Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.5013
Peer-review started: June 22, 2020
First decision: July 28, 2020
Revised: July 30, 2020
Accepted: September 2, 2020
Article in press: September 2, 2020
Published online: October 26, 2020
Processing time: 125 Days and 19.6 Hours
Dieulafoy’s lesion is a rare vascular abnormality characterized by a small abnormally dilated artery that runs a tortuous course in the submucosa. There is usually no ulcer present in Dieulafoy’s lesions and the overlying mucosa is most often normal. Bleeding caused by a Dieulafoy’s lesion is usually urgent, massive, life-threatening and prone to recurrence. Dieulafoy’s lesions have been reported throughout the digestive tract although the majority of them have been found in the upper digestive tract especially the stomach and duodenum. However, a Dieulafoy’s lesion occurring inside a duodenal diverticulum is very rare.
A 74-year-old Asian male with epigastric pain, hematemesis and melena was admitted to our clinic. Before admission, the patient had vomited 500 mL of dark red blood, and passed 200 g of black tarry stool. Conservative management was first undertaken as the patient had not been fasting. However, hemorrhage recurred and the patient went into shock. Urgent endoscopy was performed and a diverticulum of 1.8 cm × 1.2 cm × 0.8 cm was found on the anterior wall of the descending duodenum. The diverticulum was covered with a blood clot. After the clot was removed, an artery stump was observed in the diverticulum with a diameter of 2-3 mm. Two titanium hemostatic clips were inserted to clamp the vessel stump. The patient was discharged 7 d post-endoscopy and followed for 6 mo with no recurrence.
This case was diagnosed with a Dieulafoy’s lesion inside a duodenal diverticulum which has rarely been reported. Hematemesis was stopped by clamping the vessel stump with titanium clips. No complications occurred.
Core Tip: Dieulafoy’s lesion is a rare vascular abnormality characterized by a small artery with an abnormally dilated caliber that runs a tortuous course in the submucosa. Bleeding caused by a Dieulafoy’s lesion is frequently urgent and massive, prone to recurrence, and life-threatening. Dieulafoy’s lesions have been reported throughout the digestive tract, but have rarely been reported inside a duodenal diverticulum.
- Citation: He ZW, Zhong L, Xu H, Shi H, Wang YM, Liu XC. Massive gastrointestinal bleeding caused by a Dieulafoy’s lesion in a duodenal diverticulum: A case report. World J Clin Cases 2020; 8(20): 5013-5018
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/5013.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.5013
Dieulafoy’s lesion is a rare vascular abnormality characterized by a small artery with an abnormally dilated caliber that runs a tortuous course in the submucosa. Bleeding is thought to be caused by a submucosal artery causing pressure necrosis of the overlying submucosa and mucosa in the absence of an ulcer. Bleeding caused by Dieulafoy’s lesions is usually urgent, massive, life-threatening and prone to recurrence. Dieulafoy’s lesions have been reported throughout the digestive tract although the majority of them were found in the upper digestive tract, including the stomach and duodenum. However, a Dieulafoy’s lesion occurring inside a duodenal diverticulum is very rare. Here, we report a case of massive hematemesis caused by a Dieulafoy’s lesion which was located inside a duodenal diverticulum.
A 74-year-old man was admitted to our clinic with epigastric pain, hematemesis and melena.
The patient complained of epigastric pain for 3 d. One day before he was admitted, the patient had hematemesis consisting of 500 mL of dark red liquid, followed by 200 g of black tarry stool. The patient felt dizzy, weak and had palpitations.
The patient denied a history of hypertension, diabetes, and other relevant illness. He also denied ever taking any medications including non-steroidal anti-inflammatory agents, anticoagulants and herbals.
The patient denied any positive family history.
Upon admission, his temperature was 36.5°C, heart rate was 97 bpm, blood pressure was 100/76 mmHg, and respiration rate was 20 breaths/minute. The patient was conscious, anemic looking, and bowel sounds were active.
Blood analysis revealed an erythrocyte count of 2.92 × 1012/L, hemoglobin of 91 g/L, and platelet count of 152 × 109/L. Fecal occult blood test was (+). Coagulation test revealed normal prothrombin time and international normalized ratio.
Abdominal CT scan (no contrast was used) upon admission showed no obvious abnormalities of the liver, gallbladder, biliary tract, spleen and pancreas.
After admission, the patient had nothing per os, and received intravenous fluid resuscitation and proton pump inhibitors. As the patient had eaten 2 h before admission, urgent endoscopy was postponed.
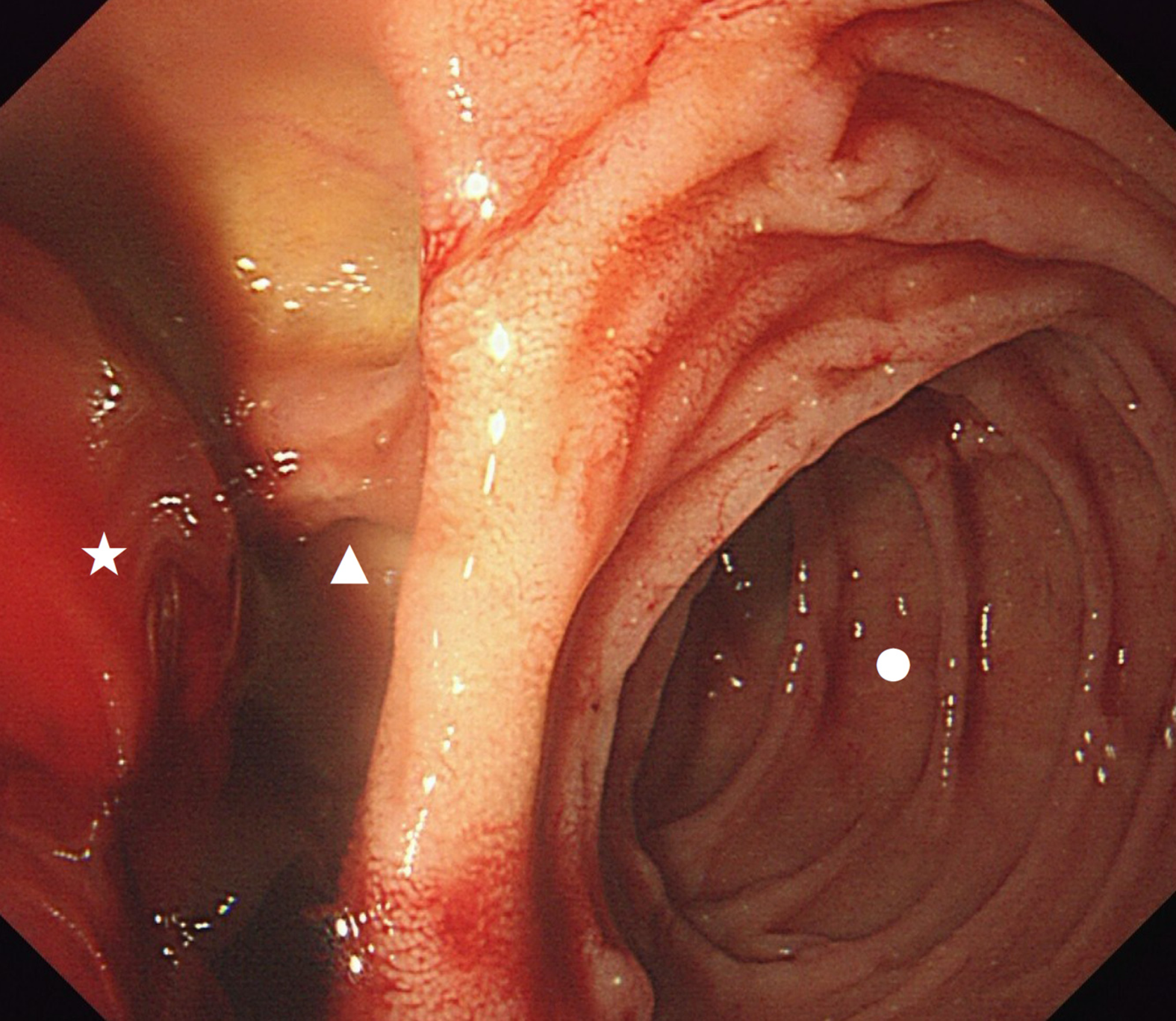
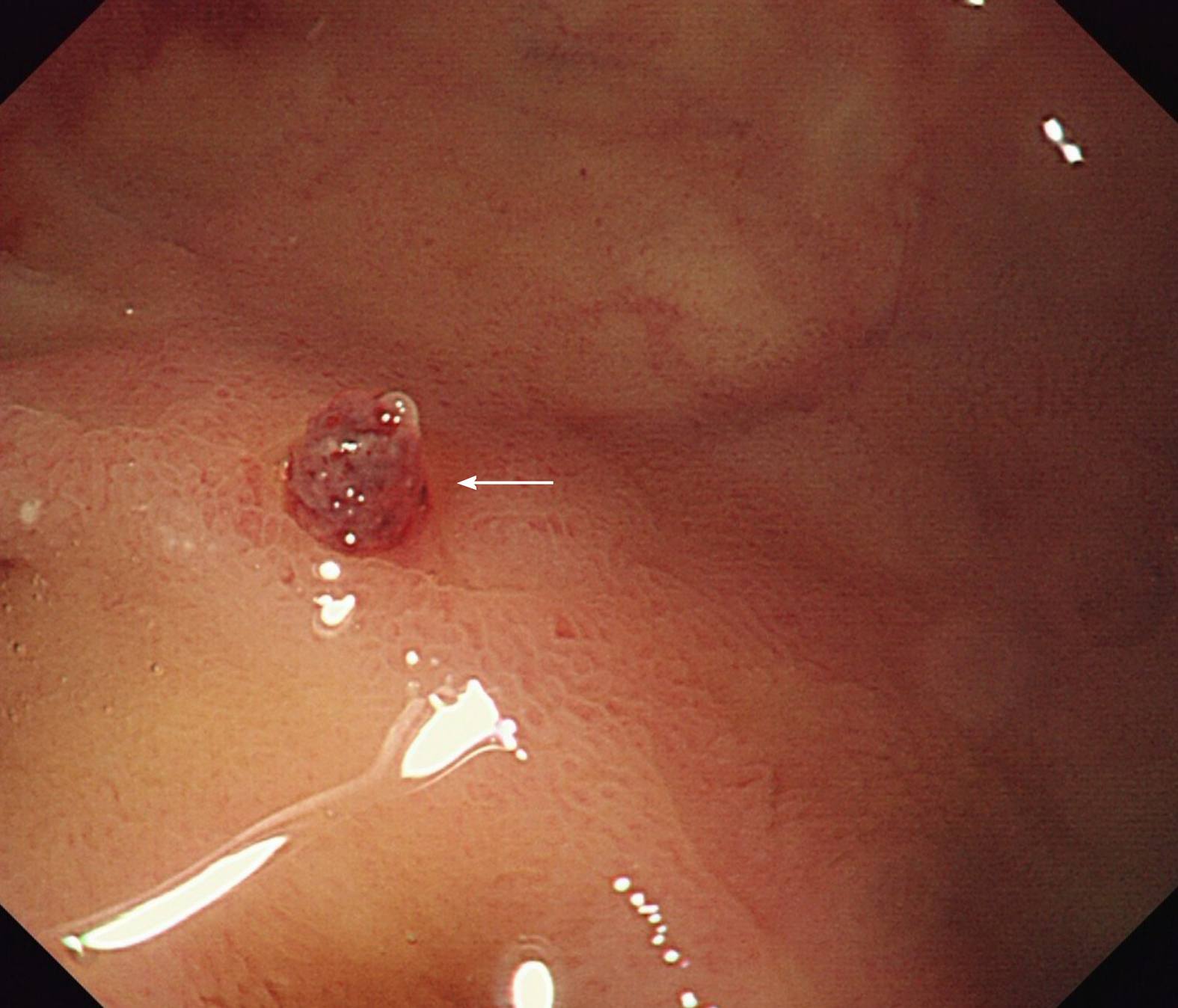
In the evening, the patient had 2 bouts of melena with a total weight of approximately 600 g, followed by increased heart rate (108 bpm), decreased blood pressure (88/50 mmHg) and hemoglobin (56 g/L). Red blood cell transfusion was given, and then urgent upper gastrointestinal endoscopy was performed. Endoscopy revealed a huge diverticulum (about 1.8 cm × 1.2 cm × 0.8 cm) in the anterior wall of the descending duodenum (close to the papilla) with a massive blood clot inside (Figure 1). A vessel stump with a diameter of 2-3 mm was exposed after removal of the clot (Figure 2).
The final diagnosis was massive upper gastrointestinal bleeding caused by a Dieulafoy’s lesion inside a duodenal diverticulum.
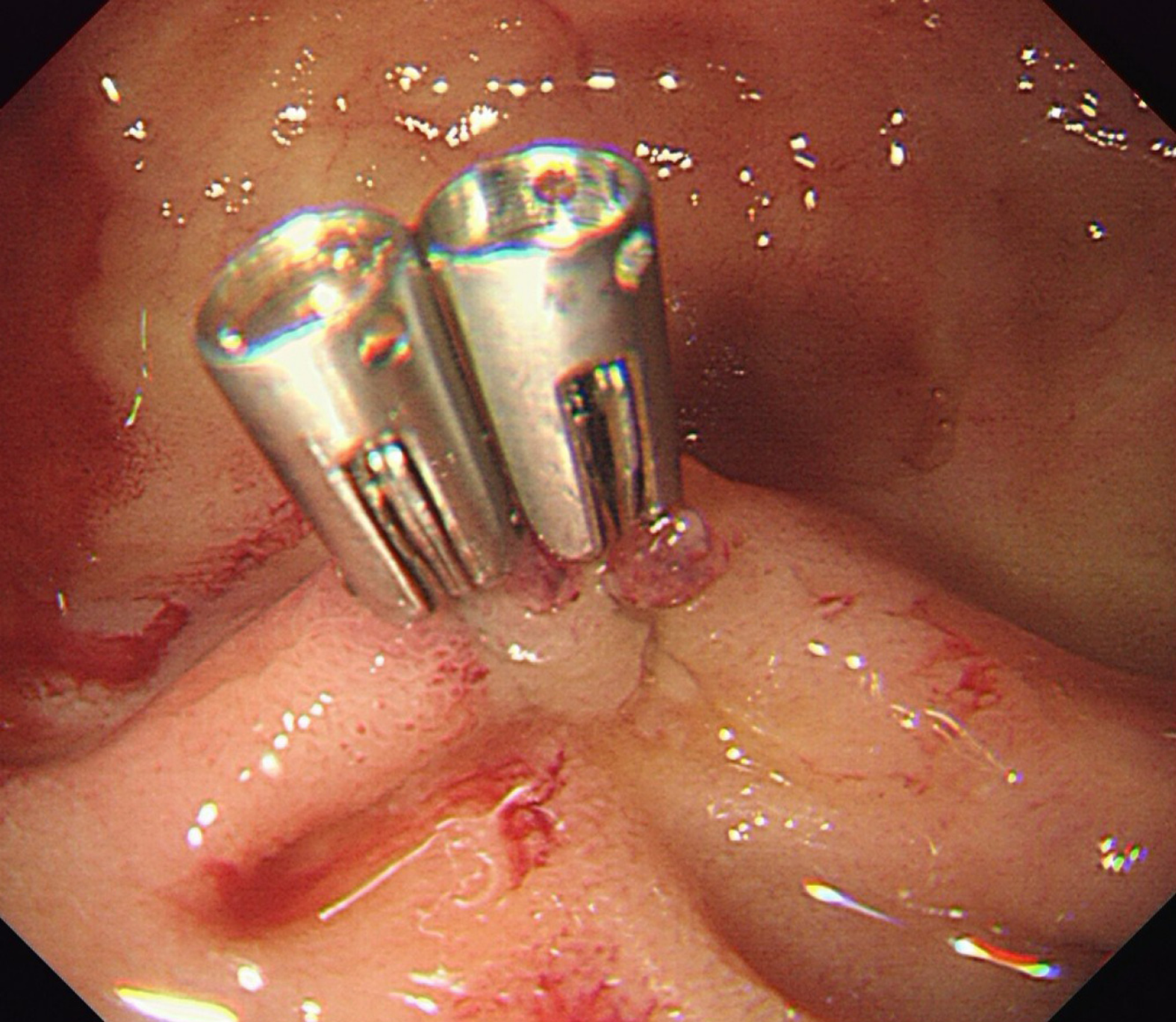
Two titanium clips were inserted to clamp the vessel stump (Figure 3). No active bleeding was observed after washing. Oral feeding with a cool liquid diet was initiated on the 1st day post-endoscopy.
No more hematemesis occurred, and melena stopped 3 d after endoscopy. The patient was discharged from hospital on the 7th day, and followed for 6 mo with no recurrence.
Dieulafoy’s lesion is a rare cause of digestive tract hemorrhage. It is a rare vascular abnormality characterized by a small abnormally dilated artery that runs a tortuous course in the submucosa[1]. Dieulafoy’s lesions are believed to be congenital, but they have been reported to occur more frequently with advancing age[2]. Dieulafoy’s lesions account for 1%-5.8% of acute gastrointestinal bleeding[3,4], but they often present with urgent and massive bleeding usually leading to shock, and even death. They also have a high rate of recurrence. Sometimes, the bleeding may cease spontaneously due to a drop in blood pressure and/or the formation of a blood clot. The arterial stump may retract and remain hidden beneath the mucosa making it very difficult to detect by endoscopy, or even surgery. Thus, a Dieulafoy’s lesion can be life-threatening.
Endoscopy has been reported to be the most effective method in diagnosing up to 70% of Dieulafoy’s lesions[2]. The endoscopic findings of Dieulafoy’s lesions are characterized by an isolated protruding vessel usually surrounded by normal mucosa or less commonly a small round or oval superficial ulcer[5,6]. The diameter of the vessel stump is usually between 1-3 mm[7]. The lesion may be actively bleeding including spurting or oozing, otherwise, it might be covered by a blood clot[5].
Dieulafoy’s lesions have been reported throughout the digestive tract with 8% in the esophagus, 71% in the stomach, 15% in the duodenum, 1% in the intestine, 2% in the colon, 2% in the rectum and 1% in gastric anastomosis[3]. Santos reported a case of a Dieulafoy’s lesion located in the gallbladder in 2020[1]. It is also reported that Dieulafoy’s lesions have been found outside the gastrointestinal tract, such as in the bronchus[8,9]. However, Dieulafoy’s lesions occurring inside a duodenum diverticulum are rare, with only 4 cases reported previously[10-13]. In the current case, the diverticulum was located in the descending duodenum where lesions are difficult to observe. There were no signs of inflammation or ulcer in the diverticulum, and the only clue was the blood clot. The exposed arterial stump could easily have been missed if the endoscopist had ignored the clot or did not wash away the clot to observe the inside of the diverticulum.
Due to urgent, massive, arterial bleeding, it is often difficult to stop the hemorrhage using common conservative therapies. Treatment by endoscopy has become the preferred and most effective way of managing a Dieulafoy’s lesion, with a reported success rate of over 90%[3]. Commonly used endoscopic hemostatic procedures include electrocoagulation, thermocoagulation, local epinephrine injection, sclerotherapy, banding, and hemoclips[7,14]. Mechanical hemostasis is considered to be more effective than injection or thermal treatment[14], and hemoclips are easier to manipulate compared to banding. The clips close the vessel stump, and a subsequent inflammation reaction forms granulation tissue which seals off the vessel. The clips fall off after 1-3 wk.
We report the case of an adult patient with massive hemorrhage of the digestive tract caused by a Dieulafoy’s lesion inside a duodenal diverticulum discovered and treated by endoscopy. Hemostasis was achieved by endoscopic placement of hemostatic clips. There were no complications. The patient was followed for 6 mo without recurrence.
| 1. | Santos T, Serra M, Oliveira A, Fernandes C. Dieulafoy lesion of the gallbladder: A rare cause of hemobilia and acute pancreatitis - Case report. Int J Surg Case Rep. 2020;66:207-210. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Marangoni G, Cresswell AB, Faraj W, Shaikh H, Bowles MJ. An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. J Pediatr Surg. 2009;44:441-443. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 43] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 3. | Baxter M, Aly EH. Dieulafoy's lesion: current trends in diagnosis and management. Ann R Coll Surg Engl. 2010;92:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 190] [Cited by in RCA: 190] [Article Influence: 11.9] [Reference Citation Analysis (0)] |
| 4. | Kolli S, Dang-Ho KP, Mori A, Gurram K. The Baader-Meinhof Phenomenon of Dieulafoy's Lesion. Cureus. 2019;11:e4595. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Chaer RA, Helton WS. Dieulafoy's disease. J Am Coll Surg. 2003;196:290-296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 6. | Yoshikumi Y, Mashima H, Suzuki J, Yamaji Y, Okamoto M, Ogura K, Kawabe T, Omata M. A case of rectal Dieulafoy's ulcer and successful endoscopic band ligation. Can J Gastroenterol. 2006;20:287-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Morowitz MJ, Markowitz R, Kamath BM, von Allmen D. Dieulafoy's lesion and segmental dilatation of the small bowel: an uncommon cause of gastrointestinal bleeding. J Pediatr Surg. 2004;39:1726-1728. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 24] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Tang P, Wu T, Li C, Lv C, Huang J, Deng Z, Ding Q. Dieulafoy disease of the bronchus involving bilateral arteries: A case report and literature review. Medicine (Baltimore). 2019;98:e17798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Sheth HS, Maldonado F, Lentz RJ. Two cases of Dieulafoy lesions of the bronchus with novel comorbid associations and endobronchial ablative management. Medicine (Baltimore). 2018;97:e9754. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | de Benito Sanz M, Cimavilla Román M, Torres Yuste R. A Dieulafoy's lesion in a duodenal diverticulum. An infrequent cause of UGIB. Rev Esp Enferm Dig. 2018;110:266-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Ko KH, Lee SY, Hong SP, Hwang SK, Park PW, Rim KS. Duodenal perforation after endoscopic hemoclip application for bleeding from Dieulafoy's lesion in a duodenal diverticulum. Gastrointest Endosc. 2005;62:781-2; discussion 782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 12. | Relea Pérez L, Magaz Martínez M, Pons Renedo F. Massive upper gastrointestinal bleeding due to a Dieulafoy's lesion inside a duodenal diverticulum. Rev Esp Enferm Dig. 2017;109:876-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 13. | Sadio A, Peixoto P, Castanheira A, Cancela E, Ministro P, Silva A, Caldas A. Dieulafoy's lesion in a duodenal diverticulum successfully treated with N-butyl-2-cyanoacrylate. Rev Esp Enferm Dig. 2010;102:396-398. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Chung IK, Kim EJ, Lee MS, Kim HS, Park SH, Lee MH, Kim SJ, Cho MS. Bleeding Dieulafoy's lesions and the choice of endoscopic method: comparing the hemostatic efficacy of mechanical and injection methods. Gastrointest Endosc. 2000;52:721-724. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 128] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Coelho-Prabhu N, Jain M, Velayos B S-Editor: Ma YJ L-Editor: Webster JR P-Editor: Zhang YL