Published online Sep 26, 2020. doi: 10.12998/wjcc.v8.i18.4266
Peer-review started: April 8, 2020
First decision: April 22, 2020
Revised: July 20, 2020
Accepted: July 30, 2020
Article in press: July 30, 2020
Published online: September 26, 2020
Processing time: 166 Days and 15.1 Hours
Cardiac resynchronization therapy (CRT) is a well-established therapy for patients with cardiomyopathy.
The patient underwent left bundle branch area and left ventricular (reaching the left ventricular lateral vein through the coronary sinus) pacing. The optimal CRT was performed under the right bundle branch of the patient by adjusting the optimal a-v and v-v interphases to achieve the maximal benefit of the treatment.
The patient was diagnosed with left bundle branch block and heart failure. A left bundle branch area pacemaker assisted in correcting the complete left bundle branch block. However, the shorter QRS wave shape after pacemaker implantation through the left bundle branch area indicated a complete right bundle branch block pattern. Hence, the left bundle branch area pacemaker is not always considered as the optimal treatment. The left bundle branch pacing with the optimization of cardiac resynchronization treatment may serve as a new CRT strategy.
Core Tip: The traditional cardiac resynchronization therapy (CRT) method was not employed; rather the left bundle branch region was used for pacing. Then, the coronal sinus left ventricular wire was combined with the right bundle branch to fuse the down transmission, which significantly narrowed the electrocardiogram QRS and achieved the optimal effect of CRT.
- Citation: Zhang DH, Lang MJ, Tang G, Chen XX, Li HF. Left bundle branch pacing with optimization of cardiac resynchronization treatment: A case report. World J Clin Cases 2020; 8(18): 4266-4271
- URL: https://www.wjgnet.com/2307-8960/full/v8/i18/4266.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i18.4266
The main treatment methods for patients with chronic heart failure include medication therapy and device therapy. Cardiac resynchronization therapy (CRT) can obviously reduce the hospitalization rate and mortality for patients with heart failure combined with complete left bundle branch block. However, nearly a third of the patients undergoing CRT with the traditional double ventricular pacing do not show any improvement. Thus, the traditional dual-chamber pacing may not be the best way for CRT. The left bundle branch pacing can work together with the coronal sinus left ventricular wire, thus making the left and right ventricles more synchronized and the QRS duration more shortened. Herein, we report a case of left bundle branch pacing with the optimization of CRT.
A 63-year-old female patient had repeated experiences of heart fatigue and shortness of breath after activities in the last 3 years. She had no symptoms of syncope, blackness, chest tightness, or chest pain.
The patient was admitted to the hospital due to the aggravation of heart fatigue and tightness of breath.
The patient had no medical history.
The physical examination results revealed blood pressure of 98/62 mm Hg, enlarged heart border on the left lower side, heart rate of 70 times/min, dull heart tone, and 2/6 systolic blowing murmur.
The N-terminal pro-B-type natriuretic peptide level was 2600 pg/mL.
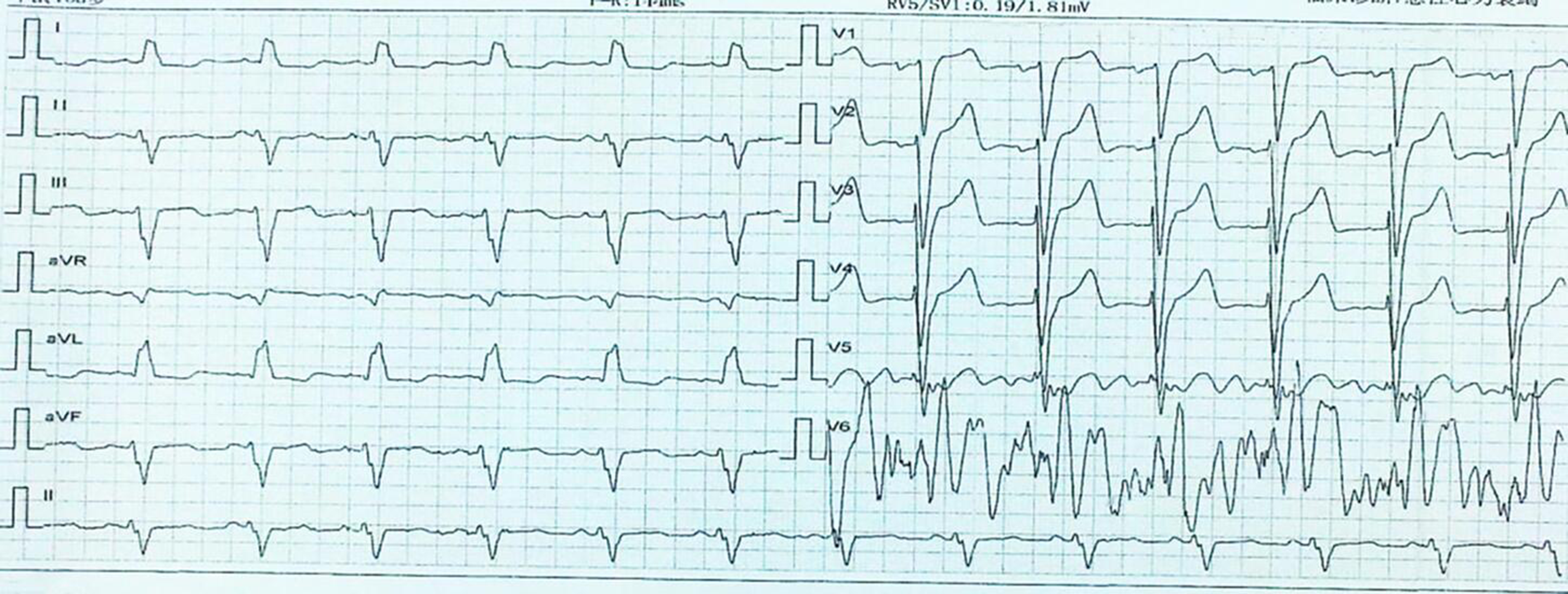
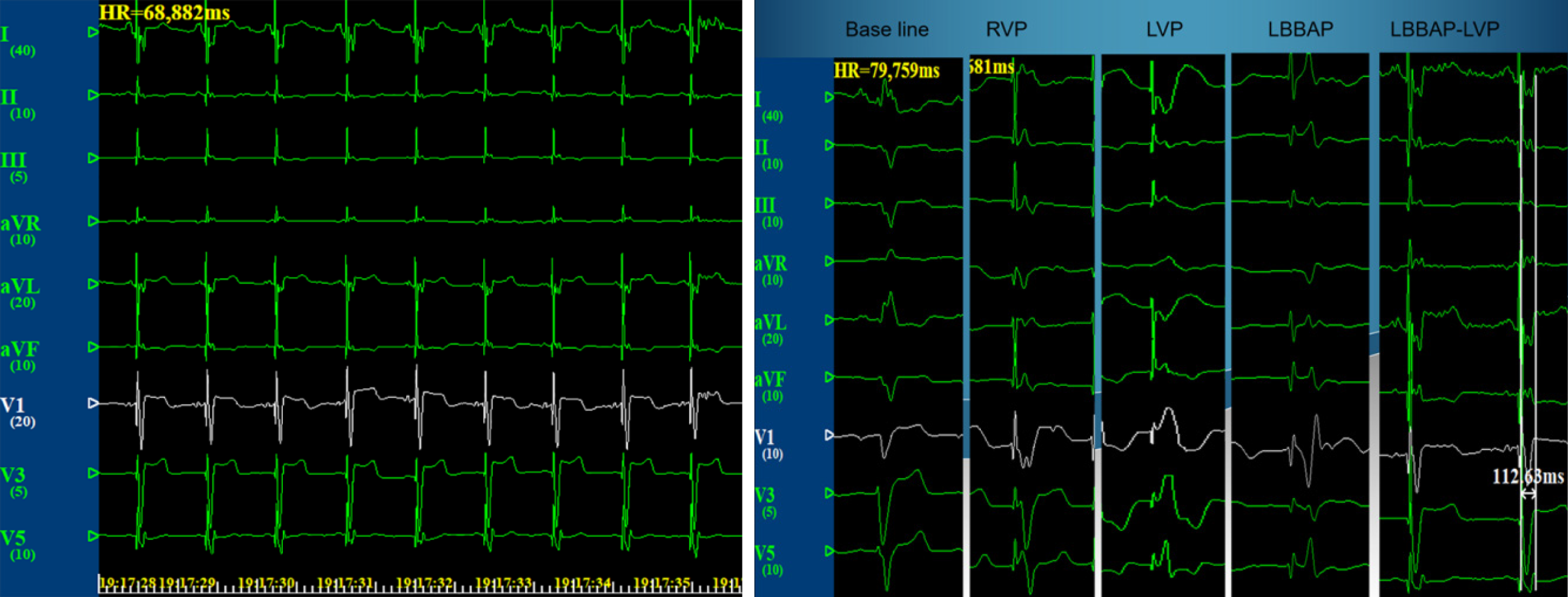
The electrocardiogram (ECG) results showed sinus rhythm, complete left bundle branch block, and QRS duration of 160 ms (Figure 1). Color Doppler ultrasound revealed a left atrial diameter of 45 mm, left ventricular diastolic diameter of 73 mm, and left ventricular ejection fraction of 21%. Coronary angiography results revealed no obvious stenosis in the left and right coronary arteries.
The patient was diagnosed with dilated cardiomyopathy New York Heart Association (NYHA) cardiac function level III, and therefore CRT (model C2TR01, Medtronic, United States) was performed.
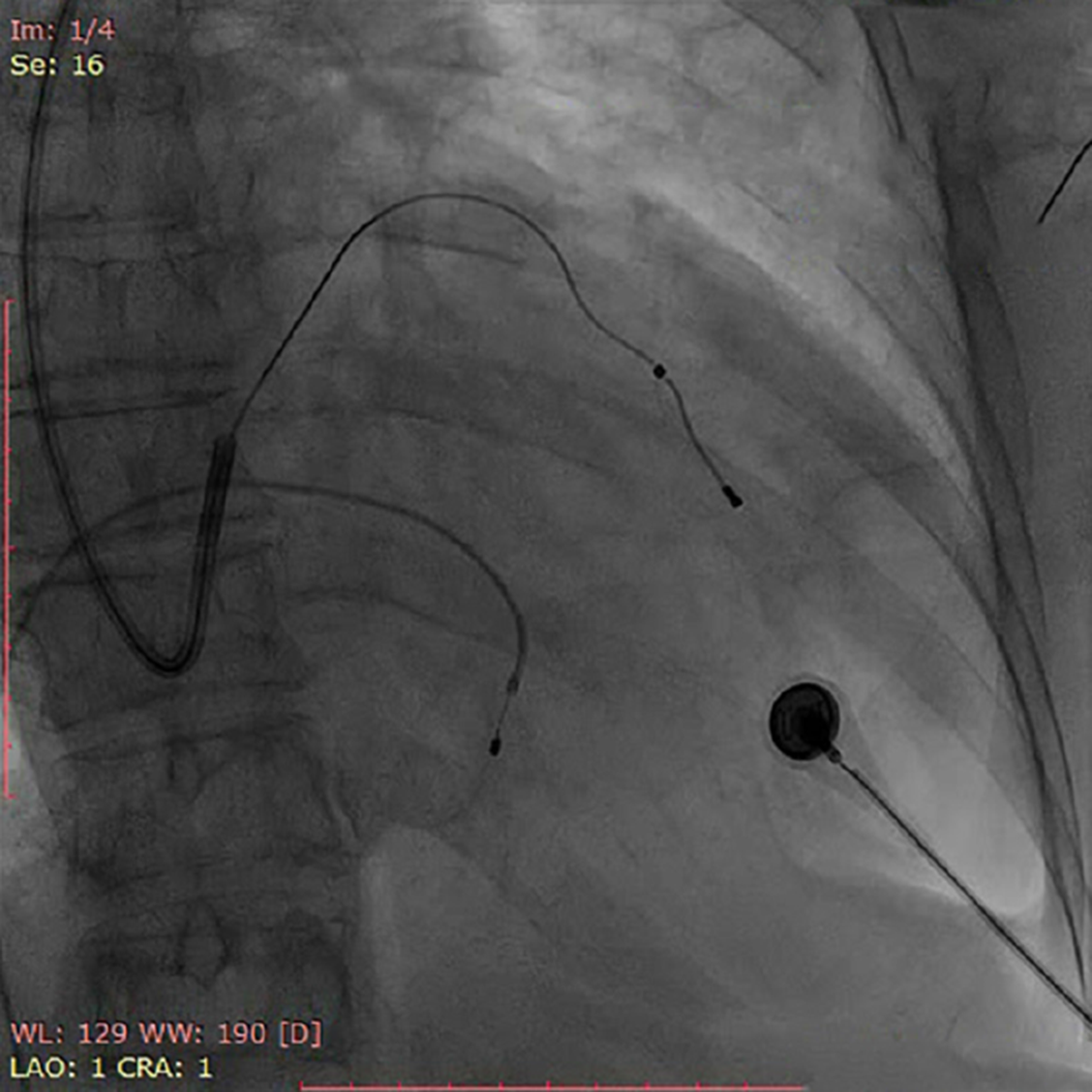
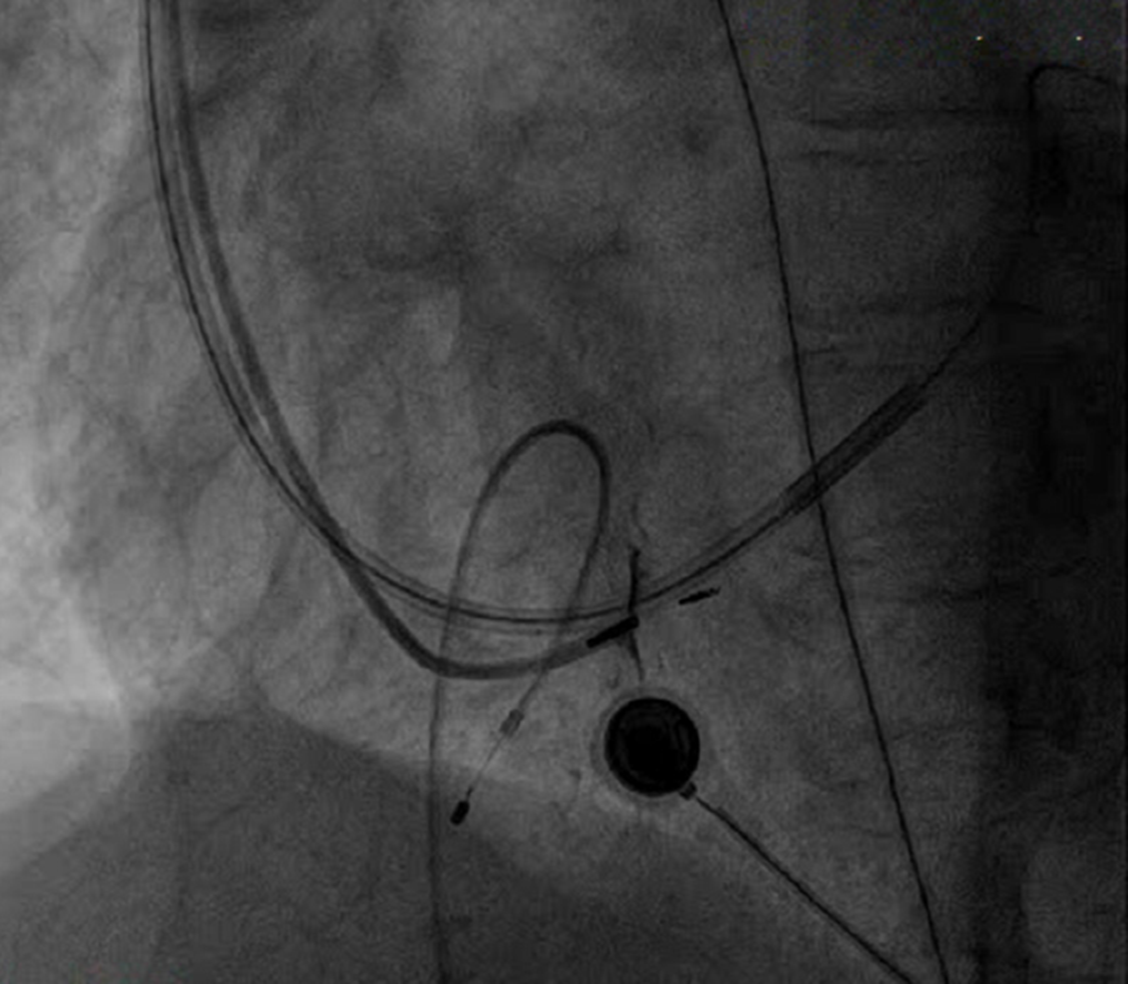
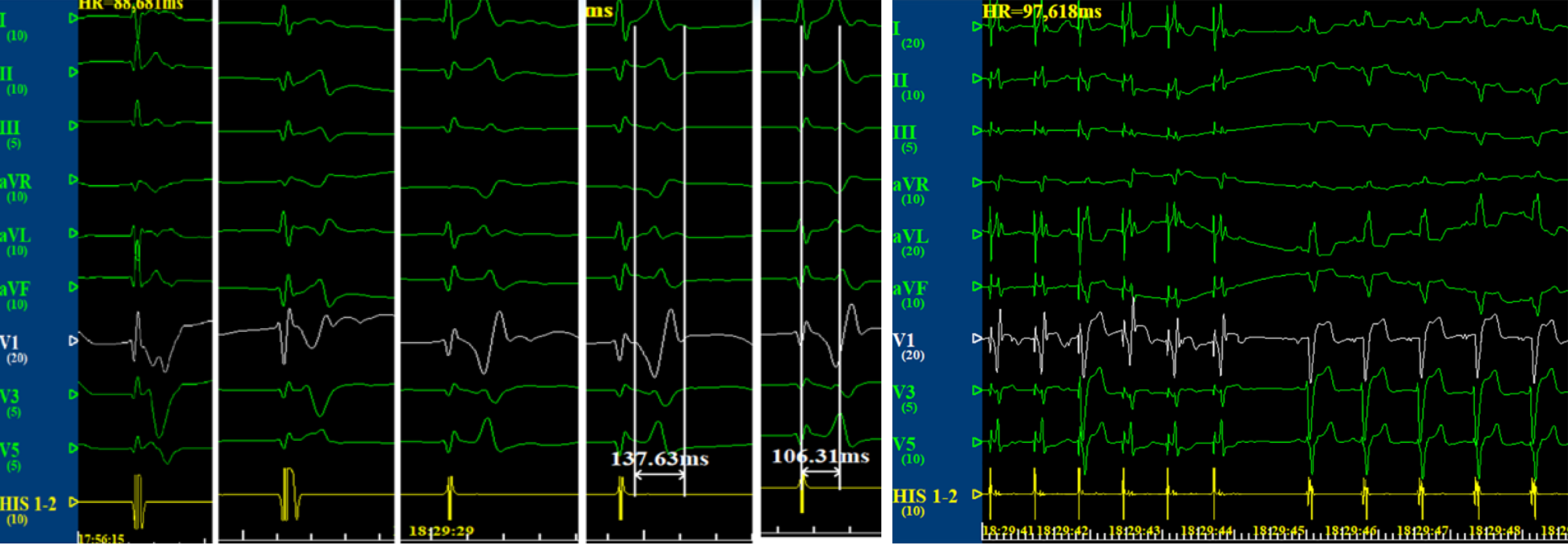
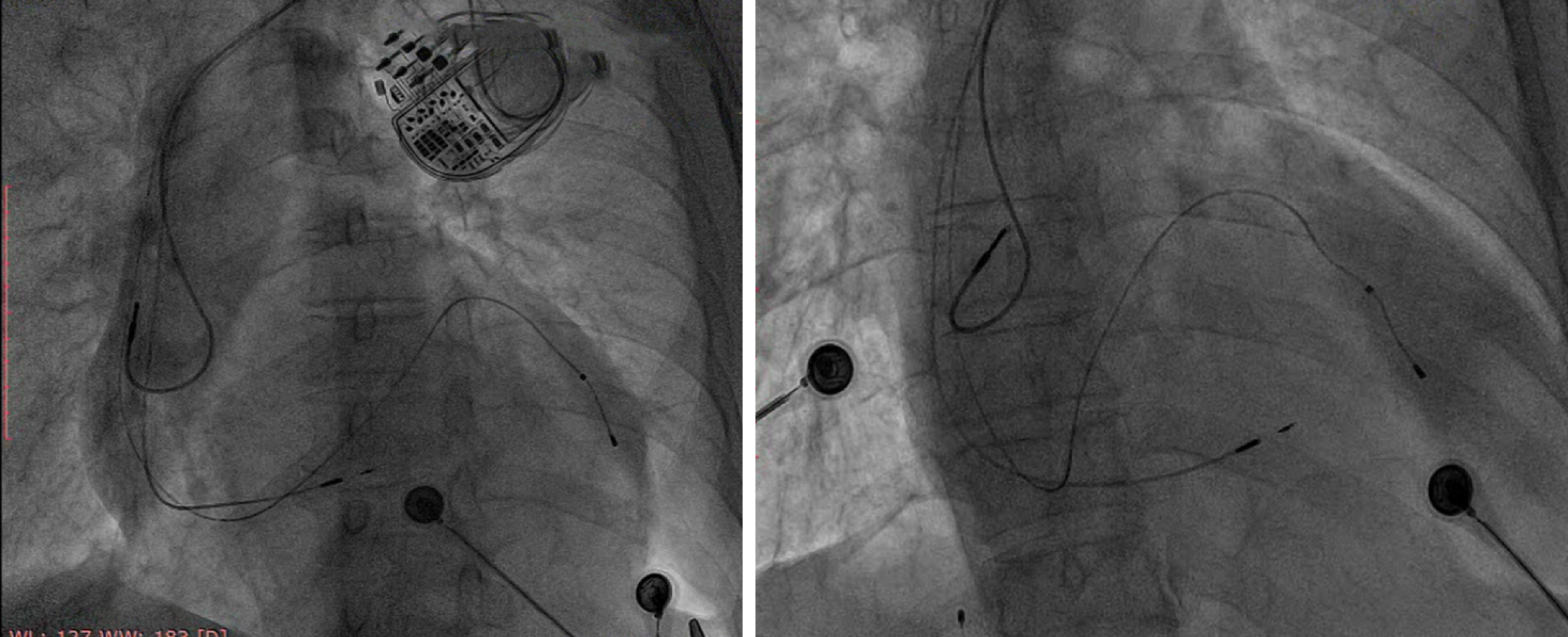
The left bundle branch pacing with the optimization of CRT was adopted. The left axillary vein was punctured during the surgery, and the pacemaker bag was successfully placed. This was followed by the introduction of a 10-stage electrophysiological catheter into the long sheath of the left ventricle via the coronary sinus. Coronary angiography was performed for choosing a left ventricular lateral vein as the target vessel[1]. A Medtronic 4296 left ventricular electrode was used to guide the filament along the percutaneous transluminal coronary angioplasty finger into the anterior coronary sinus. The lateral wall of the left ventricle was successfully paced (Figure 2), with a pacing threshold of 0.8 V, diaphragmatic muscle stimulation of 10 V, and application of Medtronic 3830 electrodes with C315HIS long sheath. The electrodes were placed across the tricuspid valve for about 1.5-cm interval as the implant site in the left bundle branch area. Then, the Medtronic 3830 pacing lead was screwed. Multi-body fluoroscopy was used, and the left bundle branch was paced after two to four turns of the lead screw. The ECG showed a complete left bundle branch block pattern, namely, V1 as QS type, I and AVL QRS wave of >120 ms, a notch on the top, output voltage of 1.5 V, pulse width of 0.4 ms, perception of 5.5 V, and impedance of 580 Ω. The findings indicated that the electrode was located in the right ventricular space. Further, the 3830 electrode penetrated into the interventricular septum (Figure 3). Multiple-lead QRS wave was observed, which was obviously narrowed to 120–138 ms. The pattern in lead V1 was suggestive of the presence of the right bundle branch block (Figure 4). This observation indicated that the electrode turned into the left bundle branch area of the His-Purkinje system, which was paced with an output voltage of 1.0 V, pulse width of 0.4 ms, perception of 10.0 V, and impedance of 960 Ω. The pacemaker threshold, impedance, and perception parameters were monitored repeatedly during the surgery. The orderly implanted atrial electrodes were tested, revealing good test parameters. The outer sheath of electrode C315 in the left bundle branch, the electrode connected to the right ventricular jack, and the atrial electrode connected to the atrial socket were removed, and the bag was sutured with the pacing threshold of 1.2 V, perception of 3 V, and impedance of 780 Ω[2]. The pacemaker after the surgery was programmed by adjusting atrioventricular (AV) delay and VV interphase for fusing the left bundle branch area electrode and the left ventricular electrode with the right bundle branch, and then transmitted down to achieve the narrowest QRS wave graph (Figure 5A). Compared with the initial ECG, the QRS wave showed significant narrowing (Figure 5B), and the electrode position was observed through multiple postures (Figure 6).
The follow-up at 3 mo after the surgery showed that the patient's NYHA heart function was recovered to level II, with good pacing threshold, perceived impedance, and perceived parameters of atrial electrode, left bundle branch area electrode, and left ventricular electrode.
CRT is a therapy used for treating cardiomyopathy, heart failure, and left bundle branch block[3]. The self-conscious symptoms, exercise tolerance, and quality of life of patients with heart failure can be improved by enhancing the cardiac atrioventricular, interventricular, and left ventricular movement in coordination and improving the hemodynamics. Long-term treatment can reverse left ventricular remodeling, thus significantly reducing hospitalization and mortality in patients with heart failure. About 30% of patients undergoing conventional CRT showed no response due to the following reasons: (1) Improper position of the left ventricular electrode; (2) Advanced heart failure; (3) Left ventricular free wall with a transmural myocardial infarction; and (4) Mild ventricular dyssynchrony[4]. Vijayaraman et al[5] achieved satisfactory clinical results, including clinical prognosis and ultrasonic findings, using His-optimized CRT. However, the stability and perception of the electrode remained poor, and the technical requirements were high, with certain risks of short- and long-term electrode dislocation[6]. Therefore, the left bundle branch pacing with the optimization of CRT may serve as a potential CRT strategy.
The left bundle branch area pacemaker assists in correcting the complete left bundle branch block partly, which then cooperates with the coronary sinus left ventricular pacing lead. By adjusting the optimal AV delay and VV interphase, the electrode in the region of the left bundle branch and the electrode in the left ventricle were fused with the right bundle branch to produce a narrower QRS. This was considered as an independent predictor of the effectiveness of treatment[7] and helped in maximizing electric resynchronization and improving the prognosis of patients with heart failure. In this study, the effect of CRT was achieved in a patient with dilated cardiomyopathy and class III NYHA cardiac function. By adjusting the AV delay to 130 ms, the QRS wave was reduced to 110 ms using the two-chamber pacing fusion technique with the right bundle branch to fuse the down transmission. The patient was followed 3 mo postoperatively. The results showed that the patient's NYHA cardiac function recovered to level II, and she had good pacing threshold, perceived impedance, and perceived parameters of atrial electrode, left bundle branch area electrode, and left ventricular electrode. The patient was followed for only a few months. Longer follow-ups are needed to observe electrode stability and clinical improvement.
| 1. | Cheng XL, Huang QL, Zhang J. Clinical application of percutaneous axillary vein puncture technique in the implantation of permanent pacemaker. Zhongwai Yiliao Zazhi. 2017;28:115-117. [DOI] [Full Text] |
| 2. | Feng XF, Yu Y, Zhao Y, Lu QF, Li YG. Experience report of single center pacing in the region of left bundle branch via right axillary vein route. Zhonghua Xinlv Shichangxue Zazhi. 2019;23:96-101. [DOI] [Full Text] |
| 3. | McMurray JJ, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V, Filippatos G, Fonseca C, Gomez-Sanchez MA, Jaarsma T, Køber L, Lip GY, Maggioni AP, Parkhomenko A, Pieske BM, Popescu BA, Rønnevik PK, Rutten FH, Schwitter J, Seferovic P, Stepinska J, Trindade PT, Voors AA, Zannad F, Zeiher A; ESC Committee for Practice Guidelines. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2012;33:1787-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3411] [Cited by in RCA: 3589] [Article Influence: 256.4] [Reference Citation Analysis (0)] |
| 5. | Vijayaraman P, Herweg B, Ellenbogen KA, Gajek J. His-Optimized Cardiac Resynchronization Therapy to Maximize Electrical Resynchronization: A Feasibility Study. Circ Arrhythm Electrophysiol. 2019;12:e006934. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 145] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 6. | Lustgarten DL, Calame S, Crespo EM, Calame J, Lobel R, Spector PS. Electrical resynchronization induced by direct His-bundle pacing. Heart Rhythm. 2010;7:15-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 114] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Lecoq G, Leclercq C, Leray E, Crocq C, Alonso C, de Place C, Mabo P, Daubert C. Clinical and electrocardiographic predictors of a positive response to cardiac resynchronization therapy in advanced heart failure. Eur Heart J. 2005;26:1094-1100. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 186] [Article Influence: 8.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Zavras N S-Editor: Zhang L L-Editor: Wang TQ P-Editor: Xing YX