Published online Jan 26, 2020. doi: 10.12998/wjcc.v8.i2.255
Peer-review started: September 6, 2019
First decision: November 12, 2019
Revised: November 29, 2019
Accepted: December 21, 2019
Article in press: December 21, 2019
Published online: January 26, 2020
Processing time: 133 Days and 3.7 Hours
Fulminant myocarditis is the critical form of myocarditis that is often associated with heart failure, malignant arrhythmia, and circulatory failure. Patients with fulminant myocarditis who end up with severe multiple organic failure and death are not rare.
To analyze the predictors of in-hospital major adverse cardiovascular events (MACE) in patients diagnosed with fulminant myocarditis.
We included a cohort of adult patients diagnosed with fulminant myocarditis who were admitted to Beijing Anzhen Hospital from January 2007 to December 2017. The primary endpoint was defined as in-hospital MACE, including death, cardiac arrest, cardiac shock, and ventricular fibrillation. Baseline demographics, clinical history, characteristics of electrocardiograph and ultrasonic cardiogram, laboratory examination, and treatment were recorded. Multivariable logistic regression was used to examine risk factors for in-hospital MACE, and the variables were subsequently assessed by the area under the receiver operating characteristic curve (AUC).
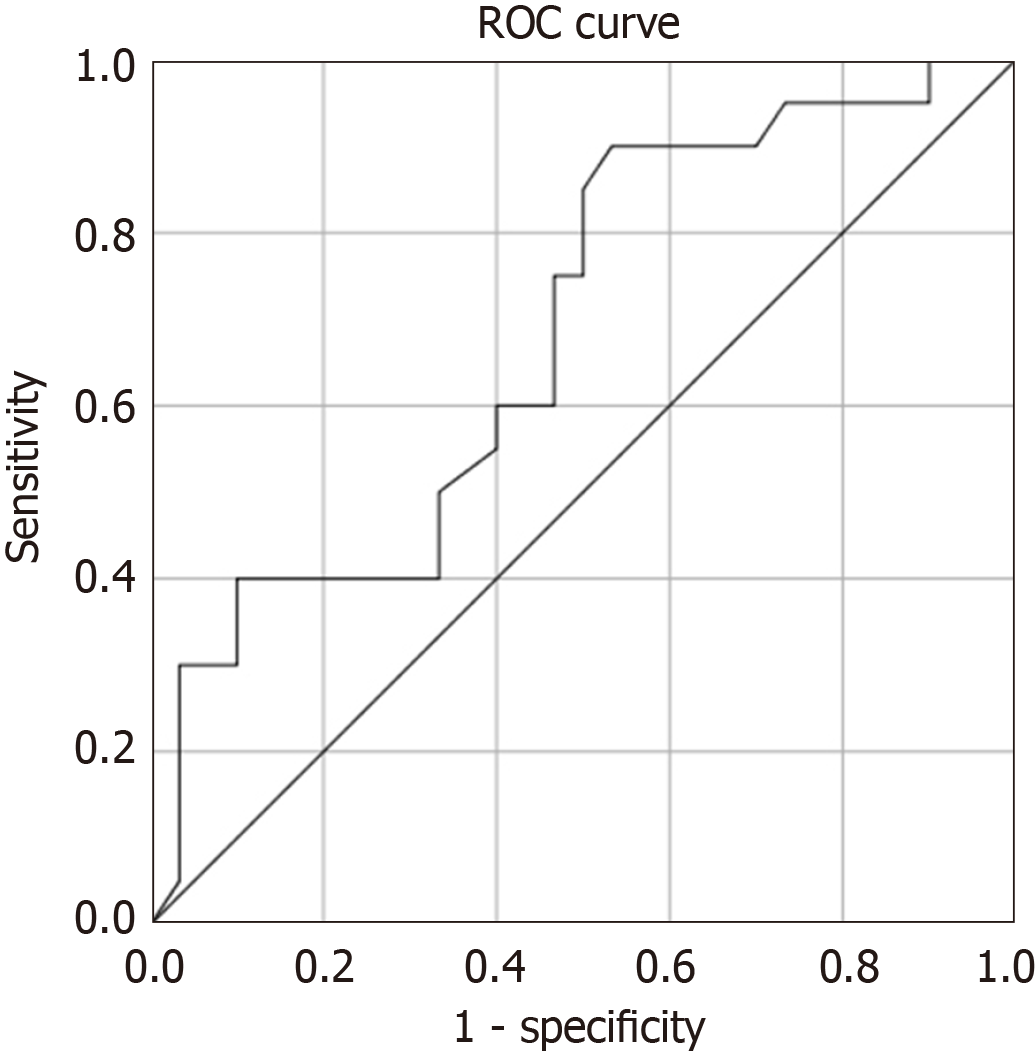
The rate of in-hospital MACE was 40%. Multivariable logistic regression analysis revealed that baseline QRS duration > 120 ms was the independent risk factor for in-hospital MACE (odds ratio = 4.57, 95%CI: 1.23-16.94, P = 0.023). The AUC of QRS duration > 120 ms for predicting in-hospital MACE was 0.683 (95%CI: 0.532-0.833, P = 0.03).
Patients with fulminant myocarditis has a poor outcome. Baseline QRS duration is the independent risk factor for poor outcome in those patients.
Core tip: The onset of outbreak myocarditis is acute, and the incidence of major adverse cardiovascular events (MACE) is higher in female patients during hospitalization. QRS broadening in baseline electrocardiogram (QRS > 120 ms) is an independent risk factor for the occurrence of MACE in outbreak myocarditis patients during hospitalization. Baseline QRS width has predictive value for the occurrence of MACE in outbreak myocarditis patients during hospitalization. In clinical practice, patients with these characteristics should be treated actively as soon as possible, and mechanical support should be given when necessary, in order to improve the prognosis of patients.
- Citation: Kang TD, Ren YL, Zhao H, Ning SQ, Liu WX. Risk factors for adverse cardiac events in adults with fulminant myocarditis during hospitalization. World J Clin Cases 2020; 8(2): 255-263
- URL: https://www.wjgnet.com/2307-8960/full/v8/i2/255.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i2.255
Myocarditis is an inflammatory disease of the myocardium that may be triggered by different non-ischemic stimuli. It has a broad spectrum of clinical presentations, ranging from mild symptoms such as malaise and chest pain without (or with minimal) heart dysfunction to life-threatening arrhythmias and/or severe heart failure (HF). Fulminant myocarditis is the critical form among them and is often associated with heart failure, malignant arrhythmia, and circulatory failure. Most of the time, the inflammation and subsequent myocardial injury can resolve spontaneously without clinically relevant residual damage[1]. Whereas, patients with fulminant myocarditis who end up with severe multiple organic failure and death are not rare. In this study, we sought to investigate the relationship between clinical characteristics and major adverse cardiovascular events (MACE) in patients with fulminant myocarditis.
This retrospective study enrolled 50 patients with fulminant myocarditis hospitalized at Beijing Anzhen hospital, Capital Medical University from January 2007 to December 2017. The patients were consecutively enrolled, and there were no pre-specified exclusion criteria. The patients received therapy in accordance with contemporary practice guidelines. Baseline and procedural data for all participants were collected by independent clinical research coordinators. The diagnostic criteria for fulminant myocarditis were defined as acute illness (< 4 wk of history since symptom onset), hemodynamic instability due to cardiogenic shock or arrhythmias (including aborted sudden cardiac death), and need for hemodynamic support (inotrope/mechanical circulatory support)[2].
Clinical data were collected, including the history of precursor infection, baseline blood pressure and heart rate at admission, laboratory test data, electrocardiogram (ECG) findings, echocardiogram results, main treatment during hospitalization (including drug treatment and mechanical adjuvant therapy), complications, and outcomes.
Death, cardiac arrest, cardiogenic shock, and ventricular fibrillation during hospitalization were defined as MACE. The patients were divided into an MACE group and event-free group. The differences between the two groups were compared and the influencing factors were analyzed.
Measurement data conforming to a normal distribution are expressed as the mean ± SD. Intergroup comparisons were performed by the t-test. Measurement data not conforming to a normal distribution are expressed as the median and interquartile spacing [M (Q1, Q3)]. The rank sum test was used for inter-group comparisons. Count data are expressed as frequencies and percentages. The Chi-square test or Fisher's exact probability method was used for comparisons between groups. Logistic regression was used to analyze the influencing factors of adverse cardiac events in adult patients with fulminant myocarditis during hospitalization. The significant level was set at P < 0.05 and variables with P > 0.10 were excluded. The predictive value of baseline QRS width for MACE during hospitalization was assessed by receiver operating characteristic (ROC) curve analysis. SPSS 25.0 was used for statistical analyses, and P values < 0.05 were considered statistically significant.
Among the 50 patients enrolled, 20 were in the MACE group (7 died, 10 needed extra-cardiac compression for cardiac arrest, 17 had cardiogenic shock, and 7 had ventricular fibrillation) and 30 in the event-free group. The age of patients in the two groups was similar. The proportion of women in the MACE group was significantly higher than that in the event-free group. The proportion of patients with clear precursory symptoms in the two groups was similar. Compared with the event-free group, systolic blood pressure was significantly lower and heart rate was significantly faster in the MACE group at admission (Table 1).
| MACE group (n = 20) | Event-free group (n = 30) | P value | |
| Age (yr) | 31.00 (25.50-48.00) | 26.50 (19.75-34.25) | 0.058 |
| Gender | 0.049 | ||
| Male | 7 (35) | 19 (63.3) | |
| Female | 13 (65) | 11 (36.7) | |
| Precursory symptoms | 19 (95) | 25 (83.3) | 0.381 |
| Fever | 16 (80) | 18 (60) | 0.137 |
| Systolic blood pressure (mmHg) | 87.40 ± 14.91 | 105.77 ± 19.07 | 0.001 |
| Hart rate (beats per minute) | 103.05 ± 22.70 | 86.97 ± 25.04 | 0.025 |
Compared with the group without MACE, the numbers of leukocytes and neutrophils in the MACE group were higher. Hemoglobin in the MACE group was slightly lower than that in the group without MACE, and there was no significant difference in platelet count between the two groups. The levels of urea nitrogen and creatinine in the MACE group were significantly higher than those in the group without MACE, and there was no significant difference in myocardium between the two alanine aminotransferase groups. In the detection of markers and enzymes, the baseline levels of TnI, TnI peak, baseline creatine kinase-MB (CK-MB), CK-MB peak, baseline CK, and CK peak in the MACE group were significantly higher than those in the event-free group; the D-dimer level in the MACE group was higher than that in the event-free group; and the baseline lactate level in the MACE group was significantly higher than that in the event-free group (Table 2).
| MACE group (n = 20) | Event-free group (n = 30) | P value | |
| WBC (×109/L) | 15.16 ± 7.12 | 9.11 ± 3.20 | 0.002 |
| NEUT (×109/L) | 12.88 ± 6.88 | 6.66 ± 2.94 | 0.001 |
| Hemoglobin (g/L) | 123.36 ± 21.04 | 136.11 ± 18.03 | 0.026 |
| Platelets (×109/L) | 171.89 ± 115.79 | 208.85 ± 69.53 | 0.165 |
| ALT (U/L) | 133.50 (65.25-1584.25) | 72.00 (38.75-446.25) | 0.076 |
| BUN | 9.60 (6.36-17.00) | 5.55 (4.11-7.67) | < 0.001 |
| Creatine (μmol/L) | 109.65 (78.35-322.65) | 79.45 (66.70-87.48) | 0.003 |
| Troponin I (ng/mL) | 28.80 (8.35-87.95) | 10.30 (2.22-28.61) | 0.012 |
| Peak troponin I (ng/mL) | 34.92 (15.74-100.26) | 12.09 (2.38-48.44) | 0.014 |
| CK-MB (ng/mL) | 94.30 (31.00-122.10) | 21.40 (6.70-64.60) | 0.004 |
| Peak CK-MB (ng/mL) | 116.10 (66.10-170.60) | 22.30 (7.40-68.30) | 0.002 |
| CK (U/L) | 959.00 (307.00-1432.00) | 423.00 (149.50-710.00) | 0.044 |
| Peak CK (U/L) | 1545.00 (821.00-2067.00) | 464.00 (206.25-860.00) | 0.010 |
| D-dimer (μg/L) | 1706.00 (493.00-8608.00) | 303.00 (86.00-620.75) | 0.001 |
| Lactic acid (mmol/L) | 3.35 (2.03-6.83) | 1.45 (0.98-1.93) | < 0.001 |
Echocardiographic studies found that although left ventricular ejection fraction (LVEF) at admission in the MACE group was lower than that in the event-free group, there was no significant difference between them. The proportion of patients with LVEF < 50% was similar between the two groups, and there was no significant difference in left ventricular end diastolic diameter or interventricular septal thickness between the two groups. The analysis of abnormal ECG showed that the proportion of patients with ST segment elevation and III degree atrioventricular block (AVB) was similar in the two groups; the baseline QRS width in the MACE group was significantly higher than that in the event-free group, and the proportion of patients with QRS wave broadening (> 120 ms) in the MACE group was significantly higher (Table 3).
| MACE group (n = 20) | Event-free group (n = 30) | P value | |
| EF (%) | 35.55 ± 20.34 | 45.37 ± 11.96 | 0.062 |
| EF < 50% | 15 (75) | 21 (70) | 0.700 |
| LVEDD (mm) | 46.55 ± 4.82 | 49.07 ± 6.19 | 0.132 |
| IVST (mm) | 11.00 (8.25-12.00) | 9.00 (8.00-11.23) | 0.255 |
| ST elevation | 14 (70) | 13 (43.3) | 0.064 |
| III°AVB | 9 (45) | 11 (36.7) | 0.556 |
| QRS widen | 16 (80) | 14 (46.7) | 0.018 |
| QRS duration (ms) | 138.50 (111.75-160.25) | 111.00 (94.00-146.00) | 0.030 |
The proportion of patients with positive inotropic drugs and vasoactive drugs (dopamine, norepinephrine, and adrenaline) used in the MACE group was higher than that in the event-free group, and the proportion of patients with diuretics used in the two groups was similar. The proportion of patients with glucocorticoid and immunoglobulin used in the two groups was similar; breathing machine, continuous renal replacement therapy, extracorporeal membrane oxygenation (ECMO), and intra-aortic balloon pump (IABP) were used in the MACE group (five cases). There was no significant difference in the proportion of patients with temporary pacemaker used between the two groups (Table 4).
| MACE group (n = 20) | Event-free group (n = 30) | P value | |
| Diuretics | 14 (70) | 22 (73.3) | 0.797 |
| Inotropic agents | 14 (70) | 9 (30) | 0.005 |
| Vasoactive agents | 20 (100) | 11 (36.7) | < 0.001 |
| Glucocorticoid | 6 (30) | 10 (33.3) | 0.804 |
| Immune globulin | 6 (30) | 8 (26.7) | 0.797 |
| Temporary pacemaker | 5 (25) | 8 (26.7) | 0.895 |
| Ventilator | 13 (65) | 1 (3.3) | < 0.001 |
| CRRT | 9 (45) | 0 (0) | < 0.001 |
| ECMO | 9 (45) | 1 (3.3) | 0.001 |
| IABP | 6 (30) | 0 (0) | 0.002 |
Logistic regression analysis showed that QRS broadening in baseline electrocardiogram (QRS > 120 ms) was an independent risk factor for MACE in patients with fulminant myocarditis during hospitalization. Compared with patients with normal QRS width, the odds ratio of MACE in patients with widened QRS was 4.57 (P = 0.023, 95%CI: 1.23-16.94). The predictive value of baseline QRS width for MACE during hospitalization was analyzed using ROC. The area under the curve (AUC) was 0.683 (SE = 0.077, P = 0.030, 95%CI: 0.532-0.833) (Figure 1).
This study retrospectively analyzed the clinical data of 50 adult patients with fulminant myocarditis, and compared the characteristics of patients with and without MACE during hospitalization. The age of the two groups was similar, and most of them were young and middle-aged. Although the overall numbers of male and female patients with fulminant myocarditis were close, the proportion of female patients in the MACE group was significantly higher than that in the event-free group. Some studies reported that the prognosis of female patients was poor, and the condition of adult female patients with fulminant myocarditis might be more critical[3]. There was no difference in the symptoms of prodromal infection between the two groups. Compared with the patients without MACE, the systolic blood pressure was lower and the heart rate was faster in the MACE group at admission, suggesting that the patients with MACE had more unstable hemodynamic performance at admission and needed active treatment as soon as possible.
In terms of laboratory tests, this study found that the blood leucocytes and neutrophils in the MACE group were higher than those in the event-free group, suggesting that the patients in the MACE group may have more severe infections. The hemoglobin in the MACE group was slightly lower than that of the event-free group. The reason is that there is a gender difference in hemoglobin concentration itself, and the higher proportion of women in the MACE group may lead to this difference. In terms of liver and kidney function, the levels of urea nitrogen and creatinine in the MACE group were significantly higher than those in the event-free group, suggesting that the patients in this group were more likely to suffer from acute renal function damage. After analyzing the myocardial markers and myocardial enzymatic characteristics of the two groups, it was found that the baseline levels of TnI, TNI peak, baseline CK-MB, CK-MB peak, baseline CK, and CK peak in the MACE group were significantly higher than those in the event-free group, suggesting that myocardial cell damage was more serious and the condition was more critical in the former group of patients. The levels of D-dimer and lactic acid in the MACE group were higher than those in event-free group. The significant increase of D-dimer suggested that hypercoagulability, thrombosis, and secondary hyper-fibrinolysis might exist in the body. In shock state, tissue perfusion insufficiency and endothelial cell injury can lead to micro-thrombosis and elevated D-dimer in blood[4], and elevated blood lactic acid is also a manifestation of tissue and organ perfusion insufficiency. In this study, the baseline D-dimer and lactic acid levels in the MACE patients increased significantly, suggesting that organ tissue perfusion is seriously insufficient.
In terms of echocardiography, the study found that the mean value of LVEF at admission was less than 50% of the normal level in both groups. Compared with the event-free group, the LVEF at admission in the MACE group was lower, but there was no significant difference. The proportion of patients with LVEF < 50% in both groups was > 50%. There was no significant difference between the two groups. The left ventricular end-diastolic diameter values of the two groups were within the normal range, and there was no significant difference between the two groups. On the one hand, in patients with fulminant myocarditis, besides myocardial cell damage and necrosis, some myocardial cells are in a highly edematous state, which together lead to serious damage of cardiac function. When the cardiac structure has not yet changed compensatively, the pump function has been significantly reduced, the disease progresses rapidly, and it is more prone to drastic changes in hemodynamics. Although the interventricular septal thickness in the MACE group was thicker than that in the event-free group, there was no significant difference between the two groups. Some studies have found that patients with fulminant myocarditis may have ventricular septal thickening in the early days of the disease, and then gradually return to normal, while the left ventricular end-diastolic diameter is basically normal in the course of the disease[5-7]. The reason for the increase of ventricular septal thickness may be due to myocardial cell edema. In this study, no difference in ventricular septal thickness was found between the two groups, presumably due to the bias of retrospective study.
The analysis of abnormal ECG showed that the baseline QRS width of the MACE group was significantly higher than that of the event-free group, and the proportion of patients with QRS wave broadening (> 120 ms) in the MACE group was significantly higher than that of the event-free group. Further logistic regression analysis showed that QRS wave broadening (QRS > 120 ms) was an independent risk factor for MACE in patients with fulminant myocarditis during hospitalization. Compared with patients with normal QRS wave width, the OR of MACE in patients with QRS wave broadening in baseline electrocardiogram during hospitalization was 4.57 (P = 0.023, 95%CI: 1.23-16.94). ROC was used to analyze the predictive value of baseline QRS width for MACE during hospitalization, and the result (AUC = 0.683, SE = 0.077, P = 0.030, 95%CI: 0.532-0.833) suggested that baseline QRS width had predictive value for MACE during hospitalization in patients with fulminant myocarditis. Some studies have shown that QRS wave broadening suggests serious involvement of the cardiac conduction system, which may be related to diffuse infiltration of inflammation[8-10]. The disease usually changes more rapidly, often predicting a poor prognosis. The results in this paper are consistent with the relevant reports, which suggest that clinical workers should closely monitor the patients with myocarditis with QRS wave broadening in the early stage. Early initiation of more aggressive treatment, including mechanical support therapy, can improve the prognosis of patients. In the aspect of severe bradyarrhythmia, there was no significant difference in the proportion of patients with high AVB between the two groups. Some studies showed that the high degree AVB did not predict a worse prognosis in patients with myocarditis[11].
The onset of fulminant myocarditis is a rapid process, and serious hemodynamic changes often occur in no time. Therefore, more active drug treatment or even mechanical adjuvant therapy should be adopted in the treatment of fulminant myocarditis, so as to stabilize the vital signs of patients as soon as possible. In this study, the proportion of patients with vasoactive drugs (dopamine, norepinephrine, and adrenaline) and positive inotropic drugs used in the MACE group was higher than that in the event-free group, which was related to more hemodynamic instability in this group. At present, there is no specific recommendation for the use of glucocorticoids and intravenous immunoglobulin therapy. Some case reports and small-scale studies found that patients may benefit from such treatment, but large-scale clinical trials are needed to verify the application timing, dosage, and course of immunosuppressive immunomodulation therapy[12-16]. With regard to mechanical support therapy, fulminant myocarditis has its own limitation. Although the myocardial cells of patients have serious dysfunction in a short time, resulting in rapid deterioration of hemodynamics, if the myocardial cells recover gradually after the acute phase, they may have a better prognosis. Therefore, effective auxiliary support in the acute phase may play a role in the prognosis of patients. At present, ECMO has gradually become an effective adjuvant therapy in patients with fulminant myocarditis[17-22]. However, the optimal timing of ECMO implantation and the indication of weaning are not clearly recommended, and more clinical studies are needed to explore this issue. For patients with high atrioventricular block, temporary pacemaker implantation is a simple and effective method. Patients with fulminant myocarditis involving the cardiac conduction system will gradually resume conduction function after several days. Most patients can successfully remove temporary pacemaker[23]. IABP can relieve the left ventricular afterload and play an auxiliary role in patients with severe left ventricular dysfunction, but its role still depends on the residual left ventricular function, while the cardiac function of some patients with fulminant myocarditis decreases sharply in the early stage or almost has no effective contraction. At this time, the role of IABP in patients with fulminant myocarditis is extremely limited. In this study, IABP was used in combination with ECMO to reduce left ventricular afterload to a certain extent.
There are some limitations in this study. There is a lack of pathological data of myocardial biopsy and sufficient etiological data. In addition, the sample size of this study is relatively small, and it is a retrospective study performed in a single center. There may be some bias in selection. Further research is needed after further enlarging the sample size.
In summary, the onset of outbreak myocarditis is acute, and the incidence of MACE is higher in female patients during hospitalization. QRS broadening in baseline electrocardiogram (QRS > 120 ms) is an independent risk factor for the occurrence of MACE in outbreak myocarditis patients during hospitalization. The baseline QRS width has predictive value for the occurrence of MACE in outbreak myocarditis patients during hospitalization. In clinic, patients with these characteristics should be treated actively as soon as possible, and mechanical support should be given when necessary, in order to improve the prognosis of patients.
Fulminant myocarditis is the critical form of myocarditis often associated with heart failure, malignant arrhythmia, and circulatory failure. Patients with fulminant myocarditis who end up with severe multiple organic failure and death are not rare.
In this study, the authors aimed to analyze the predictors of in-hospital major adverse cardiovascular events (MACE) in patients diagnosed with fulminant myocarditis.
The authors built a cohort of adult patients diagnosed with fulminant myocarditis. The primary endpoint was defined as in-hospital MACE, including death, cardiac arrest, cardiac shock, and ventricular fibrillation. Baseline demographics, clinical history, characteristics of electrocardiograph and ultrasonic cardiogram, laboratory examination, and treatment were recorded.
The rate of in-hospital MACE was 40%. Multivariable logistic regression analysis demonstrated that baseline QRS duration > 120 ms was an independent risk factor for in-hospital MACE. The area under curve of QRS duration > 120 ms for predicting in-hospital MACE was 0.683.
The onset of outbreak myocarditis is acute, and the incidence of MACE is higher in female patients during hospitalization. QRS broadening in baseline electrocardiogram (QRS > 120 ms) is an independent risk factor for the occurrence of MACE in outbreak myocarditis patients during hospitalization.
Baseline QRS width has predictive value for the occurrence of MACE in outbreak myocarditis patients during hospitalization. Patients with these characteristics should be treated actively as soon as possible in clinic, and mechanical support should be given when necessary, in order to improve the prognosis of patients.
| 1. | Cooper LT. Myocarditis. N Engl J Med. 2009;360:1526-1538. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1075] [Cited by in RCA: 1023] [Article Influence: 60.2] [Reference Citation Analysis (0)] |
| 2. | Ammirati E, Veronese G, Cipriani M, Moroni F, Garascia A, Brambatti M, Adler ED, Frigerio M. Acute and Fulminant Myocarditis: a Pragmatic Clinical Approach to Diagnosis and Treatment. Curr Cardiol Rep. 2018;20:114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 84] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 3. | Kytö V, Sipilä J, Rautava P. The effects of gender and age on occurrence of clinically suspected myocarditis in adulthood. Heart. 2013;99:1681-1684. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 4. | Yucel O, Yucel H, Zorlu A. D-dimer is a predictor of cardiovascular death, and new-onset atrial fibrillation in patients with systolic heart failure. Int J Cardiol. 2017;247:39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Felker GM, Boehmer JP, Hruban RH, Hutchins GM, Kasper EK, Baughman KL, Hare JM. Echocardiographic findings in fulminant and acute myocarditis. J Am Coll Cardiol. 2000;36:227-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 279] [Cited by in RCA: 265] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 6. | Morimoto S, Kato S, Hiramitsu S, Uemura A, Ohtsuki M, Kato Y, Sugiura A, Miyagishima K, Yoshida Y, Hishida H. Role of myocardial interstitial edema in conduction disturbances in acute myocarditis. Heart Vessels. 2006;21:356-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 7. | Hiramitsu S, Morimoto S, Kato S, Uemura A, Ohtsuki M, Kato Y, Sugiura A, Miyagishima K, Mori N, Yoda R, Mori K, Iwase M, Hishida H. Significance of transient left ventricular wall thickening in acute lymphocytic myocarditis. Heart Vessels. 2007;22:25-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Ukena C, Mahfoud F, Kindermann I, Kandolf R, Kindermann M, Böhm M. Prognostic electrocardiographic parameters in patients with suspected myocarditis. Eur J Heart Fail. 2011;13:398-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 130] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 9. | Lee CH, Tsai WC, Hsu CH, Liu PY, Lin LJ, Chen JH. Predictive factors of a fulminant course in acute myocarditis. Int J Cardiol. 2006;109:142-145. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Kato S, Morimoto S, Hiramitsu S, Uemura A, Ohtsuki M, Kato Y, Miyagishima K, Yoshida Y, Hashimoto S, Hishida H. Risk factors for patients developing a fulminant course with acute myocarditis. Circ J. 2004;68:734-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Wang Z, Wang Y, Lin H, Wang S, Cai X, Gao D. Early characteristics of fulminant myocarditis vs non-fulminant myocarditis: A meta-analysis. Medicine (Baltimore). 2019;98:e14697. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 12. | Chen HS, Wang W, Wu SN, Liu JP. Corticosteroids for viral myocarditis. Cochrane Database Syst Rev. 2013;CD004471. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 71] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 13. | Kohno K, Aoyama N, Shimohama T, Yoshida M, Machida Y, Fukuda N, Aizaki T, Suzuki K, Kurosawa T, Izumi T. Resuscitation from fulminant myocarditis associated with refractory ventricular fibrillation. Jpn Circ J. 2000;64:139-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Nakashima H, Umeyama Y, Minami K. Successive immunosuppressive treatment of fulminant myocarditis that is refractory to mechanical circulatory support. Am J Case Rep. 2013;14:116-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Tsai YG, Ou TY, Wang CC, Tsai MC, Yuh YS, Hwang B. Intravenous gamma-globulin therapy in myocarditis complicated with complete heart block: Report of one case. Acta Paediatr Taiwan. 2001;42:311-313. [PubMed] |
| 16. | Goland S, Czer LS, Siegel RJ, Tabak S, Jordan S, Luthringer D, Mirocha J, Coleman B, Kass RM, Trento A. Intravenous immunoglobulin treatment for acute fulminant inflammatory cardiomyopathy: series of six patients and review of literature. Can J Cardiol. 2008;24:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 51] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 17. | Chen YS, Yu HY, Huang SC, Chiu KM, Lin TY, Lai LP, Lin FY, Wang SS, Chu SH, Ko WJ. Experience and result of extracorporeal membrane oxygenation in treating fulminant myocarditis with shock: what mechanical support should be considered first? J Heart Lung Transplant. 2005;24:81-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 18. | Hsu KH, Chi NH, Yu HY, Wang CH, Huang SC, Wang SS, Ko WJ, Chen YS. Extracorporeal membranous oxygenation support for acute fulminant myocarditis: analysis of a single center's experience. Eur J Cardiothorac Surg. 2011;40:682-688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 64] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 19. | Lorusso R, Centofanti P, Gelsomino S, Barili F, Di Mauro M, Orlando P, Botta L, Milazzo F, Actis Dato G, Casabona R, Casali G, Musumeci F, De Bonis M, Zangrillo A, Alfieri O, Pellegrini C, Mazzola S, Coletti G, Vizzardi E, Bianco R, Gerosa G, Massetti M, Caldaroni F, Pilato E, Pacini D, Di Bartolomeo R, Marinelli G, Sponga S, Livi U, Mauro R, Mariscalco G, Beghi C, Miceli A, Glauber M, Pappalardo F, Russo CF; GIROC Investigators. Venoarterial Extracorporeal Membrane Oxygenation for Acute Fulminant Myocarditis in Adult Patients: A 5-Year Multi-Institutional Experience. Ann Thorac Surg. 2016;101:919-926. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 138] [Article Influence: 12.5] [Reference Citation Analysis (0)] |
| 20. | Chen YS, Wang MJ, Chou NK, Han YY, Chiu IS, Lin FY, Chu SH, Ko WJ. Rescue for acute myocarditis with shock by extracorporeal membrane oxygenation. Ann Thorac Surg. 1999;68:2220-2224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 42] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Asaumi Y, Yasuda S, Morii I, Kakuchi H, Otsuka Y, Kawamura A, Sasako Y, Nakatani T, Nonogi H, Miyazaki S. Favourable clinical outcome in patients with cardiogenic shock due to fulminant myocarditis supported by percutaneous extracorporeal membrane oxygenation. Eur Heart J. 2005;26:2185-2192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 162] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 22. | Ganatra S, Neilan TG. Immune Checkpoint Inhibitor-Associated Myocarditis. Oncologist. 2018;23:879-886. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 225] [Article Influence: 28.1] [Reference Citation Analysis (0)] |
| 23. | Lee EY, Lee HL, Kim HT, Lee HD, Park JA. Clinical features and short-term outcomes of pediatric acute fulminant myocarditis in a single center. Korean J Pediatr. 2014;57:489-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Malieckal A, Treepongkaruna S S-Editor: Wang JL L-Editor: Wang TQ E-Editor: Qi LL