Published online Dec 26, 2020. doi: 10.12998/wjcc.v8.i24.6524
Peer-review started: September 25, 2020
First decision: October 18, 2020
Revised: October 26, 2020
Accepted: November 2, 2020
Article in press: November 2, 2020
Published online: December 26, 2020
Processing time: 85 Days and 8.1 Hours
Idiopathic adulthood ductopenia (IAD) is a chronic cholestatic liver disease of unknown etiology that usually presents as unexplained jaundice. It is characterized by adult onset, lack of autoantibodies, inflammatory bowel disease and loss of interlobular bile ducts.
This case presents a 27-year-old woman with elevation of transaminases and alkaline phosphatase without clinical symptoms. Five years ago, the patient had abnormal transaminases but no cholestasis. Three months before admission, physical examination revealed an increase in transaminases. Oral hepatoprotective drugs did not show any significant improvement, and she was admitted to hospital for further diagnosis and treatment. Liver biopsy confirmed IAD. After about 2 wk of ursodeoxycholic acid treatment, serological and histological examination showed a significant response.
IAD is a manifestation of cholestasis, but also may be an abnormal increase in transaminase in the early stage.
Core Tip: Idiopathic adulthood ductopenia (IAD) is a chronic cholestatic liver disease that has unclear etiology, usually manifested as cholestasis. We report a case with no cholestasis or obvious clinical symptoms, only an increase in transaminases. The diagnosis of IAD relies on liver tissue biopsy. However, this examination is invasive and thus not acceptable by all patients. Therefore, in the clinical diagnostic process, many cases of unexplained liver damage and jaundice are missed. Furthermore, this case proved that the application of ursodeoxycholic acid has an obvious positive effect in the treatment of IAD.
- Citation: Zhang XC, Wang D, Li X, Hu YL, Wang C. Idiopathic adulthood ductopenia with elevated transaminase only: A case report. World J Clin Cases 2020; 8(24): 6524-6528
- URL: https://www.wjgnet.com/2307-8960/full/v8/i24/6524.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i24.6524
Idiopathic adulthood ductopenia (IAD) is a rare chronic liver disease that is often misdiagnosed. IAD was first described in 1988 by Ludwig et al[1], with interlobular bile ducts disappearing without a clear origin[2]. So far, less than 100 cases have been reported[3]. In recent years, the pathology and pathogenesis of bile duct loss have been widely studied, and a number of hepatobiliary diseases have been added to the list of ductopenic diseases[4]. IAD is a special type of ductopenic disease that is characterized by adult onset, autoantibodies negative, inflammatory bowel disease and absence of interlobular bile ducts[5].
This report presents a case that had no obvious clinical symptoms. The patient was diagnosed with IAD and was treated with ursodeoxycholic acid (UDCA).
A 27-year-old female was hospitalized for continuous elevation of transaminases and alkaline phosphatase without clinical symptoms or signs.
The patient had abnormally elevated transaminases at physical examination 5 years ago, but this was not concerning to her. The patient found abnormal transaminases again at physical examination 2 years ago, and was admitted to the hospital. After admission, the patient was tested for ceruloplasmin, which was negative. The patient had no viral hepatitis markers, and autoantibodies were absent. The patient was discharged from the hospital when her liver function improved after hepatoprotective treatment. In the past 2 years, liver function was rechecked three times, and it was still abnormal. Liver function test results 3 mo before the present admission were: Aspartate transaminase (AST) 213.8 U/L (0-40 U/L), alanine transaminase (ALT) 321.8 U/L (0-40 U/L), alkaline phosphatase (ALP) 317 U/L (15-112 U/L) and γ-glutamyltransferase (GGT) 172.1 U/L (7-32 U/L). After oral bicyclol treatment (25 mg/d), liver function was rechecked 8 d before admission, showing the following results: AST 251 U/L (13-35 U/L), ALT 419 U/L (7-40 U/L), ALP 337 U/L (35-100 U/L) and GGT 232 U/L (7-45 U/L). There were no improvements, so the patient was admitted to the hospital again.
The patient had taken oral Chinese medicine to treat folliculitis 3 years ago.
The patient did not have any family history.
The liver area was sensitive to light palpation, and there were no obvious positive signs.
Her liver function results were as follows: AST 169.5 U/L, ALT 261.5 U/L, ALP 231.6 U/L and GGT 167.7 U/L; erythrocyte sedimentation rate: 24 mm/h (2-20 mm/h); five items of immunity: Immunoglobulin G 21.50 g/L (6-16 g/L), complement C3 1.47 g/L (0.7-1.28 g/L) and antinuclear antibody normal. There were no abnormalities in hepatitis B and C markers, Treponema pallidum antibody, anti-human immunodeficiency virus antibody, antimitochondrial antibody M2 and tumor markers.
Multi-row computed tomography of the liver, gallbladder, spleen and pancreas demonstrated diffuse fatty liver or chronic liver injury.
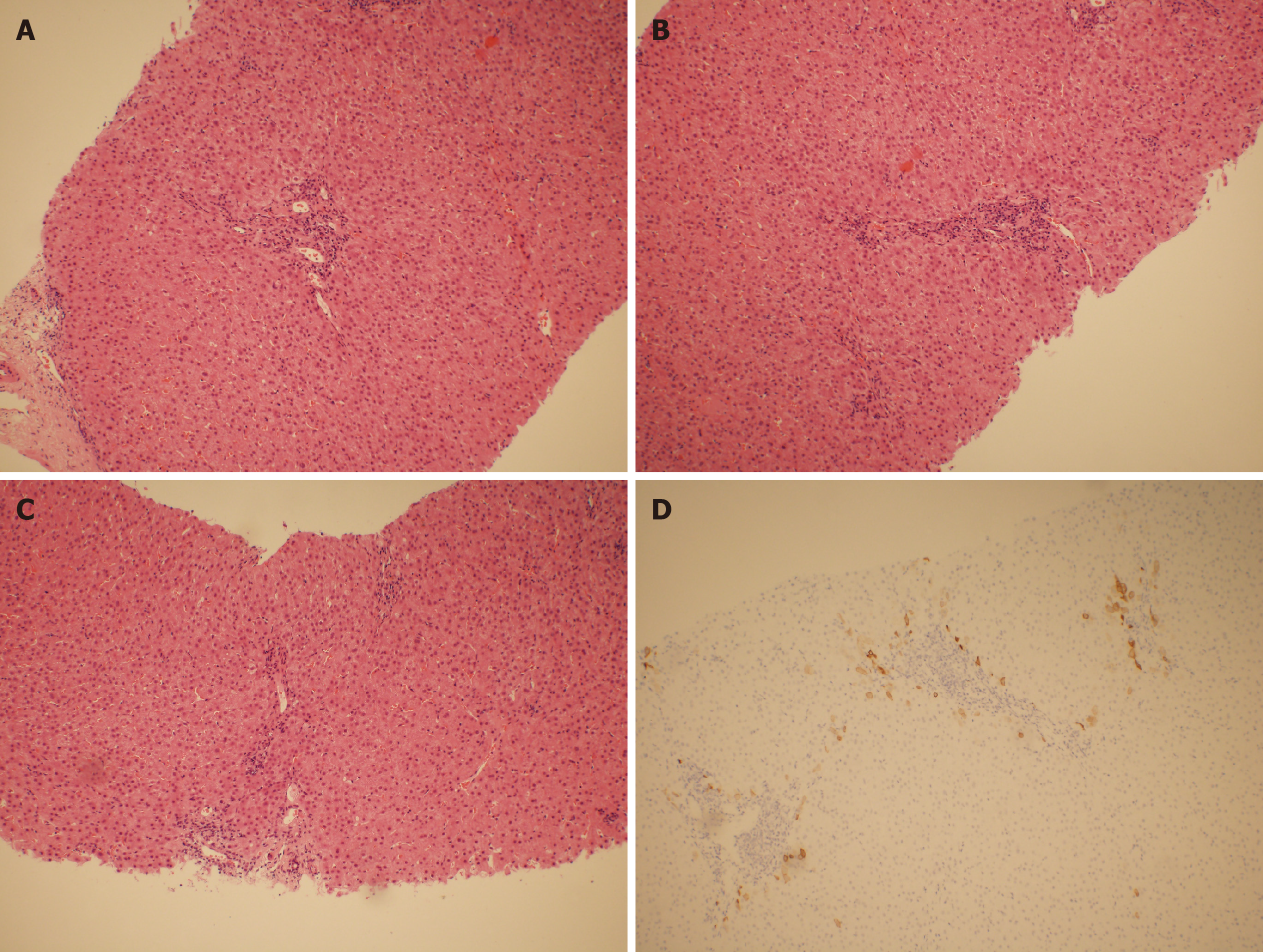
After 5 d of hepatoprotective treatment, the liver function was rechecked, with AST 130.4 U/L, ALT 84.8 U/L, ALP 236.9 U/L and GGT 194.4 U/L. AST and ALT decreased significantly, but ALP and GGT did not improve significantly. After that, liver biopsy was performed, and the pathological results suggested the following: (1) Local I with balloon-like degeneration of hepatocytes, mild expansion and fibrosis in some portal areas, infiltration of plasma cells and a few lymphocytes in the stroma. (2) Part of the inherent bile duct disappeared (> 50%), degeneration of the bile duct and mild hyperplasia of the thin bile duct (Figure 1). It was recommended to exclude vanishing bile duct syndrome. Pathological results at Beijing Youan Hospital were: (1) Vanishing bile duct syndrome; (2) More plasma cell infiltration and focal interfacial inflammation in portal areas; and (3) Lobular hepatitis in the recovery period that may have been related to recent medication.
IAD.
The patient was given UDCA (250 mg twice daily) after admission.
Re-examination of liver function after 2 wk of treatment showed that AST and ALT had returned to normal, and ALP was 146.1 U/L and GGT 114.8 U/L. According to the pathological results, the treatment was considered effective.
This patient was a young female without a clear cause of IAD. A retrospective medical history revealed that there were abnormal transaminases 5 years ago, but no cholestasis. There were no obvious clinical symptoms, but only mild percussion pain in the liver area. Imaging examinations after admission suggested chronic liver injury. The abnormal liver function was mainly due to elevated a-fetoprotein and GGT accompanied by mild cholestasis, so autoimmune liver disease was considered. Related laboratory tests excluded the possibility of autoimmune hepatitis and primary biliary cholangitis. Although the patient had a history of oral Chinese medicine, liver function tests showed abnormal transaminases before taking the medicine, so it is unlikely that IAD was caused by drug-induced liver injury. Therefore, the diagnosis depended on liver biopsy. The patient had a normal extrahepatic biliary tract and had no evidence of inflammatory bowel disease. A liver biopsy specimen presented loss of interlobular bile ducts from > 50% of the portal area. Combined with liver histological features, a diagnosis of IAD was made.
The diagnostic criteria for IAD include the following: (1) The patient must be an adult or at least an adolescent; (2) Biopsy ought to show a reduction in intrahepatic bile ducts in at least 50% of the portal areas; and (3) There should be no identifiable causes of cholestasis[1]. As for therapy, related research has shown that some patients have improvement in liver function tests with UDCA[6]. Since the patient was admitted to hospital, she has been treated with UDCA. Liver biopsy can establish whether UDCA is effective for treatment of IAD. However, for patients with rapid disease progression, UDCA does not improve the condition, and they will ultimately require liver transplantation[7]. Cirrhosis caused by IAD has been reported in some cases, and its progression is faster than other types of cirrhosis[8].
IAD is a manifestation of cholestasis, but also may be an abnormal increase in transaminase in the early stage. For liver injury of unknown cause, when we exclude primary biliary cholangitis, autoimmune hepatitis and drug-induced liver injury, liver biopsy can be performed to clarify the diagnosis. For patients who have been diagnosed, long-term UDCA treatment should be used to reduce liver cell damage and help with liver cell repair and bile duct regeneration and reconstruction. UDCA has a positive effect on the long-term prognosis of the disease. Further examinations are still necessary to evaluate the recovery of bile ducts and arrest the disease progress in a timely manner.
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Frascio M S-Editor: Gao CC L-Editor: Filipodia P-Editor: Li JH
| 1. | Ludwig J. Idiopathic adulthood ductopenia: an update. Mayo Clin Proc. 1998;73:285-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 53] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 2. | Ludwig J, Wiesner RH, LaRusso NF. Idiopathic adulthood ductopenia. A cause of chronic cholestatic liver disease and biliary cirrhosis. J Hepatol. 1988;7:193-199. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 105] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 3. | Bilal M, Kazemi A, Babich M. Idiopathic Adulthood Ductopenia: 'It Is Out There'. Case Rep Gastroenterol. 2016;10:95-98. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Nakanuma Y, Tsuneyama K, Harada K. Pathology and pathogenesis of intrahepatic bile duct loss. J Hepatobiliary Pancreat Surg. 2001;8:303-315. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 79] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Park BC, Park SM, Choi EY, Chae HB, Yoon SJ, Sung R, Lee SK. A case of idiopathic adulthood ductopenia. Korean J Intern Med. 2009;24:270-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Moreno A, Carreño V, Cano A, González C. Idiopathic biliary ductopenia in adults without symptoms of liver disease. N Engl J Med. 1997;336:835-838. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 41] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Müller C, Ulrich W, Penner E. Manifestation late in life of idiopathic adulthood ductopenia. Liver. 1995;15:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Douglass KM, Willner IR, Glenn DJ, Jones RM. Idiopathic Adulthood Ductopenia Causing Cirrhosis. ACG Case Rep J. 2020;7:e00349. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |