Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4499
Peer-review started: June 30, 2020
First decision: July 24, 2020
Revised: August 4, 2020
Accepted: August 26, 2020
Article in press: August 26, 2020
Published online: October 6, 2020
Processing time: 88 Days and 21.2 Hours
In most cases, it is not difficult to differentiate common bile duct (CBD) stone from Ascaris infection because they are different disease entities and have different imaging findings. The two diseases usually demonstrate unique characteristic findings on computed tomography or magnetic resonance cholangiopancreatography. However, we report a rare case from our experience in which a CBD stone mimicked and was misdiagnosed as Ascaris.
A 72-year-old male presented with elevated serum liver enzymes. Computed tomography showed a hyper-attenuated, elongated lesion in the CBD lumen and associated biliary inflammation. Magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography revealed a linear filling defect in the bile duct. Moreover, elongated echogenic material with a central hypoechogenic area was seen on endoscopic ultrasound. Although the imaging findings caused us to suspect infection with the nematode Ascaris, the lesion was revealed to be a dark-brown-colored CBD stone through endoscopic extraction.
We report a rare case of a CBD stone that mimicked Ascaris. We also review the literature for side-by-side comparisons of the imaging features of CBD stones and ascariasis.
Core Tip: Although common bile duct stone and Ascaris are not commonly discussed as differential diagnosis each other, they can be misunderstood in case of the elongated common bile duct stone. We should be able to learn the differential points through this case.
- Citation: Choi SY, Jo HE, Lee YN, Lee JE, Lee MH, Lim S, Yi BH. Ascaris-mimicking common bile duct stone: A case report. World J Clin Cases 2020; 8(19): 4499-4504
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4499.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4499
Choledocholithiasis, or common bile duct (CBD) stones, is a relatively common disease, and 10% to 15% of people with gallstones also have stones in the bile duct[1,2]. Biliary stones usually have angulated shapes or lamellated appearances and commonly accompany biliary inflammation. CBD stones are not difficult to diagnose when they manifest as high-density lesions in the distal CBD lumen without enhancement on computed tomography (CT) and when they demonstrate biliary filling defects with relatively low signal intensity on T2-weighted images of magnetic resonance (MR) cholangiography[2].
However, Ascaris infection can complicate diagnosis of choledocholithiasis. Although its incidence has been decreasing, ascariasis is still an important cause of pancreatobiliary disease in Asia, Africa, and South America. The worms are usually found in the intestinal lumen, but they occasionally move into the bile duct and gallbladder through the ampulla of Vater[3]. Diagnosis of hepatobiliary ascariasis can be made by visualizing the larvae in the biliary tree, as they may manifest as a cylindrical filling defect with or without movement on imaging studies[4].
Usually, there is little confusion in differentiation of CBD stone and Ascaris since they are different disease entities with different imaging manifestations. However, we report a case of a CBD stone that mimicked and was misdiagnosed as Ascaris lumbricoides.
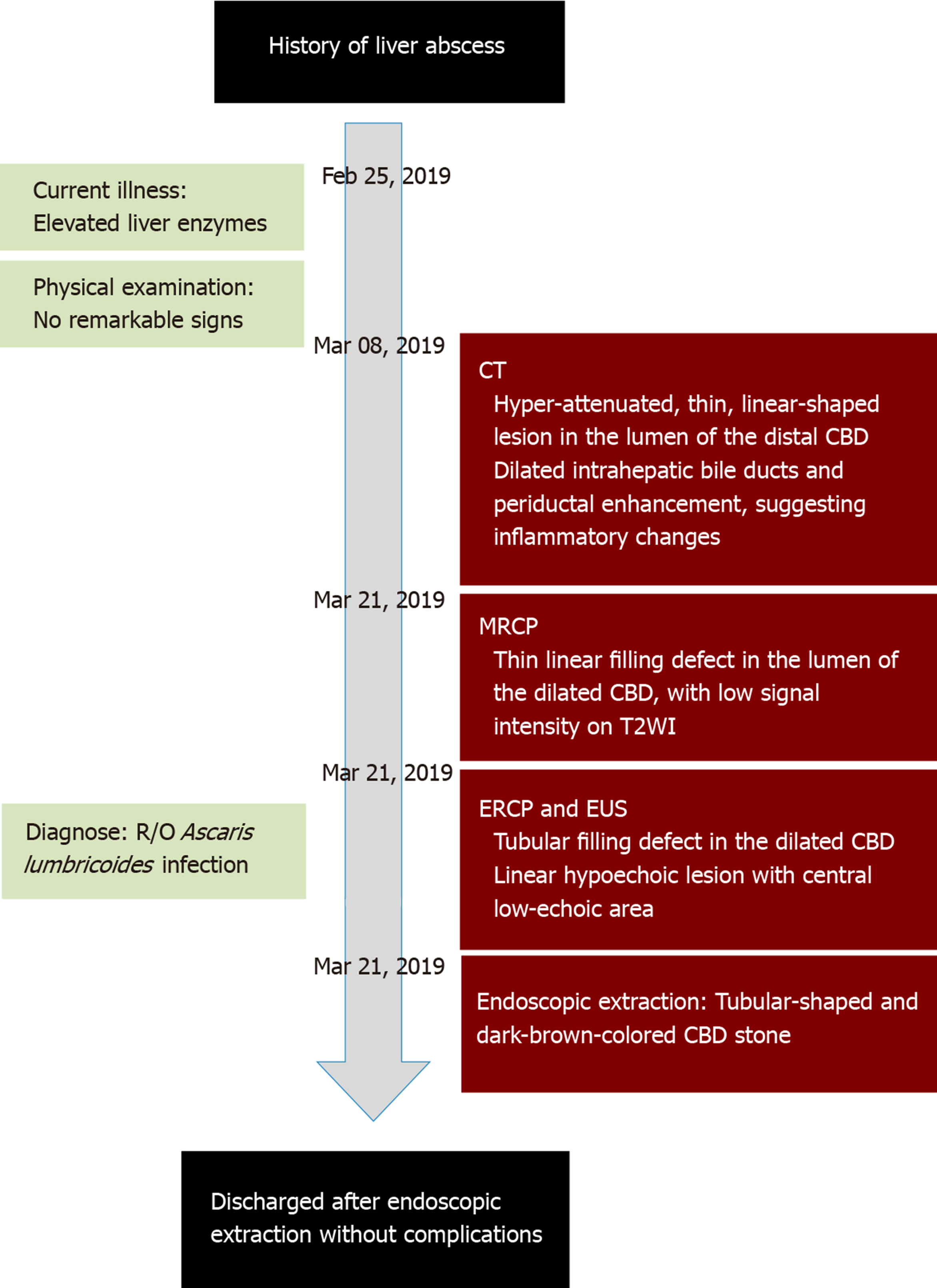
A 72-year-old male visited our outpatient clinic with elevated liver enzymes.
He did not complain of any symptoms.
He had been previously admitted to our hospital for a liver abscess about 10 years prior, when he had visited our outpatient clinic.
There were no remarkable signs, and his vital signs were normal.
Laboratory values revealed conspicuous elevation of alkaline phosphatase and gamma-glutamyl transpeptidase (γ-GT) in addition to mild elevation of serum amylase.
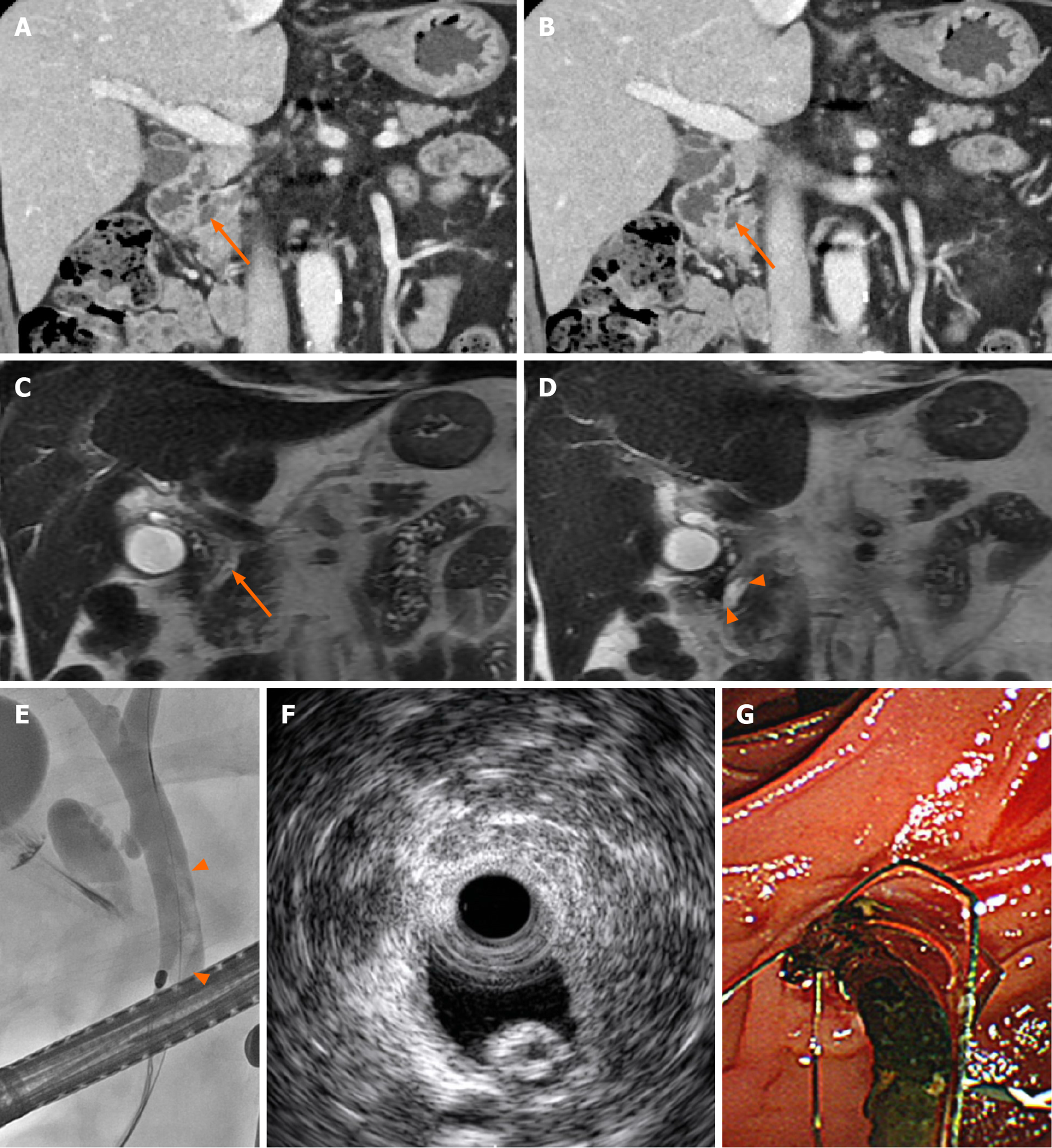
On CT (Figure 1A and B), a hyper-attenuated, thin, linear-shaped lesion was found in the lumen of the distal CBD. In addition, dilated intrahepatic bile ducts and periductal enhancement on the arterial phase suggested inflammatory changes of the intrahepatic bile duct. MR cholangiopancreatography (MRCP; Figure 1C and D) revealed a thin, linear filling defect in the lumen of the dilated CBD that had low signal intensity on T2-weighted images, and the findings were sufficient to diagnose a parasitic larva, such as Ascaris. Subsequently, endoscopic retrograde cholangiopancreatography (ERCP) demonstrated a tubular filling defect in the dilated CBD (Figure 1E), and a linear, hyperechoic lesion with a central low-echoic area was seen on endoscopic ultrasound (EUS) (Figure 1F).
After removal by an endoscopic procedure, the lesion was found to be a tubular-shaped CBD stone (Figure 1G).
The final diagnosis was CBD stone.
The patient was treated with antibiotics for three days and was discharged without any complications (Figure 2).
Subsequent follow-up blood tests conducted at an outpatient clinic showed gradual decrease in the abnormal liver function test values.
Unless it is radiolucent, a CBD stone is not difficult to diagnose on CT. Biliary stones can appear in various attenuations on CT, and only about 20% show high attenuation[5]. Most biliary stones are either round or amorphous-shaped. In addition to the imaging findings from the biliary stone itself, low attenuated bile surrounding the stone and associated ductal dilatation or narrowing can improve the likelihood of correct diagnosis of biliary stone[5]. In addition, a signal void in the CBD or a fluid level with low signal intensity in the dependent portion of the CBD on MR imaging can suggest a CBD stone[6]. Even though ERCP is an invasive procedure, it has the benefit of simultaneous diagnosis and treatment[7]. Moreover, EUS has excellent diagnostic ability when it is performed with ERCP, and a biliary stone can be characteristically seen as a hyperechoic lesion accompanying a posterior acoustic shadow in the CBD on EUS[8,9].
On the other hand, Ascaris can appear as an elongated, high-density structure in the biliary tree on CT, although this modality is only used as complementary for diagnosis[6]. On MR cholangiogram, Ascaris demonstrates a “double-tube” appearance, a hypointense tubular defect inside the CBD with central hyperintense material representing the fluid-filled gut of the worm[10]. On ERCP, the worm is seen as an intraductal filling defect with motility in the bile duct[4,11]. The difference between CBD stone and Ascaris is even more obvious on EUS, in which the parasite appears as a spherical-shaped hyperechogenic lesion without posterior acoustic shadowing[12].
To the best of our knowledge, there has been only one case report of CBD stone mimicking Ascaris lumbricoides, and the report only described the sonographic findings[11]. Thus, it is not thought to be difficult to distinguish CBD stone from Ascaris infestation on imaging or clinical findings. Although they share radiologic findings of a non-enhancing high-density lesion on CT and a filling defect on T2-weighted images on MR, these two diseases rarely are part of the same differential diagnoses because their typical presentations are different. However, if these typical imaging features are not seen, differential diagnosis for tubular structures in the CBD could be confusing. Although we had never previously experienced an elongated-shaped CBD stone, we did experience an ascariasis patient who manifested similar imaging findings to the present case (Supplementary Figure 1).
In the present case, not only did the stone appear very similarly shaped to an Ascaris worm on CT and MR cholangiography, but it was also mistaken for Ascaris on EUS due to its elongated shape with a central hypoechoic area, rather than the nodular or angular appearance of a typical CBD stone. However, Ascaris could have been distinguished from a CBD stone in the present case by the relatively longer (15-49 cm) and thicker (2-6 mm in females)[13] body size of Ascaris compared to CBD stones, even if no motility was observed[14].
Although this was a rare case of CBD stone mimicking biliary ascariasis, it serves as a reminder that patients complaining of biliary colic or imaging finding of an elongated filling defect occupying the CBD should not be diagnosed by shape alone, and a CBD stone can mimic biliary Ascaris.
Although CBD stone and Ascaris are not commonly discussed in the same differential diagnosis, they can be confused in cases with an elongated CBD stone.
| 1. | Tazuma S. Gallstone disease: Epidemiology, pathogenesis, and classification of biliary stones (common bile duct and intrahepatic). Best Pract Res Clin Gastroenterol. 2006;20:1075-1083. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 262] [Cited by in RCA: 317] [Article Influence: 15.9] [Reference Citation Analysis (2)] |
| 2. | Yeh BM, Liu PS, Soto JA, Corvera CA, Hussain HK. MR imaging and CT of the biliary tract. Radiographics. 2009;29:1669-1688. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 106] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 3. | Lim JH, Kim SY, Park CM. Parasitic diseases of the biliary tract. AJR Am J Roentgenol. 2007;188:1596-1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 36] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Das AK. Hepatic and biliary ascariasis. J Glob Infect Dis. 2014;6:65-72. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 62] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Miller FH, Hwang CM, Gabriel H, Goodhartz LA, Omar AJ, Parsons WG. Contrast-enhanced helical CT of choledocholithiasis. AJR Am J Roentgenol. 2003;181:125-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Das CJ, Kumar J, Debnath J, Chaudhry A. Imaging of ascariasis. Australas Radiol. 2007;51:500-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 35] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Fulcher AS. MRCP and ERCP in the diagnosis of common bile duct stones. Gastrointest Endosc. 2002;56:S178-S182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Petrov MS, Savides TJ. Systematic review of endoscopic ultrasonography versus endoscopic retrograde cholangiopancreatography for suspected choledocholithiasis. Br J Surg. 2009;96:967-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 9. | Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, Yamamoto N, Hirano K, Komatsu Y, Tada M, Yoshida H, Kawabe T, Ohtomo K, Omata M. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271-275. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 148] [Cited by in RCA: 141] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 10. | Ng KK, Wong HF, Kong MS, Chiu LC, Tan CF, Wan YL. Biliary ascariasis: CT, MR cholangiopancreatography, and navigator endoscopic appearance--report of a case of acute biliary obstruction. Abdom Imaging. 1999;24:470-472. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 17] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Misra SP, Awasthy DN, Dwivedi M. Choledocholithiasis mimicking Ascaris lumbricoides: problem in ultrasound differential diagnosis. Trop Doct. 1999;29:110-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Sharma M, Somani P. EUS of pancreatic ascariasis. Arab J Gastroenterol. 2018;19:47-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Roberts LS, Janovy, Jr J. Foundations of parasitology. Foundations of parasitology. 8th ed. Boston, MA: McGraw-Hill, 2008. |
| 14. | Dold C, Holland CV. Ascaris and ascariasis. Microbes Infect. 2011;13:632-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 161] [Cited by in RCA: 170] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Geramizadeh B S-Editor: Yan JP L-Editor: A P-Editor: Liu JH