Published online Jun 26, 2020. doi: 10.12998/wjcc.v8.i12.2484
Peer-review started: February 26, 2020
First decision: March 31, 2020
Revised: May 25, 2020
Accepted: May 30, 2020
Article in press: May 30, 2020
Published online: June 26, 2020
Processing time: 118 Days and 19.9 Hours
In 2018, the diagnosis-related groups prospective payment system (DRGs-PPS) was introduced in a trial operation in Beijing according to the requirements of medical and health reform. The implementation of the system requires that more than 300 disease types pay through the DRGs-PPS for medical insurance. Colorectal cancer (CRC), as a common malignant tumor with high prevalence in recent years, was among the 300 disease types.
To investigate the composition and factors related to inpatient medical expenditure in CRC patients based on disease DRGs, and to provide a basis for the rational economic control of hospitalization expenses for the diagnosis and treatment of CRC.
The basic material and cost data for 1026 CRC inpatients in a Grade-A tertiary hospital in Beijing during 2014-2018 were collected using the medical record system. A variance analysis of the composition of medical expenditure was carried out, and a multivariate linear regression model was used to select influencing factors with the greatest statistical significance. A decision tree model based on the exhaustive χ2 automatic interaction detector (E-CHAID) algorithm for DRG grouping was built by setting chosen factors as separation nodes, and the payment standard of each diagnostic group and upper limit cost were calculated. The correctness and rationality of the data were re-evaluated and verified by clinical practice.
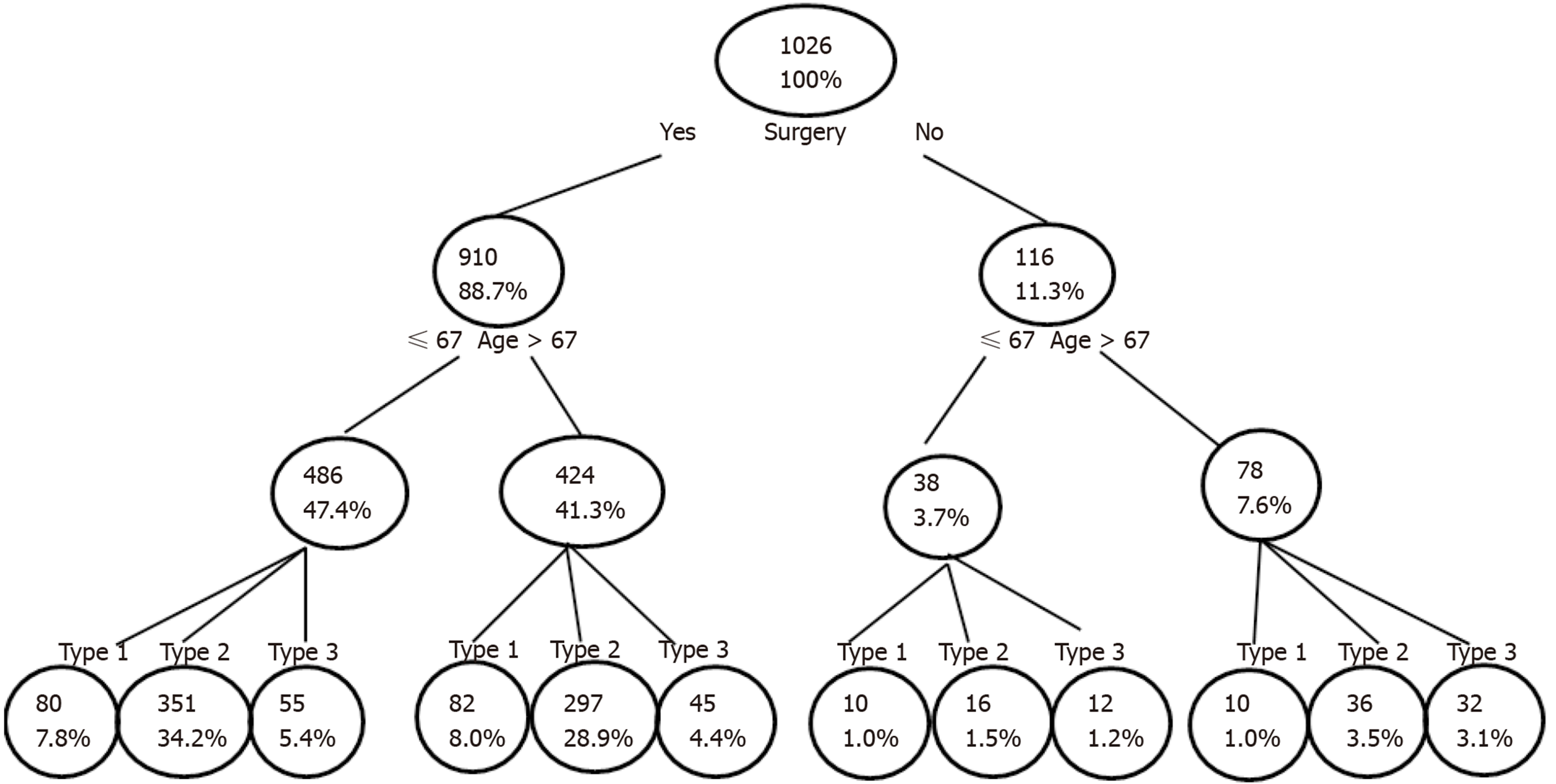
The average hospital stay of the 1026 CRC patients investigated was 18.5 d, and the average hospitalization cost was 57872.4 RMB yuan. Factors including age, gender, length of hospital stay, diagnosis and treatment, as well as clinical operations had significant influence on inpatient expenditure (P < 0.05). By adopting age, diagnosis, treatment, and surgery as the grouping nodes, a decision tree model based on the E-CHAID algorithm was established, and the CRC patients were divided into 12 DRG cost groups. Among these 12 groups, the number of patients aged ≤ 67 years, and underwent surgery and chemotherapy or radiotherapy was largest; while patients aged > 67 years, and underwent surgery and chemotherapy or radiotherapy had the highest medical cost. In addition, the standard cost and upper limit cost in the 12 groups were calculated and re-evaluated.
It is important to strengthen the control over the use of drugs and management of the hospitalization process, surgery, diagnosis and treatment to reduce the economic burden on patients. Tailored adjustments to medical payment standards should be made according to the characteristics and treatment of disease types to improve the comprehensiveness and practicability of the DRGs-PPS.
Core tip: This study analyzed the influencing factors on inpatient medical expenditure in colorectal cancer patients and the grouping results of diagnosis-related groups (DRGs) payment. A decision tree model based on the exhaustive χ2 automatic interaction detector algorithm for DRG grouping was built by setting chosen factors as separation nodes, and the payment standard of each diagnostic group and upper limit cost were calculated. By reorganizing and verifying the grouping payment standards through the practical study of real cases, the study provided a theoretical basis and validation methodology for the full implementation of DRGs payment management.
- Citation: Wu SW, Pan Q, Chen T. Research on diagnosis-related group grouping of inpatient medical expenditure in colorectal cancer patients based on a decision tree model. World J Clin Cases 2020; 8(12): 2484-2493
- URL: https://www.wjgnet.com/2307-8960/full/v8/i12/2484.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v8.i12.2484
In 2018, the diagnosis-related groups prospective payment system (DRGs-PPS) was introduced in a trial operation in Beijing according to the requirements of medical and health reform. Implementation of the system requires that more than 300 disease types pay through the DRGs-PPS for medical insurance. The concept of DRGs is now widely accepted as an international payment management system[1]. The basic mechanism of DRGs is to classify and combine diseases with similar characteristics into different diagnostic and treatment groups[2]. Accordingly, the principle of DRGs-PPS is to set a payment standard for each disease group according to the homogeneity of the clinical process and the similarity of resource consumption. By compre-hensively considering the overall physical condition, diagnosis, treatment, and prognosis of patients, the performance of homogeneous cases among different service providers can therefore be compared, so that the excessive growth of medical expenses can be regulated[3]. In clinical practice, patients and hospitals settle accounts according to the types of diseases, while medical insurance agencies allocate medical funds to hospitals accordingly. In this process, if the actual medical expenses of patients exceed the payment standards of the disease group, the medical service provider will need to share the responsibility of the overspend up to a certain proportion[4]. However, the limitation in disease coverage and sample capacity may generate deviations from the practical situation, which make it difficult for medical services to be provided effectively and efficiently to patients in need, leading to a separation of medical quality and medical consumption. For example, patients with cancer regardless of tumor type, metastasis and treatment, adopt a unified payment standard according to the current payment system[5]. Therefore, it is imperative to design a more practical methodology to specify the classification to conduct a more accurate payment standard calculation of DRG groups and strengthen medical expense control.
Colorectal cancer (CRC) is a common malignant tumor with high prevalence in recent years. The incidence of CRC ranks second of all malignant tumors in developed countries, and the mortality ranks third[6]. In China, the incidence and mortality of CRC have also significantly increased in recent years. Currently, the incidence of CRC ranks fourth of all malignant tumors, suggesting that it has become a serious public health issue in China[7]. Its high morbidity also leads to rapid growth in medical costs, which poses heavy economic pressure on patients and society.
In this study, we determined the main influencing factors related to inpatient medical expenditure in patients with CRC, to help medical institutions standardize the clinical diagnosis and treatment process in order to control medical cost[8]. Data on hospitalization cost for 1053 CRC patients in a Grade-A tertiary hospital in Beijing from 2014 to 2018 were collected. In building the decision tree model, indicators reflecting the intensity of resource consumption were used as the grouping nodes to classify the CRC cases into specified DRGs payment groups[9]. In this way, the study introduced the methodology to verify DRGs medical insurance payment standards, and provided a theoretical basis and practical application for the implementation of DRGs-PPS.
Medical records and cost information related to 1053 inpatients with CRC as the main diagnosis in a Grade-A tertiary hospital in Beijing from 2014 to 2018 were collected, and 1026 cases were included after removing cases with incomplete data. Basic information on these patients including age, gender, operation, treatment, prognosis, length of hospital stay and cost of hospitalization were obtained using the medical record system.
Single factor analysis was used to determine the influencing factors related to hospitalization expenses, and the results of variance analysis were further analyzed by multiple linear regression[10]. As the distribution of inpatient cost composition showed a skewed distribution, the analysis was carried out after logarithmic transformation. After the conversion, normally distributed data were represented by mean ± standard deviation, data with a non-normal distribution were represented by median number, enumeration data were represented by percentage, and P < 0.05 were considered statistically significant[11]. The influencing factors with the greatest impact on medical expenditure were selected and a cost prediction model was built to calibrate the relatively reasonable data. Finally, a decision tree model was established based on exhaustive χ2 automatic interaction detector (E-CHAID) to classify the cases into DRG groups, and the predicted cost of each group was determined through simulation prediction[12]. The rationality of grouping was evaluated according to data distribution by examining the heterogeneity between groups and the homogeneity within groups. All data and material collected were entered into Excel 2010 software (Microsoft Corporation, Redmond, Washington, United States), and statistical analyses were performed using SPSS21.0 (SPSS Inc., Chicago, IL, United States).
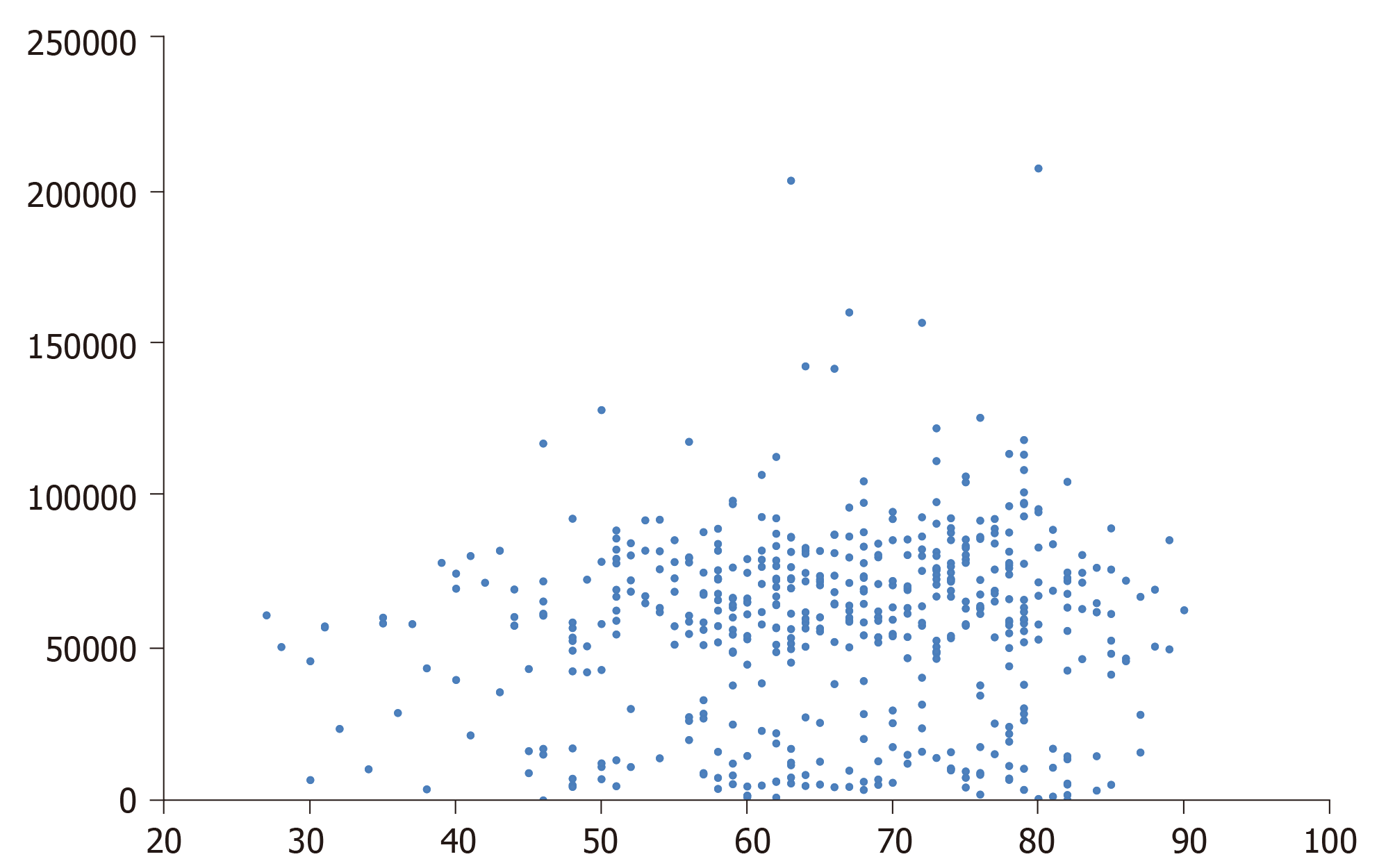
Of the 1026 inpatients with complete data, 489 were male and 537 were female; the average age was 67 ± 17 years; and the average length of hospital stay was 18.5 d. Among them, 1022 patients were cured or improved at discharge, accounting for 99.6%; while 4 patients died, accounting for 0.4%. The distribution of patients with different medical expenditure and age are shown in Figure 1. According to the scatter diagram, the greatest density of patients was distributed in the 60-70 age group with a total payment of 50000-100000 RMB yuan.
In the past 5 years, the average medical expenditure of CRC patients has been 57872.4 RMB yuan. According to the statistical analysis, the composition of hospitalization expenses mainly included: drug expenses of 20062.5 yuan (35.36%), surgery expenses of 18218.9 yuan (31.48%), treatment expenses of 10339.3 yuan (17.87%), examination expenses of 8225.9 yuan (14.21%), and other expenses (including blood transfusion expenses, nursing expenses, and bed expenses) of 1025.8 yuan (1.78%). Drug expenses accounted for the highest proportion of all items examined; while operation expenses, treatment expenses, and examination expenses were also important parts of hospitalization expenses.
Inpatient medical expenditure was converted logarithmically from a skewed distribution to normal distribution, and the factors affecting medical expenditure were statistically analyzed. The results showed that age, gender, length of hospital stay, and surgery had a significant impact on medical expenditure in the sample cases, and the difference was statistically significant (P < 0.05). The occurrence of hospital infection was not directly related to inpatient medical expenditure, as shown in Table 1.
| Influencing factors | Number | Average medical cost in RMB yuan | t / F | P value |
| Gender | 3. 732 | 0.025 | ||
| Male | 489 | 59273.4 | ||
| Female | 537 | 56596.6 | ||
| Age in yr | 3.184 | 0.011 | ||
| ≤ 0 | 118 | 47184.4 | ||
| 50-84 | 206 | 56413.4 | ||
| 60-13 | 290 | 59724.5 | ||
| 70-24 | 314 | 63554.3 | ||
| > 80 | 98 | 50122.0 | ||
| Length of hospital stay in d | ||||
| ≤ en | 182 | 16967.4 | 145.352 | 0.000 |
| 11-005 | 592 | 60226.3 | ||
| 21-26 | 198 | 73877.1 | ||
| > 30 | 56 | 109912.1 | ||
| Surgery | 231.157 | 0.000 | ||
| Yes | 910 | 63290.1 | ||
| No | 116 | 15371.1 | ||
| Hospital infection | 0.171 | |||
| Yes | 12 | 59790.5 | ||
| No | 1014 | 57849.7 | ||
| Treatment | ||||
| Maintenance therapy | 144 | 55757.4 | 0.004 | |
| Radiotherapy | 38 | 62032.2 | ||
| Chemotherapy | 662 | 56028.4 | ||
| Radiotherapy and chemotherapy | 182 | 65019.6 | ||
According to the results of single factor analysis, statistically significant factors such as gender, age, length of hospital stay, surgery and treatment were included in the multiple regression analysis, and the assignment of variables is shown in Table 2. The results showed that the length of hospital stay, surgery and treatment had negative effects on inpatient medical expenditure, while lower age had a positive effect. All of the factors investigated had a certain impact on medical expenditure. According to the standard regression coefficient, different types of treatment, the length of hospital stay, surgery and age had a greater influence on inpatient medical expenditure, while gender showed had a minor influence on medical cost. The imitative effect was preferable (R2adj = 0.962) upon examination, so that the model could be adopted as the basis for cost prediction and the data were regarded as reasonable data for DRG grouping[13].
| Variable | Variable assignment | Regression coefficient | Standardregression coefficient | t | P value |
| Gender | Male = 0 | ||||
| Female = 1 | -0.007 | -0.032 | 2.017 | < 0.05 | |
| Age | Actual value | 0.015 | 0.043 | 9.371 | < 0.05 |
| Length of hospital stay | Actual value | 0.039 | 0.231 | 18.27 | < 0.05 |
| Surgery | No = 0 | < 0.05 | |||
| Yes = 1 | 0.595 | 0.109 | 15.67 | < 0.05 | |
| Treatment | Maintenance therapy = 0 | < 0.05 | |||
| Radiotherapy = 1 | 5.294 | 0.042 | 2.62 | < 0.05 | |
| Chemotherapy = 2 | 4.786 | 0.073 | 2.37 | < 0.05 | |
| Radiotherapy and chemotherapy = 3 | 2.813 | 0.321 | 25.84 | < 0.05 |
Selection of node variables: According to the above-mentioned results, different types of treatment, length of hospital stay, surgery, and age had the greatest impact on medical expenditure. We decided to choose treatment, surgery, and age as node variables. Although length of hospital stay also had a significant influence on medical cost, considering the great variance in hospitalization, length of hospital stay was included as an influencing variable instead of a grouping variable in the decision tree model[14].
When the grouping node variables were selected, we constructed and conducted branch reduction on the decision tree model using SPSS 21.0 software, and the E-CHAID algorithm was adopted to build the decision tree[15]. In this study, we set inpatient medical expenditure as the dependent variable; length of hospital stay as the influencing variable; and age, surgery and follow-up treatment as classification nodes. The parameters used in this study were as follows: the maximum depth of the decision tree was 3, the minimum sample number of the parent node was 100, the minimum sample number of the child node was 50, and the significance level of the splitting node was α = 0.05. The difference between groups was examined using the Kruskal-Wallis test, and the variation coefficient was used to examine the rationality and effectiveness of grouping[16]. The grouping results are shown in Figure 2.
Grouping results and the calculation of standard medical costs in different DRGs: The 1026 inpatients were divided into 12 DRG groups using the variable nodes of treatment, surgery and age, as shown in Table 3. Among the 12 groups, group 3 had the largest number of patients aged ≤ 67 years, and underwent surgery and chemotherapy or radiotherapy; the patients aged > 67 years, and underwent surgery and chemotherapy or radiotherapy had the highest medical cost. The range of the payment standard for each DRG was defined by taking the concentration trend indicators and the trend indicators as references. The median medical cost of each combination was taken as the referential cost, and 75% of the referential cost of each combination plus 1.5 times the interquartile distance was used to calculate the upper limit of inpatient medical expenditure[17]. Cases exceeding the control line were marked as abnormal data for further analyses, so that the influence of amplitude in data variation could be eliminated. In addition, a dynamic adjustment on payment standards could be made by investigating the severity of the disease and medical resource consumption of cases exceeding the control limit[18].
| Group No. | Combination description | Number | Mean in RMB yuan | Standard deviation | Median in RMB yuan | Upper limit in RMB yuan | CV |
| 1 | Surgery, maintenance therapy, age ≤ 67 yr | 55 | 50726.7 | 14973.5 | 49335.7 | 71075.8 | 0.24 |
| 2 | Surgery, maintenance therapy, age > 67 yr | 45 | 53285.4 | 16784.2 | 51533.9 | 78229.0 | 0.42 |
| 3 | Surgery, chemotherapy or radiotherapy, age ≤ 67 yr | 351 | 56827.3 | 17256.3 | 55964.2 | 89934.1 | 0.33 |
| 4 | Surgery, chemotherapy or radiotherapy, age > 67 yr | 297 | 61154.3 | 15147.8 | 60924.5 | 91365.2 | 0.54 |
| 5 | Surgery, chemotherapy and radiotherapy, age ≤ 67 yr | 80 | 62244.6 | 18475.6 | 61574.3 | 93574.2 | 0.65 |
| 6 | Surgery, chemotherapy and radiotherapy, age > 67 yr | 82 | 65647.3 | 17985.1 | 65879.1 | 95498.3 | 0.14 |
| 7 | Non-surgery, maintenance therapy, age ≤ 67 yr | 12 | 41995.3 | 11425.5 | 42703.1 | 67470.7 | 0.31 |
| 8 | Non-surgery, maintenance therapy, age > 67 yr | 32 | 42203.3 | 12574.3 | 44217.5 | 68154.2 | 0.56 |
| 9 | Non-surgery, chemotherapy or radiotherapy, age ≤ 67 yr | 16 | 52309.7 | 16785.1 | 50557 | 71256.1 | 0.64 |
| 10 | Non-surgery, chemotherapy or radiotherapy, age > 67 yr | 36 | 52775 | 14287.1 | 51427.2 | 72546.3 | 0.45 |
| 11 | Non-surgery, chemotherapy and radiotherapy, age ≤ 67yr | 10 | 55681.4 | 17694.2 | 53214.5 | 76085. 4 | 0.41 |
| 12 | Non-surgery, chemotherapy and radiotherapy, age > 67 yr | 10 | 56930 | 21454.1 | 53945.7 | 78945.0 | 0.71 |
According to epidemiological statistics, the incidence and mortality of CRC have been increasing in China over the past few years[19]. It has become a serious threat to public health, and has led to an escalation of medical cost that poses economic burden on patients and society. The results of this study showed that during 2014-2018, the average length of stay for CRC patients in the sample hospital was 18.5 d, and the average inpatient medical expenditure in CRC patients was 57872.4 yuan. It was also revealed that the overall medical cost for CRC patients mainly included drug cost, surgery cost, treatment cost, and examination cost. Among them, drug cost accounted for the highest proportion of the overall medical cost. Surgery, treatment, and examination costs also accounted for a large proportion of the medical expenditure. The high cost of medication was obviously related to the extensive use of high-value drugs during chemotherapy and molecule-targeted therapy[20]. Therefore, it is necessary for medical institutions to strengthen the management of clinical medication and place greater emphasis on rational drug use in clinical practice. The high expenditure on surgery, treatment, and examination were also in accordance with the characteristics of cancer treatment. This increased tendency reflected the positive effect of medical reform policy as the labor force of medical staff has been increasingly recognized[21].
Our results showed that the differences in treatment and length of hospital stay, were crucial influencing factors for inpatient medical expenditure in CRC patients. It was obvious that the variation in treatment was directly related to the differences in the cost of hospitalization[12]. It can be seen from the grouping results that the calculated standard cost and upper limit cost of patients who underwent chemotherapy and/or radiotherapy were significantly higher than of those who underwent maintenance therapy in the same age groups and with similar other related factors. In addition, the adoption of surgical treatment also adds to the medical expenditure as it increases the cost and difficulty of treatment, and the patient requires more time to recover[22].
Also, the length of hospital stay is widely recognized as an important factor in medical cost. An extended hospitalization would therefore increase the medical costs of patients. In addition, advanced age is also positively correlated with increased medical expenditure in CRC inpatients, as elderly patients are inclined to suffer from more underlying diseases that require special treatments[23]. Thus, the length of hospital stay in elderly patients is prolonged, which results in a further increase in medical expenditure. Therefore, on the basis of ensuring the quality and safety of medical service, it is imperative for medical institutions to strengthen hospitalization control as reducing hospital stay could promote efficiency, reduce waste of medical resources, and alleviate the economic burden on patients.
The E-CHAID algorithm is an improved version of the CHAID algorithm, which is widely used in the analysis of classified quantitative data. It is based on the principle of objective optimization, with the functions of target selection, variable selection and clustering analysis[24]. By conducting optimal segmentation of the given dependent variable through the selection of explanatory variables in the data, and using the χ2 test or variance analysis to automatically determine the significance of grouping, the differences between subgroups are as distant as possible, whereas the differences within subgroups are as close as possible[25]. In conducting the E-CHAID algorithm, the grouping process was carried out to select the best grouping variable nodes, which is more suitable for establishing a DRG classification model[17].
The aim of DRGs-PPS is to classify and combine disease categories with similar diagnoses and treatments, and set a payment standard for each group. It is widely adopted and recognized as an ideal method of payment management among medical institutions in China[20]. However, the accuracy and practicability of the results should be carefully verified through clinical practice by considering the characteristics of epidemiology, patients as well as diagnoses and treatments of the diseases. In the present study, CRC was chosen as a sample disease, and the basic medical data on inpatients within a Grade-A tertiary hospital in Beijing during 2014-2018 were collected. In this study, we chose factors with the greatest influence on medical expenditure as grouping nodes, and a decision tree model was adopted to classify the cases according to the medical resource consumption. The grouping results and the calculation of standard charges were consistent with the practical situation in the clinic through re-validation, which greatly enhanced the practicability and effectiveness of grouping[26]. The study provided a solid basis for the actual implementation of DRGs payment within the region, and offered a practical methodology for health administrative departments to formulate and adjust medical insurance payment standards.
There were some limitations in this study. It is widely acknowledged that medical expenditures are affected by a number of factors such as the basic condition and individual characteristics of patients, along with other objective factors such as regional price index, the size and scale of the hospital as well as social and economic characteristics of the region. Therefore, factors such as clinical diagnosis and treatment, demands of patients, and local epidemiology should all be taken into account in setting cost standards[27]. In addition, the prospective change due to the impact of medical reform policy in medical institutions such as the removal of drug and medical material compensation, and the promotion on the charge of medical service, should also be considered in real practice. In this study, the basic and cost data on CRC inpatients within a Grade-A tertiary hospital in Beijing over 5 years were used as the sample for analysis. Due to regional and periodic limitation in the accessibility of data, the generalization of these results in other areas should be carried out with caution. The data of patients from other medical institutions over a longer time period are suggested to be included to improve the reliability and validity of the present study, and the results should be re-evaluated and adjusted by further investigation and practice.
In conclusion, this study analyzed the influencing factors on inpatient medical expenditure in CRC patients and the grouping results of DRGs payment. The grouping payment standards were reorganized and verified through a practical study of real cases, and provided a theoretical basis and validation methodology for the full implementation of DRGs payment management. In order to strengthen cost management in CRC, it is suggested that medical institutions should attach greater importance to the process of diagnosis and treatment, emphasize rational drug use, shorten the average length of hospital stay to effectively control hospitalization cost in CRC patients, and reduce the financial burden on families and society.
In 2018, the diagnosis-related groups prospective payment system (DRGs-PPS) was introduced in a trial operation that required more than 300 disease types pay through the DRGs-PPS for medical insurance in Beijing.
The study investigated the composition and factors related to inpatient medical expenditure in colorectal cancer (CRC) patients based on disease DRGs, and provide a basis for the rational economic control of hospitalization expenses for the diagnosis and treatment of CRC.
In practice, the basic material and cost data for 1026 CRC inpatients in a Grade-A tertiary hospital in Beijing during 2014-2018 were collected.
Variance analysis of the composition of medical expenditure as well as the multivariate linear regression model were used to select influencing factors. Then, a decision tree model based on the E-CHAID algorithm for DRG grouping was built by setting chosen factors as separation nodes, and the payment standard of each diagnostic group and upper limit cost were calculated, while the correctness and rationality of the data were re-evaluated and verified by clinical practice.
Results showed that the average hospital stay of the 1026 CRC patients investigated was 18.5 d, and the average hospitalization cost was 57872.4 RMB yuan. Factors including age, gender, length of hospital stay, diagnosis and treatment, as well as clinical operations had a significant influence on inpatient expenditure. Age, diagnosis, treatment, and surgery were adopted as the grouping nodes in building the decision tree model, and the CRC patients were divided into 12 DRGs cost groups, the standard cost and upper limit cost of each group were calculated and re-evaluated.
The study provided a practical methodology for the practical implementation of the DRGs-PPS and enhanced the comprehensiveness and practicability in cost control management.
| 1. | Schlembach D, Hund M, Schroer A, Wolf C. Economic assessment of the use of the sFlt-1/PlGF ratio test to predict preeclampsia in Germany. BMC Health Serv Res. 2018;18:603. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Richards F, Pitluk H, Collier P, Powell S, Dion C, Struchen-Shellhorn W, Plunkett M. Reducing unnecessary Medicare hospital admissions for chest pain in Arizona and Florida. Prof Case Manag. 2008;13:74-84; quiz 85-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Zindel S, Stock S, Müller D, Stollenwerk B. A multi-perspective cost-effectiveness analysis comparing rivaroxaban with enoxaparin sodium for thromboprophylaxis after total hip and knee replacement in the German healthcare setting. BMC Health Serv Res. 2012;12:192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Epelboym I, Winner M, Allendorf JD. MRCP is not a cost-effective strategy in the management of silent common bile duct stones. J Gastrointest Surg. 2013;17:863-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Gutensohn W, Thiel E, Buschette S. Ecto-5'-nucleotidase as a leukemia marker. Adv Exp Med Biol. 1984;165 Pt B:249-253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 6. | Montazeri Z, Li X, Nyiraneza C, Ma X, Timofeeva M, Svinti V, Meng X, He Y, Bo Y, Morgan S, Castellví-Bel S, Ruiz-Ponte C, Fernández-Rozadilla C, Carracedo Á, Castells A, Bishop T, Buchanan D, Jenkins MA, Keku TO, Lindblom A, van Duijnhoven FJB, Wu A, Farrington SM, Dunlop MG, Campbell H, Theodoratou E, Zheng W, Little J. Systematic meta-analyses, field synopsis and global assessment of the evidence of genetic association studies in colorectal cancer. Gut. 2019;. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 7. | Wong CK, Lam CL, Poon JT, McGhee SM, Law WL, Kwong DL, Tsang J, Chan P. Direct medical costs of care for Chinese patients with colorectal neoplasia: a health care service provider perspective. J Eval Clin Pract. 2012;18:1203-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 8. | Alefan Q, Malhees R, Mhaidat N. Direct medical cost associated with colorectal cancer in north of Jordan. Curr Probl Cancer. 2017;41:371-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Shi J, Liu G, Wang H, Mao A, Liu C, Guo L, Huang H, Ren J, Liao X, Bai Y, Sun X, Zhu X, Wang J, Song B, Zhou J, Zhu L, Lei H, Liu Y, Liu Y, Du L, He Y, Zhang K, Li N, Chen W, Dai M, He J. Medical expenditures for colorectal cancer diagnosis and treatment: A 10-year high-level-hospital-based multicenter retrospective survey in China, 2002-2011. Chin J Cancer Res. 2019;31:825-837. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 10. | Tanguy-Melac A, Aguade AS, Fagot-Campagna A, Gastaldi-Ménager C, Sabaté JM, Tuppin P. Management and intensity of medical end-of-life care in people with colorectal cancer during the year before their death in 2015: A French national observational study. Cancer Med. 2019;8:6671-6683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Grubinger T, Kobel C, Pfeiffer KP. Regression tree construction by bootstrap: model search for DRG-systems applied to Austrian health-data. BMC Med Inform Decis Mak. 2010;10:9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Ferrando A, Pagano E, Scaglione L, Petrinco M, Gregori D, Ciccone G. A decision-tree model to estimate the impact on cost-effectiveness of a venous thromboembolism prophylaxis guideline. Qual Saf Health Care. 2009;18:309-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Luo AJ, Chang WF, Xin ZR, Ling H, Li JJ, Dai PP, Deng XT, Zhang L, Li SG. Diagnosis related group grouping study of senile cataract patients based on E-CHAID algorithm. Int J Ophthalmol. 2018;11:308-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Kobayashi D, Takahashi O, Arioka H, Koga S, Fukui T. A prediction rule for the development of delirium among patients in medical wards: Chi-Square Automatic Interaction Detector (CHAID) decision tree analysis model. Am J Geriatr Psychiatry. 2013;21:957-962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 15. | Li H, Wu TT, Yang DL, Guo YS, Liu PC, Chen Y, Xiao LP. Decision tree model for predicting in-hospital cardiac arrest among patients admitted with acute coronary syndrome. Clin Cardiol. 2019;42:1087-1093. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 16. | Feretzakis G, Kalles D, Verykios VS. Hiding Decision Tree Rules in Medical Data: A Case Study. Stud Health Technol Inform. 2019;262:368-371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Imai S, Yamada T, Kasashi K, Ishiguro N, Kobayashi M, Iseki K. Construction of a flow chart-like risk prediction model of ganciclovir-induced neutropaenia including severity grade: A data mining approach using decision tree. J Clin Pharm Ther. 2019;44:726-734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Kuo CY, Yu LC, Chen HC, Chan CL. Comparison of Models for the Prediction of Medical Costs of Spinal Fusion in Taiwan Diagnosis-Related Groups by Machine Learning Algorithms. Healthc Inform Res. 2018;24:29-37. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 19. | Lee S, Harland K, Mohr NM, Matthews G, Hess EP, Bellolio MF, Han JH, Weckmann M, Carnahan R. Evaluation of emergency department derived delirium prediction models using a hospital-wide cohort. J Psychosom Res. 2019;127:109850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 20. | Murphy EL, Comiskey CM. Using chi-Squared Automatic Interaction Detection (CHAID) modelling to identify groups of methadone treatment clients experiencing significantly poorer treatment outcomes. J Subst Abuse Treat. 2013;45:343-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 12] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Miller B, Fridline M, Liu PY, Marino D. Use of CHAID decision trees to formulate pathways for the early detection of metabolic syndrome in young adults. Comput Math Methods Med. 2014;2014:242717. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Jian W, Lu M, Han W, Hu M. Introducing diagnosis-related groups: is the information system ready? Int J Health Plann Manage. 2016;31:E58-E68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 23. | Peltola M, Quentin W. Diagnosis-related groups for stroke in Europe: patient classification and hospital reimbursement in 11 countries. Cerebrovasc Dis. 2013;35:113-123. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 24. | Avilés-Jurado FX, León X. Prognostic factors in head and neck squamous cell carcinoma: comparison of CHAID decision trees technology and Cox analysis. Head Neck. 2013;35:877-883. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 25. | Yu T, He Z, Zhou Q, Ma J, Wei L. Analysis of the factors influencing lung cancer hospitalization expenses using data mining. Thorac Cancer. 2015;6:338-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Chen S. Detection of fraudulent financial statements using the hybrid data mining approach. Springerplus. 2016;5:89. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 32] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 27. | Atieh MA, Pang JK, Lian K, Wong S, Tawse-Smith A, Ma S, Duncan WJ. Predicting peri-implant disease: Chi-square automatic interaction detection (CHAID) decision tree analysis of risk indicators. J Periodontol. 2019;90:834-846. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
Open-Access: This article is an open-access article that was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution NonCommercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See:
Manuscript source: Unsolicited manuscript
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Faerch K, Ishibashi H, Munjal K S-Editor: Zhang L L-Editor: Filipodia E-Editor: Xing YX