Published online Nov 6, 2020. doi: 10.12998/wjcc.v8.i21.5415
Peer-review started: June 22, 2020
First decision: July 24, 2020
Revised: August 5, 2020
Accepted: September 29, 2020
Article in press: September 29, 2020
Published online: November 6, 2020
Processing time: 136 Days and 19.8 Hours
Gallbladder adenoma is a relatively rare benign tumor with a potential for malignant transformation if found to be greater than 1 cm in size.
Herein, we report a case of a 51-year-old female with large 3 cm × 3 cm mass of gallbladder adenoma that was misdiagnosed as adenocarcinoma due to its clinical presentation. Computed tomography and magnetic resonance imaging scans showed an irregularly shaped cauliflower-like lump in the gallbladder measuring 38 mm × 32 mm corresponding to a malignant tumor and several gallbladder stones with low diffusion-weighted imaging and equisignal of T1-weighted imaging and T2-weighted imaging; moreover, the CA 19-9 levels were very high (184.1 U/mL). Pathology reports after tumor resection showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration.
Computed tomography and magnetic resonance imaging scans need to be carefully scrutinized in certain rare cases of adenomas with abnormal imaging features.
Core Tip: Computed tomography and magnetic resonance imaging scans showed an irregularly shaped cauliflower-like lump in the gallbladder measuring 38 mm × 32 mm corresponding to a malignant tumor and several gallbladder stones with low diffusion-weighted imaging and equisignal of T1-weighted imaging and T2-weighted imaging; moreover, the CA 19-9 levels were very high (184.1 U/mL). Pathology reports after tumor resection showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration.
- Citation: Cao LL, Shan H. Large and unusual presentation of gallbladder adenoma: A case report. World J Clin Cases 2020; 8(21): 5415-5419
- URL: https://www.wjgnet.com/2307-8960/full/v8/i21/5415.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i21.5415
Gallbladder adenomas (GBA) are primary neoplasms of the gallbladder that are not very common and are estimated to be found in about 0.1%-10% of cholecystectomy cases. These benign tumors that usually present as single polypoid masses are classified as tubulary, papillary and tubulopapillary based on histological morphology. GBA are categorized as pyloric gland, intestinal and biliary type adenomas depending on their origin. GBA occur in mostly in females and middle-aged individuals[1,2]. Gallbladder adenocarcinoma (GBC), a malignant tumor of the biliary tract, is known to be the fifth common neoplasm of the digestive tract[3]; it varies in its geographical distribution and ethnicity[4]. Presence of cholelithiasis, polyps bigger than 1 cm in diameter, female gender, advancing age, increased body mass index and chronic gallbladder inflammation are some of the risk factors for GBC[5]. GBA are usually smaller than 20 mm in size[6], and those that are more than 1cm in size have a risk of developing into adenocarcinomas[2]. In the current report, we present the clinical data, images and pathological results of a case of gallbladder adenoma of size 3 cm × 3 cm that was misdiagnosed as adenocarcinoma due to its unusual clinical presentation.
A 51-year-old female of Han Chinese ethnicity from Nanjing, Jiangsu province of China, presented at the Emergency Department of our institution (Jiangsu Second Hospital of Traditional Chinese Medicine) with an acute pain in the right upper quadrant of her abdomen on August 2, 2017.
The pain was colic and radiated to the back. Concomitant symptoms included nausea, vomiting and diarrhea but no fever or chills. Neither weight loss nor anorexia was observed. She was prescribed omeprazole once a day for 2 d and sent home. Although the medication gave her temporary relief from the pain, she continued to experience severe abdominal spasms.
There was no previous medical history of hypertension, diabetes, coronary heart disease, hepatitis, tuberculosis, typhoid fever and other infectious diseases. There was also no history of trauma, surgery, blood transfusion or recent vaccination.
Physical examination revealed no abdominal lumps, jaundice or itchy skin. Tenderness was observed in the right upper quadrant with a positive Murphy’s sign. There was no rebound tenderness.
Results of routine blood and urine tests were normal. Liver function test results showed higher than normal values (alanine transaminase: 164 U/L, aspartate transaminase: 179 U/L, gamma-glutamyltransferase: 371 U/L). Levels of CA19-9 were found to be elevated at 184.1 U/mL. Levels of other tumor markers were as follows: alpha-fetoprotein: 7.53 ng/mL, carcinoembryonic antigen: 1.87 ng/mL, CA125: 12.56 U/mL, CA153: 18.54 U/mL and CA724: 1.18 U/mL.
Abdominal computed tomography (CT) scan showed pathological conditions corresponding to a large cauliflower-like mass in the gallbladder. CT (Figure 1) and magnetic resonance imaging (MRI, Figure 2) scans performed on August 4, 2017 revealed an irregularly shaped cauliflower-like lump in the gallbladder measuring 38 mm × 32 mm corresponding to malignant tumor (GBC) and multiple stones in the gallbladder. T1-weighted imaging and T2-weighted imaging (T2WI) were equisignal with low diffusion-weighted imaging (DWI) signal. There was no detectable extension through the gallbladder wall or invasion of adjacent structures. The biliary system was normal with no associated hepatic lesions and no apparent liver damage or abnormalities in the cystic duct, common hepatic duct or intrahepatic ducts.
Pathology reports after tumor resection showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration.
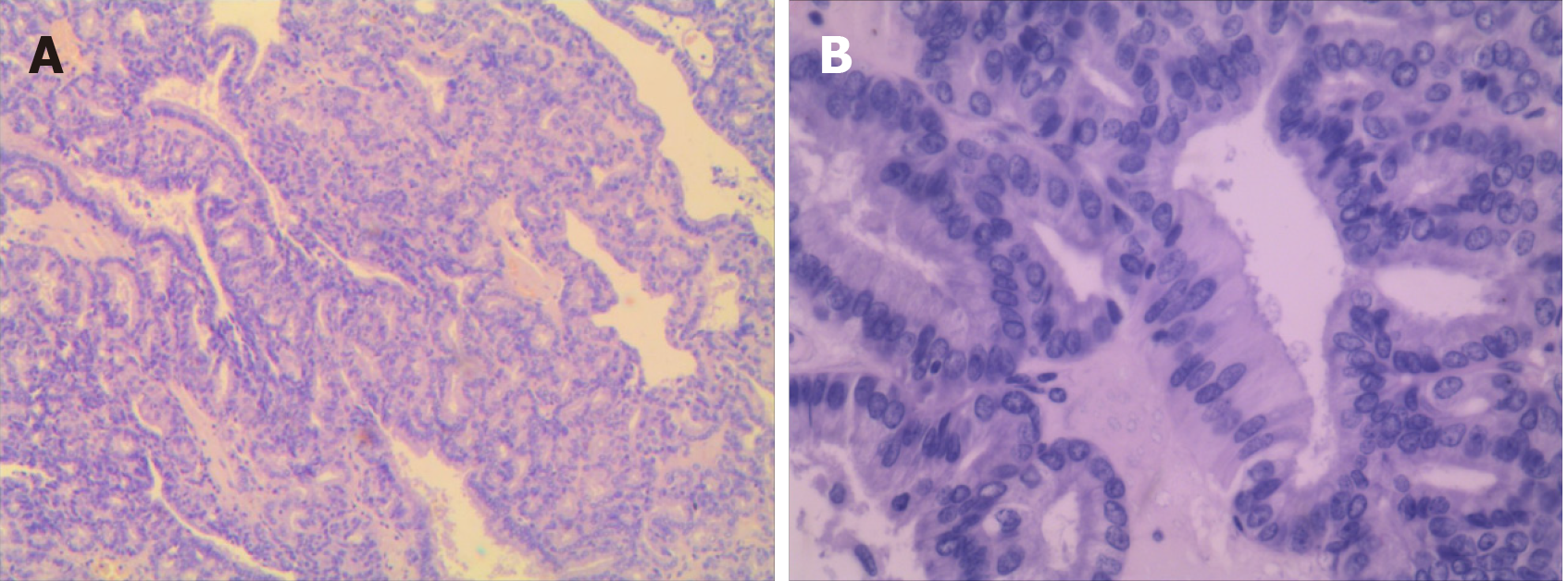
As per the patient’s wishes, laparoscopic cholecystectomy was performed under general anesthesia. Intraoperative probe revealed no obvious abnormality in the liver, common bile duct dilation with mild adhesion of the omentum to the gallbladder, gallbladder bile duct expansion, gallbladder size about 10 cm × 5 cm and no invasion of the serosal layer. Irregular masses measuring 3 cm × 3 cm and several stones of different sizes in the gallbladder were found at surgery. The resected samples were sent for histopathological examination. After the surgery, the patient was treated with medications that included anti-inflammatory, acid inhibition, gastric protection, fluid supplementation, water and electrolyte balance and anticoagulation. The patient was discharged without any complications. Pathological assessment of the tumors showed adenoma with moderate epithelial atypia and moderate atypia in the focal area with fine pedicle and no clear infiltration (Figure 3).
A follow-up was conducted on September 18, 2017. Ultrasound examination showed no evidence of any abnormality in the gallbladder area.
The incidence of GBA, which are benign and highly vascularized tumors, is low[1]. They are generally asymptomatic unless there are multiple large adenomas or the tumor tissues are detached resulting in floating fragments in the bile duct or attached to the gallstones[7]. They usually appear as sessile polypoid isoechoic or hyperechoic lesions on imaging. Differentiating GBA from GBC might be difficult because polypoid lesion with arterial enhancement may be seen in early-stage adenocarcinoma[8]. On CT imaging, GBC appears as a mass completely occupying or replacing the gallbladder lumen, focal or diffuse asymmetric gallbladder wall thickening or an intraluminal polypoid lesion. GBA and GBC can sometimes coexist making diagnosis a challenge because wall thickening patterns or polypoid growth result in overlap of imaging findings leading to uncertainty in preoperative diagnosis[9].
In our patient, the misdiagnosis of GBA as GBC was due to: (1) The appearance of the lesion being irregular and cauliflower-shaped; (2) The lesion had a wide base; (3) Contrast-enhanced CT showed obvious and significantly enlarged masses consistent with the features of malignant tumors; and (4) CA19-9 levels of our patient were very high, which coincided with the fact that the patient presented the highest incidence of cholecystic carcinoma and that CA19-9 is considered a prognostic marker for GBC[9]. In this case, both T1WI and T2WI signals during MRI were equal, whereas for adenomas, T1WI signal is low and T2WI signal is high. Moreover, the diameter of the lesion that was more than 3 cm was confined to the gallbladder, and there was no distant metastasis. Hence, it was not easy to differentiate GBA from GBC. Interestingly in this case, the DWI signal was low, whereas the DWI signal is expected to be high in malignant tumor. Therefore, the diagnosis was not easy in this case. From this case, it is important to note that misdiagnosis can be prevalent due to large size of polypoid lesions with DWI signals being low and elevated levels of tumor markers; but physicians could check for T1WI and T2WI signals to be equal, which can give an estimation whether the tumor is GBA.
Recently, techniques such as multidetector CT, high-resolution ultrasound and use of apparent diffusion coefficient and lesion to spinal cord ratio DWI have been proposed to increase the diagnosis and differentiation between malignant and benign tumors[10,11]. In spite of these technical advancements, the detection of gallbladder cancer from clinical and imaging data at curative stages still remains tricky and challenging. GBA are reported to be benign lesions of cauliflower shape, narrow base, with mulberry shape and uniform reinforcement. DWI can help to differentiate GBC from adenoma and well-differentiated from higher-grade adenocarcinoma[12]. GBC is highly suspected when a large gallbladder mass that nearly fills or replaces the lumen and often directly invades the surrounding liver parenchyma. GBA is often confined to the gallbladder and it will not infiltrate the surrounding structure. Generally, in gallbladder adenoma, the CA19-9 level is not high[13]; in our patient, this tumor index increased significantly. Therefore, careful examination of MRI along with other clinical and laboratory examination could improve the diagnostic accuracy.
In conclusion, our case report highlights the importance for oncologists to carefully evaluate characteristic imaging appearances and values of CT/MRI scans of primary gallbladder tumors to determine the stage of cancer for appropriate treatment regimen. The incidence of gallbladder adenoma is relatively low and is predisposed to malignancy. Hence, carefully distinguishing between GBA and GBC is necessary for optimizing the treatment strategy for the patients.
| 1. | Gaur JH, Khan S, Hasan J, Jetley S, Husain M. Adenomatous Polyposis of Gall Bladder: A Rare Presentation in HCV Positive Female. IJPRP. 2017;6:998-1001. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Jian YX, Li Zhu, Han L, Xing YY, Lu FC, Wu SY, Wang JP. Imaging diagnosis of gallbladder adenoma. Biomed Res. 2018;29:238-242. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Goetze TO. Gallbladder carcinoma: Prognostic factors and therapeutic options. World J Gastroenterol. 2015;21:12211-12217. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 173] [Cited by in RCA: 210] [Article Influence: 19.1] [Reference Citation Analysis (1)] |
| 4. | Sharma A, Sharma KL, Gupta A, Yadav A, Kumar A. Gallbladder cancer epidemiology, pathogenesis and molecular genetics: Recent update. World J Gastroenterol. 2017;23:3978-3998. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 212] [Cited by in RCA: 287] [Article Influence: 31.9] [Reference Citation Analysis (4)] |
| 5. | Zimmermann A. Adenocarcinoma of the Gallbladder: Risk Factors and Pathogenic Pathways. In: Tumors and Tumor-Like Lesions of the Hepatobiliary Tract. Springer, Cham. 2016: 1-10. [DOI] [Full Text] |
| 6. | Jin W, Zhang C, Liu J, Zhao Z. Large villous adenoma of gallbladder: A case report. Int J Surg Case Rep. 2013;4:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Yang G, Qin H, Raza A, Saukel GW, Solomon N, Michelotti M, Raghavan R. Pyloric gland adenoma of gallbladder-reports of two cases and a brief review of literature. J Gastrointest Oncol. 2016;7:S81-S87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 8. | Lin LY, Chiou HJ, Chou YH, Wang HK, Lai YC, Lin YH. A Case of Tubular Adenoma of Gallbladder Diagnosed Using Contrast-Enhanced Ultrasonography. J Med Ultrasound. 2018;26:218-221. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Wang YF, Feng FL, Zhao XH, Ye ZX, Zeng HP, Li Z, Jiang XQ, Peng ZH. Combined detection tumor markers for diagnosis and prognosis of gallbladder cancer. World J Gastroenterol. 2014;20:4085-4092. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 88] [Cited by in RCA: 105] [Article Influence: 8.8] [Reference Citation Analysis (2)] |
| 10. | Kim SW, Kim HC, Yang DM, Ryu JK, Won KY. Gallbladder carcinoma: causes of misdiagnosis at CT. Clin Radiol. 2016;71:e96-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 11. | Kitazume Y, Taura S, Nakaminato S, Noguchi O, Masaki Y, Kasahara I, Kishino M, Tateishi U. Diffusion-weighted magnetic resonance imaging to differentiate malignant from benign gallbladder disorders. Eur J Radiol. 2016;85:864-873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 12. | Lee NK, Kim S, Moon JI, Shin N, Kim DU, Seo HI, Kim HS, Han GJ, Kim JY, Lee JW. Diffusion-weighted magnetic resonance imaging of gallbladder adenocarcinoma: analysis with emphasis on histologic grade. Clin Imaging. 2016;40:345-351. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Chen Z, Liu Z, Zhang Y, Wang P, Gao H. Combination of CA19-9 and the Neutrophil-to-Lymphocyte Ratio for the Differential Diagnosis of Gallbladder Carcinoma. Cancer Manag Res. 2020;12:4475-4482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Nath J S-Editor: Huang P L-Editor: Filipodia P-Editor: Li JH