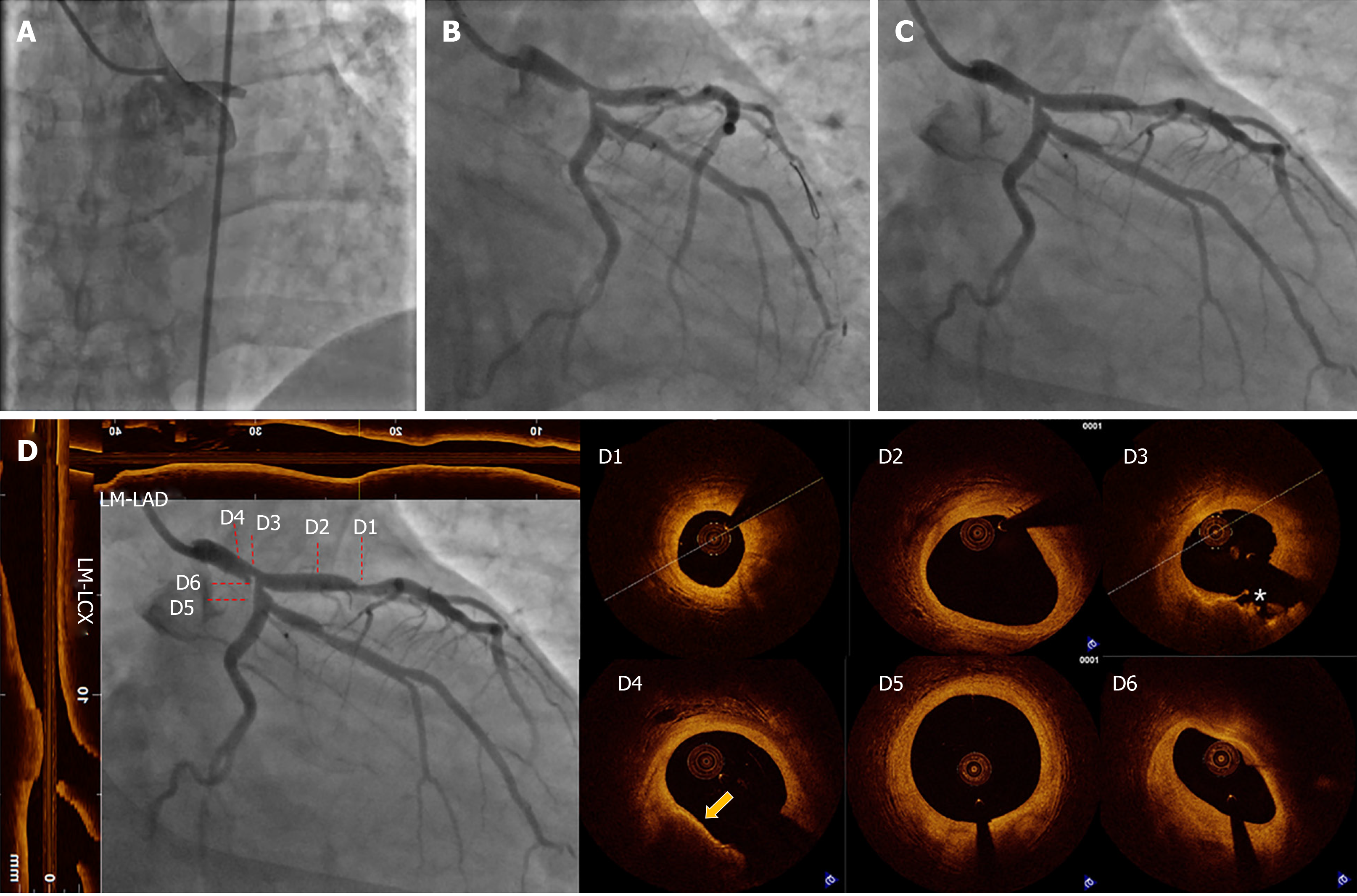
Electrocardiography (ECG) in the ambulance showed anterior lead and lateral lead ST segment elevation. Emergency coronary angiography (CAG) was performed with a femoral approach, which showed occlusion of the LM artery (Figure 1A).
According to the patient’s symptoms, ECG findings, cardiac biomarkers, CAG findings, esophagogastroduodenoscopy findings, and the entire disease course, he was diagnosed with acute anterior wall ST-segment elevation myocardial infarction (LM acute total occlusion) and cardiogenic shock (Killip class IV).
A 6-French JL3.5 guiding catheter was engaged in the LM ostium. When the guidewire (Runthrough NS, Terumo) passed the occlusion, the cardiac monitor showed ventricular fibrillation. With the help of persistent cardio-pulmonary resuscitation, electrical defibrillation and intra-aortic balloon pump (IABP) support, the LM artery was successfully recanalized. Following thrombus aspiration (EXPORT AP, Medtronic, UA, United States), TIMI flow returned to grade 3. A LM bifurcation lesion was identified (Figure 1B). There was severe stenosis in the distal LM and the ostium of the left circumflex artery (LCX). His chest pain was relieved and the elevated ECG lead signals returned to normal. As the blood flow in the left anterior descending artery (LAD) and LCX returned, the procedure was stopped due to treatment decision-making, which consisted of coronary artery bypass grafting and stent implantation. The patient’s family strongly opposed stent implantation, even though refusal of the intervention would result in great risk. The patient was administered intensified antithrombotic therapy (aspirin 100 mg pd, ticagrelor 90 mg bid, and GPI for 24 h) and continuous IABP support in the intensive care unit post-procedure.
The patient refused to undergo further intervention until one week later, during which time his symptoms and cardiac enzyme levels were closely monitored to prevent the onset of serious cardiac events. One week later, the patient had neither recurrent angina nor difficulty breathing. Creatine kinase-MB (3.40 ng/mL) and troponin I (0.89 ng/mL) levels decreased compared with admission levels. Echocardiography indicated normal left ventricular function (ejection fraction 60%). As the patient was relatively stable without angina and heart failure, IABP support was removed. CAG was carried out and showed no significant improvement compared with the previous recording (Figure 1C).
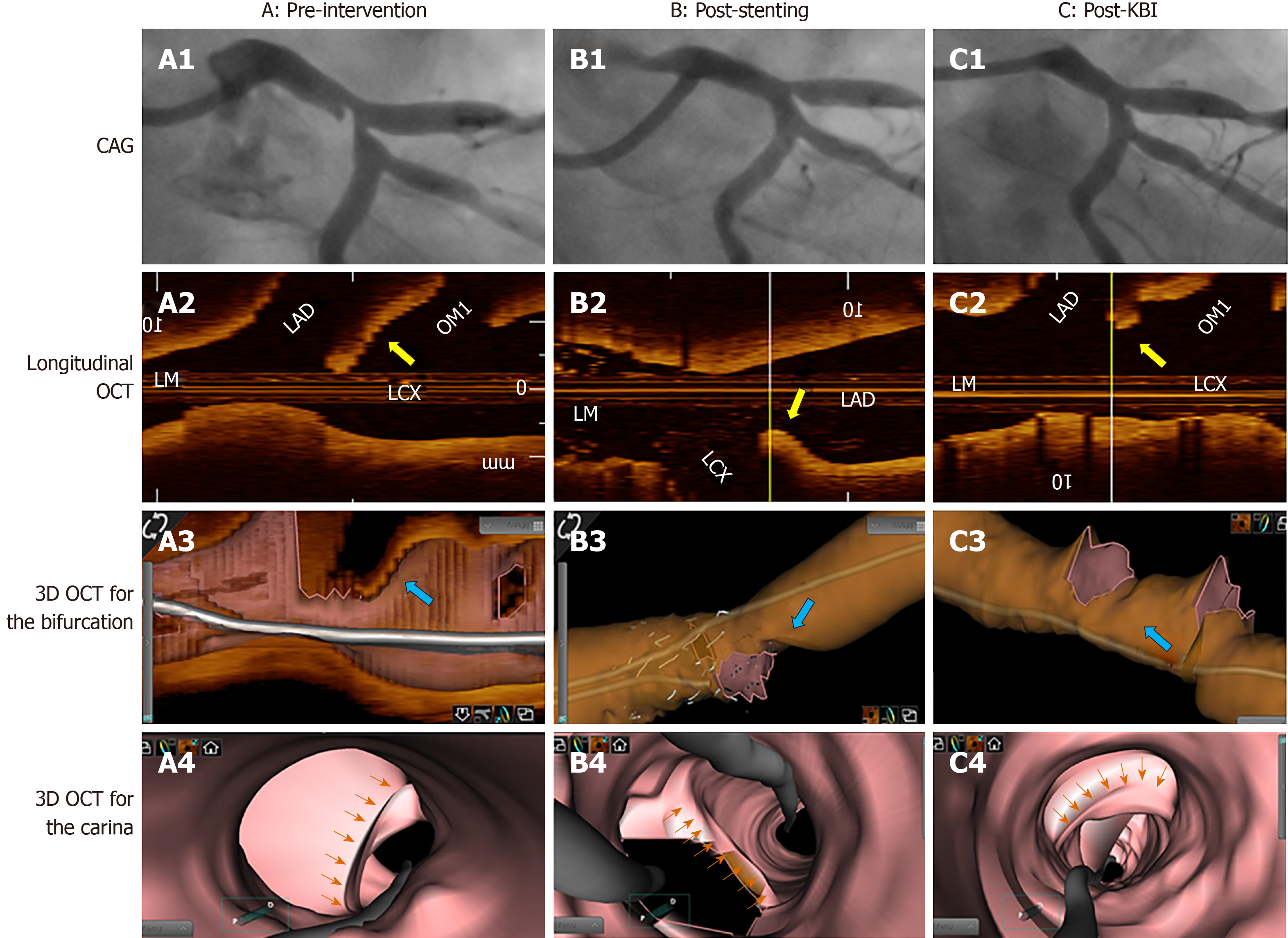
After discussion between the heart team and the patient, percutaneous transluminal coronary revascularization was recommended and then performed to treat the LM bifurcation lesion. A radial approach and a 6-French extra back up 3.5 guiding catheter were selected for controlled angiography. The Runthrough NS guidewire was inserted through the stenosis in the LM and the LAD to the distal LAD. Nitroglycerin (400 μg) was administered intracoronary to exclude coronary spasm. OCT was re-evaluated from the LAD to LM. There was a vulnerable lesion in the LM body and plaque rupture in the distal LM. The stenosis in the proximal LAD was moderate (Figure 1D). OCT was performed from the LCX to the LM and showed a sharp shape change in the ostium of the LCX, which indicated that the stenosis was caused by the carina (Figure 1D). 3D reconstruction confirmed the presence of the long carina at the ostium of the LCX (Figure 2).
After discussion, a crossover strategy from the proximal LCX to the LM with a jailed wire technique protecting the side branch (LAD) was chosen to treat this lesion. The reference diameters of the proximal LCX, proximal LAD, and LM were measured accordingly (Figure 1D). A 3.5/12 mm Promus Element stent (Boston Scientific, Natick, MA, United States) was implanted (14 atm) from the proximal segment of the LCX to the LM. Post-dilation was performed with a 4.0/8 mm balloon (26 atm) at the LM stent with OCT visualization. Good stent apposition and expansion (stent diameter of the LM body was 4.32 mm) was confirmed by OCT after POT in the LM. Thereafter, the carina shifted from the LCX to the LAD (Figure 2). This geometrical change was confirmed by OCT and 3D reconstruction. Rewiring the guidewire (Runthrough NS) was performed easily through the distal stent cell struts to the distal LAD. The kissing balloon inflation technique was performed with two 3.5 NC balloons (Boston Scientific, Natick, MA, United States) to adjust the carina. The final cine images of the coronaries were evaluated and showed partial relief of the stenosis of the ostial LAD. OCT was repeated, and showed the presence of tissue (broken carina) protrusion into the LCX stent lumen (Figure 2).
The patient was discharged from hospital three days after the procedure. Close follow-up of the patient was recommended. The patient’s good clinical course was confirmed by telephone one month and three months after the intervention.
We describe the rescue treatment of a patient with LM acute myocardial infarction, the follow-up intervention process with the guidance of intracoronary imaging and the convenience of 3D-OCT during the intervention for the critical bifurcation lesion.
Emerging data have compared the efficacy and safety of immediate stenting and deferred stenting in the acute myocardial infarction setting. Although large randomized trials and meta-analyses have demonstrated no definite beneficial effect of deferred stenting[6-8], it still has many applications in high risk thrombus acute myocardial infarction patients after thrombus aspiration. However, few studies have compared deferred stenting and immediate stenting when treating LM coronary diseases due to the high risk of mortality, an exclusion criterion[9]. In our patient, the concern of deferring stenting under the premise of good TIMI flow was mainly for two reasons: the patient and his family strongly opposed further intervention and the high risk of treating the LM bifurcation complex lesions in a hemodynamic unstable patient without the family’s consent.
No consensus has been reached regarding the choice of simple or complex strategies and the different techniques one should undertake when a two-stent strategy is needed to treat coronary bifurcation lesions. For LM artery bifurcation lesions, single crossover stenting is better than complex stenting from the point of view of long-term clinical events[10]. In the present case, OCT confirmed the absence of lesion in the ostium and proximal LAD; therefore, we chose a one-stent strategy and crossover from the LCX to the LM. Although the ostium area in the LAD was reduced as a result of carina deviation to the LAD, after rewiring and kissing balloon inflation, a good bifurcation was finally achieved. In addition, as fractional flow reserve has been proved to be a good indicator of side branch long-term prognosis[11], fractional flow reserve guidance may have been better for the intervention in this case.
OCT has been increasingly used to treat complex coronary lesions, such as bifurcation interventions[5,12]. 3D-OCT is a more powerful tool, which can allow a better understanding of space changes of the carina during the procedure and determine the necessary strategy to be undertaken[5,13]. In this case, 3D-OCT clearly showed the angular deviation of the carina, which resulted in the corresponding stenosis seen on CAG. Additionally, 3D-OCT helped to verify optimal rewiring after stenting.
Carina shift is a common mechanism for side branch ostial compromise during coronary bifurcation intervention. 3D-OCT imaging can provide better visualization for bifurcation lesion intervention and better real-time results and long-term outcome.
| 1. | Sawaya FJ, Lefèvre T, Chevalier B, Garot P, Hovasse T, Morice MC, Rab T, Louvard Y. Contemporary Approach to Coronary Bifurcation Lesion Treatment. JACC Cardiovasc Interv. 2016;9:1861-1878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 134] [Article Influence: 14.9] [Reference Citation Analysis (1)] |
| 2. | Gwon HC, Song YB, Pan M. The story of plaque shift and carina shift. EuroIntervention. 2015;11 Suppl V:V75-V77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 3. | Xu J, Hahn JY, Song YB, Choi SH, Choi JH, Lu C, Lee SH, Hong KP, Park JE, Gwon HC. Carina shift versus plaque shift for aggravation of side branch ostial stenosis in bifurcation lesions: volumetric intravascular ultrasound analysis of both branches. Circ Cardiovasc Interv. 2012;5:657-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 4. | Jia H, Dai J, Hou J, Xing L, Ma L, Liu H, Xu M, Yao Y, Hu S, Yamamoto E, Lee H, Zhang S, Yu B, Jang IK. Effective anti-thrombotic therapy without stenting: intravascular optical coherence tomography-based management in plaque erosion (the EROSION study). Eur Heart J. 2017;38:792-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 124] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 5. | Longobardo L, Mattesini A, Valente S, Di Mario C. OCT-guided Percutaneous Coronary Intervention in Bifurcation Lesions. Interv Cardiol. 2019;14:5-9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 24] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 6. | Kelbæk H, Høfsten DE, Køber L, Helqvist S, Kløvgaard L, Holmvang L, Jørgensen E, Pedersen F, Saunamäki K, De Backer O, Bang LE, Kofoed KF, Lønborg J, Ahtarovski K, Vejlstrup N, Bøtker HE, Terkelsen CJ, Christiansen EH, Ravkilde J, Tilsted HH, Villadsen AB, Aarøe J, Jensen SE, Raungaard B, Jensen LO, Clemmensen P, Grande P, Madsen JK, Torp-Pedersen C, Engstrøm T. Deferred versus conventional stent implantation in patients with ST-segment elevation myocardial infarction (DANAMI 3-DEFER): an open-label, randomised controlled trial. Lancet. 2016;387:2199-2206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 125] [Cited by in RCA: 241] [Article Influence: 24.1] [Reference Citation Analysis (0)] |
| 7. | Qiao J, Pan L, Zhang B, Wang J, Zhao Y, Yang R, Du H, Jiang J, Jin C, Xiong E. Deferred Versus Immediate Stenting in Patients With ST-Segment Elevation Myocardial Infarction: A Systematic Review and Meta-Analysis. J Am Heart Assoc. 2017;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Belle L, Motreff P, Mangin L, Rangé G, Marcaggi X, Marie A, Ferrier N, Dubreuil O, Zemour G, Souteyrand G, Caussin C, Amabile N, Isaaz K, Dauphin R, Koning R, Robin C, Faurie B, Bonello L, Champin S, Delhaye C, Cuilleret F, Mewton N, Genty C, Viallon M, Bosson JL, Croisille P; MIMI Investigators*. Comparison of Immediate with Delayed Stenting Using the Minimalist Immediate Mechanical Intervention Approach in Acute ST-Segment-Elevation Myocardial Infarction: The MIMI Study. Circ Cardiovasc Interv. 2016;9:e003388. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 68] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 9. | Ramadan R, Boden WE, Kinlay S. Management of Left Main Coronary Artery Disease. J Am Heart Assoc. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 69] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 10. | Cho S, Kang TS, Kim JS, Hong SJ, Shin DH, Ahn CM, Kim BK, Ko YG, Choi D, Song YB, Hahn JY, Choi SH, Gwon HC, Hong MK, Jang Y. Long-Term Clinical Outcomes and Optimal Stent Strategy in Left Main Coronary Bifurcation Stenting. JACC Cardiovasc Interv. 2018;11:1247-1258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 11. | Lee CH, Choi SW, Hwang J, Kim IC, Cho YK, Park HS, Yoon HJ, Kim H, Han S, Kim JY, Lee JM, Doh JH, Shin ES, Koo BK, Hur SH, Nam CW. 5-Year Outcomes According to FFR of Left Circumflex Coronary Artery After Left Main Crossover Stenting. JACC Cardiovasc Interv. 2019;12:847-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 12. | Nagoshi R, Okamura T, Murasato Y, Fujimura T, Yamawaki M, Ono S, Serikawa T, Hikichi Y, Nakao F, Sakamoto T, Shinke T, Kijima Y, Kozuki A, Shibata H, Shite J. Data on two- and three-dimensional optical coherence tomography guidance for the treatment for the bifurcation lesion. Data Brief. 2018;16:865-868. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Murasato Y, Mori T, Okamura T, Nagoshi R, Fujimura T, Yamawaki M, Ono S, Serikawa T, Nakao F, Shite J; 3D-OCT Bifurcation Registry Investigators. Efficacy of the proximal optimization technique on crossover stenting in coronary bifurcation lesions in the 3D-OCT bifurcation registry. Int J Cardiovasc Imaging. 2019;35:981-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: European Society of Cardiology, Acute Cardiovascular Care Association, No. 087109300.
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Peteiro J, Ueda H S-Editor: Zhang L L-Editor: Webster JR E-Editor: Ma YJ