Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.410
Peer-review started: October 17, 2019
First decision: December 4, 2019
Revised: December 4, 2019
Accepted: December 22, 2019
Article in press: December 22, 2019
Published online: January 26, 2020
Processing time: 91 Days and 11.8 Hours
The eye is a rare site for lung cancer metastasis. Indeed, ocular metastasis is one of the greatest challenges to quality of life in a cancer patient. Here we present a patient with lung adenocarcinoma and ocular metastasis.
The patient was a 70-year-old man diagnosed with lung adenocarcinoma who developed eye metastasis mimicking anterior scleritis. Brain magnetic resonance imaging showed an abnormal signal in the right eye. Based on next generation sequencing of the surgical specimen, the patient was shown to have a KRAS point mutation (p.G12D).
Multidiscipline expertise collaboration is needed to make the early diagnosis and determine the prompt treatment in patients. We hope to increase the awareness of the possibility of lung cancer metastasizing to the eye.
Core tip: The eye is a rare site for lung cancer metastasis. We report the case of a patient with lung adenocarcinoma and ocular metastasis. Brain magnetic resonance imaging showed an abnormal signal in the right eye. Based on next generation sequencing of the surgical specimen, the patient was shown to have a KRAS point mutation (p.G12D). The clinical feature and treatment of the disease are presented and discussed.
- Citation: Chen HF, Wang WX, Li XF, Wu LX, Zhu YC, Du KQ, Xu CW. Eye metastasis in lung adenocarcinoma mimicking anterior scleritis: A case report. World J Clin Cases 2020; 8(2): 410-414
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.410
Non-small cell lung cancer (NSCLC) is the leading cause of cancer-related deaths worldwide[1]. Common metastatic sites of lung cancer include the brain, bone, liver, adrenal glands, intrapulmonary sites, and the thorax[2]. The eye is a rare site for lung cancer metastasis. The incidence of lung cancer ocular metastasis is 0.1%-7.0%[3]. The uvea is the most common site for intraocular metastasis, followed by the choroid, iris, and ciliary body[4,5]. Between 11% and 23% of patients are asymptomatic[5]. Symptoms of malignant tumors with ocular metastases include blurred vision, loss of vision, pain, floaters, visual field defects, lumps, red eyes, flashing sensation, and diplopia[5]. Visual impairment caused by tumor metastasis seriously affects the quality of life and shortens the survival of cancer patients.
For lung cancer patients with ocular symptoms as the first manifestation, ocular metastasis and a primary lung tumor diagnosis can be difficult to establish. Because the symptoms are not specific, eye metastases are easily overlooked. At the same time, it is extremely difficult to treat ocular metastatic lesions locally and lung cancer systemically. The diagnosis and treatment of lung cancer combined with ocular metastasis are an enormous challenge for ophthalmologists and oncologists. Further improvement in the understanding of lung cancer eye metastasis, shortening the time to diagnosis, improving the diagnostic rate, and developing new targeted local treatment strategies and systemic anti-tumor treatment strategies are needed.
Herein we report a patient with lung adenocarcinoma and ocular metastasis. We also review the literature for relevant cases and analyze the clinical features, treatment, and prognosis of lung cancer patients with ocular metastasis to better guide follow-up care.
A 70-year-old male smoker presented to our hospital with a 1-mo history of body pain, chest discomfort, and right eye soreness (Figure 1).
A positron emission tomography/computed tomography scan revealed a mass in the superior lobe of the right lung. F-18 fluorodeoxyglucose hypermetabolic nodules in the right kidney suggested tumorous lesions; no hypermetabolic lesions were demonstrated in other sites.
The patient underwent a thoracoscopic right inferior lobectomy in December 2017. Hematoxylin and eosin (HE) staining showed a typical morphology for adenocarcinoma. Immunohistochemistry (IHC) demonstrated positivity for TTF-1 and Napsin A. Postoperative pathological staging revealed T1N0M0, IA. The tumor tissue was subjected to next generation sequencing (NGS; Geneplus, Beijing, China), which showed a KRAS mutation (p.G12D); EGFR, ALK, and RET were all negative. The NGS assay used HiSEquation 4000 (Illumina, San Diego, CA, United States).
The family history was unremarkable.
The patient had a regular examination postoperatively.
Chest computed tomography (CT) images obtained 2.0 mo postoperatively demonstrated a decrease in tumor size of the right renal lesion.
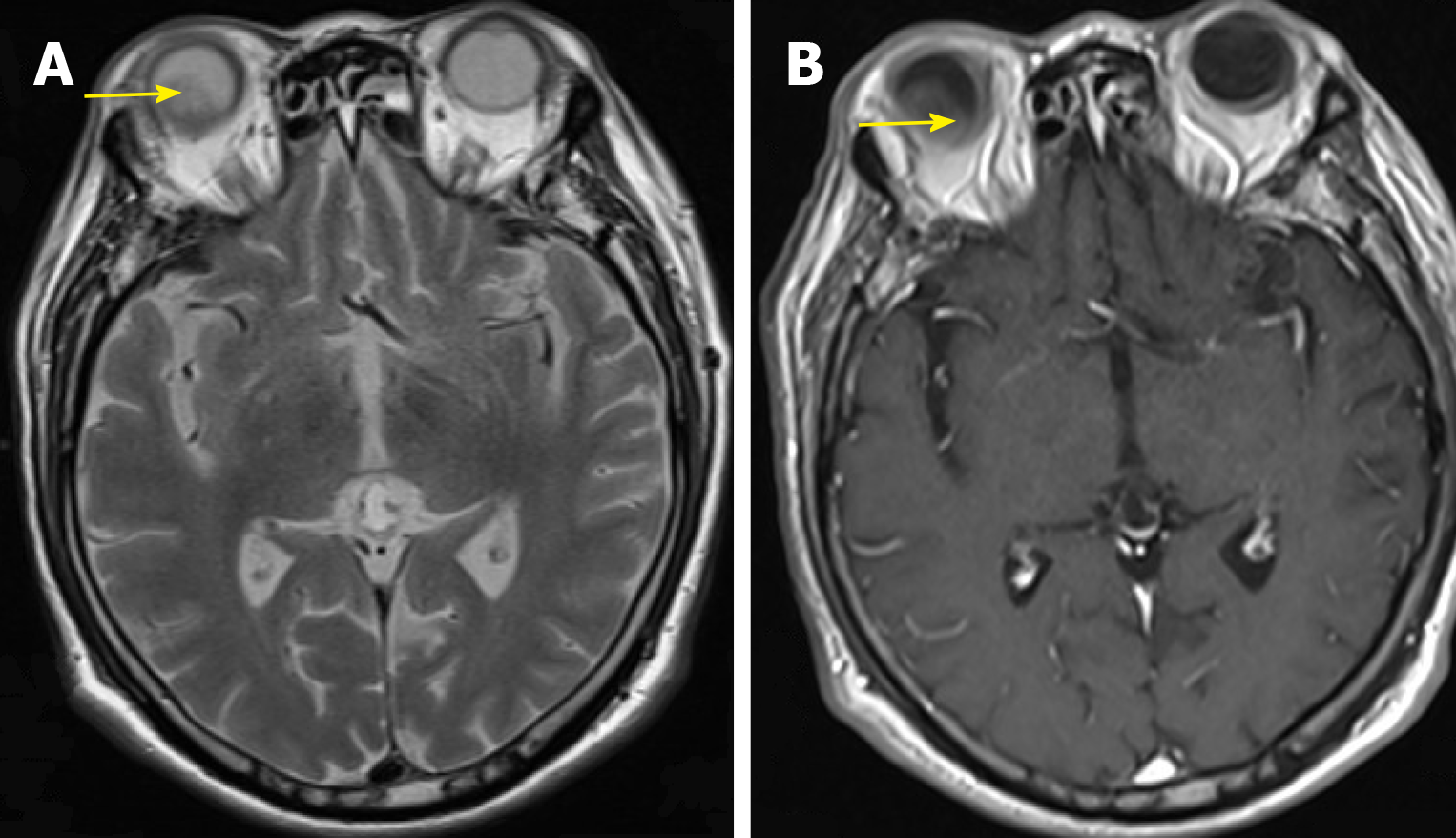
To define the nature of the mass (primary or metastasis), the patient underwent excision of the renal mass in February 2018. The postoperative pathology showed the mass to be a poorly differentiated lung adenocarcinoma metastatic to the kidney. IHC demonstrated positivity for TTF-1 and Napsin A. Brain magnetic resonance imaging (MRI) showed an abnormal signal in the right eye (Figure 2A and B). No apparent lung lesions were detected. The patient had right eye pain.
The eye lesion was considered to be metastases and symptomatic treatment was offered. The eye examinations such as visual acuity test and corneal opacity test were not performed, because the eyes were blind. The patient had a history of atrial fibrillation and was unable to tolerate chemotherapy (PS score 3). The patient was treated with the MEK inhibitor selumetinib (AZD6244; 100 mg po bid) in March 2018. After 1 week, the patient improved; the right eye and cervical vertebra pain was relieved. After 1.0 mo, brain MRI showed that the eye lesion resolved. According to the Response Evaluation Criteria in Solid Tumors guidelines (version 1.1), the patient was considered to have a partial response to selumetinib. During treatment with selumetinib, there were no treatment-related adverse events, including gastrointestinal reactions, rashes, and cordis damage; however, after 2.0 months, progression of disease occurred and left lower extremity CT suggested a left tibial neoplastic lesion (metastatic tumor was considered) in May 2018. He then received palliative radiotherapy for bone metastases. At the same time, we noted dark purple skin nodules on the right chest wall and the right lower abdomen, which were considered as subcutaneous metastases. The physical status score was 2 and we thought that he should receive chemotherapy. We initiated pemetrexed monotherapy (500 mg/m2) in June 2018. Regrettably, after 10 days, he developed a lung infection and severe anemia.
The patient died in July 2018.
Eye metastasis of lung cancer is rare; while the incidence is low, the clinical symptoms are severe. Ocular metastasis has a serious impact on the quality of life and the prognosis is poor. We report a case of lung adenocarcinoma with eye metastasis and review the clinical features, diagnosis, treatment, and prognosis of patients with lung cancer with ocular metastases. Considering this rare condition, we encourage clinicians to be aware of the existence of eye metastases from primary lung cancer in NSCLC patients. Upon diagnosis, appropriate treatment must be promptly initiated.
Eye metastasis of lung cancer is caused by blood-borne dissemination of tumors. Analysis of uveal metastases in 229 eyes from 194 patients showed that 88% of the tumors were located in the choroid; iris (10%) and ciliary body metastases (2%) also occurred, and 18% had bilateral metastases[7]. Xu et al[6] reported nine patients with ocular metastases of lung cancer and also found that the choroid was the major site. The choroid is supplied by the much larger posterior ciliary artery behind the eyeball, and there is extensive anastomotic communication between the choroidal vessels. The blood flow is rich and susceptible to metastases. Therefore, the choroid is the most common site for metastasis noted in the clinic.
Symptoms of the eye caused by eye metastasis include blurred vision, pain, floating mosquitoes, visual field defects, lumps, red eyes, flashing sensation, and double vision. Our patient had eye pain; however, the patient was initially thought to have scleritis. It is worth noting that some patients are asymptomatic. In a previous report, some patients had no ocular symptoms and choroidal metastasis was only found during routine screening[8]. Currently, whether or not such asymptomatic patients require routine screening is still controversial, but we still must be alert to the existence of such metastasis.
Imaging plays a pivotal role in the diagnosis and treatment of metastatic lesions[9]. If necessary, fine needle aspiration biopsy is needed to confirm the diagnosis[10]; however, very few patients need eye surgery for treatment and pathological evaluation to determine the diagnosis of eye metastasis from lung cancer. For patients with confirmed lung cancer, the significance of new eye symptoms should be further evaluated by eye ultrasound and/or ocular MRI. Combined with a fundus examination, it is easy to diagnose eye metastases.
The management of patients with metastasis to the eye involves cooperation between an eye cancer specialist, medical oncologist, and radiation therapist. For patients with lung cancer and ocular metastases, treatment includes systemic anti-tumor therapy and ocular local treatment, such as photocoagulation, cryosurgery, surgical resection, or radiotherapy. Patient survival depends on the efficacy of systemic therapy. Xu et al[6] analyzed the clinical efficacy of 25 patients receiving chemotherapy and found that even with systemic chemotherapy, the systemic disease control rate of patients with ocular metastases was only 28%, and the therapeutic effect was extremely poor. Combination of intravenous bevacizumab and chemotherapy in four patients controlled the tumors, suggesting that chemotherapy and anti-angiogenesis therapy can be applied, but the number of cases is small and further research is needed. For patients with EGFR mutations or who are ALK-positive, targeted therapy can alleviate systemic lesions and ocular metastases. In our case, the patient had a KRAS mutation, which is one of the most frequently mutated oncogenes in patients with NSCLC. Chemotherapy and TKI treatment in NSCLC patients with KRAS mutations yield inferior outcomes and are associated with a negative prognosis and shorter survival. Interestingly, in our report the eye lesion resolved after selumetinib treatment and demonstrated the treatment to be effective. Therefore, for lung cancer patients with ocular metastases, driver gene detection should be actively carried out, and targeted therapy be administered. Local treatment of the eye is palliative, and the purpose of treatment is to maintain visual function and improve quality of life, which includes in vitro radiotherapy (distance radiotherapy), plaque radiotherapy, and topical anti-angiogenic therapy[9].
The prognosis of lung cancer with choroidal metastasis is relatively poor, and the median survival time after diagnosis of choroidal metastasis is only 6.0-13.0 mo[9]. Our patient had a survival time of 7.0 mo. Hence, the survival prognosis depends on the treatment strategy and efficacy.
Eye metastasis is easy to be misdiagnosed and missed. Patients with lung cancer who have blurred eyesight, such as blurred vision and eye pain, should be alert to eye metastasis. The ophthalmologist has an important role in diagnosing orbital metastases in lung cancer. Therefore, multidiscipline expertise collaboration is needed to make the early diagnosis and determine the prompt treatment in patients. Lung cancer with ocular metastasis is more common in adenocarcinoma. Local treatment of the eye can control local symptoms. While systemic chemotherapy is poor, chemotherapy combined with bevacizumab or targeted therapy may be effective for systemic anti-tumor therapy.
Manuscript source: Unsolicited Manuscript
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tamura M S-Editor: Ma YJ L-Editor: Wang TQ E-Editor: Wu YXJ
| 1. | Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019;69:7-34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13300] [Cited by in RCA: 15614] [Article Influence: 2230.6] [Reference Citation Analysis (7)] |
| 2. | Hoffman PC, Mauer AM, Vokes EE. Lung cancer. Lancet. 2000;355:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 498] [Cited by in RCA: 539] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 3. | Niu FY, Zhou Q, Yang JJ, Zhong WZ, Chen ZH, Deng W, He YY, Chen HJ, Zeng Z, Ke EE, Zhao N, Zhang N, Sun HW, Zhang QY, Xie Z, Zhang XC, Wu YL. Distribution and prognosis of uncommon metastases from non-small cell lung cancer. BMC Cancer. 2016;16:149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 126] [Article Influence: 12.6] [Reference Citation Analysis (0)] |
| 4. | Kreusel KM, Wiegel T, Stange M, Bornfeld N, Hinkelbein W, Foerster MH. Choroidal metastasis in disseminated lung cancer: frequency and risk factors. Am J Ophthalmol. 2002;134:445-447. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 86] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 5. | Shields CL, Shields JA, Gross NE, Schwartz GP, Lally SE. Survey of 520 eyes with uveal metastases. Ophthalmology. 1997;104:1265-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 612] [Cited by in RCA: 622] [Article Influence: 21.4] [Reference Citation Analysis (1)] |
| 6. | Xu Y, Sun Y, Zhao J, Chen M, Jiangde L, Li L, Zhong W, Wang M. [Ocular Metastasis in Lung Cancer: a Retrospective Analysis in a Single Chinese Hospital and Literature Review]. Zhongguo Fei Ai Za Zhi. 2017;20:326-333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (2)] |
| 7. | Shah SU, Mashayekhi A, Shields CL, Walia HS, Hubbard GB, Zhang J, Shields JA. Uveal metastasis from lung cancer: clinical features, treatment, and outcome in 194 patients. Ophthalmology. 2014;121:352-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 115] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 8. | Barak A, Neudorfer M, Heilweil G, Merimsky O, Lowenstein A, Inbar M, Yaal-Hahoshen N. Decreased prevalence of asymptomatic choroidal metastasis in disseminated breast and lung cancer: argument against screening. Br J Ophthalmol. 2007;91:74-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 34] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 9. | Lampaki S, Kioumis I, Pitsiou G, Lazaridis G, Syrigos K, Trakada G, Kakolyris S, Zarogoulidis K, Mpoukovinas I, Rapti A, Zarogoulidis P. Lung cancer and eye metastases. Med Hypothesis Discov Innov Ophthalmol. 2014;3:40-44. [PubMed] |
| 10. | Singh AD, Biscotti CV. Fine needle aspiration biopsy of ophthalmic tumors. Saudi J Ophthalmol. 2012;26:117-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 1.8] [Reference Citation Analysis (1)] |