Published online Jul 26, 2020. doi: 10.12998/wjcc.v8.i14.3050
Peer-review started: April 3, 2020
First decision: April 22, 2020
Revised: May 1, 2020
Accepted: July 15, 2020
Article in press: July 15, 2020
Published online: July 26, 2020
Processing time: 112 Days and 4.5 Hours
Tumors located in the pylorus are technically more complex to resect by endoscopic resection, as the anatomical characteristics of this region can affect the adequate assessment of margins and performance of the procedure. We reported the results of underwater endoscopic mucosal resection (UEMR) of benign mucosal neoplasms located in the pyloric ring.
This case series describes 4 patients with 4 mucosal neoplasms located in the pyloric ring. The diameter of each neoplasm was less than 15 mm. We performed UEMR for the lesions. Water immersion enabled slight floating of the lesions, resulting in easy identification. We achieved en bloc resection with a snare and electrosurgical unit. All procedure were performed within 3 min without adverse events. Pathologic examination showed low-grade dysplasia with clear resection margins in one case and hyperplastic polyps in three cases.
UEMR can be an effective and safe treatment method for neoplasms in the gastric pyloric ring.
Core tip: We present four patients who underwent underwater endoscopic mucosal resection (UEMR) for the resection of neoplasms in the pyloric ring. UEMR for neoplasms in the pyloric ring has benefits similar to those of UEMR for colonic neoplasms: (1) Superficial lesions float into the snare as protruding lesions in underwater conditions; (2) UEMR decreases thermal damage; (3) Submucosal vessels usually remain within the resection wound, as the resection plane is superficial; and (4) The pyloric narrow lumen is constantly distended, retaining enough working space. Our case series suggested the potential of UEMR for treating neoplasms in the pyloric ring.
- Citation: Kim DH, Park SY, Park CH, Kim HS, Choi SK. Underwater endoscopic mucosal resection for neoplasms in the pyloric ring of the stomach: Four case reports. World J Clin Cases 2020; 8(14): 3050-3056
- URL: https://www.wjgnet.com/2307-8960/full/v8/i14/3050.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i14.3050
Performing endoscopic resection for tumors located in the pyloric ring is technically more difficult, as the anatomical characteristics of this region can affect the adequate assessment of margins and the working space for the procedure. Moreover, peristaltic movements of the peripyloric muscles are aggravated by submucosal injection or thermal stimuli during endoscopic procedures, preventing meticulous dissection of the lesion. These technical difficulties may be associated with incomplete resection of tumors and an increase in local recurrence and adverse events. Recently, underwater endoscopic mucosal resection (UEMR) was suggested by Binmoeller et al[1], which has been used in the treatment of challenging lesions in the duodenum and colorectum near the appendiceal orifice and dentate line; UEMR has shown good treatment results with a high complete resection rate and low adverse event rate[2-5]. UEMR has also been adapted for recurrent or residual lesions after endoscopic resection[6,7]. Here, we reported our experience of using UEMR for benign mucosal neoplasms located in the pyloric ring. To our knowledge, it is the first report on the effectiveness of UEMR for tumors in the pyloric ring.
Gastric neoplasms on pyloric ring.
Four patients diagnosed with gastric neoplasms on pyloric ring through screening endoscopy.
All four patients had no underlying disease that could promote bleeding or medications to promote bleeding.
All patients had no abnormal findings on physical examination.
In all patients, hemoglobin level, platelet count, activated partial thromboplastin time, and prothrombin time were all within normal range.
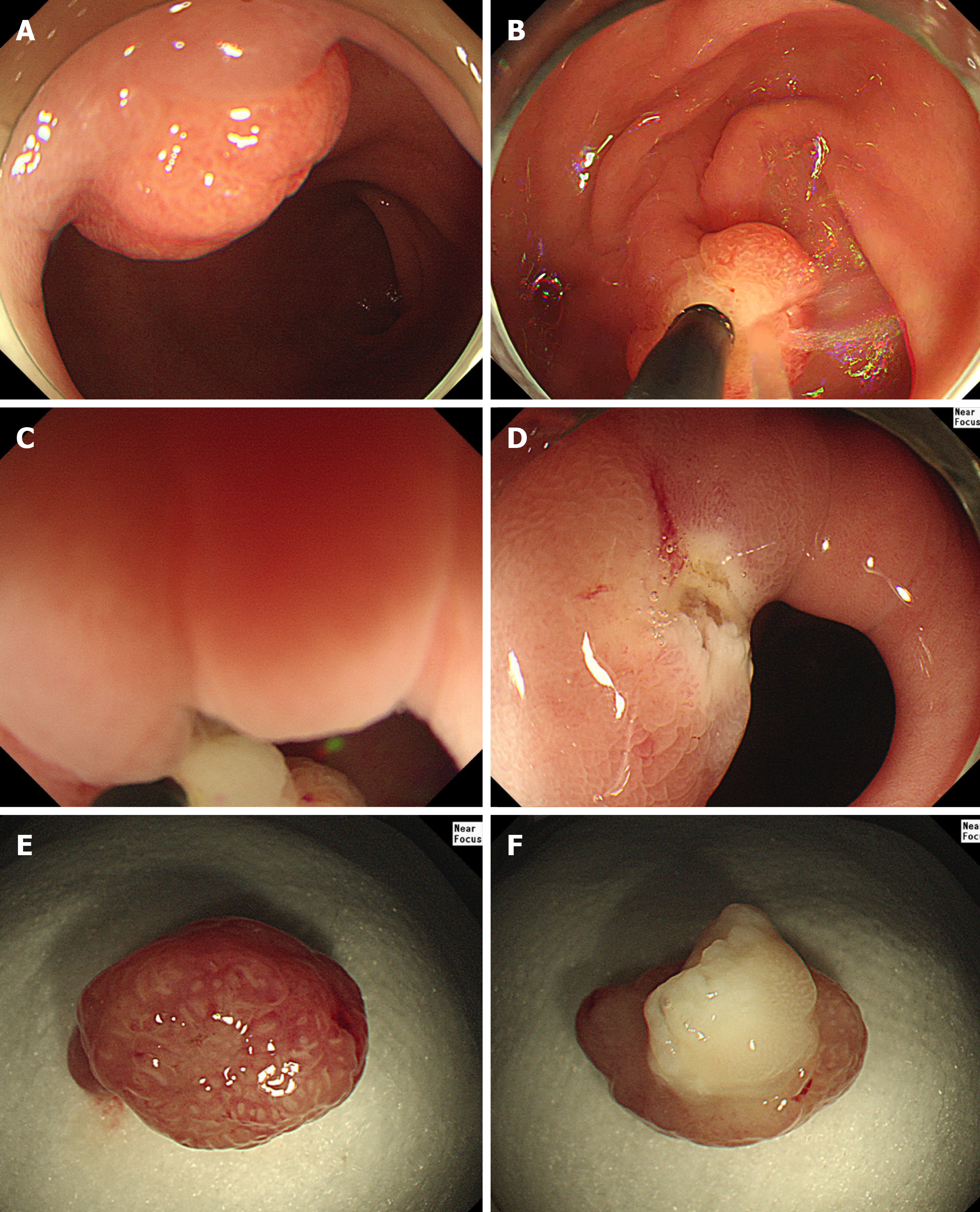
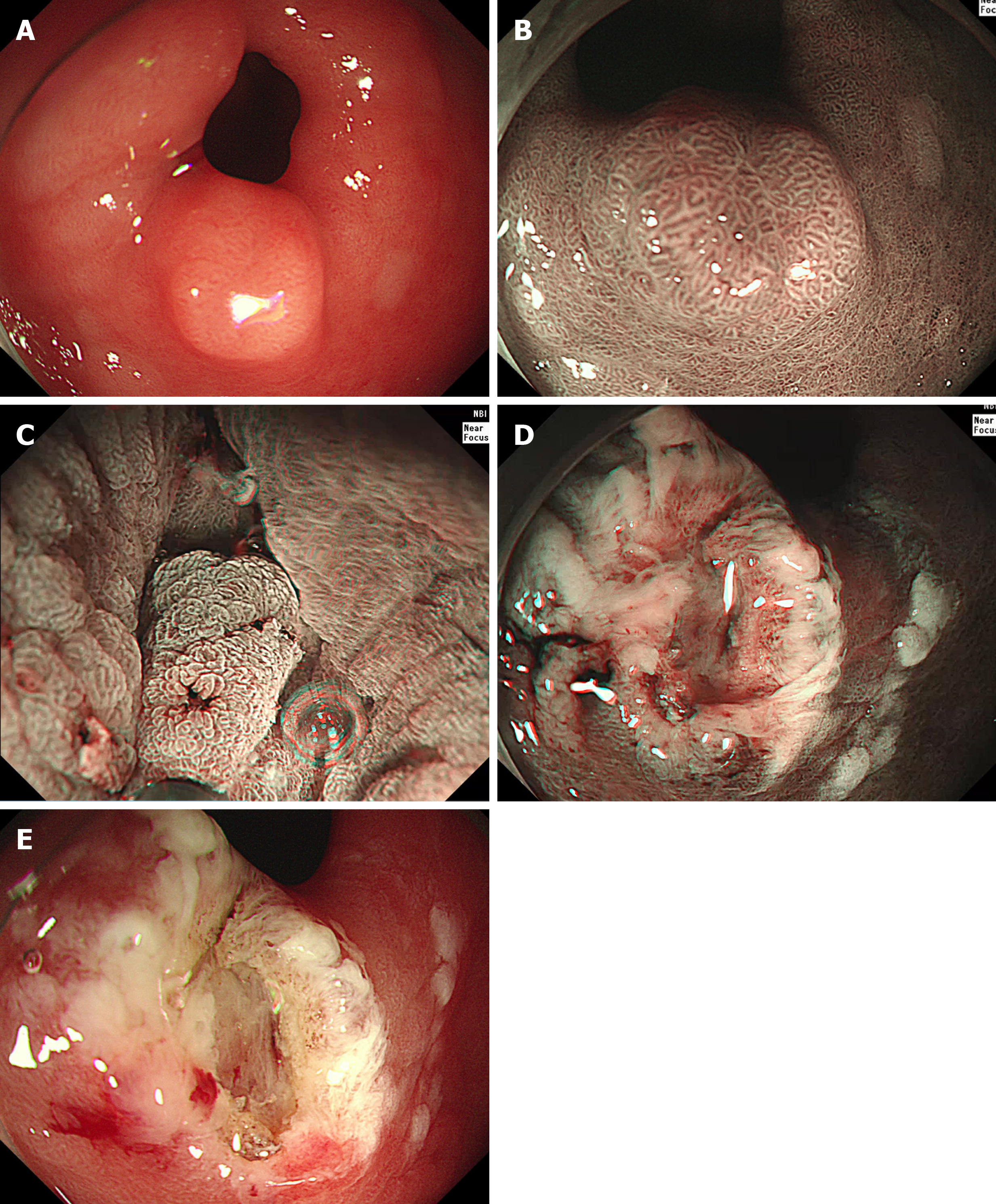
We performed UEMR for 4 patients with 4 mucosal neoplasms located in the pyloric ring. For moderate sedation, balanced sedation was performed in case 1, 3 and 4. Patients received initial intravenous induction of 25 mg pethidine and 0.05 mg/kg midazolam. After 2 min, intravenous propofol (10-20 mg increments) was given repetitively, to achieve an adequate sedation level. In case 2, the endoscopic procedure was consciously performed with an initial intravenous bolus administration of 25 mg pethidine. We used cap-assisted duodenoscopy with narrow-band imaging and a water jet pump device (GIF HQ290, Olympus). All endoscopic procedures were performed with the patient in the left lateral decubitus position. The stomach and the duodenal bulb were initially collapsed by aspiration, followed by instillation of 200-400 mL of water into the antrum and duodenal bulb. After performing UEMR, we removed instilled water as soon as possible to reduce the risk of aspiration pneumonia. The diameter of each neoplasm was less than 15 mm. We achieved en bloc resection with a crescent-type snare (Olympus device) and electrosurgical unit (VAIO 300D, ERBE Co. Ltd., Tubingen, Germany) with a high-frequency generator in all 4 patients. The settings of the VAIO 300D were as follows: Endocut-Q, effect 2, incision time 3, and incision interval 5. In a 48-year-old woman (Case No. 1), a 10-mm sized Yamada type III polyp on the pyloric ring of the stomach could not be entirely visualized using forward-viewing endoscopes (Figure 1). However, water infusion enabled slight floating of the lesion, and it was easily identified and grasped using a snare. A 64-year-old woman (Case No. 2) presented with a 7-mm sized Yamada type II polyp on the pyloric ring of the stomach. UEMR was performed in the same way as in the first case. In a 50-year-old man (Case No. 3), water infusion enabled slight floating of the lesion, and it was easily grasped using a snare (Figure 2). Finally, in a 60-year-old woman (Case No. 4), a 10-mm sized Yamada type II polyp was successfully removed by UEMR. All procedures were performed within 3 min without adverse events. Pathologic examination showed low-grade dysplasia with a clear resection margin in Case No. 3 and hyperplastic polyps in the other three cases (Table 1).
| Case No. | Age (yr)/sex | Neoplasm diameter | Yamada classification | Location of the lesion | Procedure time (s) | En bloc resection | Pathology |
| 1 | 48/Female | 10 mm | III | LC-AW | 129 | Yes | Hyperplastic polyp |
| 2 | 64/Female | 7 mm | II | PW | 169 | Yes | Hyperplastic polyp |
| 3 | 50/Male | 10 mm | I | GC | 147 | Yes | Low-grade dysplasia |
| 4 | 60/Female | 10 mm | II | PW | 144 | Yes | Hyperplastic polyp |
Mucosal neoplasm in the pyloric ring of the stomach.
Underwater endoscopic mucosal resection.
UEMR was successfully performed within 3 min without adverse events in 4 patients with a mucosal neoplasm in the pyloric ring. All patients were discharged without any adverse events after the procedure.
It is difficult to achieve complete resection of tumors located in the pyloric ring using conventional endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) due to limited working space, incomplete visualization using forward-viewing endoscopes, and peristaltic contractions of the lesion. These technical difficulties may lead to an increase in local recurrence[8]. To overcome incomplete visualization of the entire tumor or to determine the distal tumor margin, retroflexion maneuvers in the duodenum are suggested for the management of tumors in the pyloric ring. Another option is transnasal endoscope-assisted endoscopic resection, which enables submucosal tissue retraction to visualize the cutting line and increase the rate of complete resection[8-10]. However, these techniques need highly advanced endoscopic skills and facilities.
Our case series suggested the potential of UEMR for the treatment of neoplasms located in the pyloric ring. UEMR, with a relative short procedure time and low rate of adverse events, does not require high technical skills in endoscopic procedures[6]. UEMR for the management of neoplasms in the pyloric ring has benefits similar to those of UEMR for colorectal neoplasms: (1) Superficial lesions float into the snare as protruding lesions in underwater conditions; (2) UEMR decreases the thermal damage to the gastrointestinal wall, which helps prevent delayed perforation; and (3) The resection plane in UEMR is superficial; thus, the submucosal vessels usually remain within the resection wound, whereas in conventional EMR, the submucosal vessels are disrupted[2]. Moreover, the narrow pyloric lumen is constantly distended, resulting in sufficient working space.
Even though our case series included patients with neoplasms less than 15 mm in diameter located in the pyloric ring, UEMR for mucosal neoplasms involving the pyloric ring can be expected to have advantages over conventional EMR or ESD. Further studies are needed to elucidate the effectiveness and safety of UEMR for larger mucosal neoplasms located in the pyloric ring.
UEMR can be an effective and safe treatment method for lesions in the pyloric ring of the stomach. Further studies are needed to elucidate the effectiveness and safety of UEMR for variable-sized mucosal neoplasms in the pyloric ring.
| 1. | Binmoeller KF, Shah JN, Bhat YM, Kane SD. "Underwater" EMR of sporadic laterally spreading nonampullary duodenal adenomas (with video). Gastrointest Endosc. 2013;78:496-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 89] [Cited by in RCA: 121] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 2. | Yamasaki Y, Uedo N, Takeuchi Y, Higashino K, Hanaoka N, Akasaka T, Kato M, Hamada K, Tonai Y, Matsuura N, Kanesaka T, Arao M, Suzuki S, Iwatsubo T, Shichijo S, Nakahira H, Ishihara R, Iishi H. Underwater endoscopic mucosal resection for superficial nonampullary duodenal adenomas. Endoscopy. 2018;50:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 3. | Shibukawa G, Irisawa A, Sato A, Abe Y, Yamabe A, Arakawa N, Takasaki Y, Maki T, Yoshida Y, Igarashi R, Yamamoto S, Ikeda T, Hojo H. Endoscopic Mucosal Resection Performed Underwater for Nonampullary Duodenal Epithelial Tumor: Evaluation of Feasibility and Safety. Gastroenterol Res Pract. 2018;2018:7490961. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Binmoeller KF, Hamerski CM, Shah JN, Bhat YM, Kane SD. Underwater EMR of adenomas of the appendiceal orifice (with video). Gastrointest Endosc. 2016;83:638-642. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 5. | Ishaq S, Kuwai T. Rectal polyp reaching the dentate line: underwater EMR without submucosal lift. VideoGIE. 2017;2:53-54. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Iwagami H, Takeuchi Y, Yamasaki Y, Nakagawa K, Ohmori M, Matsuno K, Inoue S, Iwatsubo T, Nakahira H, Matsuura N, Shichijo S, Maekawa A, Kanesaka T, Higashino K, Uedo N, Ishihara R. Feasibility of underwater endoscopic mucosal resection and management of residues for superficial non-ampullary duodenal epithelial neoplasms. Dig Endosc. 2020;32:565-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 38] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 7. | Shichijo S, Uedo N, Takeuchi Y, Iwagami H, Ohmori M, Inoue S, Ishihara R. Underwater endoscopic mucosal resection of residual duodenal tumor. Endoscopy. 2019;51:E329-E330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Jung SW, Jeong ID, Bang SJ, Shin JW, Park NH, Kim DH. Successful outcomes of endoscopic resection for gastric adenomas and early cancers located on the pyloric ring (with video). Gastrointest Endosc. 2010;71:625-629. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Park JC, Kim JH, Youn YH, Cheoi K, Chung H, Kim H, Lee H, Shin SK, Lee SK, Kim H, Park H, Lee SI, Lee YC. How to manage pyloric tumours that are difficult to resect completely with endoscopic resection: comparison of the retroflexion vs. forward view technique. Dig Liver Dis. 2011;43:958-964. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Ahn JY, Choi KD, Choi JY, Kim MY, Lee JH, Choi KS, Kim DH, Song HJ, Lee GH, Jung HY, Kim JH. Transnasal endoscope-assisted endoscopic submucosal dissection for gastric adenoma and early gastric cancer in the pyloric area: a case series. Endoscopy. 2011;43:233-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Corresponding Author's Membership in Professional Societies: The Korean Society of Gastroenterology.
Specialty type: Medicine, research and experimental
Country of origin: South Korea
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Xie H S-Editor: Ma YJ L-Editor: A E-Editor: Xing YX