Published online Oct 6, 2020. doi: 10.12998/wjcc.v8.i19.4349
Peer-review started: June 18, 2020
First decision: July 24, 2020
Revised: August 5, 2020
Accepted: September 2, 2020
Article in press: September 2, 2020
Published online: October 6, 2020
Processing time: 101 Days and 10.7 Hours
Coronavirus disease 19 (COVID-19) is a global pandemic and has had a profound impact on our routine surgical activities. Acute appendicitis is the most common abdominal emergency worldwide. Therefore, it is highly essential to assess the influence the pandemic has on acute appendicitis.
To assess the efficacy of the management of acute appendicitis during the COVID-19 pandemic.
We retrospectively analyzed 90 patients who presented with acute appendicitis during the outbreak of COVID-19 in Jiaxing, China. Clinical data regarding appendectomies patients were also collected for the corresponding time frame from 2019. Preoperative management, intraoperative protective measures, and postoperative management were conducted.
After screening, six patients were identified as unqualified due to fever and were then referred to the COVID-19 expert group. The results of the nucleic acid test were negative. Of the 76 patients enrolled in the simple group, nine patients received medication therapy, and all others underwent surgery. From this same group, 66 patients were diagnosed with suppurative appendicitis, and one patient was diagnosed with perforated appendicitis after surgery. There were 14 patients in the complex group, for which the postoperative diagnosis indicated perforated appendicitis. The proportion of men with perforated appendicitis was higher than that in 2019 (P < 0.05). The chief complaint duration for perforated appendicitis patients in 2020 was longer than that in 2019 (P < 0.05). The routine blood test showed that white blood cell counts and neutrophil ratios were higher in perforated appendicitis patients in 2020 than in 2019 (P < 0.05). The ratio of open appendectomies to the amount of mean blood loss during surgery was greater in 2020 than in 2019 (P < 0.05). Online consultation after discharge was selected in 59 cases (65.6%). No perioperative infection with COVID-19 or long-term postoperative complications were found.
The management of acute appendicitis from Jiaxing effectively reduced the influence of the pandemic and minimized the risk of nosocomial infection.
Core Tip: This retrospective study evaluated the efficacy of the management of acute appendicitis during the coronavirus disease 19 (COVID-19) pandemic. Emergency preoperative management included appendicitis evaluation and COVID-19 screening. Our research showed that the number of perforated appendicitis with longer chief complaint duration was higher than last year. The shunt used in the simple and complex groups not only supplied appropriate treatment but also reduced the pressure for emergency surgery preparation. Laparoscopic appendectomy was recommended if COVID-19 screening results were negative. No COVID-19 infection occurred. Our management effectively reduced the influence of the pandemic and minimized nosocomial infection risk.
- Citation: Zhou Y, Cen LS. Managing acute appendicitis during the COVID-19 pandemic in Jiaxing, China. World J Clin Cases 2020; 8(19): 4349-4359
- URL: https://www.wjgnet.com/2307-8960/full/v8/i19/4349.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i19.4349
Since the first confirmed case of novel coronavirus in Wuhan in December 2019, coronavirus disease 19 (COVID-19) has widely spread to other cities and countries. While most medical resources were allocated to treat COVID-19 patients, emergency surgeries still needed to be handled. The COVID-19 pandemic has had a profound impact on our routine surgical activities, especially when it comes to emergency surgery[1]. Acute appendicitis, with an estimated lifetime risk reported to be 7%-8%, is the most common abdominal emergency worldwide, and emergency appendectomy is one of the most commonly performed surgical procedures for all age groups[2]. Some patients complain of symptoms such as fever, vomiting, diarrhea, and abdominal pain, which are similar to COVID-19 gastrointestinal symptoms[3,4]. The diagnosis of acute appendicitis needs to be more carefully differentiated to avoid misdiagnosis. With the worldwide progress of the pandemic, we are facing unprecedented challenges in reducing nosocomial infection risks and minimizing the influence of the pandemic on both patients and surgeons.
Jiaxing is a medium-sized city located between Hangzhou and Shanghai in East China. As the only fixed-point hospital for COVID-19 patients in this region, The First Hospital of Jiaxing has had a total of 50 cases of COVID-19 since January 27, 2020. As non-infective specialists, it was a great challenge for surgeons to handle emergency surgeries that may involve COVID-19, especially during the early stages of the pandemic, when little was known about COVID-19. Effective emergency management strategies are essential for acute appendicitis. We retrospectively analyzed the clinical data of acute appendicitis patients admitted to The First Hospital of Jiaxing during the initial outbreak of COVID-19. Our experience will help other surgeons handle acute appendicitis emergencies during this and future pandemics.
This retrospective clinical study was conducted using data from 90 patients with acute appendicitis during the initial outbreak of COVID-19 in Jiaxing, China from January 27 to March 31, 2020. Informed consent was obtained from all participants. Clinical data regarding acute appendicitis from January 27 to March 31, 2019 were also collected. Our research was approved by the Ethics Committee of The First Hospital of Jiaxing.
The diagnosis of acute appendicitis was mainly based on clinical manifestations, routine blood tests, and ultrasound (US) or computed tomography (CT) scans. Exclusion criteria included: (1) Patients with a history of chronic appendicitis; (2) Incidental findings of appendicitis during other procedures; (3) Surgical contraindications including, acute myocardial infarction, blood coagulation disorders, and cardiopulmonary insufficiency; and (4) Refusal of surgery.
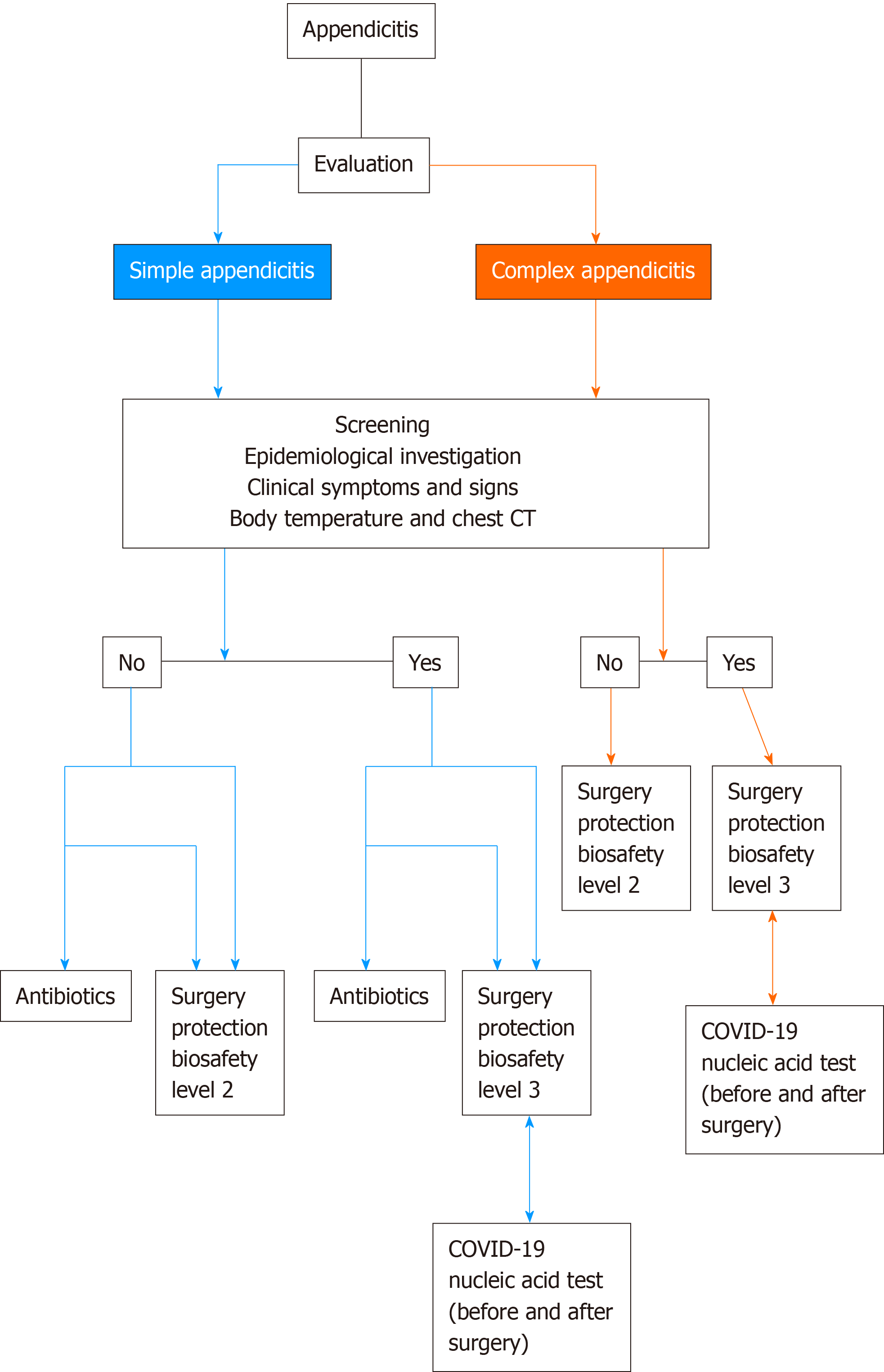
Emergency preoperative management: Emergency evaluation was conducted by trained emergency attendants and included an appendicitis evaluation and COVID-19 screening (Figure 1). Medical history, physical examination, and routine blood tests were also performed.
We preliminarily divided patients into two groups: Simple (non-perforated) and complex (gangrenous or perforated). All patients were asked to undergo either abdominal CT scan or US imaging. Patients with signs and symptoms of appendicitis along with an US- or CT-indicated perforation were enrolled in the complex group. The preparation time for surgery was less than 60 min. Patients diagnosed with appendicitis without perforation were enrolled in the simple group. These patients were prepared for surgery or prescribed antibiotics based on the progression of the appendicitis and the patient’s choice. Patients who were prescribed antibiotics were closely monitored at the outpatient clinic. Patients were reexamined with routine blood tests and US or CT imaging if symptoms of the chief complaint persisted or worsened. The reevaluation interval time was less than 12 h. The preoperative assessment time was recorded.
COVID-19 screening was performed prior to admission. Epidemiological questions, such as history of exposure to COVID-19 patients or pandemic areas, were also asked. Clinical signs and symptoms of respiratory tract infection such as fever and cough were recorded. We also carefully identified gastrointestinal symptoms of COVID-19 and appendicitis. Body temperature was checked, and chest CT was performed prior to admission. The CT report was reviewed by two trained radiologists. Additionally, an abdominal CT scan was performed if the patient was highly suspected to have perforated appendicitis. If the results of the pre-admission COVID-19 screening were abnormal, we consulted an expert group for COVID-19, which was a newly built professional team during the pandemic for the sample, diagnosis, and treatment of COVID-19 patients. The expert group’s assessment would help us take appropriate measures for further treatment. Other preoperative tests were prepared as done previously. If COVID-19 was excluded, surgery was performed under secondary protection, as was done previously. If COVID-19 could not be excluded, surgery was performed with tertiary protection, without waiting for nucleic acid test results. The patient was temporarily placed in a special surgical ward singly before the nucleic acid test result was available. A nucleic acid test was required before and after surgery. If any of the two results were positive, the patient was admitted to a special negative pressure ward singly for the simultaneous treatment of COVID-19. If the result was negative, the patient was sent to the special surgical ward singly, and the nucleic acid test was repeated on the basis of the status of the illness. The test sample was selected using a nasopharyngeal test paper. The nucleic acid test was conducted using a novel coronavirus nucleic acid detection kit (Hunan Shengxiang Biotechnology Co. LTD, China), and the results were obtained after 6 h.
Intraoperative protective measures: Body temperature and epidemiological history were rechecked by a surgical nurse preoperatively. We opted to perform laparoscopic appendectomy under secondary protection if the COVID-19 screening was normal. Patients with suspected or confirmed COVID-19 were scheduled for surgery in the negative pressure operating room under tertiary protection. Most of the COVID-19 positive or suspected positive patients underwent an open appendectomy. The number of surgical assistants was controlled based on the type of surgery. Visitors were prohibited from entering the operation room.
Postoperative management: Postoperative fever was carefully monitored, and the expert group for COVID-19 was consulted if a suspicious case occurred. If patients could ingest liquids or semi-liquids without abdominal pain or fever, they were discharged with education regarding their stitches 5-7 d after surgery. The length of the hospital stay and cost were recorded.
Postoperative follow-up: All patients were required to attend a follow-up visit 2 wk after surgery. Online consultation via the internet or telephone was encouraged. Additionally, COVID-19 related symptoms were also investigated.
Statistical analysis: Statistical analysis was performed using t-test or Pearson’s chi-square test, and P values < 0.05 was considered statistically significant. The SPSS (version 17.0, Chicago, IL, NY, United States)) software program was used for the calculations. The statistical methods of this study were reviewed by Professor Chen Ling from the Zhejiang University of Finance and Economics.
Emergency preoperative screening was conducted for 90 patients with acute appendicitis during the initial outbreak period of COVID-19 (Table 1). There were 59 men and 31 women, with an average age of 42.9 years and a range of 3-80 years. Of the patients screened, 76 patients were enrolled in the simple group, of whom nine received medication therapy and all others underwent surgery. Of this group, 66 patients were diagnosed with suppurative appendicitis, and one patient presented with perforated appendicitis after surgery. There were 14 patients in the complex group, for which the postoperative diagnosis indicated perforated appendicitis. In total, six patients were identified as unqualified due to fever.
| Appendicitis type | Treatment, medical/surgery | Postoperative diagnosis, suppurative/perforated appendicitis | Unqualified total | Screening type | ||
| CT | Fever | Epidemiology | ||||
| Simple (76) | 9/67 | 66/1 | 5 | 0 | 5 | 0 |
| Complex (14) | 0/14 | 0/14 | 1 | 0 | 1 | 0 |
A total of six patients were referred to the COVID-19 expert group, and a total of six appendectomies were conducted under tertiary protection. The results of the nucleic acid test were negative, and there were no COVID-19-positive cases among the acute appendicitis patients. Assessment by the expert group revealed that four cases in simple group and one case in complex group were assessed as having intraperitoneal inflammation. One patient in simple group was considered as amygdalitis. After the surgery, all patients were transferred to a special surgical ward singly for follow-up treatments.
The number of surgeries was reduced in 2020 compared with 2019 (81 vs 121). The total ratio of males was higher than that for 2019 (P < 0.05). The ratio of perforated appendicitis cases was also higher than that for 2019. The proportion of males with perforated appendicitis was higher than that in 2019 (P < 0.05). There was no significant difference in age or regional distribution of patients or pediatric perforated appendicitis ratio between 2019 and 2020 (Table 2).
| Period | 2019 | 2020 | χ²/t | P value |
| Age in yr | 37.7 ± 19.8 | 40.9 ± 19.9 | 1.13 | 0.26 |
| Male/female | 63/58 | 54/27 | 4.244 | 0.039 |
| Children/adults | 19/102 | 12/69 | 0.029 | 0.864 |
| Local/nonlocal | 116/5 | 79/2 | 0.058 | 0.81 |
| Suppurative appendicitis, male/female | 58/53 | 40/26 | 1.169 | 0.28 |
| Perforated appendicitis, male/female | 5/5 | 14/1 | 6.343 | 0.012 |
| Suppurative/perforated pediatric appendicitis | 18/1 | 10/2 | 1.063 | 0.302 |
| Suppurative/perforated appendicitis | 111/10 | 66/15 | 4.704 | 0.03 |
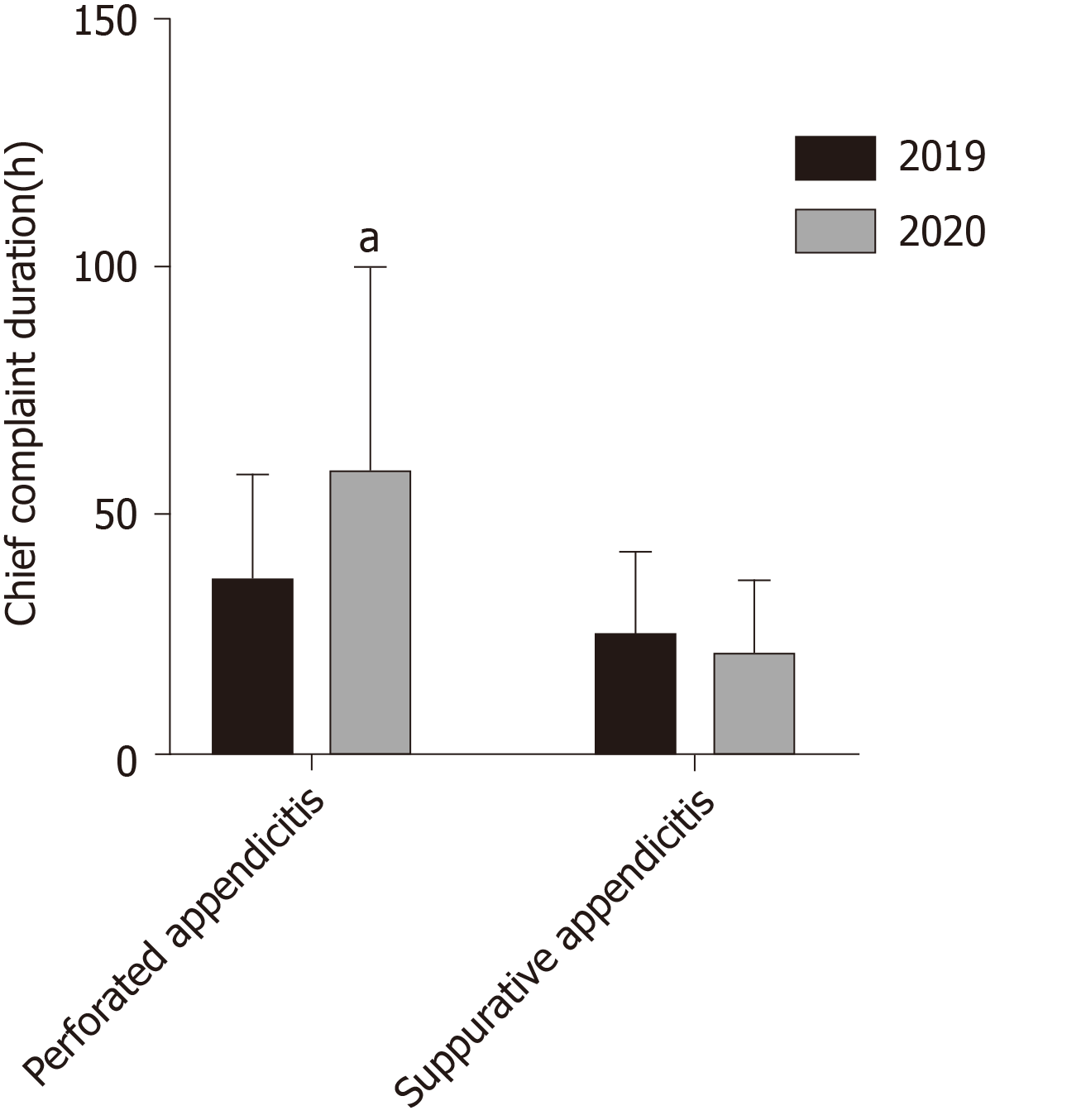
The chief complaint duration for perforated appendicitis patients in 2020 was longer than that for 2019 (63.0 ± 36.2 h vs 35.6 ± 23.8h, P < 0.05). The routine blood tests showed white blood cell counts (WBC) and neutrophil ratios were higher in perforated appendicitis patients in 2020 than in 2019 (13.5 × 109/L ± 3.9 × 109/L vs 9.8 × 109/L ± 4.8 × 109/L, P < 0.05; 89.3 ± 5.4% vs 83.3 ± 8.3%, P < 0.05). There were no significant differences in chief complaint duration, WBC count, or neutrophil ratio for suppurative appendicitis patients between 2019 and 2020 (22.5 ± 20.6 h vs 19.4 ± 16.8 h, 10.9 × 109/L ± 4.1 × 109/L vs 11.2 × 109/L ± 4.5 × 109/L, 80.2 ± 11.6% vs 80.7 ± 10.7%) (Figures 2-4).
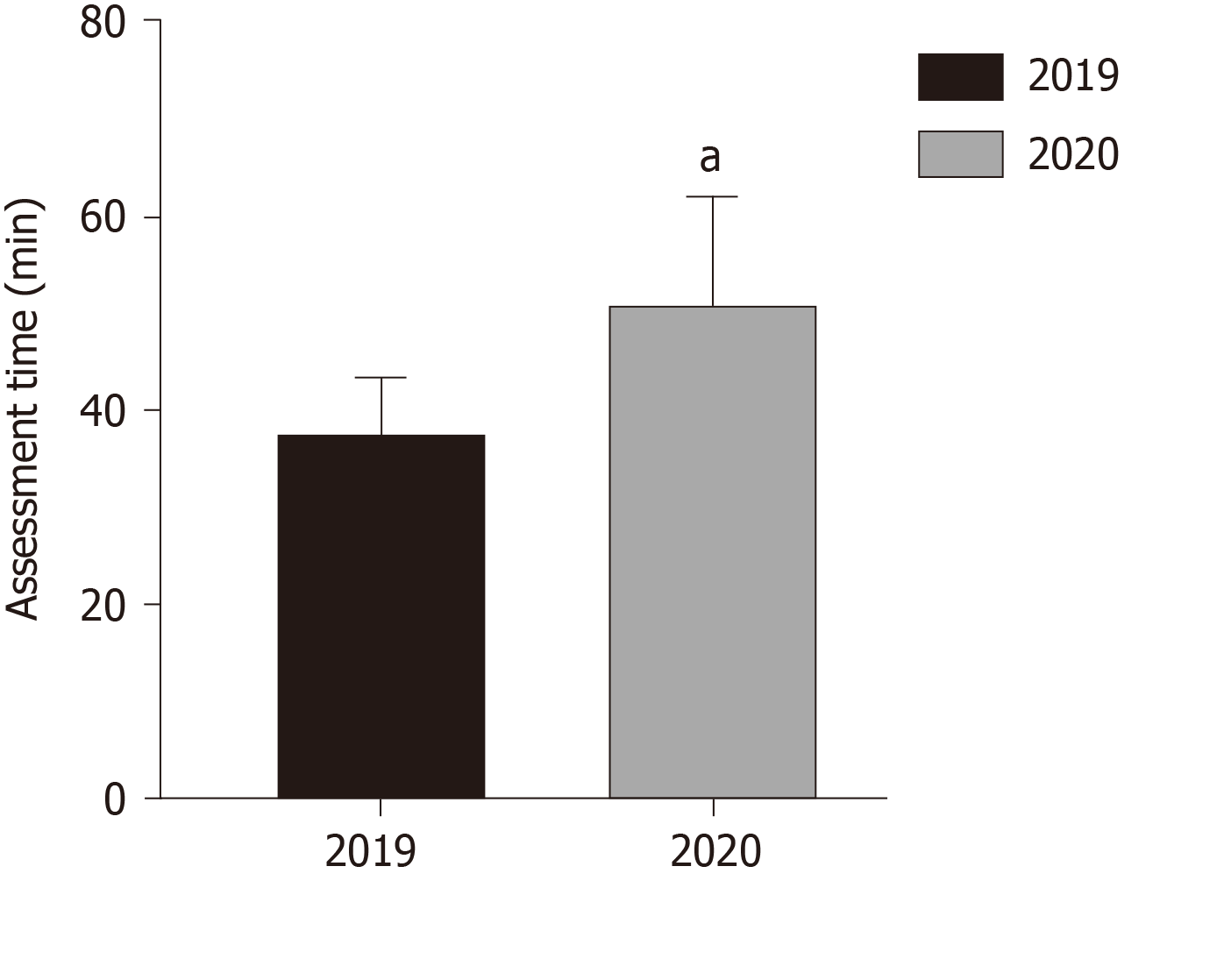
The emergency preoperative assessment time was longer in 2020 than in 2019 (53.9 ± 8.8 min vs 37.0 ± 8.5 min, P < 0.05) (Figure 5).
It was found that the ratio of open appendectomies and the amount of mean blood loss during surgery was greater in 2020 than in 2019 (12/69 vs 7/114, 14.9 ± 13.0 mL vs 11.5 ± 6.6 mL, P < 0.05). There were no significant differences in operating time and short-term complications between 2019 and 2020 (Table 3).
| Year | Cases, n | Surgical method, n, open/laparoscope | Operating time in h | Blood loss, mL | Short-term complications, yes/no |
| 2019 | 121 | 7/114 | 60.8 ± 22.0 | 11.5 ± 6.6 | 4/117 |
| 2020 | 81 | 12/69 | 61.3 ± 27.3 | 14.9 ± 13.0 | 3/78 |
| χ2/t | 4.643 | 0.137 | 2.396 | 0.000 | |
| P value | 0.031 | 0.891 | 0.017 | 1.000 |
There were no significant differences in hospital stay duration and cost between 2019 and 2020 (Table 4).
| Period | Cases, n | Hospital stay in d | Cost in RMB |
| 2019 | 121 | 5.4 ± 3.0 | 11196.4 ± 3685.0 |
| 2020 | 81 | 6.1 ± 3.7 | 11737.4 ± 5348.1 |
| T | 1.551 | 0.851 | |
| P | 0.122 | 0.396 |
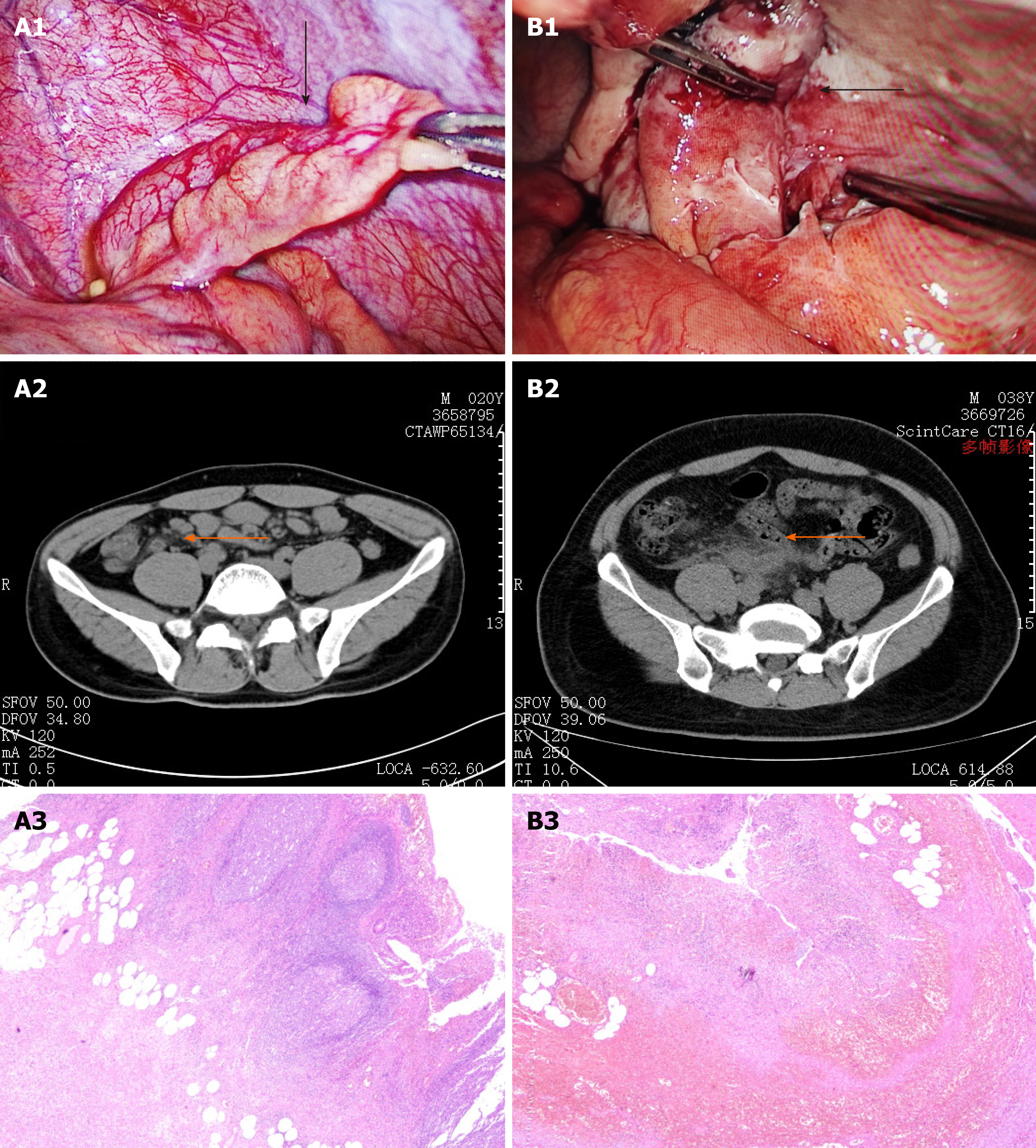
Figure 6 (A1, A2, A3) was selected from a 20-year-old male with chief complaint of abdominal pain for 4 h in February 2020. He was assigned to simple group, and postoperative diagnosis was suppurative appendicitis. Figure 6 (B1, B2, B3) was selected from a 38-year-old male with chief complaint of abdominal pain for 72 h in March 2020. He was assigned to complex group and postoperative diagnosis was perforated appendicitis.
A total of 90 patients were followed-up after discharge, of which 31 (34.4%) came to the hospital for reexamination or stitch removal 2 wk after surgery. The remaining 59 patients (65.6%) opted for an online consultation.
There were three cases with short-term complications. There was one case of surgical incision infection, one case of intraperitoneal infection, and one case of venous thrombosis of the lower limbs. All three patients recovered after a timely treatment. There were no long-term complications in these cases. No COVID-19 infection occurred.
In the early stage of the COVID-19 pandemic, acute appendicitis was more common in men, and the proportion of perforated appendicitis was higher in our research. Men were reported more often with perforated appendicitis[5], which is consistent with the conclusion of our study. Chinese people often return to their hometown during the Spring Festival holiday, so appendicitis patients in this area are mainly local residents during February and March. Holiday and traffic restrictions may be reasons for the declined number of appendicitis patients. The significant decrease in the number of appendicitis patients was also found in other cities such as Jerusalem, Israel[6], where there is no holiday or traffic restriction. Patients’ willingness to go out and see a doctor was also affected by the pandemic[7]. This could be a main reason for declined number of appendicitis cases, because the incidence of acute appendicitis itself should not be affected by an outbreak of respiratory disease. Some patients with mild symptoms may have achieved relief by taking pills themselves. However, most patients should be treated under physician supervision, as delayed medical treatment can aggravate appendicitis progression[8]. Our research shows that the chief complaint duration for perforated appendicitis patients was longer, accompanied by a higher WBC count and neutrophil ratio. It has been noted that diagnosis was delayed and there were higher complication rates in pediatric appendicitis cases during the COVID-19 outbreak[9]. Our results show no significant differences of pediatric perforated appendicitis ratio between 2019 and 2020. One of the main reasons is that local parents tend to go to children's hospitals for surgery. Nonetheless, we should pay more attention to patients, especially children and males with prolonged symptoms during the COVID-19 pandemic, since delay in diagnosis and treatment may become as big threat as COVID-19 itself.
The accuracy of a surgeon’s judgment regarding the surgical indications of appendicitis may be influenced by the COVID-19 pandemic. When major supplies and personnel were diverted to departments, such as the intensive care unit, infection prevention, and pulmonology for COVID-19 treatment, the other hospital departments inevitably faced difficulties, such as a shortage of protective equipment, a lack of isolation wards, and a shortage of available medical staff[10]. Sometimes, it is difficult to differentiate between the inflamed and perforated appendix based on abdominal palpation, while it has been proven that US and CT imaging are very useful in the early and accurate diagnosis of perforated appendicitis[2]. The postoperative diagnosis was most often consistent with the preoperative assessment in our complex group, and only one case of perforated appendicitis occurred in the simple group. Besides, surgeons are inclined to select a conservative approach during pandemic[11]. We agree with Collard et al[12] that the non-surgical treatment was the preferred alternative for adults with simple acute appendicitis during the initial stage of the COVID-19 pandemic. However, a survey in Ireland[12] showed that 54% acute appendicitis patients in the conservative care group had on-going discomfort on follow-up post-discharge. Sixty-three percent would choose up-front appendicectomy if they could decide again. As the epidemic is becoming normalized, more specific measures for conservative treatment is required for better recovery, and timely re-evaluation is necessary for patients under conservative treatment.
Laparoscopic appendectomy has shown great advantages over open appendectomy for many aspects of postoperative rehabilitation such as postoperative pain, wound infection rate, hospital stay, and recovery time[13,14]. However, the virus may spread via surgical smoke emitted during laparoscopy of infected cases[15]. Our understanding of the process of viral transmission in surgery is limited especially during the early period of the pandemic. In February, we conducted three laparoscopic appendectomies on suspected COVID-19 patients using tertiary protection. We opted to perform open appendectomies during the later stage of this research for patients with abnormal COVID-19 screening results. The ratio of open appendectomies was higher this year, and therefore, the amount of blood loss increased due to the surgical method. In addition, the higher proportion of perforated appendicitis was also an important cause of increased blood loss. Although surgeons suffered intense physical and mental pressure, our study showed the quality of surgical practice was not degraded during the COVID-19 pandemic. The limitation of our study was that there was no evidence of surgery being performed on any COVID-19 positive patients.
Telemedicine follow-up was more convenient for patients and also reduced the risk of human-to-human transmission; therefore, follow-up via the internet or telephone was encouraged. Psychological counseling was widely necessary during the pandemic[16]. Online consultation during a relatively free time could relieve the patients’ anxiety, and it was a substitute for the traditional face-to-face follow-up. In our research, 65.6% of the patients chose an online follow-up, and only three cases with short-term complications occurred.
Our management of acute appendicitis was a coping strategy in the early stages of the pandemic when little was known about COVID-19. In addition, our effective perioperative management was based on the strict control of relevant populations of COVID-19 patients by local disease control and prevention centers[17]. The delay in care and challenges we all are facing are not only in emergency surgeries but also in other health care specialties like cancer[18], dialysis dependent end-stage renal disease[19], hematopoietic stem cell transplantation[20], etc. We should make our clinical management compatible with the challenges and threats of this pandemic while trying to achieve the optimal therapeutic effect.
The management of acute appendicitis from Jiaxing effectively reduced the influence of the pandemic and minimized nosocomial infection risk.
At present, coronavirus disease 19 (COVID-19) has profoundly influenced our routine surgical activities. How to handle acute appendicitis emergencies during this and future pandemics is emerging as an urgent issue.
There have been rare reports about acute appendicitis emergencies during COVID-19 pandemics. Our experience will help other surgeons or physicians choose ideal treatments for other emergencies or delays.
To assess the efficacy of the management of acute appendicitis during the COVID-19 pandemic.
We retrospectively analyzed the clinical data of acute appendicitis patients admitted to The First Hospital of Jiaxing during the initial outbreak of COVID-19. Clinical data were also collected for the corresponding time frame from 2019. Preoperative management, intraoperative protective measures, and postoperative management data were conducted.
After screening, six patients were identified as unqualified due to fever, and their results of nucleic acid test were negative. Seventy-six patients were enrolled in the simple group, and 14 patients were enrolled in the complex group. The proportion of men with perforated appendicitis was higher in 2020 than that in 2019. The chief complaint duration for perforated appendicitis patients in 2020 was longer than that in 2019. The routine blood test showed white blood cell counts and neutrophil ratios were higher in perforated appendicitis patients in 2020 than in 2019. The ratio of open appendectomies to the amount of mean blood loss during surgery was greater in 2020 than in 2019. Online consultation after discharge was selected in 59 cases. No perioperative infection with COVID-19 or long-term postoperative complications were found.
The management of acute appendicitis from Jiaxing effectively reduced the influence of the pandemic and minimized the risk of nosocomial infection.
The delay in care and challenges we all are facing are not only in emergency surgeries but also in other health care specialties. We should make our clinical management compatible with the challenges and threats of this pandemic while trying to achieve the optimal therapeutic effect.
| 1. | Cheeyandira A. The effects of COVID-19 pandemic on the provision of urgent surgery: a perspective from the USA. J Surg Case Rep. 2020;2020:rjaa109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 15] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 2. | Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278-1287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 535] [Cited by in RCA: 750] [Article Influence: 68.2] [Reference Citation Analysis (1)] |
| 3. | Cholankeril G, Podboy A, Aivaliotis VI, Tarlow B, Pham EA, Spencer SP, Kim D, Hsing A, Ahmed A. High Prevalence of Concurrent Gastrointestinal Manifestations in Patients With Severe Acute Respiratory Syndrome Coronavirus 2: Early Experience From California. Gastroenterology. 2020;159:775-777. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 166] [Article Influence: 27.7] [Reference Citation Analysis (0)] |
| 4. | Lin L, Jiang X, Zhang Z, Huang S, Zhang Z, Fang Z, Gu Z, Gao L, Shi H, Mai L, Liu Y, Lin X, Lai R, Yan Z, Li X, Shan H. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020;69:997-1001. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 630] [Cited by in RCA: 663] [Article Influence: 110.5] [Reference Citation Analysis (0)] |
| 5. | Marudanayagam R, Williams GT, Rees BI. Review of the pathological results of 2660 appendicectomy specimens. J Gastroenterol. 2006;41:745-749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 163] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 6. | Tankel J, Keinan A, Blich O, Koussa M, Helou B, Shay S, Zugayar D, Pikarsky A, Mazeh H, Spira R, Reissman P. The Decreasing Incidence of Acute Appendicitis During COVID-19: A Retrospective Multi-centre Study. World J Surg. 2020;44:2458-2463. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 7. | Slim K, Veziant J. Urgent digestive surgery, a collateral victim of the COVID-19 crisis? J Visc Surg. 2020;157:S5-S6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 8. | Westfall KM, Charles AG. Risk of Perforation in the Era of Nonemergent Management for Acute Appendicitis. Am Surg. 2019;85:1209-1212. [PubMed] |
| 9. | Snapiri O, Rosenberg Danziger C, Krause I, Kravarusic D, Yulevich A, Balla U, Bilavsky E. Delayed diagnosis of paediatric appendicitis during the COVID-19 pandemic. Acta Paediatr. 2020;109:1672-1676. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 129] [Article Influence: 21.5] [Reference Citation Analysis (0)] |
| 10. | Giorgi PD, Villa F, Gallazzi E, Debernardi A, Schirò GR, Crisà FM, Talamonti G, D'Aliberti G. The management of emergency spinal surgery during the COVID-19 pandemic in Italy. Bone Joint J. 2020;102-B:671-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 51] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 11. | Kelly ME, Murphy E, Bolger JC, Cahill RA. COVID-19 and the treatment of acute appendicitis in Ireland: a new era or short-term pivot? Colorectal Dis. 2020;22:648-649. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 12. | Collard M, Lakkis Z, Loriau J, Mege D, Sabbagh C, Lefevre JH, Maggiori L. Antibiotics alone as an alternative to appendectomy for uncomplicated acute appendicitis in adults: Changes in treatment modalities related to the COVID-19 health crisis. J Visc Surg. 2020;157:S33-S42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 13. | Jaschinski T, Mosch CG, Eikermann M, Neugebauer EA, Sauerland S. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2018;11:CD001546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 138] [Article Influence: 17.3] [Reference Citation Analysis (0)] |
| 14. | Wang D, Dong T, Shao Y, Gu T, Xu Y, Jiang Y. Laparoscopy versus open appendectomy for elderly patients, a meta-analysis and systematic review. BMC Surg. 2019;19:54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 15. | Vigneswaran Y, Prachand VN, Posner MC, Matthews JB, Hussain M. What Is the Appropriate Use of Laparoscopy over Open Procedures in the Current COVID-19 Climate? J Gastrointest Surg. 2020;24:1686-1691. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 125] [Article Influence: 20.8] [Reference Citation Analysis (0)] |
| 16. | Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, Ho RC. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4551] [Cited by in RCA: 5177] [Article Influence: 862.8] [Reference Citation Analysis (1)] |
| 17. | Xiang B, Li P, Yang X, Zhong S, Manyande A, Feng M. The impact of novel coronavirus SARS-CoV-2 among healthcare workers in hospitals: An aerial overview. Am J Infect Control. 2020;48:915-917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 40] [Cited by in RCA: 37] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 18. | Jindal V, Sahu KK, Gaikazian S, Siddiqui AD, Jaiyesimi I. Cancer treatment during COVID-19 pandemic. Med Oncol. 2020;37:58. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 19. | Shen Q, Wang M, Che R, Li Q, Zhou J, Wang F, Shen Y, Ding J, Huang S, Yap HK, Warady BA, Xu H, Zhang A; Chinese Society of Pediatric Nephrology and Chinese Medical Doctor Association of Pediatric Nephrology. Consensus recommendations for the care of children receiving chronic dialysis in association with the COVID-19 epidemic. Pediatr Nephrol. 2020;35:1351-1357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Sahu KK, Siddiqui AD, Cerny J. COVID-19 pandemic and impact on hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 20] [Cited by in RCA: 31] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Invited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Cure E, Sahu KK S-Editor: Huang P L-Editor: Filipodia P-Editor: Xing YX