Published online Feb 6, 2020. doi: 10.12998/wjcc.v8.i3.630
Peer-review started: October 13, 2019
First decision: November 13, 2019
Revised: November 19, 2019
Accepted: December 6, 2019
Article in press: December 6, 2019
Published online: February 6, 2020
Processing time: 115 Days and 19.4 Hours
The 2018 American Heart Association/American Stroke Association guidelines for early management of acute ischemic stroke recommend the use of retrievable stents for mechanical thrombectomy in patients with acute internal carotid artery or middle cerebral artery M1 occlusion that can be treated within 6 h from onset. For cases of carotid artery with ipsilateral middle cerebral artery tandem embolization, the operation is more complicated and challenging. We here report a case of a tandem embolism, and the anatomy of the aortic arch was complex. Direct carotid artery incision and thrombectomy can not only prevent the escape of the carotid embolus but also save time during establishment of the thrombectomy access.
The patient was a 70-year-old man. He was admitted to hospital due to sudden inability to speak and inability to move his right limb for 3 h. Imaging confirmed a diagnosis of a tandem embolism in the left carotid artery with left M1 occlusion. Carotid artery incision thrombectomy combined with stent thrombectomy was performed. The operation was successful, and 24 h later the patient was conscious and mentally competent but had motor aphasia. His bilateral limb muscle strength level was 5, and his neurologic severity scores score was 2.
Carotid artery incision thrombectomy combined with stenting for carotid artery plus cerebral artery tandem embolization is clinically feasible. For patients with a complicated aortic arch and an extremely tortuous carotid artery, carotid artery incision can be chosen to establish the interventional path.
Core tip: We report a case of acute carotid artery and ipsilateral middle cerebral artery occlusion. The anatomy of the aortic arch was complex. We chose carotid artery incision thrombectomy combined with stent thrombectomy for this patient because of the following reasons. First, the anatomy of the aortic arch was complex, and simple intravascular treatment would take a longer time to establish the interventional path. Second, the embolus was located in the bifurcation of the carotid artery and the ipsilateral middle cerebral artery. There was no obvious embolus in the remaining segments of the internal carotid artery, so there was positive blood flow in the internal carotid artery. In such patients, carotid stent implantation for carotid artery embolization might result in distal escape of the thrombus.
- Citation: Zhang M, Hao JH, Lin K, Cui QK, Zhang LY. Combined surgical and interventional treatment of tandem carotid artery and middle cerebral artery embolus: A case report. World J Clin Cases 2020; 8(3): 630-637
- URL: https://www.wjgnet.com/2307-8960/full/v8/i3/630.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i3.630
The 2018 American Heart Association/American Stroke Association guidelines for early management of acute ischemic stroke recommend the use of retrievable stents for mechanical thrombectomy in patients with acute internal carotid artery or middle cerebral artery M1 occlusion that can be treated within 6 h from onset[1]. Few cases of carotid artery combined with ipsilateral middle cerebral artery tandem embolism, have been reported. In addition, the operation is more complex and challenging, and the prognosis of such patients is poor[2]. We treated a case of carotid artery combined with middle cerebral artery tandem embolization with carotid artery incision thrombectomy combined with stenting. The result was satisfactory.
A 70-year-old man complained of sudden inability to speak and inability to move his right limb for 3 h.
A history of atrial fibrillation for more than 1 year.
No history of hypertension, diabetes, coronary heart disease or other chronic diseases. There was no similar event or known genetic history in his family.
The patient presented with drowsiness and complete mixed aphasia. The right nasolabial groove had become shallow, and his mouth was askew to the left. His left limb was movable, and the right limb was unmovable. The muscle tension of the extremities was normal, and pathological signs on the right side were positive. His baseline neurologic severity scores (NHISS) score was 23.
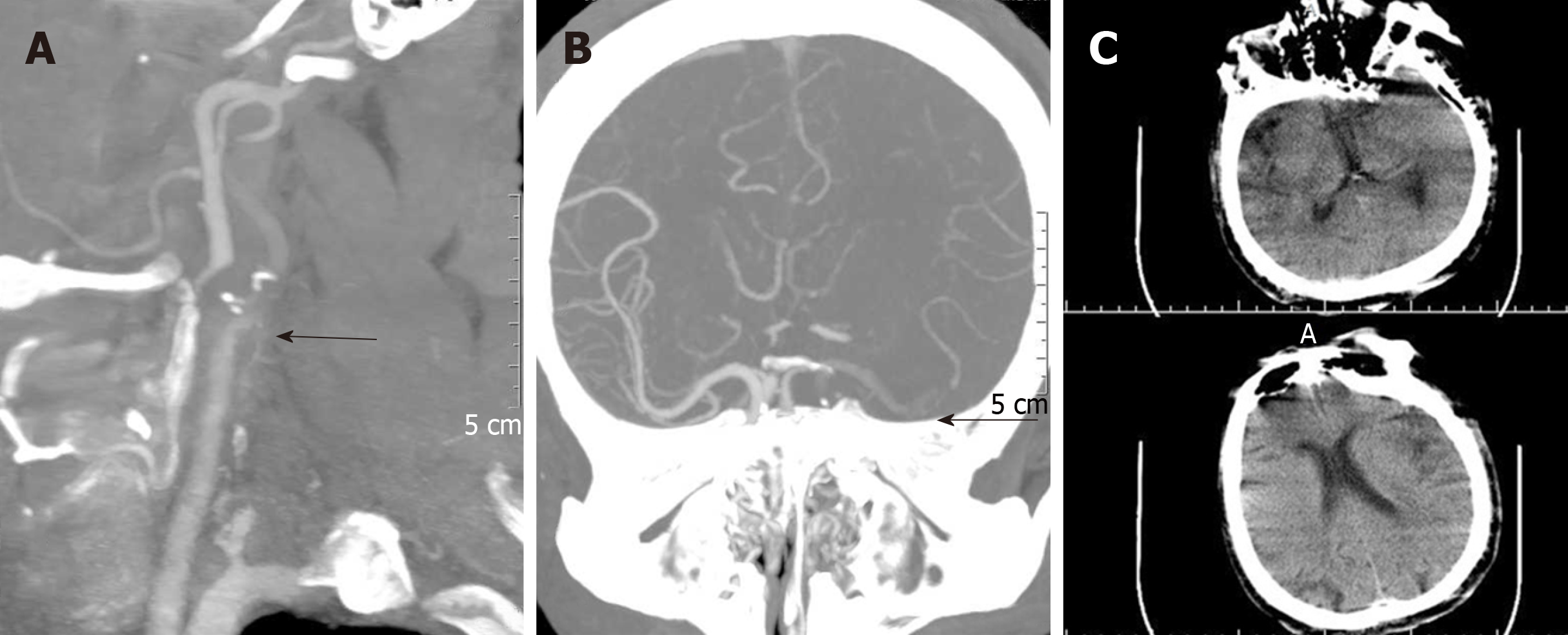
Electrocardiogram examination showed atrial fibrillation. Head and neck computed tomography angiography (CTA) showed embolisms in the left carotid bifurcation and left middle cerebral artery. Brain computed tomography showed a small infarct in the left insular lobe (Figure 1).
Blood routine examination and coagulation mechanism showed no obvious abnormalities.
Carotid artery combined with ipsilateral middle cerebral artery acute tandem embolism.
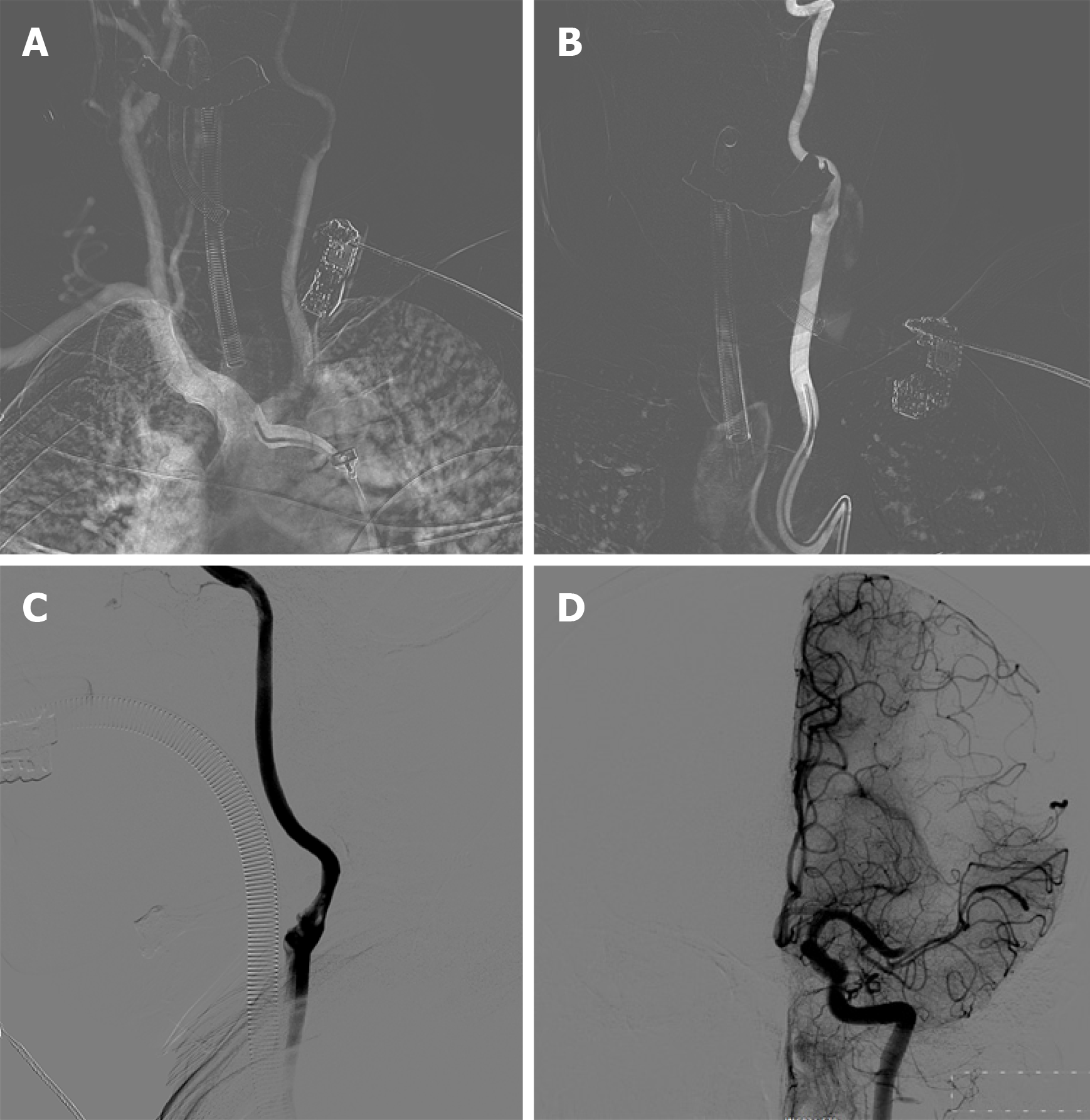
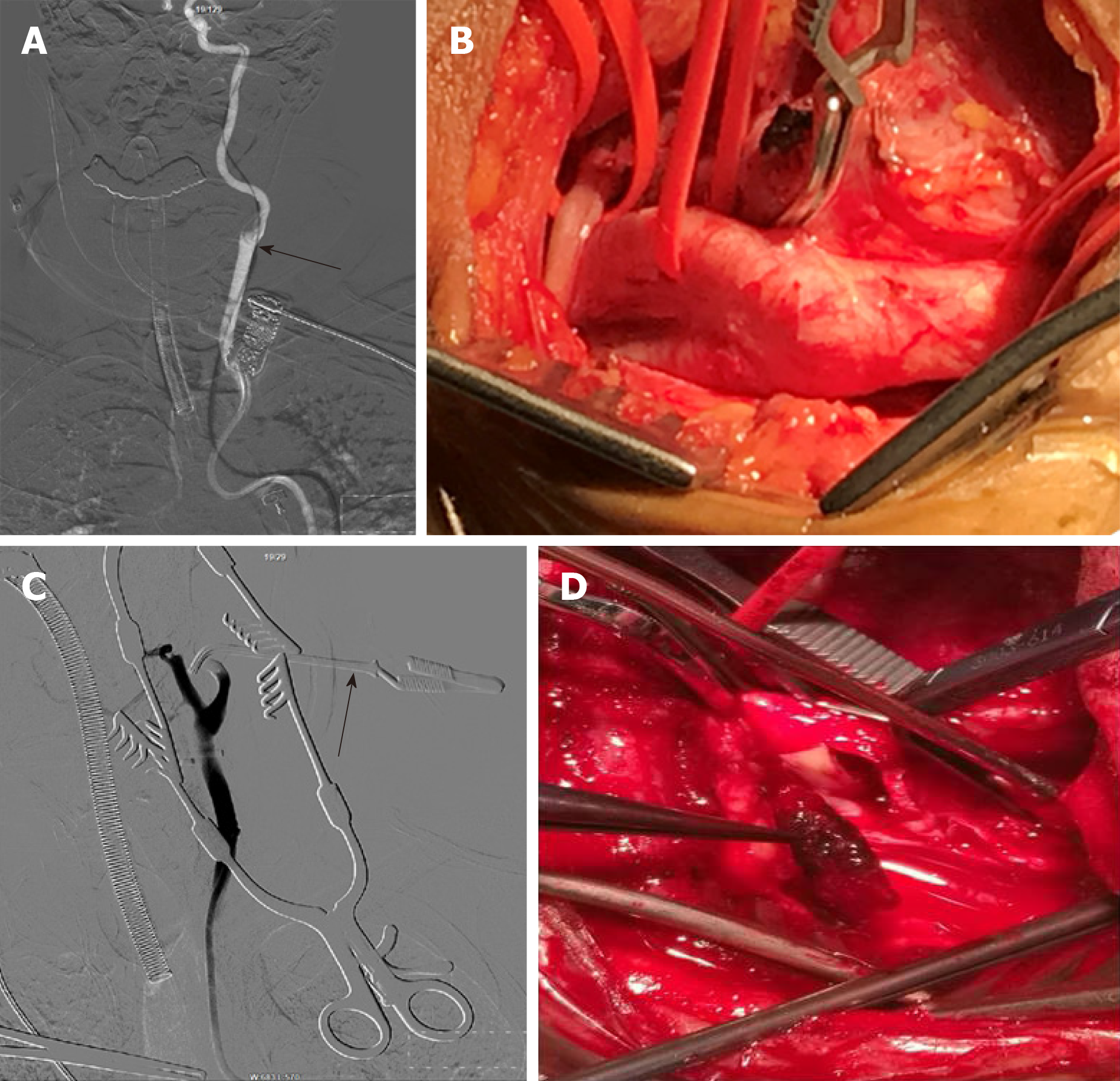
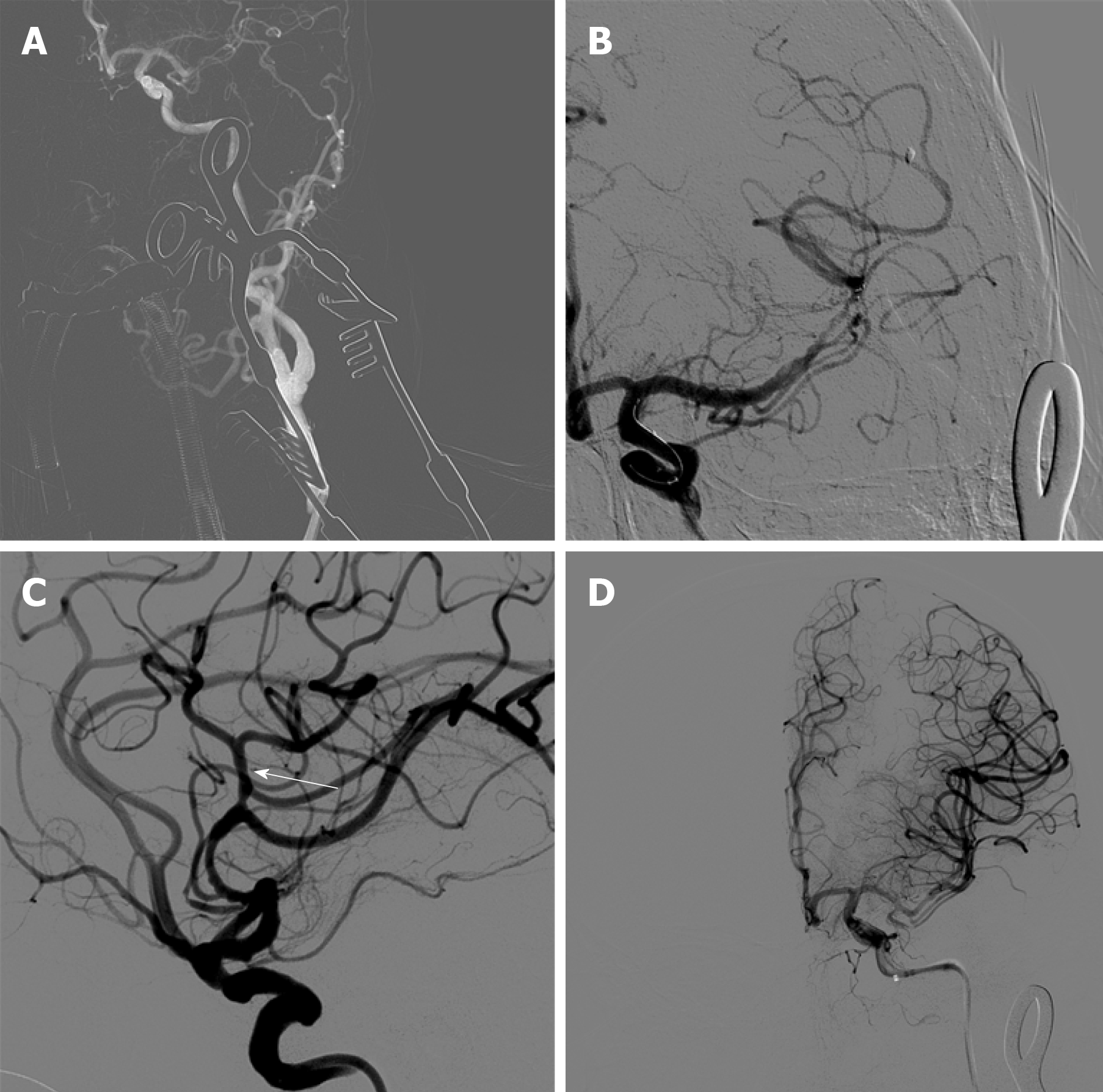
Alteplase was administered at a dose of 0.9 mg/kg 200 min after symptom onset. Revascularization was initiated 210 min after onset. Cerebral angiography showed a type III aortic arch, where the left common carotid artery shared the main trunk with the brachiocephalic trunk. A Simmon 2 angiography catheter was placed for left common carotid artery angiography. The left external carotid artery was not visible, and the left internal carotid artery showed slow blood flow. Thrombosis at the beginning of the internal carotid artery and occlusion of the upper trunk of the left middle cerebral artery was considered. The left anterior cerebral artery provided secondary compensatory blood supply to the left middle cerebral artery (Figure 2). Repeated attempts were made to place the 8F guiding catheter into the left common carotid artery, which took 40 min. The 8F guiding catheter was aspirated at the bifurcation of the left carotid artery, and no reverse bleeding was observed. A percutaneous carotid artery incision was made to remove the thrombus in the neck under direct vision, and it only took 20 min (Figure 3). The left carotid artery was sutured, and angiography showed that the thrombosis in the bifurcation of the carotid artery had disappeared and that the internal and external carotid arteries were unblocked. Using the Solitaire intermediate catheter for mechanical thrombectomy , a 5Fr Navien intermediate catheter was placed across the carotid bifurcation into the petrosal segment. The left middle cerebral artery clot was removed with a Solitaire FR 6–30 mm. After two attempts, the patient was re-examined by angiography, which revealed middle cerebral artery blood flow recanalization, with modified thrombolysis in cerebral infarction score level III (Figure 4).
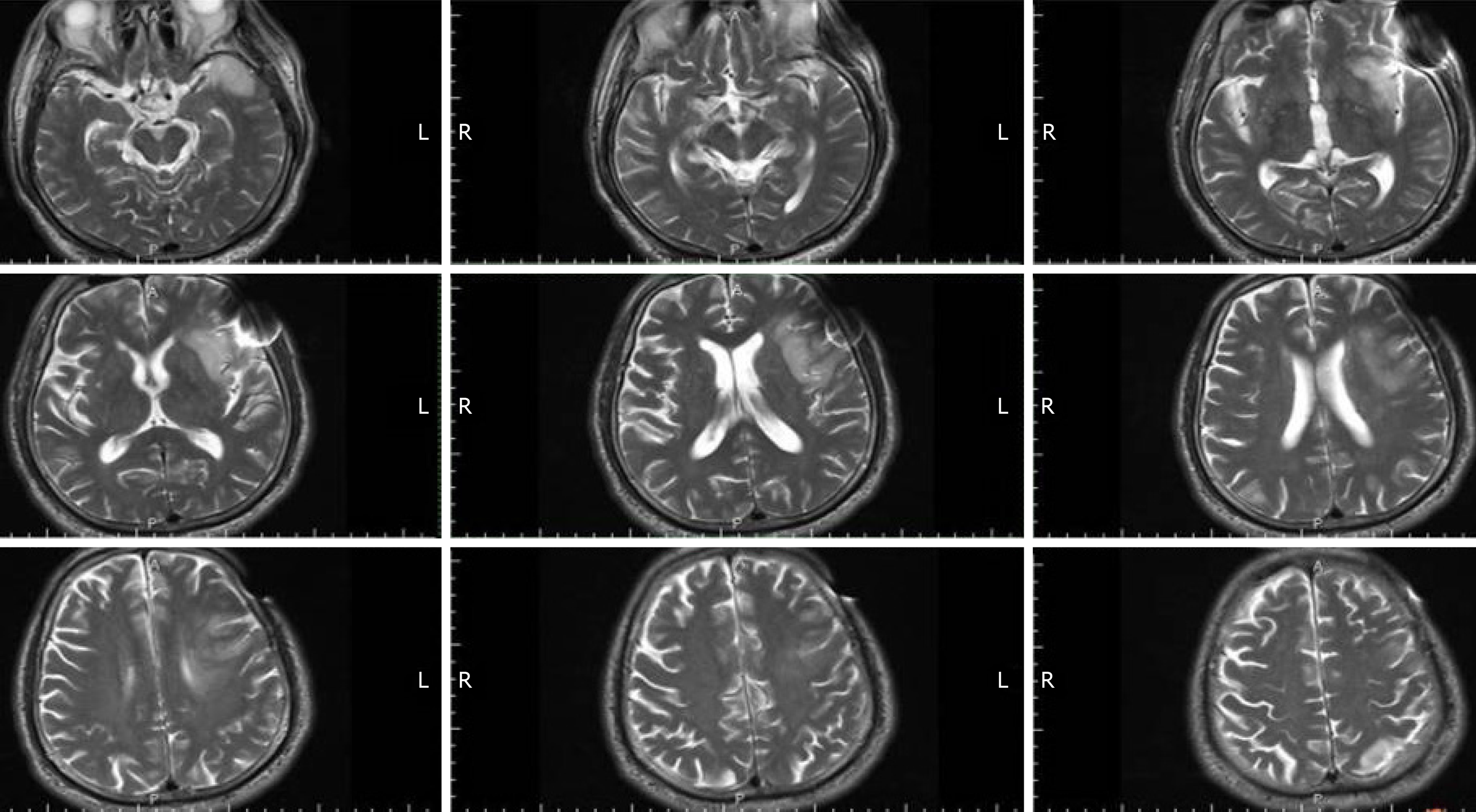
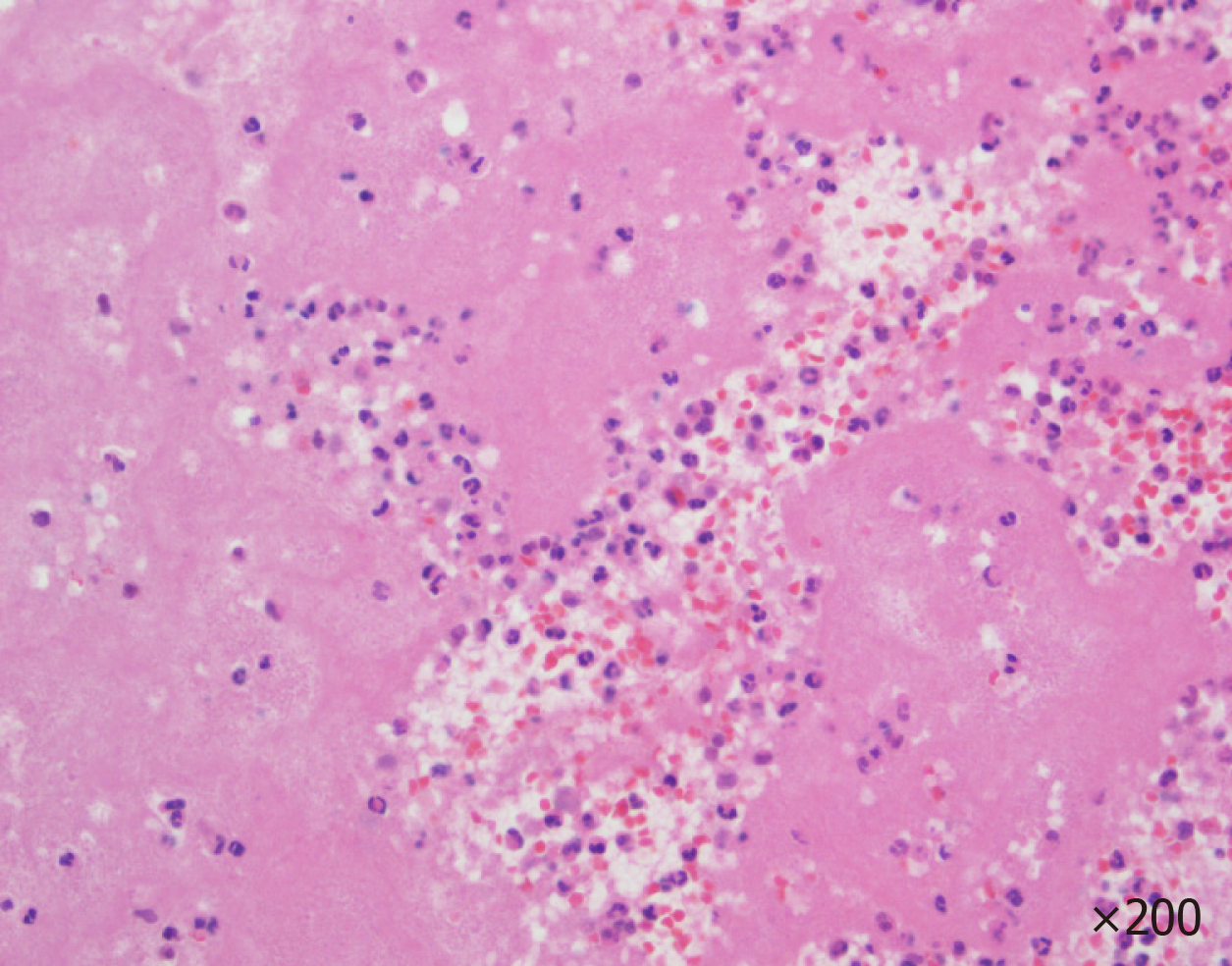
Neurological examination was performed 24 h after the operation. The patient was conscious and mentally competent, accompanied by motor aphasia. His bilateral limb muscle strength level was 5, and his NHISS score was 2. Brain magnetic resonance imaging showed small infarcts in the frontal and temporal lobes (Figure 5). Pathological examination of the thrombus showed a mixed thrombus (Figure 6). His mRS score was 0 at 3 mo of follow-up (Table 1).
| Clinical information | |
| Age (yr) | 70 |
| Chief complaint | Sudden inability to speak; inability to move his right limb for 3 h |
| History of present illness | Atrial fibrillation history for more than 1 yr |
| Physical examination | Drowsiness and completely mixed aphasia; right limb was not movable |
| Electrocardiogram examination | Atrial fibrillation |
| CTA | Embolisms in the left carotid bifurcation and left middle cerebral artery |
| CT | A small infarct in the left insular lobe |
| NIHSS | 23 |
Severe acute ischemic stroke is often caused by acute tandem occlusion of the internal carotid artery and the ipsilateral middle cerebral artery. External carotid artery occlusion is mainly caused by arterial dissection and atherosclerotic plaques[3]. Ipsilateral middle cerebral artery occlusion is usually caused by thrombus or plaque detachment in the lesion site near the internal carotid artery[4-6]. Treatment for patients with such tandem occlusions has been reported at several centers[7-9]. Balloon dilatation or combined stenting was used to treat the occlusion of the external segment of the internal carotid artery, and mechanical thrombectomy was used to solve the occlusion of the ipsilateral middle cerebral artery. It has also been reported that due to the hardness of the plaque in the initial segment of the internal carotid artery, various microcatheter and guidewire techniques were attempted but could not pass through the occlusion site of the external cranial segment of the internal carotid artery. Carotid artery puncture was performed to establish thrombectomy access. Mechanical thrombectomy of the ipsilateral middle cerebral artery occlusion was performed first, and carotid endarterectomy was then performed to treat the internal carotid artery lesions[10]. One study evaluated outcomes and feasibility of carotid artery stenting versus carotid endarterectomy, and performed both procedures in the same patient. Carotid endarterectomy confirms its efficacy in carotid revascularization, but carotid artery stenting constitutes a good alternative when the procedures are selected based on patient-specific risk factors[11].
The case reported here is considered to be due to embolic events and is thus different from tandem occlusion due to atherosclerotic plaques and arterial dissection. It is also different from the occlusion of the internal carotid artery and middle cerebral artery caused by a high load embolism. The embolus in this patient was located in the bifurcation of the carotid artery and the ipsilateral middle cerebral artery, and no obvious embolus was found in the remaining internal carotid artery, so there was positive blood flow in the internal carotid artery. If a carotid artery embolization is treated with carotid stent implantation in such patients, it may result in distal escape of the thrombus. Studies have shown that aortic arch and proximal carotid artery anatomic factors seriously affect the time required for thrombectomy and are independent risk factors leading to a poor prognosis[12,13]. Carotid puncture is an option. It is difficult to stop the bleeding after postoperative removal of the artery sheath tube after carotid artery puncture. Nii et al[14] applied percutaneous carotid artery puncture for intracranial aneurysm embolization in 27 patients, and 4% of the patients developed a neck hematoma after surgery. In this case, the thrombus was located at the bifurcation of the carotid artery, and percutaneous carotid artery puncture was likely to cause embolus shedding and embolization of the distal blood vessel.
During the operation in the presented case, simple endovascular treatment was considered first. Repeated attempts were made to place the 8F guiding catheter into the left carotid artery, which took 40 min. The 8F catheter was used to aspirate the thrombus at the bifurcation. There was no obvious recanalization of blood after the aspiration, and it was believed that the catheter was stuck against the vessel wall or the thrombus blocked the tube. Then, the 8F catheter was withdrawn to the common carotid artery at the time of aspiration, and no reverse blood was found. The thrombus was considered to be large and stiff and obstructed the 8F catheter. If the 8F catheter is withdrawn from the body, it will take too long to replace the catheter and the thrombus may detach into the femoral artery sheath during retraction. So we chose to dissect and expose the carotid bifurcation. First, the internal carotid artery blood flow was blocked and partial recanalization of the external carotid artery was found by low-flow hand push angiography. However, some thrombus had still not been removed, so carotid artery incision thrombectomy was selected. The internal carotid artery was blocked during the process to avoid the distal escape of the embolus. The safety of emergency carotid endarterectomy (CEA) after intravenous thrombolysis has been confirmed by many reports, and the shortest time reported so far for CEA surgery after intravenous thrombolysis is 120 min[10,15,16].
Carotid artery incision thrombectomy combined with stenting for the treatment of carotid artery plus cerebral artery tandem embolization is clinically feasible. For patients with a complicated aortic arch and an extremely tortuous carotid artery who cannot receive simple endovascular treatment, carotid artery incision can be chosen to establish the interventional path. A large sample of cases is still needed for further study and confirmation.
| 1. | Warner JJ, Harrington RA, Sacco RL, Elkind MSV. Guidelines for the Early Management of Patients with Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. Stroke. 2019;50:3331-3332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 87] [Article Influence: 12.4] [Reference Citation Analysis (0)] |
| 2. | Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, Alvarez-Sabín J, Molina CA. Tandem internal carotid artery/middle cerebral artery occlusion: an independent predictor of poor outcome after systemic thrombolysis. Stroke. 2006;37:2301-2305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 260] [Cited by in RCA: 315] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 3. | Soize S, Kadziolka K, Estrade L, Serre I, Barbe C, Pierot L. Outcome after mechanical thrombectomy using a stent retriever under conscious sedation: comparison between tandem and single occlusion of the anterior circulation. J Neuroradiol. 2014;41:136-142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 4. | Maurer CJ, Joachimski F, Berlis A. Two in One: Endovascular Treatment of Acute Tandem Occlusions in the Anterior Circulation. Clin Neuroradiol. 2015;25:397-402. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 51] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 5. | Grigoryan M, Haussen DC, Hassan AE, Lima A, Grossberg J, Rebello LC, Tekle W, Frankel M, Nogueira RG. Endovascular Treatment of Acute Ischemic Stroke Due to Tandem Occlusions: Large Multicenter Series and Systematic Review. Cerebrovasc Dis. 2016;41:306-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 68] [Cited by in RCA: 67] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 6. | Lockau H, Liebig T, Henning T, Neuschmelting V, Stetefeld H, Kabbasch C, Dorn F. Mechanical thrombectomy in tandem occlusion: procedural considerations and clinical results. Neuroradiology. 2015;57:589-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 109] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 7. | Fahed R, Redjem H, Blanc R, Labreuche J, Robert T, Ciccio G, Smadja D, Smajda S, Piotin M. Endovascular Management of Acute Ischemic Strokes with Tandem Occlusions. Cerebrovasc Dis. 2016;41:298-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 36] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 8. | Cohen JE, Gomori JM, Rajz G, Itshayek E, Eichel R, Leker RR. Extracranial carotid artery stenting followed by intracranial stent-based thrombectomy for acute tandem occlusive disease. J Neurointerv Surg. 2015;7:412-417. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 76] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 9. | Al-Mufti F, Amuluru K, Manning NW, Khan I, Peeling L, Gandhi CD, Prestigiacomo CJ, Pushchinska G, Fiorella D, Woo HH. Emergent carotid stenting and intra-arterial abciximab in acute ischemic stroke due to tandem occlusion. Br J Neurosurg. 2017;31:573-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Frenkel MB, Renfrow JJ, Singh J, Garg N, Wolfe SQ. Combined interventional and surgical treatment of tandem middle cerebral artery embolus and internal carotid artery occlusion: case report. J Neurosurg. 2018;129:718-722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Ciccone MM, Scicchitano P, Cortese F, Gesualdo M, Zito A, Carbonara R, Dentamaro I, Pulli R, Salerno C, Impedovo G, Marinazzo D, Angiletta D, Guido D, Regina G. Carotid stenting versus endarterectomy in the same patient: A "direct" comparison. Vascular. 2017;25:290-298. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Kaesmacher J, Gralla J, Mosimann PJ, Zibold F, Heldner MR, Piechowiak E, Dobrocky T, Arnold M, Fischer U, Mordasini P. Reasons for Reperfusion Failures in Stent-Retriever-Based Thrombectomy: Registry Analysis and Proposal of a Classification System. AJNR Am J Neuroradiol. 2018;39:1848-1853. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 80] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 13. | Kaymaz ZO, Nikoubashman O, Brockmann MA, Wiesmann M, Brockmann C. Influence of carotid tortuosity on internal carotid artery access time in the treatment of acute ischemic stroke. Interv Neuroradiol. 2017;23:583-588. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 58] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 14. | Nii K, Kazekawa K, Onizuka M, Aikawa H, Tsutsumi M, Tomokiyo M, Iko M, Kodama T, Matsubara S, Go Y, Tanaka A. Direct carotid puncture for the endovascular treatment of anterior circulation aneurysms. AJNR Am J Neuroradiol. 2006;27:1502-1504. [PubMed] |
| 15. | Azzini C, Gentile M, De Vito A, Traina L, Sette E, Fainardi E, Mascoli F, Casetta I. Very Early Carotid Endarterectomy After Intravenous Thrombolysis. Eur J Vasc Endovasc Surg. 2016;51:482-486. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Bazan HA, Zea N, Jennings B, Smith TA, Vidal G, Sternbergh WC. Urgent carotid intervention is safe after thrombolysis for minor to moderate acute ischemic stroke. J Vasc Surg. 2015;62:1529-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 28] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ciccone MM, Grawish M S-Editor: Zhang L L-Editor: MedE-Ma JY E-Editor: Qi LL