Published online Feb 6, 2020. doi: 10.12998/wjcc.v8.i3.546
Peer-review started: November 12, 2019
First decision: December 23, 2019
Revised: January 9, 2020
Accepted: January 15, 2020
Article in press: January 15, 2020
Published online: February 6, 2020
Processing time: 85 Days and 20.6 Hours
Several studies have demonstrated that airborne transmission of Mycobacterium tuberculosis bacteria from patients with active pulmonary tuberculosis (TB) to other passengers or crew members can occur during long flights. As such, non-infectious TB patients are usually allowed to undertake air travel after taking the appropriate anti-TB drugs. However, the global guidelines for air travel for patients with TB are inconsistent and insufficiently detailed with respect to cavitary pulmonary TB (CPTB).
Here, we report a case in which a patient with multiple CPTB was permitted air travel, following negative sputum acid-fast bacilli smear tests after administration of proper anti-TB medication. The patient’s culture results were pending.
This case revealed that more specific guidelines regulating air travel for patients with CPTB are necessary.
Core tip: Patients with cavitary pulmonary tuberculosis (CPTB) could have an active infection for longer periods than non-CPTB patients. Air travel may be inevitable for these patients, but the paucity of consistent guidelines regulating the protocol for permitting air travel for such patients renders decision making difficult. Based on this case, we think that if air travel is unavoidable for patients with CPTB who are still considered potentially infectious, it might be possible to board the flight if proper anti-TB medication is administered, confirmatory acid-fast bacilli smear tests are negative, and a suitable N95 mask is worn under observation.
- Citation: Jo W, Pak C, Jegal Y, Seo KW. Boarding issue in a commercial flight for patients with cavitary pulmonary tuberculosis: A case report. World J Clin Cases 2020; 8(3): 546-551
- URL: https://www.wjgnet.com/2307-8960/full/v8/i3/546.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i3.546
In general, a lot of patients with drug-sensitive tuberculosis (TB) become non-infectious following 2 wk of adequate treatment[1-3]. However, patients with cavitary pulmonary TB (CPTB) could have active infection for longer periods, may require treatment for a longer duration[4-6], and be more contagious than patients with non-CPTB[7]. Although bacterial smears and cultures are usually performed simultaneously, from the same specimen, there is a lag between obtaining acid-fast bacilli (AFB) smear and culture results because bacterial culture requires more time than a smear[4]. The global guidelines for air travel of individuals with infectious or potentially infectious TB are inconsistent[8-11]. Abiding by the World Health Organization (WHO) recommendations, which are contingent on confirming culture conversion, would require too much time to ascertain if individuals with CPTB or even potentially infectious TB can travel in an airplane without endangering the safety of other passengers. Thus, some researchers have argued that this might infringe upon the individual’s rights[12].
A 30-year-old Indian man was referred to the emergency center of the Ulsan University Hospital for evaluation of an abnormal chest X-ray and persistent cough since the past two months, when his ship had made an intermediate stop in South Korea.
The patient had intermittent high-spiking fever and night sweats but denied having chills or weight loss.
The patient had a free previous medical history.
The patient was working as a navigator on an Indian merchant ship. He was suspected of having pulmonary TB after physical examinations and chest radiographs performed in the emergency room and was placed in isolation, under negative pressure in the emergency center. He did not seem to have cachexia on examination. However, lung auscultation revealed coarse breathing sounds arising from both lung fields.
On physical examination, the following measurements were obtained: BP, 142/88 mmHg; body temperature, 38.8 °C; heart rate, 115 beats/min; respiratory rate, 20 breaths/min; room air oxygen saturation, 95%; body weight, 68.6 kg; height, 180 cm; and body mass index, 21.2.
Laboratory examinations yielded the following results: white blood cell 9280/µL; hemoglobin, 12.2 g/dL; glucose 108 mg/dL; creatinine 0.81 mg/dL; albumin 3.5 g/dL; and C-reactive protein 7.92 mg/dL (normal range < 0.5 mg/dL). Human immunodeficiency virus antibodies were absent. The results of other biochemical tests were unremarkable.
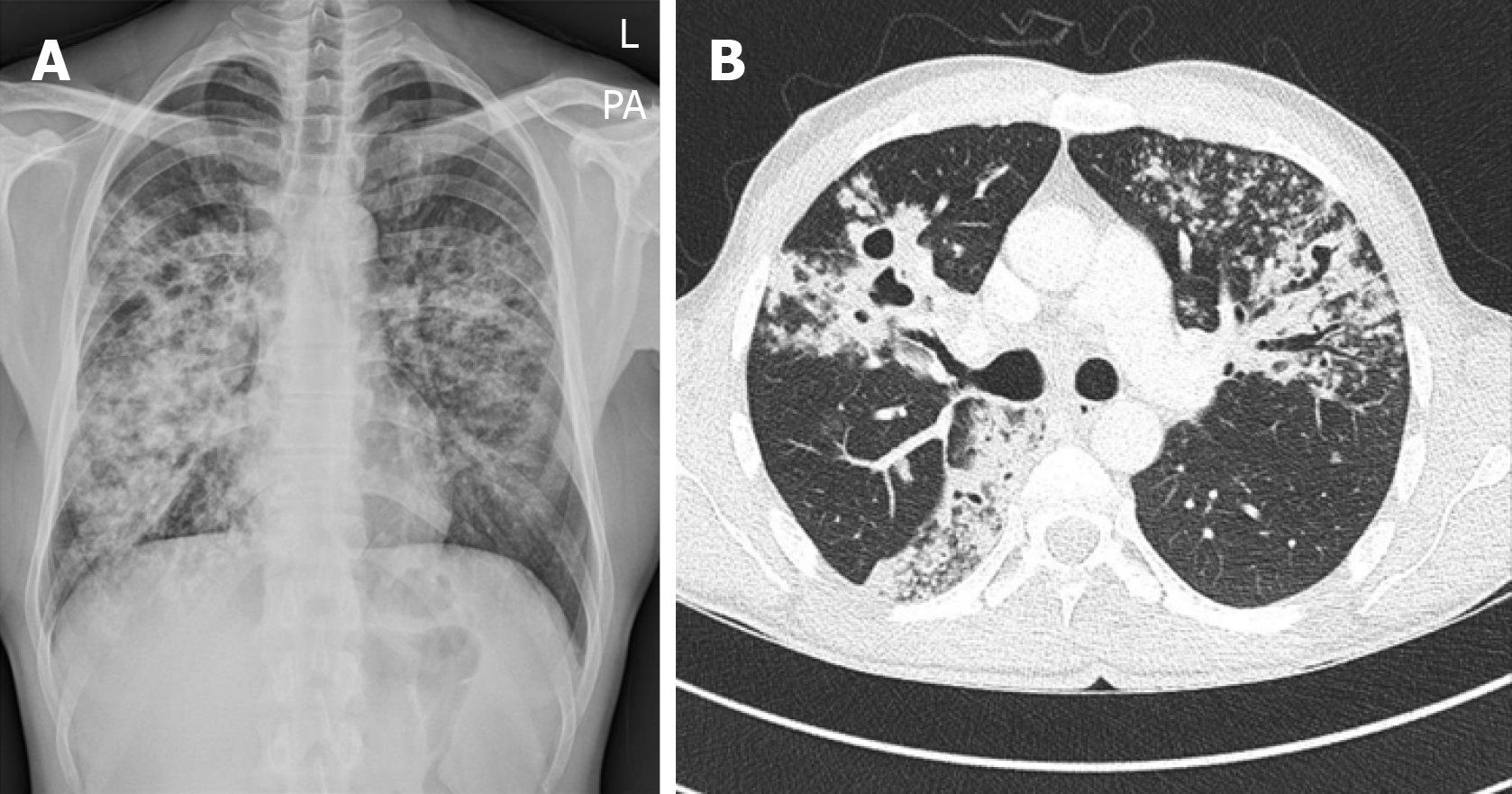
Chest radiography revealed diffuse, ill-defined heterogeneous nodular to confluent opacities, with multiple cavities in both lungs (Figure 1A). Chest computed tomography (CT) revealed four cavitary nodules with consolidation and centrilobular nodules in both lobes and lymphadenopathy in the right paratracheal, hilar, and subcarinal spaces (Figure 1B).
The AFB smear was grade three (3+) positive. The Xpert® MTB/RIF assay was positive but revealed no rifampin resistance.
He was ultimately diagnosed with multifocal CPTB.
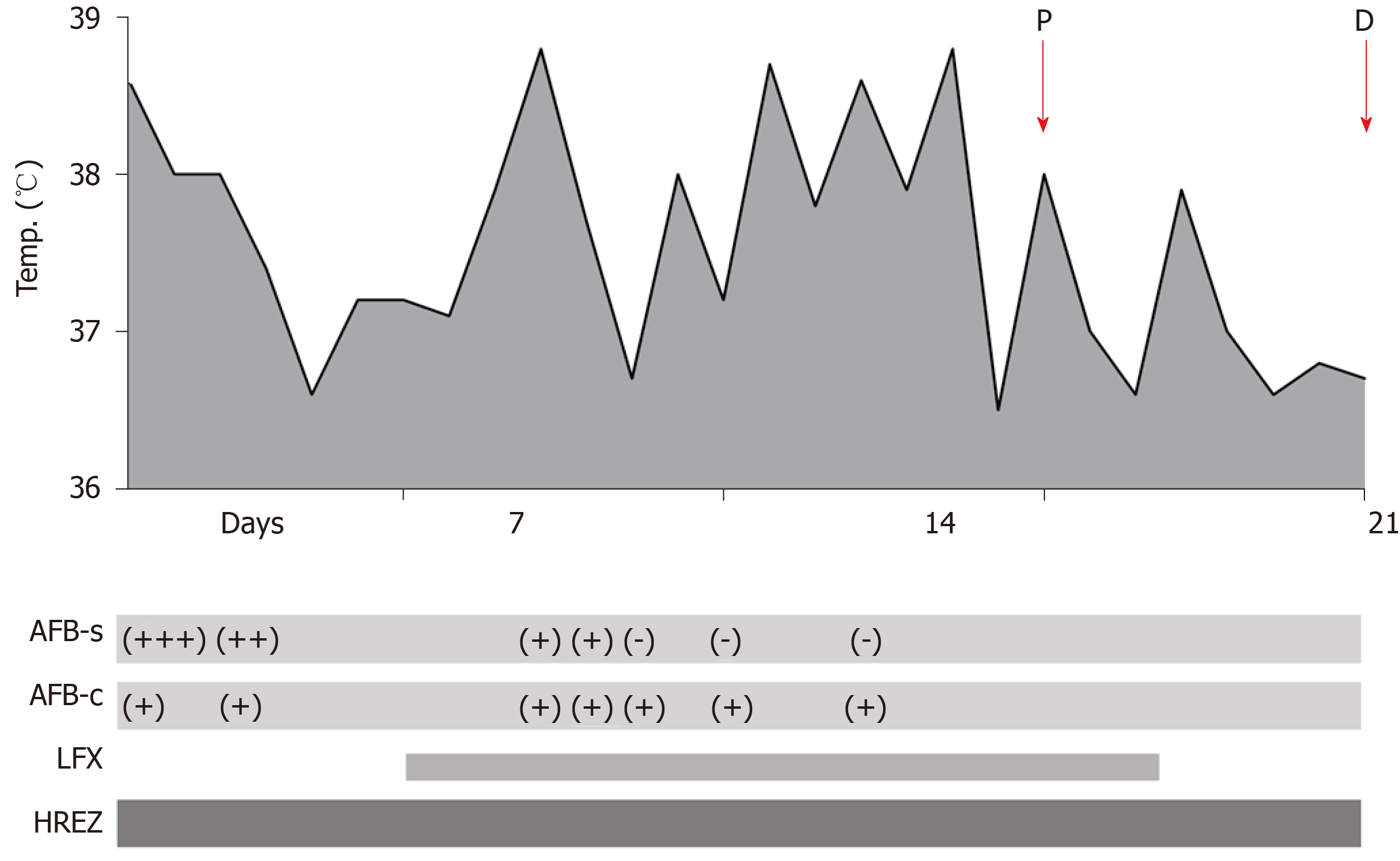
He was administered anti-TB medication (consisting of isoniazid, rifampin, ethambutol, and pyrazinamide) immediately following the diagnostic results. The doctor registered him as a patient with TB at the local public health authority and began to discuss the procedure for his return home. The spiking fever persisted for 3 wk and normalized after the twenty-fifth day (Figure 2). He underwent fiberoptic bronchoscopy on the second day of hospitalization, which revealed no endobronchial lesions, except for a moderate amount of purulent secretion in the right bronchi. On the seventh day, the physician added intravenous levofloxacin to the treatment regimen, owing to suspicions of comorbid pneumonia along with CPTB, for 16 d. levofloxacin was chosen because it is indicated for the treatment of community-acquired pneumonia, and it can also be used to treat TB.
Three consecutive AFB smears were negative, by the seventeenth day of hospitalization. Thus, the patient was eager to return home to India. However, his physician explained that CPTB, unlike non-CPTB, could be contagious for a more extended period, which means that he could still infect other passengers on the plane. Therefore, air travel could not be justified until it was confirmed that he was no longer infectious. Following discussions between his physician and the local public health authority, his physician provided a medical certificate stating that the probability that the patient could infect other passengers was small, if he were to wear an appropriate N95 mask and was accompanied by an observer throughout the entire 8-hour flight. Through his agent in Korea he sought an airline, which would allow him to board under these conditions.
One airline informed him that they would authorize boarding, if he met the stipulated conditions on his twenty-first day of hospitalization. Eventually, his company sent two co-workers to South Korea, who helped him embark; he was able to meet the prerequisite conditions and boarded the plane to India on the twenty-eighth day since hospitalization (Figure 2). All the sputum AFB tests, including the three negative smears, were cultured after his departure. A drug-susceptible test from his first (cultured) MTB assay revealed that his TB was all drug-sensitive. The Korean agent conveyed the results of drug-susceptible test to the patient.
The WHO stipulates that infectious TB consists entirely of respiratory (pulmonary or laryngeal) TB, which is sputum smear-positive and culture-positive, while potentially infectious TB is sputum smear-negative and culture-positive. The WHO recommends that individuals with both, infectious and potentially infectious TB should avoid traveling by commercial air transportation on flights of any duration[8]. Meanwhile, The European Centre for Disease Prevention and Control advises that patients with infectious pulmonary can be allowed to board commercial flights, after receiving adequate treatment with clinical improvement for a minimum of 2 wk[9]. In contrast, in the United Kingdom, the National Institute for Health and Care Excellence recommends that fellow passengers are not routinely required to be contacted, following a diagnosis of TB in an aircraft traveler[11]. These inconsistencies make it difficult to follow a given set of guidelines[12].
AFB smear results are available in a few minutes or hours unless the test is performed just before a weekend or holiday. While AFB culture results are available after at least 6 wk, based on the solid medium used[13]. Since patients with CPTB could be contagious for longer periods than those with non-CPTB, it may take several months or more, until the culture conversion yields two consecutive negative results. This also means that it may take a long time to prove that a patient is non-infectious, even if they really are no longer contagious. According to the criteria stipulated by the WHO, patients with CPTB, such as the one, in this case, would be considered to have potentially infectious TB. They may be prevented from undertaking air travel for a long time, which can be problematic if air travel is inevitable for these patients. Therefore, further research is required in the development of detailed, comprehensive guidelines related to the air travel of patients with CPTB.
Meanwhile, the CDC recommends that surgical masks must be worn by patients in ambulances and other vehicles transporting patients with infectious TB[14]. To reduce the number of droplets exhaled into the air by these patients, it is recommended that they should wear a surgical mask, specifically designed to thwart their spread[14]. Nevertheless, there are several reasons why the patient, in this case, had to wear an N95 mask, instead of a surgical mask in the airplane.
First, other than the patient, who had to wear a surgical mask, the airline could not make all the passengers wear an N95 mask. Since the patient was still considered potentially infectious based on the incomplete status of his culture results, all the other passengers would be required to wear an N95 mask, to fulfill CDC recommendations. A surgical mask does not offer complete protection from an airborne infection such as TB. Dharmadhikari et al[15] reported that a surgical mask could significantly reduce the spread of airborne multidrug-resistant TB infection by 56%, but this may not be universally applicable. Respirators are designed to protect health-care workers and other individuals from inhaling droplet nuclei. Therefore, medical staff and health-care workers should wear respirators, such as an N95 mask in a room, even if the room is an airborne infection isolation room and the patients with suspected or confirmed infectious TB is wearing a surgical mask, because others people are present[14]. Since the airline could not comply with these conditions, the physician was forced to look for another way to minimize airborne TB infection.
Second, when the physician tried to fit the N95 mask (Kimberly-Clark), the patient did not find it difficult to breathe and found that he would be able to tolerate the long flight home well. Moreover, the patient was taught to manually seal the N95 mask more tightly when coughing or sneezing. Therefore, even if the patient coughed or sneezed excessively, the N95 mask was sealed.
Third, the patient wore the N95 mask because it could prevent the exhalation of droplet nuclei while coughing, to the same extent or better than a surgical mask[16,17]. Wood et al[18] investigated whether face masks could reduce the aerosol concentration of Pseudomonas aeruginosa in the cough of patients with cystic fibrosis. They demonstrated that even though participants were unable to touch or readjust their masks during the testing period, both surgical and N95 masks were highly effective in lowering the concentrations of aerosols containing viable Pseudomonas aeruginosa in droplet nuclei of varying sizes when patients with cystic fibrosis were made to cough voluntarily. Moreover, when the patient inevitably took off his mask during a meal or to drink water, he was instructed to seal the mask manually on his mouth as tightly as possible if he felt that he was about to sneeze or cough. Therefore, we believe that the N95 mask could be more effectively sealed than the surgical mask if it is tolerated well by the patient. However, further research may be required to prove this, and surgical masks, which can be more effectively sealed may be developed in the future.
In this case, the patient was confirmed to have three consecutive negative AFB smears in 17 d following proper anti-TB medication. However, all the AFB cultures were later found to be positive, and additional AFB tests were not performed periodically for economic reasons. Since the culture results could not be confirmed until the patient’s return, the physician was forced to have the patient meet two prerequisite conditions to ensure that other passengers, who boarded the same plane would remain safe and not get infected.
According to the Ulsan University Hospital’s protocol, even if pneumonia is confirmed or the possibility of non-tuberculous mycobacterium infection is high, the patient should be preemptively isolated, if comorbid respiratory TB is suspected. If proper sputum specimens cannot be obtained through sputum induction, or if the imaging test is abnormal, fiberoptic bronchoscopy with AFB smear/culture tests, polymerase chain reaction testing for TB, Xpert® MTB/RIF assay, and serum Interferon-Gamma Release Assay may be performed. If the AFB smear and Xpert results are negative, we think that the patient should be removed from isolation, while wearing a surgical mask. If TB cannot be ruled out, isolation can be extended according to the hospital’s protocol. In South Korea, the state subsidizes the costs of the appropriate isolation of patients with TB, effectively charging patients only for multi-user room costs, thereby reducing the financial burden.
Herein, we reported the case of a patient with CPTB who was allowed to board a commercial airplane, wearing an N95 mask, despite the lack of confirmation of culture conversion. The patient had potentially infectious TB according to the WHO criteria. Based on this case, we think that if air travel is unavoidable for patients with CPTB who are still considered potentially infectious, it might be possible to board the flight if proper anti-TB medication is administered, confirmatory AFB smear tests are negative, and a suitable N95 mask is worn under observation. Also, this case revealed the lack of specific air travel guidelines related to CPTB and appropriate masks and protocols. Therefore, further studies are required to assess the risk of airborne transmission of CPTB during air travel and to set appropriate guidelines and policies.
| 1. | Mitchison DA. Mechanisms of the action of drugs in the short-course chemotherapy. Bull Int Union Tuberc. 1985;60:36-40. [PubMed] |
| 2. | Frieden T. Toman's tuberculosis: case detection, treatment and monitoring - Questions and answers. 2nd ed. Geneva: World Health Organization 2004: 351. |
| 3. | World Health Organization. Tuberculosis and air travel. Second Edition. 2nd ed. Geneva: World Health Organization, 2006. |
| 4. | Al-Moamary MS, Black W, Bessuille E, Elwood RK, Vedal S. The significance of the persistent presence of acid-fast bacilli in sputum smears in pulmonary tuberculosis. Chest. 1999;116:726-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 5. | Blumberg HM, Burman WJ, Chaisson RE, Daley CL, Etkind SC, Friedman LN, Fujiwara P, Grzemska M, Hopewell PC, Iseman MD, Jasmer RM, Koppaka V, Menzies RI, O'Brien RJ, Reves RR, Reichman LB, Simone PM, Starke JR, Vernon AA; American Thoracic Society, Centers for Disease Control and Prevention and the Infectious Diseases Society. American Thoracic Society/Centers for Disease Control and Prevention/Infectious Diseases Society of America: treatment of tuberculosis. Am J Respir Crit Care Med. 2003;167:603-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1372] [Cited by in RCA: 1239] [Article Influence: 53.9] [Reference Citation Analysis (0)] |
| 6. | Singla R, Osman MM, Khan N, Al-Sharif N, Al-Sayegh MO, Shaikh MA. Factors predicting persistent sputum smear positivity among pulmonary tuberculosis patients 2 months after treatment. Int J Tuberc Lung Dis. 2003;7:58-64. [PubMed] |
| 7. | Saeed W. Cavitating pulmonary tuberculosis: a global challenge. Clin Med (Lond). 2012;12:40-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | World Health Organization. Tuberculosis and air travel: guidelines for prevention and control. 3rd ed. Geneva: World Health Organization, 2008. [PubMed] |
| 9. | European Centre for Disease Prevention and Control. Risk assessment guidelines for infectious diseases transmitted on aircraft (RAGIDA) – Tuberculosis; 2014 [cited 2019 Nov 4]. Available from: https://www.ecdc.europa.eu/en/publications-data/risk-assessment-guidelines-infectious-diseases-transmitted-aircraft-ragida-0. |
| 10. | Ahmedzai S, Balfour-Lynn IM, Bewick T, Buchdahl R, Coker RK, Cummin AR, Gradwell DP, Howard L, Innes JA, Johnson AO, Lim E, Lim WS, McKinlay KP, Partridge MR, Popplestone M, Pozniak A, Robson A, Shovlin CL, Shrikrishna D, Simonds A, Tait P, Thomas M; British Thoracic Society Standards of Care Committee. Managing passengers with stable respiratory disease planning air travel: British Thoracic Society recommendations. Thorax. 2011;66 Suppl 1:i1-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 146] [Cited by in RCA: 147] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 11. | Internal Clinical Guidelines Team (UK). Tuberculosis: prevention, diagnosis, management and service organisation: National Institute for Health and Care Excellence, 2016. [PubMed] |
| 12. | Abubakar I. Tuberculosis and air travel: a systematic review and analysis of policy. Lancet Infect Dis. 2010;10:176-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 33] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Lee HS, Kee SJ, Shin JH, Kwon YS, Chun S, Lee JH, Won EJ, Choi HJ, Kim SH, Shin MG, Shin JH, Suh SP. Xpert MTB/RIF Assay as a Substitute for Smear Microscopy in an Intermediate-Burden Setting. Am J Respir Crit Care Med. 2019;199:784-794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | CDC. Chapter 7 - Tuberculosis infection control; 2005 [cited 2019 Jan 26]. Available from: https://www.cdc.gov/tb/education/corecurr/pdf/chapter7.pdf. |
| 15. | Dharmadhikari AS, Mphahlele M, Stoltz A, Venter K, Mathebula R, Masotla T, Lubbe W, Pagano M, First M, Jensen PA, van der Walt M, Nardell EA. Surgical face masks worn by patients with multidrug-resistant tuberculosis: impact on infectivity of air on a hospital ward. Am J Respir Crit Care Med. 2012;185:1104-1109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 119] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 16. | Lee SA, Grinshpun SA, Reponen T. Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. Ann Occup Hyg. 2008;52:177-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 167] [Cited by in RCA: 147] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 17. | Grinshpun SA, Haruta H, Eninger RM, Reponen T, McKay RT, Lee SA. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Environ Hyg. 2009;6:593-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 241] [Cited by in RCA: 235] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 18. | Wood ME, Stockwell RE, Johnson GR, Ramsay KA, Sherrard LJ, Jabbour N, Ballard E, O'Rourke P, Kidd TJ, Wainwright CE, Knibbs LD, Sly PD, Morawska L, Bell SC. Face Masks and Cough Etiquette Reduce the Cough Aerosol Concentration of Pseudomonas aeruginosa in People with Cystic Fibrosis. Am J Respir Crit Care Med. 2018;197:348-355. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mousa HAL S-Editor: Dou Y L-Editor: A E-Editor: Qi LL