Published online Oct 26, 2020. doi: 10.12998/wjcc.v8.i20.4773
Peer-review started: April 23, 2020
First decision: April 29, 2020
Revised: August 16, 2020
Accepted: September 3, 2020
Article in press: September 3, 2020
Published online: October 26, 2020
Processing time: 186 Days and 2.6 Hours
Traumatic internal carotid artery dissection (TICAD) is rare and can result in severe neurological disability and even death. No consensus regarding its diagnostic screening and management has been established.
To investigate the clinical presentation, imaging features, diagnostic workup, and treatment of TICAD.
In this retrospective case series, emergency admissions for TICAD due to closed head injury were analyzed. The demographic, clinical, and radiographic data were retrieved from patient charts and the picture archiving and communication system.
Six patients (five males and one female, age range of 43-62 years, mean age of 52.67 years) presented with TICAD. Traffic accidents (4/6) were the most frequent cause of TICAD. The clinical presentation was always related to brain hypoperfusion. Imaging examination revealed dissection of the affected artery and corresponding brain infarction. All the patients were definitively diagnosed with TICAD. One patient was treated conservatively, one patient underwent anticoagulant therapy, two patients were given both antiplatelet and anticoagulant drugs, and two patients underwent decompressive craniectomy. One patient fully recovered, while three patients were disabled at follow-up. Two patients died of refractory brain infarction.
TICAD can cause catastrophic outcomes and even refractory brain hernia. Early and efficient diagnosis of TICAD is essential for initiating appropriate treatment. The treatment of TICAD is challenging and variable and is based on clinician discretion on a case-by-case basis.
Core Tip: Traumatic internal carotid artery dissection is a rare and acute condition. Early diagnosis and intervention can improve the prognosis and quality of life of patients. Case presentations and a literature review may provide insight into the pathology, clinical manifestations, imaging features, diagnosis, and treatment.
- Citation: Wang GM, Xue H, Guo ZJ, Yu JL. Cerebral infarct secondary to traumatic internal carotid artery dissection. World J Clin Cases 2020; 8(20): 4773-4784
- URL: https://www.wjgnet.com/2307-8960/full/v8/i20/4773.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i20.4773
Traumatic internal carotid artery dissection (TICAD) at an extracranial or intracranial location is rare but can result in severe neurological disability or death and is often secondary to motor vehicle accidents, sports accidents, amusement park activities, and cervical chiropractic manipulation[1-5]. The morbidity rate associated with TICAD ranges from 23%-28%, and 48%-58% of survivors have significant neurological complications[6,7].
However, only 6% of blunt TICAD cases are diagnosed at the time of initial presentation and medical evaluation[8]. Therefore, screening of asymptomatic TICAD patients after traumatic accidents is recommended as timely recognition and appropriate treatment are vital to avoid fatal brain infarction[9,10].
Currently, the diagnosis and treatment of TICAD are incompletely understood. As TICAD is uncommon, studies of this entity are limited to case reports, and few studies have depicted the clinical and radiologic course of TICAD. In the present study, we describe six patients who were diagnosed with TICAD and provide a literature review of TICAD.
All patients included in the study sustained different types of traumatic injury and were confirmed to have TICAD at the First Hospital of Jilin University between July 2013 and April 2018. The study protocol was approved by the Institutional Review Board of the First Hospital of Jilin University. Informed consent for publication of these cases was obtained from the patients or their relatives.
Data were retrospectively collected from the patients’ medical files, treatment reports, and follow-up notes. The Glasgow Coma Scale was used to evaluate the patients’ neurologic status[11]. The patients’ age, sex, symptoms, and onset time after injury were recorded, and their imaging data were obtained.
Follow-up was performed based on a clinical consultation or telephone interview. The Glasgow Outcome Scale (GOS) was used to assess prognosis, where GOS 1 indicated death, 2 indicated a persistent vegetative state, 3 indicated severe disability, 4 indicated moderate disability, and 5 indicated a good recovery[12].
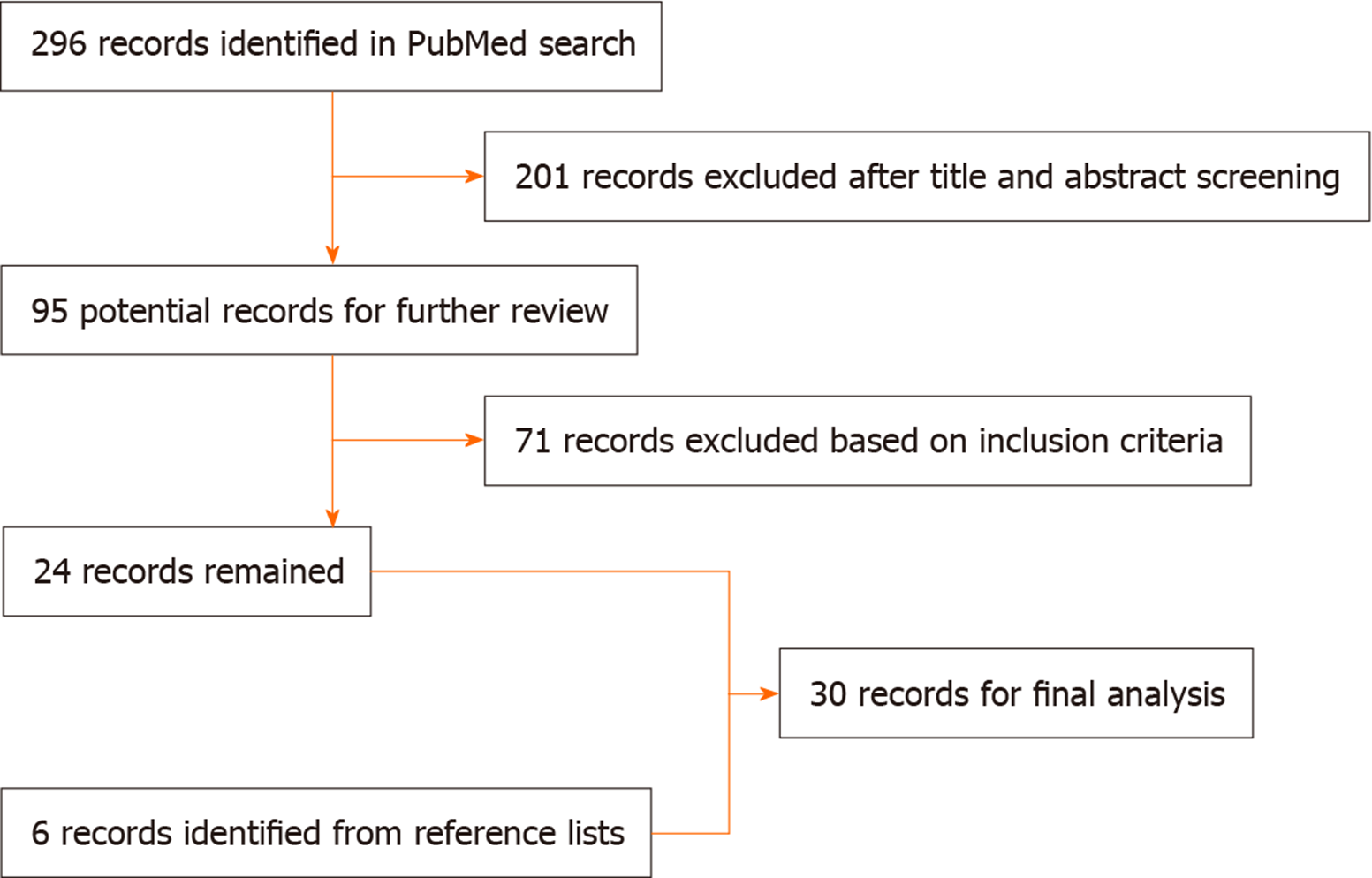
Eligible English-language articles (case reports, case series, and studies investigating TICAD) were identified by searching PubMed publications (the last search date was April 2020). The search algorithm used the terms “Traumatic internal carotid artery dissection” as the key word. The reference lists of the identified articles were also manually searched for additional studies. The resulting flowchart is depicted in Figure 1.
The inclusion criteria were as follows: (1) The full text was available; (2) Clinical data were complete; and (3) All the cases in the articles were TICAD cases. Studies without sufficient descriptions of TICAD were excluded. After a review of the obtained literature, the current status of TICAD was discussed in terms of clinical features, radiological features, treatment, and prognosis.
Six patients with closed head injuries were enrolled in the current study. Of these 6 patients (5 males and 1 female, age range of 43-62 years, mean age of 52.67 years), four were involved in traffic accidents, including car accidents (n = 2) and motorcycle accidents (n = 2), one patient fell from a height, and one patient suffered an amusement park injury.
The six patients had no symptoms immediately after the traumatic incidents; the interval from injury to symptom onset was 4-45 h, and the mean interval was 15 h. The initial symptoms included paralysis (n = 2), disturbance of consciousness (drowsiness or confusion) (n = 2), headache (n = 1), and neck pain (n = 1). Four patients had a Glasgow Coma Scale score of 15, and two patients had scores of 14 and 13.
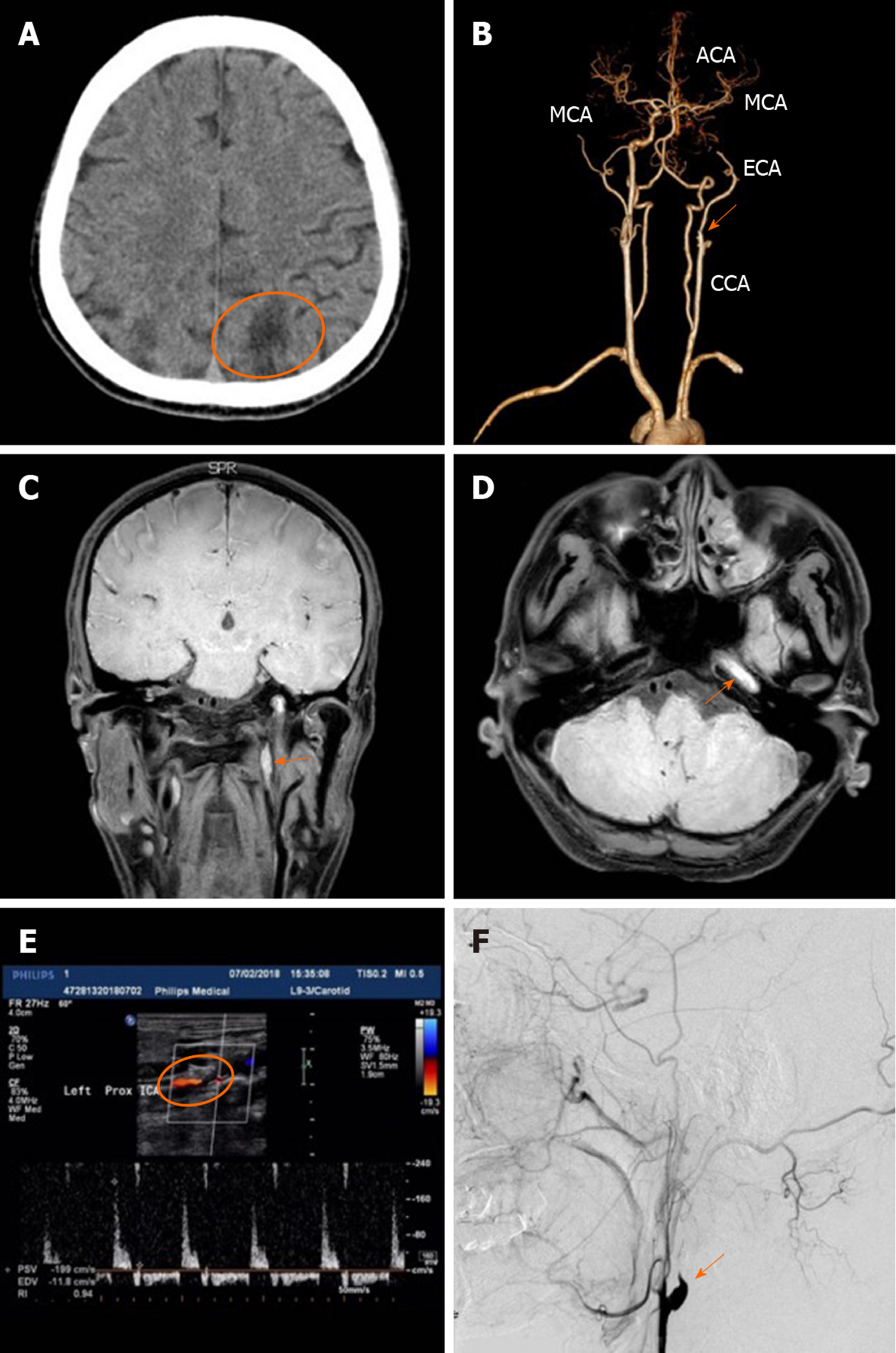
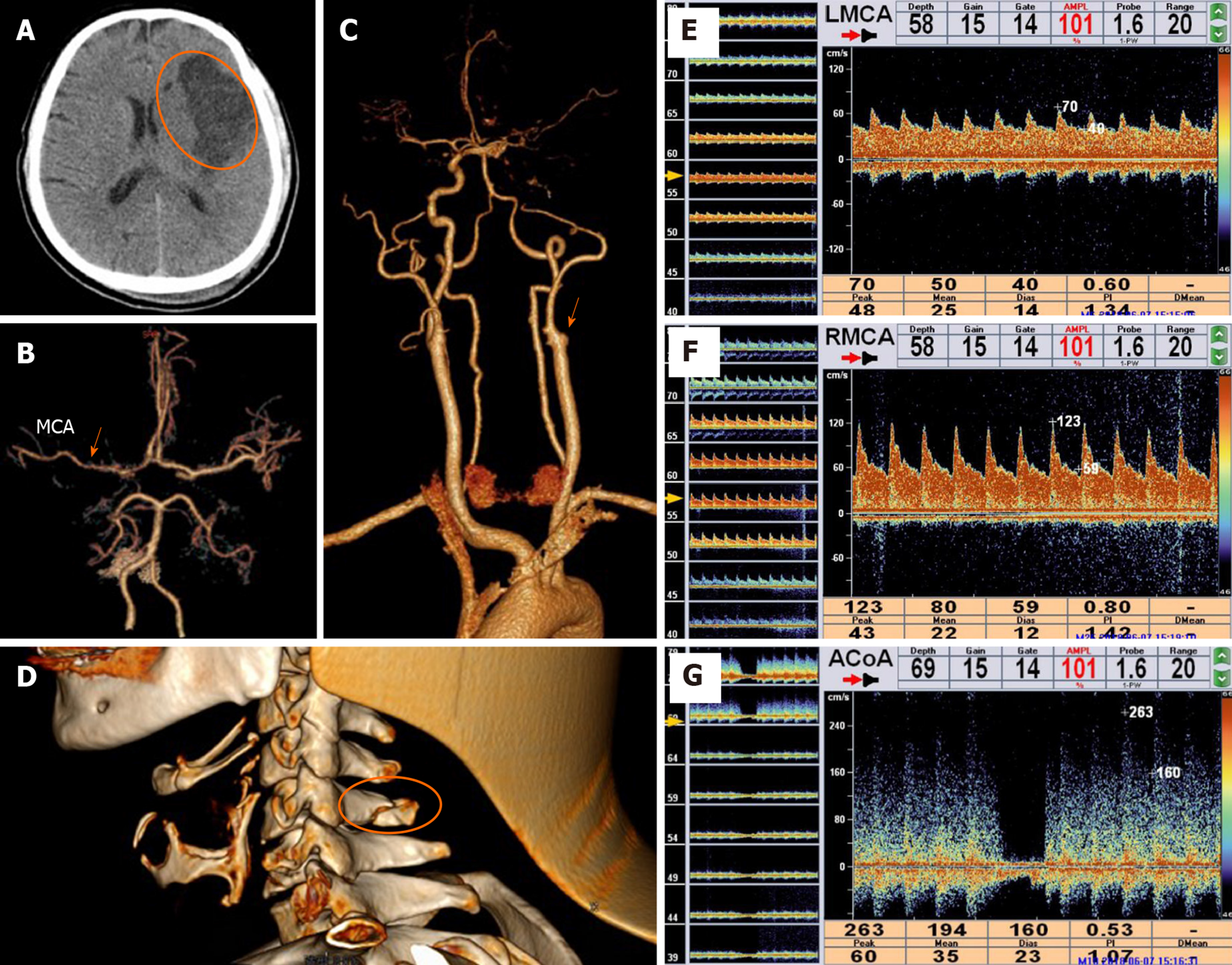
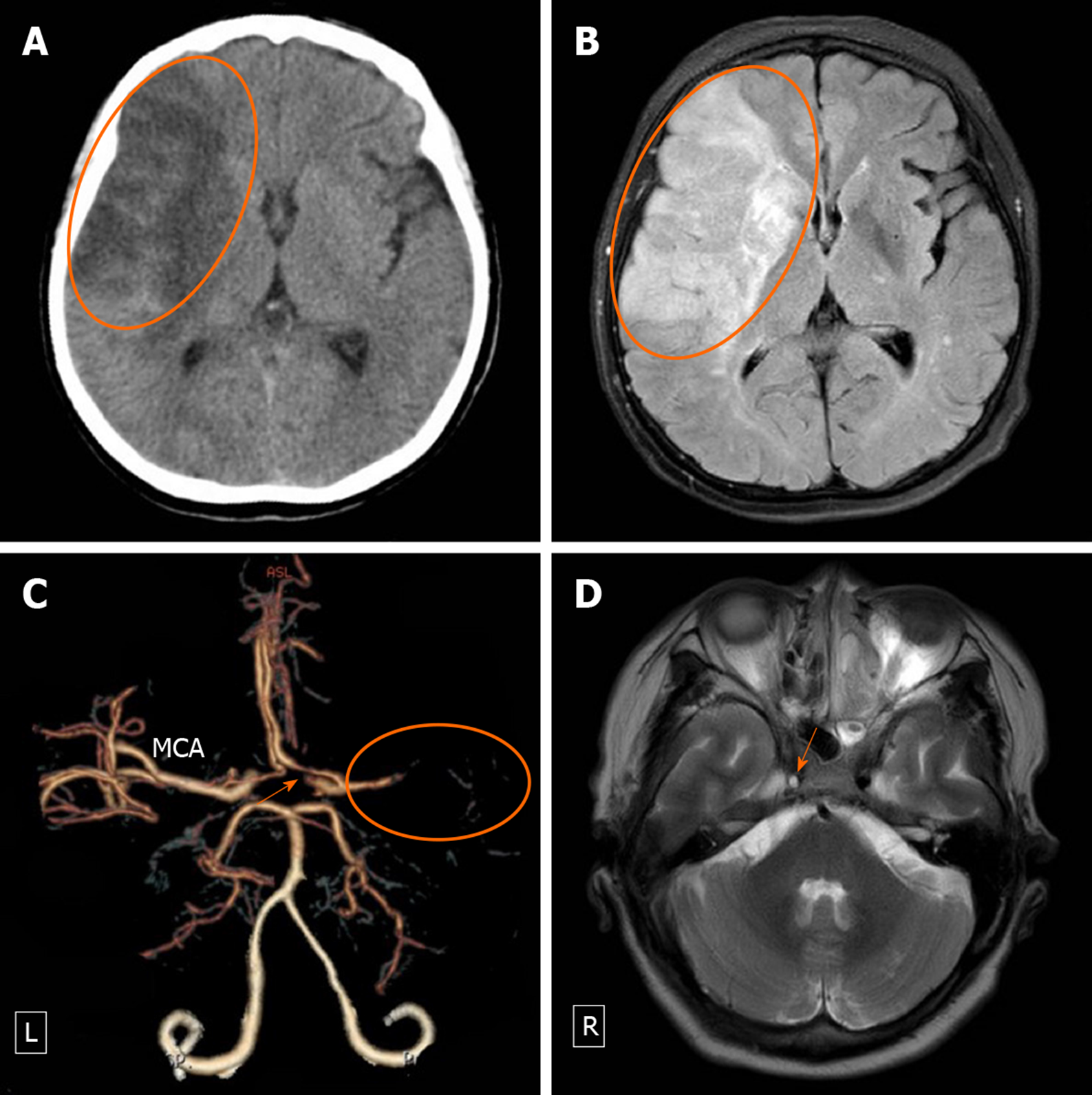
Computed tomography (CT), CT angiography (CTA), duplex ultrasonography (DU), digital subtraction angiography (DSA), magnetic resonance imaging (MRI), and transcranial doppler (TCD) were selectively performed in these six patients, which revealed TICAD, cerebral infarction, and insufficient intracranial blood flow. CT and CTA were performed in three cases. CT, CTA, and MRI were performed in one case. CT, CTA, MRI, DU, and DSA were performed in one case. CT, CTA, MRI, DU, and TCD were performed in one case.
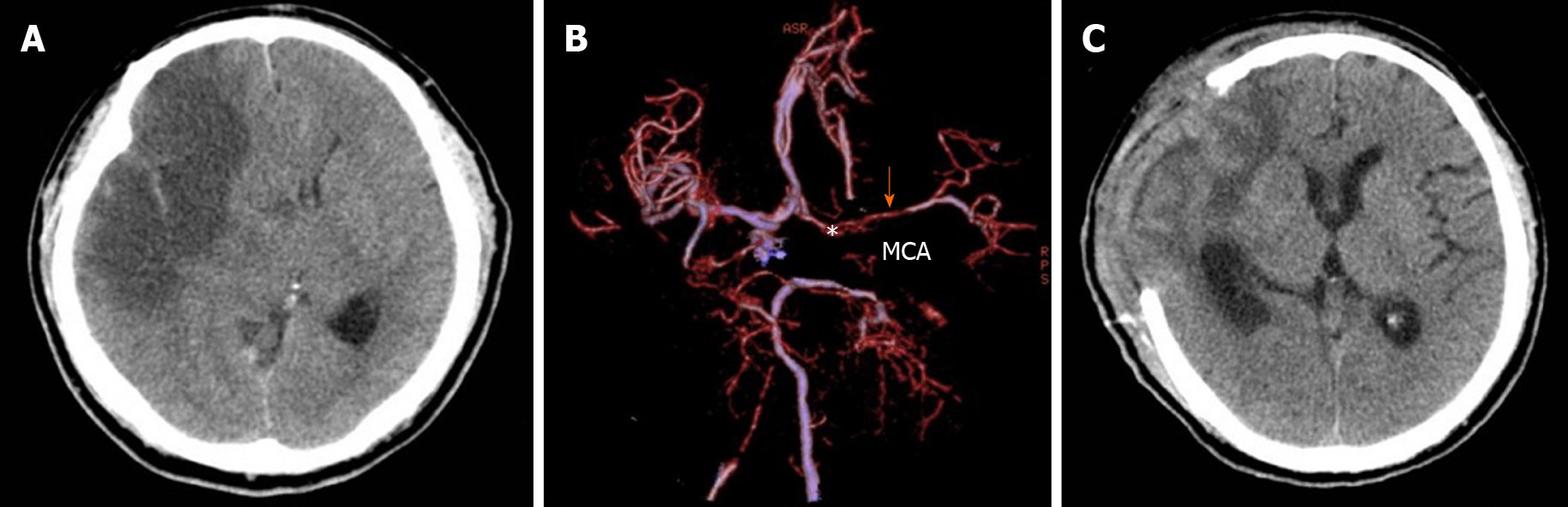
In all six patients, CT demonstrated varying degrees of cerebral infarction. A hyperdense middle cerebral artery (MCA) sign on CT was visible in one CT scan. CTA, DU, DSA, and MRI revealed an intimal flap (n = 2), tapering stenosis (n = 5), and the appearance of an intramural hematoma (n = 2).
In case 1, CTA and DSA clearly showed a rat tail sign at the beginning of the right internal carotid artery (ICA) (Figure 2B-F), and DU revealed that the true ICA lumen opened and shunted in synchrony with the vessel’s pulse (i.e. the “open and close sign”) (Figure 2E). MRI demonstrated a continuous crescentic high signal in the right ICA and an elongated, round high signal in the right MCA (Figure 2C and D), indicating the probable diagnosis of subacute dissection extending from the origin of the right ICA to the intracranial artery. Regarding case 2, a hyperdense MCA sign may be a predictor of rapidly progressive malignant lethal cerebral infarction. A later CT scan detected cerebral infarction (Figure 3B) and brain contusion (Figure 3A). Concomitant polytraumatic injuries (such as mandibular fracture) were also observed (Figure 3D). In cases 1 and 3, the left ICA was completely occluded (Figures 2B-F and Figure 4C), but the patients did not experience catastrophic cerebral infarction. CTA (Figures 2B and Figure 4B) and TCD (Figure 4E) indicated the presence of blood supply in the left MCA. The carotid compression test revealed the openness of the anterior communicating artery (Figure 4G), and in case 3, a cervical vertebra fracture was also revealed (Figure 4C). In case 5, MRI showed right ICA dissection manifested as a partial flow-void lumen surrounded by high-intensity signals due to an intramural hematoma (Figure 5D). In case 6, the patient exhibited deteriorating levels of consciousness, and decompressive craniectomy was performed to relieve the refractory high intracranial pressure (Figure 6).
Five of the six patients sustained polytraumatic injuries, including clavicular fracture (n = 1), brain contusion and mandibular fracture (n = 1), skull base fracture and C6 fracture (n = 1), and skull base fracture (n = 2).
The final diagnosis in the six cases was TICAD.
One patient underwent anticoagulant therapy. Two patients were given both antiplatelet and anticoagulant drugs. Decompressive craniectomy was performed as a last-resort procedure to manage efficiently refractory brain infarction in two patients. One patient underwent conservative treatment (without antiplatelet or/and anticoagulant drugs or surgery).
During hospitalization, two patients died of refractory brain infarction. Outpatient follow-up (range: 1-4 years) was performed in the four surviving patients. Neurological function examinations were carried out using the GOS. The results were as follows: One patient fully recovered and had a score of 5, and three patients were disabled (one patient had a score of 4, and two patients had a score of 3). The clinical data are summarized in Table 1.
| No. | Sex/age | Cause of trauma | Asymptomatic period in h | Initial syndrome | GCS | Associated polytrauma | Imaging | Treatment | Follow-up in yr | GOS |
| 1 | M/51 | Car crash | 4 | Confusion | 13 | Skull base fracture | CT, CTA, MRI, DU and DSA | Anticoagulant | 3 | 5 |
| 2 | M/52 | Motorcycle crash | 6 | Drowsiness | 14 | Brain contusion and mandibular fracture | CT and CTA | Conservative treatment | NA | 1 |
| 3 | M/62 | Car crash | 45 | Neck pain | 15 | Skull base fracture and C6 fracture | CT, CTA, MRI, DU and TCD | Anticoagulant and antiplatelet | 4 | 4 |
| 4 | M/43 | Motorcycle crash | 10 | Paralysis | 15 | Clavicular fracture | CT and CTA | DC | NA | 1 |
| 5 | F/61 | Amusement park accident | 12 | Paralysis | 15 | None | CT, CTA and MRI | Anticoagulant and antiplatelet | 3 | 3 |
| 6 | M/47 | Fall from height | 13 | Headache | 15 | Skull base fracture | CT and CTA | DC | 1 | 3 |
TICADs are markedly different from spontaneous dissections or dissections occurring in everyday life (cough, nose blowing, rapid head turning, or rapid neck extension)[13-15]. TICAD frequently occurs when high-speed traumatic cerebrovascular injuries are sustained, such as those sustained in motor vehicle crashes, car crashes, assaults, falls, or amusement park activities or when hanging[16-18]. The overall mortality rate associated with TICAD ranges from approximately 20%-40%[19,20]. In our case series, the mortality rate was 33.3% (2/6), and these two patients died of refractory brain infarction.
In most TICAD cases, the pathological background is disruption of the intima, which causes luminal narrowing or even occlusion due to collapse of the false lumen against the true lumen and interferes with the blood flow in the primary lumen[13,21]. If dissection occurs between the media and adventitia, complete or partial transection can also occur, leading to flow-related pseudoaneurysm pouch formation[22,23].
Patients with TICAD present with a variety of symptoms and signs ranging from mild symptoms, such as headache, neck pain, or cranial nerve palsy, to more serious symptoms, such as stroke and even high intracranial pressure[1]. Usually, a latent period exists between the time of injury and symptom onset, which can complicate the diagnosis[24]. The average time for stroke to develop is 12-75 h post-trauma[3,5,25]. In our six cases, the asymptomatic period ranged from 4-45 h (average 15 h), which is similar to a previous report.
One of the main goals in the management of this condition is to establish an accurate diagnosis before stroke occurs[26]. Many studies have reported a correlation between TICAD and traumatic injury near the neck, especially with cervical and facial fractures[2,27,28]. The main risk factors for TICAD after severe traumatic brain injury are fracture involving the carotid canal, cervical spine injury, and thoracic trauma[16,29-31]. A recent study found that 42% of patients with polytrauma including TICAD had cervical spine fractures[16,32]. In our case series, 5/6 (83.33%) patients had multiple injuries near the ICA.
The diagnosis of TICAD is based mainly on neuroimaging findings. When TICAD occurs, the purpose of imaging examinations is to detect the cerebral parenchyma and the corresponding supply artery. The cerebral parenchyma can easily be visualized when performing CT or MRI[33]. TICAD may be detected by conventional DSA, DU, CTA, MRI, and magnetic resonance angiography[14,34,35]. In these imaging examinations, the characteristics of TICAD may include an intimal flap, a double lumen, tapering stenosis, tandem occlusions, the appearance of an intramural hematoma, and sometimes a small pseudoaneurysm[36]. TCD can also sometimes reveal a low blood flow velocity in the affected artery[4]. Early CT scans often do not show significant abnormalities, but high-density images of the MCA may occasionally be viewed if thrombosis of the MCA occurs[37].
TICAD must be treated as cerebral infarction can occur several hours after traumatic injury, when most patients are outside the narrow therapeutic window for timely therapy. However, considering the complexity and difficulty of the diagnosis of TICAD, in certain circumstances, the major goals of treatment are to prevent thromboembolic and hemodynamic injury[25,38]. Thus, when TICAD is suspected, antiplatelet and anticoagulant agents are required. However, medical management may be contraindicated in some cases, such as in case 2 in our study in which the CT scan revealed brain contusion. Furthermore, to avoid an increased risk of intracranial hemorrhage, we did not use any medical therapy. As recently described, stenting of the carotid arteries by an endovascular approach may provide immediate revascularization and can improve perfusion and limit embolus formation in patients presenting with embolic or hemodynamic symptoms[38]. However, in our study, the definitive diagnosis was determined too late for our six patients to be treated with vascular recanalization.
The prognosis of patients depends mainly on stenosis of the lumen and thrombosis of the dissected artery. Notably, in our six cases, we found that the degree of opening and compensation of the collateral circulation, such as the anterior and posterior communicating arteries, is very important for the blood supply to the brain on the injured side. Therefore, we hypothesize in some cases that the clinical presentation and prognosis of TICAD may be determined by the opening of the collateral circulation.
We are aware of some limitations in our study (e.g., the small sample size and lack of follow-up imaging), but the various imaging techniques used revealed this traumatic arterial injury. A larger prospective randomized multicenter clinical study is required to increase the statistical power.
TICAD is referred to as arterial dissection caused by an ICA intimal tear after trauma, and thromboembolism and hypoperfusion constitute the main pathology. TICAD can result in catastrophic outcomes. When the occurrence of dissection is suspected, detailed examinations should be carried out. Early and efficient diagnosis of TICAD is essential for initiating appropriate treatment. The treatment of TICAD is challenging and is always based on clinician discretion on a case-by-case basis.
The extracranial internal carotid artery refers to the anatomic location that reaches from the common carotid artery proximally to the skull base distally and is at considerable risk for injury. No consensus regarding its diagnostic screening and management has been established. The present study compared the outcomes of six different patients who suffered traumatic internal carotid artery dissection (TICAD).
Despite a high incidence, reports of TICAD are limited to case reports or small case series. Currently, the frequency, cause, imaging changes, and influence on mortality of TICAD are not well defined. We therefore decided to conduct a retrospective study of TICAD at a tertiary medical center. The risk factors of infarction, pathophysiology, clinical and radiological features, diagnosis, treatment, and prognosis were analyzed and delineated for TICAD.
We performed a retrospective analysis and literature review of patients who were diagnosed as TICAD.
In this retrospective case series, emergency admissions for TICAD due to closed head injury were analyzed. The demographic, clinical, and radiographic data were retrieved from patient charts and the picture archiving and communication system, and a literature review of TICAD was also performed.
Six patients presented with TICAD. Traffic accidents (4/6) were the most frequent cause of TICAD. The clinical presentation was always related to brain hypoperfusion. Imaging examination revealed dissection of the affected artery and corresponding brain infarction. All the patients were definitively diagnosed with TICAD. One patient was treated conservatively, one patient underwent anticoagulant therapy, two patients were given both antiplatelet and anticoagulant drugs, and two patients underwent decompressive craniectomy. One patient fully recovered, while three patients were disabled at follow-up. Two patients died of refractory brain infarction.
We found that TICAD should be identified in patients presenting after blunt trauma, including classical dissection, pseudoaneurysm, and stenosis/occlusion.
Early diagnosis and intervention can improve the prognosis and quality of life of patients who suffered TICAD. Based on the results of this study, future research should include prospective randomized control trial with a larger patient population so that we can better understand the diagnosis and treatment of TICAD.
| 1. | Bouzat P, Francony G, Brun J, Lavagne P, Picard J, Broux C, Declety P, Jacquot C, Albaladejo P, Payen JF. Detecting traumatic internal carotid artery dissection using transcranial Doppler in head-injured patients. Intensive Care Med. 2010;36:1514-1520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 2. | Tveita IA, Madsen MRS, Nielsen EW. Dissection of the internal carotid artery and stroke after mandibular fractures: a case report and review of the literature. J Med Case Rep. 2017;11:148. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Kowalski RG, Haarbauer-Krupa JK, Bell JM, Corrigan JD, Hammond FM, Torbey MT, Hofmann MC, Dams-O'Connor K, Miller AC, Whiteneck GG. Acute Ischemic Stroke After Moderate to Severe Traumatic Brain Injury: Incidence and Impact on Outcome. Stroke. 2017;48:1802-1809. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 67] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 4. | Zhou W, Huynh TT, Kougias P, El Sayed HF, Lin PH. Traumatic carotid artery dissection caused by bungee jumping. J Vasc Surg. 2007;46:1044-1046. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Benedict WJ, Prabhu V, Viola M, Biller J. Carotid artery pseudoaneurysm resulting from an injury to the neck by a fouled baseball. J Neurol Sci. 2007;256:94-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Bajkó Z, Maier S, Moţăţăianu A, Bălaşa R, Vasiu S, Stoian A, Andone S. Stroke Secondary to Traumatic Carotid Artery Injury - A Case Report. J Crit Care Med (Targu Mures). 2018;4:23-28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 7. | Miller PR, Fabian TC, Croce MA, Cagiannos C, Williams JS, Vang M, Qaisi WG, Felker RE, Timmons SD. Prospective screening for blunt cerebrovascular injuries: analysis of diagnostic modalities and outcomes. Ann Surg. 2002;236:386-93; discussion 393. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 385] [Cited by in RCA: 355] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 8. | Krajewski LP, Hertzer NR. Blunt carotid artery trauma: report of two cases and review of the literature. Ann Surg. 1980;191:341-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 137] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 9. | Löhrer L, Vieth V, Nassenstein I, Hartensuer R, Niederstadt T, Raschke MJ, Vordemvenne T. Blunt cerebrovascular injuries in acute trauma care: a screening protocol. Eur Spine J. 2012;21:837-843. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Furtner M, Werner P, Felber S, Schmidauer C. Bilateral carotid artery dissection caused by springboard diving. Clin J Sport Med. 2006;16:76-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Teasdale G, Maas A, Lecky F, Manley G, Stocchetti N, Murray G. The Glasgow Coma Scale at 40 years: standing the test of time. Lancet Neurol. 2014;13:844-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 435] [Cited by in RCA: 668] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 12. | McMillan T, Wilson L, Ponsford J, Levin H, Teasdale G, Bond M. The Glasgow Outcome Scale - 40 years of application and refinement. Nat Rev Neurol. 2016;12:477-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 281] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 13. | Foreman PM, Harrigan MR. Blunt Traumatic Extracranial Cerebrovascular Injury and Ischemic Stroke. Cerebrovasc Dis Extra. 2017;7:72-83. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 37] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Ben Hassen W, Machet A, Edjlali-Goujon M, Legrand L, Ladoux A, Mellerio C, Bodiguel E, Gobin-Metteil MP, Trystram D, Rodriguez-Regent C, Mas JL, Plat M, Oppenheim C, Meder JF, Naggara O. Imaging of cervical artery dissection. Diagn Interv Imaging. 2014;95:1151-1161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 15. | Shindo T, Ito M, Matsumoto J, Miki K, Fujihara F, Terasaka S, Isu T, Isobe M. A Case of Juvenile Stroke due to Carotid Artery Dissection from an Elongated Styloid Process-Revisiting Conservative Management. J Stroke Cerebrovasc Dis. 2019;28:104307. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 16. | Sporns PB, Niederstadt T, Heindel W, Raschke MJ, Hartensuer R, Dittrich R, Hanning U. Imaging of Spontaneous and Traumatic Cervical Artery Dissection : Comparison of Typical CT Angiographic Features. Clin Neuroradiol. 2019;29:269-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 17. | Dandamudi VS, Thaler DE, Malek AM. Cerebral embolus following chiropractic manipulation in a patient with a calcified carotid artery. J Neuroimaging. 2013;23:429-430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Vadikolias K, Heliopoulos J, Serdari A, Vadikolia CM, Piperidou C. Flapping of the dissected intima in a case of traumatic carotid artery dissection in a jackhammer worker. J Clin Ultrasound. 2009;37:221-222. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 19. | Engelter ST, Lyrer PA, Kirsch EC, Steck AJ. Long-term follow-up after extracranial internal carotid artery dissection. Eur Neurol. 2000;44:199-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 20. | Giossi A, Ritelli M, Costa P, Morotti A, Poli L, Del Zotto E, Volonghi I, Chiarelli N, Gamba M, Bovi P, Tomelleri G, Carletti M, Checcarelli N, Meneghetti G, Morra M, Chinaglia M, De Giuli V, Colombi M, Padovani A, Pezzini A. Connective tissue anomalies in patients with spontaneous cervical artery dissection. Neurology. 2014;83:2032-2037. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 21. | Ramchand P, Mullen MT, Bress A, Hurst R, Kasner SE, Cucchiara BL, Messé SR. Recanalization after Extracranial Dissection: Effect of Antiplatelet Compared with Anticoagulant Therapy. J Stroke Cerebrovasc Dis. 2018;27:438-444. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Delgado F, Bravo-Rodríguez FA, Bautista MD, Chirosa MA, Molina T, Martos JM, Canis M. Carotid pseudoaneurysms secondary to dissection: endovascular management with bare stent-graft. Cerebrovasc Dis. 2005;19:136-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 23. | Griessenauer CJ, Foreman PM, Deveikis JP, Harrigan MR. Optical coherence tomography of traumatic aneurysms of the internal carotid artery: report of 2 cases. J Neurosurg. 2016;124:305-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Robertson JJ, Koyfman A. Extracranial Cervical Artery Dissections. Emerg Med Clin North Am. 2017;35:727-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 25. | Cohen JE, Ben-Hur T, Rajz G, Umansky F, Gomori JM. Endovascular stent-assisted angioplasty in the management of traumatic internal carotid artery dissections. Stroke. 2005;36:e45-e47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 51] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 26. | Cohen JE, Gomori JM, Itshayek E, Spektor S, Shoshan Y, Rosenthal G, Moscovici S. Single-center experience on endovascular reconstruction of traumatic internal carotid artery dissections. J Trauma Acute Care Surg. 2012;72:216-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 33] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Davis JW, Holbrook TL, Hoyt DB, Mackersie RC, Field TO Jr, Shackford SR. Blunt carotid artery dissection: incidence, associated injuries, screening, and treatment. J Trauma. 1990;30:1514-1517. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 219] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 28. | Misra S, Haas CA, August M, Eberlin KR. Delayed Carotid Dissection Following Lower Lip Revascularization in the Setting of Hyoid Fracture--A Case Report and Review of the Literature. J Oral Maxillofac Surg. 2016;74:123-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 29. | Jacobson LE, Ziemba-Davis M, Herrera AJ. The limitations of using risk factors to screen for blunt cerebrovascular injuries: the harder you look, the more you find. World J Emerg Surg. 2015;10:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 36] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 30. | Berne JD, Cook A, Rowe SA, Norwood SH. A multivariate logistic regression analysis of risk factors for blunt cerebrovascular injury. J Vasc Surg. 2010;51:57-64. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 75] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 31. | Esnault P, Cardinale M, Boret H, D'Aranda E, Montcriol A, Bordes J, Prunet B, Joubert C, Dagain A, Goutorbe P, Kaiser E, Meaudre E. Blunt cerebrovascular injuries in severe traumatic brain injury: incidence, risk factors, and evolution. J Neurosurg. 2017;127:16-22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 72] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 32. | Delgado Almandoz JE, Schaefer PW, Kelly HR, Lev MH, Gonzalez RG, Romero JM. Multidetector CT angiography in the evaluation of acute blunt head and neck trauma: a proposed acute craniocervical trauma scoring system. Radiology. 2010;254:236-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 33. | Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668-678. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 530] [Article Influence: 31.2] [Reference Citation Analysis (0)] |
| 34. | Vertinsky AT, Schwartz NE, Fischbein NJ, Rosenberg J, Albers GW, Zaharchuk G. Comparison of multidetector CT angiography and MR imaging of cervical artery dissection. AJNR Am J Neuroradiol. 2008;29:1753-1760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 203] [Cited by in RCA: 191] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 35. | Crönlein M, Sandmann GH, Beirer M, Wunderlich S, Biberthaler P, Huber-Wagner S. Traumatic bilateral carotid artery dissection following severe blunt trauma: a case report on the difficulties in diagnosis and therapy of an often overlooked life-threatening injury. Eur J Med Res. 2015;20:62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 36. | Bajkó Z, Bălaşa R, Moţăţăianu A, Bărcuţean L, Stoian A, Stirbu N, Maier S. Malignant Middle Cerebral Artery Infarction Secondary to Traumatic Bilateral Internal Carotid Artery Dissection. A Case Report. J Crit Care Med (Targu Mures). 2016;2:135-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 37. | Kurre W, Bansemir K, Aguilar Pérez M, Martinez Moreno R, Schmid E, Bäzner H, Henkes H. Endovascular treatment of acute internal carotid artery dissections: technical considerations, clinical and angiographic outcome. Neuroradiology. 2016;58:1167-1179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 27] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 38. | Daou B, Hammer C, Mouchtouris N, Starke RM, Koduri S, Yang S, Jabbour P, Rosenwasser R, Tjoumakaris S. Anticoagulation vs Antiplatelet Treatment in Patients with Carotid and Vertebral Artery Dissection: A Study of 370 Patients and Literature Review. Neurosurgery. 2017;80:368-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 54] [Article Influence: 6.0] [Reference Citation Analysis (1)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Figueiredo EG, Kawabata H S-Editor: Zhang L L-Editor: Filipodia P-Editor: Liu JH