Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.4917
Peer-review started: August 5, 2020
First decision: August 21, 2020
Revised: August 28, 2020
Accepted: September 10, 2020
Article in press: September 10, 2020
Published online: October 26, 2020
Processing time: 82 Days and 6.7 Hours
Woven coronary artery is an extremely rare disease with unknown etiology. This condition is difficult to diagnosis by traditional methods.
A 67-year-old male presented to the cardiology department with a history of mild chest pain for 6 mo. Coronary computed-tomography angiography revealed a soft plaque with a 40% stenosis in the right coronary artery (RCA). A linear shadow was seen both on left circumflex (LCX) and RCA. Further coronary angiography showed an 80% regional stenosis in the area proximal of LCX and RCA, and it was divided into different channels with diffuse stenosis. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) were performed in RCA. These confirmed a woven coronary artery. No stent was implanted. He remained asymptomatic during the 5-year follow-up period.
Woven coronary artery can be distinguished from spontaneous dissection and revascularization of thrombosis. IVUS and OCT are useful in obtaining a definite diagnosis, which decreases chances of unnecessary intervention.
Core Tip: Woven coronary artery can be distinguished from spontaneous dissection and revascularization of thrombosis. Intravascular ultrasound and optical coherence tomography are useful in obtaining a definite diagnosis, which decreases chances of unnecessary intervention.
- Citation: Wei W, Zhang Q, Gao LM. Woven coronary artery: A case report. World J Clin Cases 2020; 8(20): 4917-4921
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/4917.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.4917
Woven coronary artery (WCA) is a sporadic coronary disease, which is considered a benign condition[1], and most patients are asymptomatic. However, in some patients with WCA, sudden myocardial infarction or thrombosis may develop[2-4]. In addition, there have been reports of “woven-like” changes caused by revascularization thrombosis or spiral dissection[5-7], which are hard to distinguish by angiography. Currently, no long-time follow-up analysis of this disease is available. The pathology and etiology of woven coronary artery are elusive.
A 67-year-old male presented to the cardiology department with a 6 mo history of mild chest pain.
The patient had received coronary computed-tomography angiography, revealing that the left main artery (LM) was normal, and the right coronary artery (RCA) had a soft plaque with a 40% stenosis. A linear shadow was seen both on the left circumflex (LCX) and RCA, which was considered a spontaneous dissection.
The patient had a 30-year history of smoking and had no history of hypertension and diabetes.
No positive sign was found in the physical examination.
No abnormality was found in the laboratory examinations.
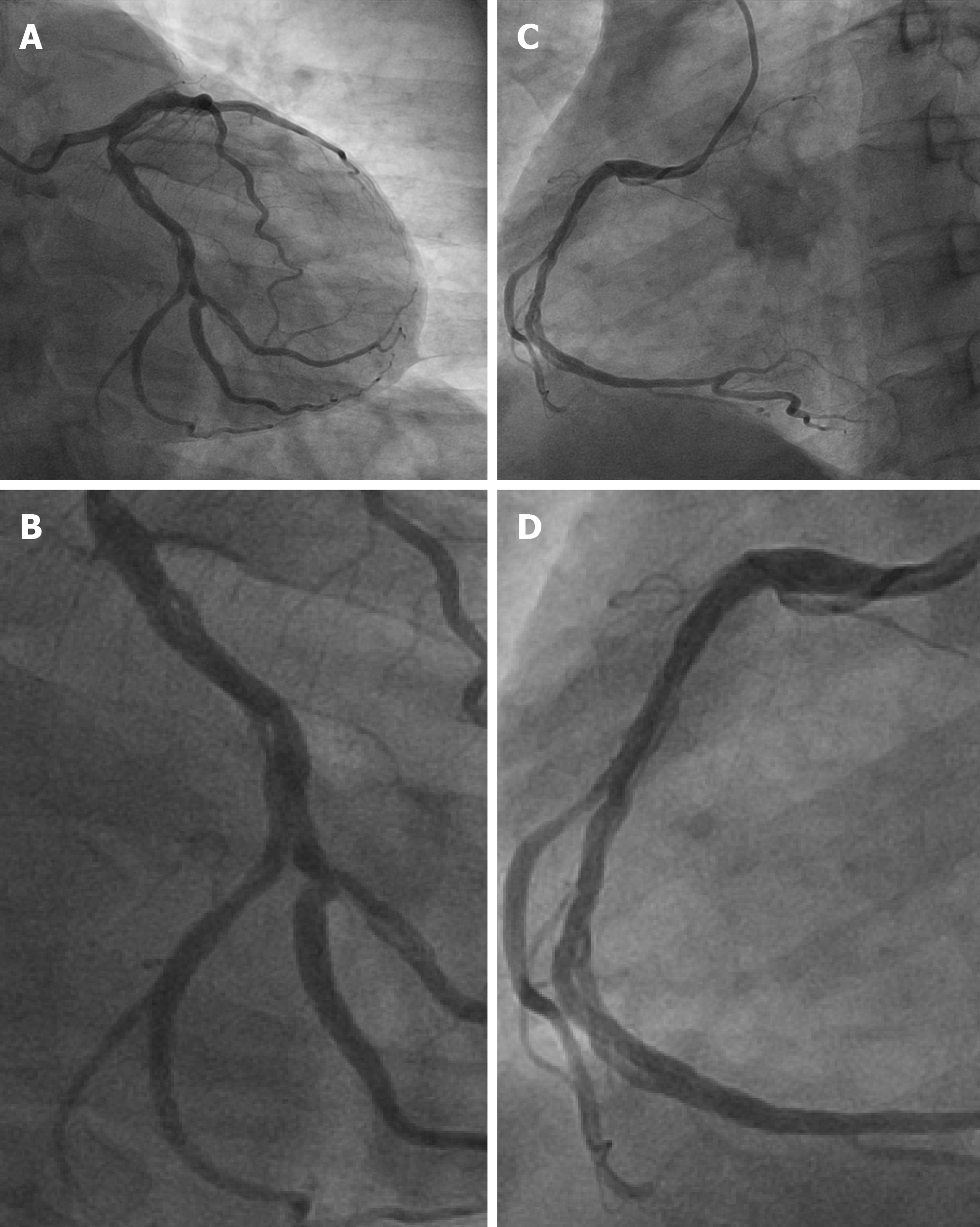
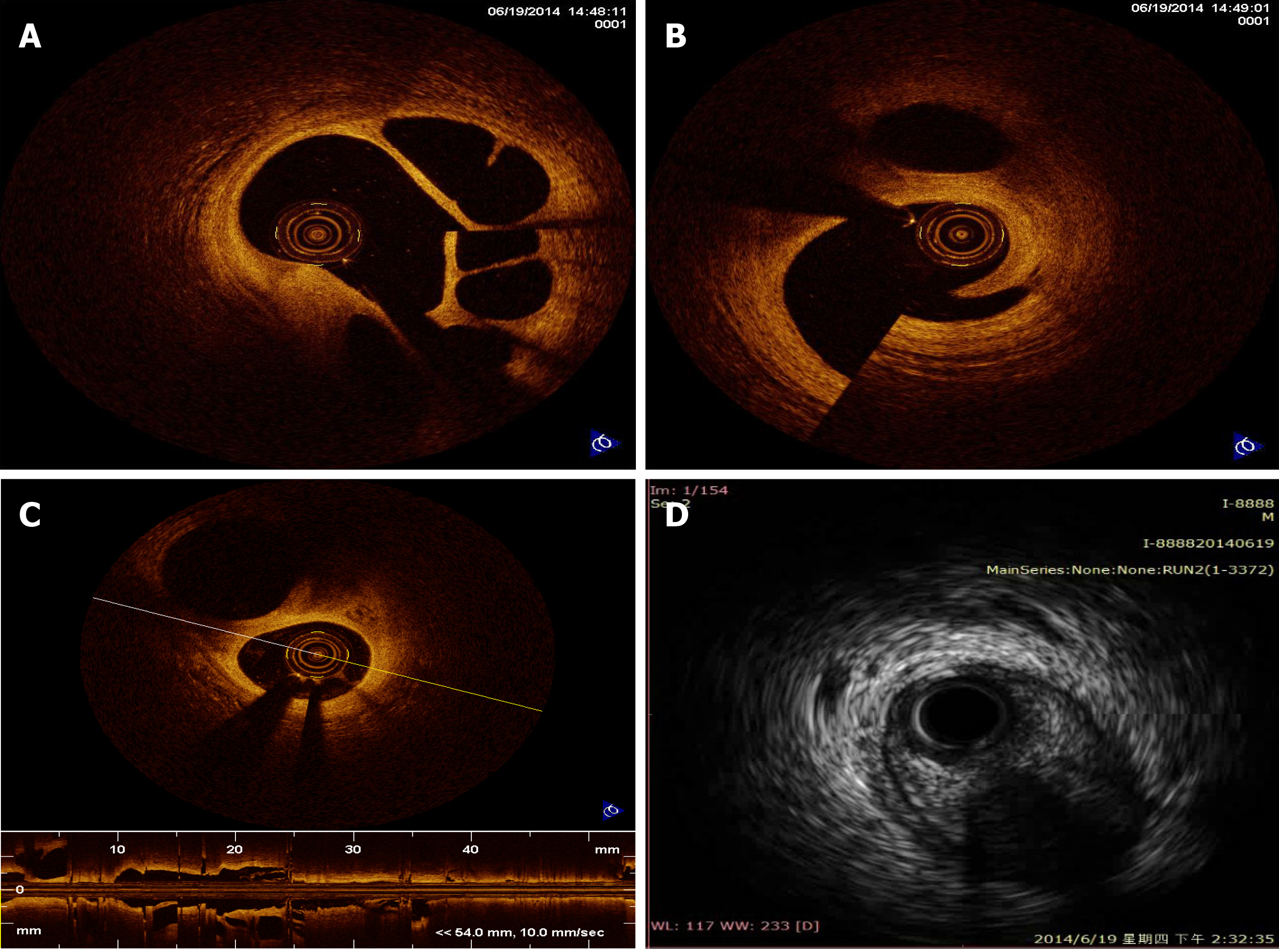
To clarify the lesions, a coronary angiography was performed. A 70% stenosis was found in the LM coronary artery, and a 30%-40% stenosis in the proximal left anterior descending. An 80% regional stenosis was found in the area proximal of LCX, which was divided into different channels with diffuse stenosis hard to describe. In addition, a diffuse and thin channel was seen in the whole RCA, with a 50% stenosis at the proximal part (Figure 1). The thrombosis in myocardial infarction (TIMI) grade was 3 in all the three vessels. Both intravascular ultrasound (IVUS) and optical coherence tomography (OCT) were performed in RCA (Figure 2). These were multiple twisted channels with intact intima, without any sign of thrombosis. All the channels were independent, shared the same tunica in the proximal segment, and merged into one lumen in the distal without abnormal flow.
These examinations revealed a WCA.
The tests suggested a benign condition that did not require further intervention. The patient was administered a single antiplatelet agent and statin before discharge from the hospital.
He was healthy and asymptomatic at the 12-mo follow-up and remained asymptomatic during the 5-year follow-up period. He continued with a single antiplatelet agent and statin for 5 years.
In 1988, Dr. Sane reported the first case of “8” sign in the right coronary artery angiography[7]. The vascular malformation looked woven, so the condition was named "woven coronary artery". Characteristically, the epicardial coronary artery is divided into multiple thin channels at the proximal segment and converged together in the distal segment, with a TIMI III distal blood flow. It was considered a benign coronary condition and a congenital anatomical anomaly. In some cases, WCA may cause acute coronary syndrome or sudden death when concomitant with atherosclerosis.
The etiology of WCA has remained unknown, but some researchers believe that it may arise from spontaneous coronary artery dissection[5]. However, it does not cause abnormal blood flow or nutrient supply or intramural hematoma. Other researchers have considered it a congenital vascular dysplasia. Previously, angiogenesis and arteriogenesis have been linked to the development of WCA. Other factors, such as slow flow, inflammation, and growth factors, are associated with the occurrence of WCA. Animal experiments confirmed that growth factors may promote the growth of coronary collateral vessels. It is also speculated that intrauterine inflammation might cause unbalanced development of the coronary artery, thereby leading to WCA.
A previous report stated that WCA can be diagnosed by coronary angiography. WCA most frequently involves the right coronary artery (54.5%), the left anterior descending artery (13.6%), and the left circumflex artery (9.1%), in that order[8]. Both left and right coronary arteries were involved in the current case. The average length of segments involved in WCA was 2.2 cm (range of 1.0-5.0). The WCA could be distinguished from spontaneous dissection and revascularization of thrombosis with or without intervention. These two conditions may show a similar pattern on angiography but have different prognosis following respective treatments. Thus, coronary angiography alone is not sufficient to make a definitive diagnosis. An intervascular image (such as IVUS and OCT) should be obtained to delineate the lumen and wall for a definite diagnosis. Here, OCT revealed multiple spiral tunnels separated by fibrous tissue in the local lumen[9]. In WCA, each tunnel contains a relatively complete three-layer vascular structure, which distinguishes WCA from thrombosis revascularization. The diagnostic features of IVUS were similar to those of OCT.
WCA is often considered a benign variant because of its normal blood flow. The lumen diameters of the true WCA between different tunnels are narrowed. If misdiagnosed as thrombus recanalization, a large coronary stent may be used, leading to vascular rupture. Therefore, clinical follow-up is recommended for WCA if there is no flow restriction. IVUS and OCT can be used to make a definite diagnosis and reduce unnecessary intervention. If stenosis or thrombosis are seen, coronary artery bypass grafting combined with medications may be safer than stent implantation based on intravascular imaging. It is unknown whether antiplatelet and statin drugs are effective in this case.
Although WCA appears to be benign without any major adverse cardiovascular events, more data and in-depth research are needed to understand this sporadic disease.
| 1. | Yildirim A, Oğuz D, Olguntürk R. Woven right and aneurysmatic left coronary artery associated with Kawasaki disease in a 9-month-old patient. Cardiol Young. 2010;20:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Uribarri A, Sanz-Ruiz R, Elízaga J, Fernández-Avilés F. Pathological insights of a woven coronary artery with optical coherence tomography. Eur Heart J. 2013;34:3005. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Val-Bernal JF, Malaxetxebarria S, González-Rodilla I, Salas-García M. Woven coronary artery anomaly presenting as sudden cardiac death. Cardiovasc Pathol. 2017;26:7-11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 4. | Pauwels R, Coeman M, De Beenhouwer T, Kayaert P. Woven coronary artery and myocardial infarction. Acta Cardiol. 2020;75:158-159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Akyuz A, Alpsoy S, Akkoyun DC. Spontaneous coronary artery dissection and woven coronary artery: three cases and a review of the literature. Korean Circ J. 2013;43:411-415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Sane DC, Vidaillet HJ Jr. "Woven" right coronary artery: a previously undescribed congenital anomaly. Am J Cardiol. 1988;61:1158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 32] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Wen W, Liu H, Li J, Zhang Q. Woven-like change following intracoronary thrombosis recanalization: a case report. BMC Cardiovasc Disord. 2019;19:317. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 8. | Yuan S. Woven coronary artery: a case report and literature review. Folia Morphol (Warsz). 2013;72:263-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG, Bouma B, Bruining N, Cho JM, Chowdhary S, Costa MA, de Silva R, Dijkstra J, Di Mario C, Dudek D, Falk E, Feldman MD, Fitzgerald P, Garcia-Garcia HM, Gonzalo N, Granada JF, Guagliumi G, Holm NR, Honda Y, Ikeno F, Kawasaki M, Kochman J, Koltowski L, Kubo T, Kume T, Kyono H, Lam CC, Lamouche G, Lee DP, Leon MB, Maehara A, Manfrini O, Mintz GS, Mizuno K, Morel MA, Nadkarni S, Okura H, Otake H, Pietrasik A, Prati F, Räber L, Radu MD, Rieber J, Riga M, Rollins A, Rosenberg M, Sirbu V, Serruys PW, Shimada K, Shinke T, Shite J, Siegel E, Sonoda S, Suter M, Takarada S, Tanaka A, Terashima M, Thim T, Uemura S, Ughi GJ, van Beusekom HM, van der Steen AF, van Es GA, van Soest G, Virmani R, Waxman S, Weissman NJ, Weisz G; International Working Group for Intravascular Optical Coherence Tomography (IWG-IVOCT). Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies: a report from the International Working Group for Intravascular Optical Coherence Tomography Standardization and Validation. J Am Coll Cardiol. 2012;59:1058-1072. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1221] [Cited by in RCA: 1483] [Article Influence: 105.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/Licenses/by-nc/4.0/
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent):
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Seto AH, Taguchi I, Tanaka A S-Editor: Yan JP L-Editor: Filipodia P-Editor: Xing YX